The coronavirus, like all viruses, has mutated numerous times since it first appeared in China in late 2019. Throughout the pandemic, a number of variants have surfaced, changing the virus transmissibility, risk profile, and even symptoms. As the virus remains to mutate and transform its underlying role to evade the immune defenses, humanity faces a major challenge. In recent times, the delta plus variant has raised serious public health issues in India, in the United Kingdom, and other nations around the globe, and it has shown viable infections in 20 to 55% of people who have recovered from COVID-19 originating from different strains.
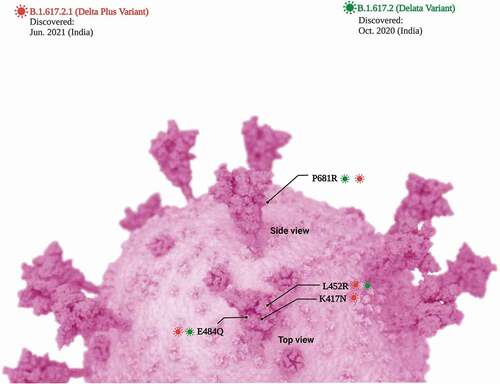
The ‘severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)’ variant strains identified in India consist of three main lineages (‘double mutant’ variant): Kappa variant, Delta variant, and B.1.618 [Citation1,Citation2]. It is believed that the delta variant lacks the 484 K/Q mutation, which has now been related to vaccination resistance [Citation3,Citation4]. Currently, 63 Delta variant genomes with the K417N mutation were recognized by the GISAID. Delta plus variant (AY.1 variant or B.1.617.2.1) is the modified version of the delta variant which has brought a devastating second COVID-19 wave in India and it has been declared as a ‘variant of concern (VOC)’ by the World Health Organization [Citation5,Citation6]. As of 28 November 2021 more than 500 cases of delta plus variant have been reported in 12 countries, in particular in the US, UK, and India [Citation7]. A molecular examination of B.1.617 receptor-binding domain (RBD) mutations (L452R and E484Q, as well as P681R at the furin cleavage site) suggests that these polymorphisms may result in higher angiotensin-converting enzyme receptor 2 binding and rate of S1-S2 cleavage, leading to improved transmissibility and perhaps the ability to avoid binding and neutralization by certain monoclonal antibodies [Citation4]. The delta plus variant differs from the conventional delta variant due to a supplemental mutation in the RBD known as K417N that is also noticed in the beta variant first identified in South Africa. The delta plus variant seems to have some tolerance against monoclonal antibody combination therapy, which is the only clinical distinction from the delta variant [Citation8,Citation9]. In addition, delta plus variant has increased transmissibility and higher binding capacity to lung epithelial cells as compared to other VOCs. Besides that, one more sublineage of the Delta variant was identified in Vietnam, which may have contributed to the latest rise in prevalence. These variations (provisionally dubbed Delta-V) were originally assumed to be a fusion virus due to mutations discovered in the S protein of the Alpha (B.1.1.7) variant [Citation9]. As per Kannan and coworkers, ‘Signature mutations in Spike (G142D, A222V, and T95I) existed at a more significant percentage in the Delta Plus variant than the Delta variant. Three mutations in Spike (K417N, V70F, and W258L) were exclusively present in the Delta Plus variant. A new mutation was identified in ORF1a (A1146T), which was only present in the Delta Plus variant with ~58% prevalence. Apart from that other four mutation are detected in the ORF1a i.e. P1604L, A3209V, V3718S, and T3750I. Furthermore, five key mutations (T95I, A222V, G142D, R158G, and K417N) were significantly more prevalent in the Delta Plus than in the Delta variant () [Citation10].’
The R number (R0 value) is a method of assessing the potential of a coronavirus or any disease to spread. R is the average number of people to whom one infected person will spread a virus. The R0 value for the alpha variant is 4–5 while for the delta variant, it is 5–8. The additional mutation in the RBD (as compared to the delta variant) influences the transmissibility and virulence of the new delta plus variant that contributes to the even higher R0 value. The delta plus variant is a sublineage of the delta variant, with the only known difference being a mutation, K417N, in the virus’ spike protein, which allows it to infect lung cells while in a combination with N501Y fully abolished the antibody effect [Citation9].
From the first case of delta plus variant surfaced in Madhya Pradesh on 10 June 2021, India reported 48 cases that had spread sporadically across nine different states from 45,000 samples sequenced while one death reported due to delta plus variant. Maharashtra reported a maximum of 20 cases, 9 in Tamil Nadu, 7 cases in Madhya Pradesh, 3 cases in Kerala, 2 each in Punjab and Gujarat while one case reported in Andhra Pradesh, J&K, Karnataka, Odisha, and Rajasthan [Citation11]. As of today delta plus variant is responsible for more than 10% of new cases of COVID-19 in the UK and 6% in the USA. Currently, 90% of the COVID-19 cases in India are due to delta variant. The Indian Government has asserted that both Covaxin® and Covishield® work well against all the VOCs of SARS-CoV-2, however, according to researchers from Oxford University, both Pfizer/BioNTech and AstraZeneca vaccines are effective against kappa and delta variants, although the effectiveness against the delta plus variant is not clear [Citation12]. One significant threat that has alarmed the medical profession is that the new delta plus strain may be able to circumvent immunity acquired by either the vaccine or previous infection. The United Kingdom is already providing booster doses of the Covid vaccine to high-risk people ahead of winter to ensure they have adequate protection against coronavirus. Mutational changes in the RBD of the viral spike protein is responsible for the antibody evasion as it is the primary target of the neutralizing antibody response. A research study conducted by Arora and coworkers suggests that the delta plus variant is resistant to neutralization by bamlanivimab and etesevimab (Due to K417N mutation) and they also noted reduced neutralization for the BNT162b2/Comirnaty vaccination [Citation9]. According to the research of Solo and Colleague [Citation13], ‘Medicinal plants rich in poly-methoxyflavones and poly-ethoxyflavones are useful as delta plus variant spike protein inhibitors.’ The Delta form is more resistant to neutralization by sera from convalescent patients who have not been immunized, especially one year following infection [Citation14]. There is 5.11 fold reduction is neutralization capability for delta plus variant infection in individuals vaccinated with the BNT162b2 (Pfizer/BioNTech) and ChAdOx1 (Oxford/AstraZeneca) vaccines [Citation15]. Similarly, Wang and colleagues also concluded that there is a need of a booster dose to the populations that exhibited lower vaccine-induced immune responses against emerging variants [Citation16]. mRNA-1273 (Moderna), BNT162b2 (Pfizer/BioNTech) and ChAdOx1 (Oxford/AstraZeneca) vaccines reduces new infections with delta variants but, efficacy and peak viral burden reduction are diminished [Citation17–19]. As per scientific study published in nature, two dose of vaccine decreses the delta variant load in the vaccinated individual as compared to unvaccinated but after two months of getting second dose immune protection starts decreses and a booster dose is needed to provide better immune protection [Citation20]. summarizes SARS-CoV-2 variants and its characteristics.
Table 1. SARS-CoV-2 variants and its characteristics
As per WHO on November 26, ‘The recently found B.1.1.529 strain of COVID-19 (first identified in southern Africa) was designated as a variant of concern status and retitled it as Omicron. The classification places Omicron in the most troublesome category of COVID-19 variants, alongside the world-dominant Delta and its weaker rivals Alpha, Beta, and Gamma [Citation21,Citation22]’. The viral spike protein has reported 32 mutations () with 15 mutations in the receptor-binding domain (RBD) that ultimately affect viral transmissibility, immune system evasion of the virus, and vaccine resistance [Citation23,Citation24]. T478 is a mutation seen in both Delta and Omicron variants. In the Omicron variation, the E484A mutation has a binding affinity that may result in improved ACE2 binding. The Omicron form of ACE2 binds to SARS-CoV-2 more strongly than the Delta variation of hACE2 [Citation25]. The outcomes of SARS-CoV-2 infections are less severe for omicron variant then with Delta variant lineages with age group from 5 to more than 65 years of age [Citation26]. According to Flemming [Citation27], ‘Although viral escape from neutralizing antibodies can facilitate breakthrough infections in vaccinated and convalescent individuals, it is worth noting that pre-existing cellular and innate immunity, non-neutralizing antibodies, as well as residual neutralizing antibodies are still likely to protect from severe disease.’ Omicron variant also showed weaker cell-cell fusion activity when compared with Delta variant in VeroE6/TMPRSS2 cells [Citation28]. The presence of a high number of Omicron variant mutations is also a distinguishing feature of the variants, implying that viral evolution in immunocompromized individuals may have played a key role in their creation [Citation29,Citation30]. Because many people around the world suffer from inherent or induced immunosuppression, the association between immunosuppression and the production of highly transmissible or pathogenic SARS-CoV-2 variants has to be researched further and mitigation techniques developed. In order to provide proper immune protection against omicron variant there is a need of booster dose for the mRNA based vaccines approved as two doses of mRNA-based vaccines elicit poor neutralization of Omicron [Citation31].
Variants with enhanced disease transmission and the ability to evade antibodies represent a threat to pandemic control and mitigation efforts. In addition, places with lower immunization coverage may experience new epidemics. Even after the mutations, no distinctive precautions are required. We must strive to vaccinate as many people as possible, increase genomic vigilance to monitor the virus transformation, and obey COVID-appropriate behavior and attitude.
Declaration of interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Acknowledgments
V.P.C wants to dedicate this article to L M College of Pharmacy, Ahmedabad (India) on 75th Year celebration of the college. The authors would like to thank the Immunology and Translational Research Group for their significant contribution. The Mechanisms and Interventions in Health and Disease Program within the Institute for Health and Sport, Victoria University, Australia, are also appreciated for their support. V.P. is grateful to the L.M. College of Pharmacy, Ahmedabad, India, for providing necessary support in carrying out the literature search. Figure is created using Biorender.com.
Additional information
Funding
References
- Ferreira I, Datir R, Papa G, et al. SARS-CoV-2 B.1.617 emergence and sensitivity to vaccine-elicited antibodies. bioRxiv. 2021:2021.05.08.443253. DOI:https://doi.org/10.1101/2021.05.08.443253.
- Liu J, Liu Y, Xia H, et al. BNT162b2-elicited neutralization of B.1.617 and other SARS-CoV-2 variants. Nature [Internet]. 2021;596:273–275.
- Ranjan R, Sharma A, and Verma MK. Characterization of the second wave of COVID-19 in India. medRxiv. 2021:2021.04.17.21255665. DOI:https://doi.org/10.1101/2021.04.17.21255665
- Cherian S, Potdar V, Jadhav S, et al. Convergent evolution of SARS-CoV-2 spike mutations, L452R, E484Q and P681R, in the second wave of COVID-19 in Maharashtra, India. bioRxiv. 2021:2021.04.22.440932. DOI:https://doi.org/10.1101/2021.04.22.440932.
- Kumar A, Parashar R, Kumar S, et al. Emerging SARS-CoV-2 variants can potentially break set epidemiological barriers in COVID-19. J Med Virol [Internet]. 2021;n/a. DOI:https://doi.org/10.1002/jmv.27467.
- Thakur V, Bhola S, Thakur P, et al. Waves and variants of SARS-CoV-2: understanding the causes and effect of the COVID-19 catastrophe. Infection [Internet]. 2021. DOI:https://doi.org/10.1007/s15010-021-01734-2.
- Yeung J, Suri M. There are at least 200 known cases of the Delta Plus coronavirus variant worldwide. Here’s what we know [Internet]. CNN Heal. [cited 2021 Nov 28]. p. Updated 0209 GMT (1009 HKT) June 26, 2021. Available from: https://edition.cnn.com/2021/06/25/health/delta-plus-variant-explainer-intl-hnk-scn/index.html
- Raman R, Patel KJ, Ranjan KCOVID-19. Unmasking emerging SARS-CoV-2 variants, vaccines and therapeutic strategies. Biomolecules. 2021;12:11.
- Arora P, Kempf A, Nehlmeier I, et al. Delta variant (B.1.617.2) sublineages do not show increased neutralization resistance. Cell Mol Immunol [Internet]. 2021;18:2557–2559.
- Kannan SR, Spratt AN, and Cohen AR, et al. Evolutionary analysis of the delta and delta plus variants of the SARS-CoV-2 viruses. J Autoimmun. 2021;124:102715.
- Explained: what is Covid-19 delta plus variant [Internet]. Times of India; 2021 [cited 2021 Nov 26]. p. Updated: Jun 25, 2021, 18:49 IST. Available from: https://timesofindia.indiatimes.com/india/explained-what-is-covid-19-delta-plus-variant/articleshow/83840705.cms
- Jeong M. Delta plus variant of SARS-CoV-2: how does it compare with the delta variant? [Internet]. 2021 [cited 2021 Nov 28]. Available from: https://www.medicalnewstoday.com/articles/delta-plus-variant-of-sars-cov-2-how-does-it-compare-with-the-delta-variant
- Solo P, and Doss MA. Potential inhibitors of SARS-CoV-2 (COVID 19) spike protein of the delta and delta plus variant: in silico studies of medicinal plants of North-East India. Curr Res Pharmacol Drug Discov [Internet]. 2021;2:100065. Available from: https://www.sciencedirect.com/science/article/pii/S2590257121000523
- Planas D, Veyer D, Baidaliuk A, et al. Reduced sensitivity of SARS-CoV-2 variant delta to antibody neutralization. Nature. 2021;596:276–280.
- Davis C, Logan N, Tyson G, et al. Reduced neutralisation of the Delta (B.1.617.2) SARS-CoV-2 variant of concern following vaccination. medRxiv [Internet]. 2021;2021.06.23.21259327. Available from: http://medrxiv.org/content/early/2021/06/28/2021.06.23.21259327.abstract
- Wang B, Goh YS, Fong S-W, et al. Resistance of SARS-CoV-2 Delta variant to neutralization by BNT162b2-elicited antibodies in Asians. Lancet Reg Heal – West Pacific [Internet]. 2021;15. Available from: https://doi.org/https://doi.org/10.1016/j.lanwpc.2021.100276
- Lopez Bernal J, Andrews N, Gower C, et al. Effectiveness of Covid-19 vaccines against the B.1.617.2 (delta) variant. N Engl J Med [Internet]. 2021;385:585–594.
- Pouwels KB, Pritchard E, Matthews PC, et al. Impact of Delta on viral burden and vaccine effectiveness against new SARS-CoV-2 infections in the UK. medRxiv [Internet]. 2021:2021.08.18.21262237. Available from: http://medrxiv.org/content/early/2021/08/24/2021.08.18.21262237.abstract
- Liu J, Liu Y, Xia H, et al. BNT162b2-elicited neutralization of delta plus, lambda, and other variants. bioRxiv [Internet]. 2021:2021.09.13.460163. Available from: http://biorxiv.org/content/early/2021/09/14/2021.09.13.460163.abstract
- Levine-Tiefenbrun M, Yelin I, Alapi H, et al. Viral loads of delta-variant SARS-CoV-2 breakthrough infections after vaccination and booster with BNT162b2. Nat Med [Internet]. 2021;27:2108–2110.
- WHO. Classification of Omicron (B.1.1.529): SARS-CoV-2 variant of concern [Internet]. [cited 2021 Nov 30]. Available from: https://www.who.int/news/item/26-11-2021-classification-of-omicron-(b.1.1.529)-sars-cov-2-variant-of-concern.
- Basu D, Chavda VP, and Mehta AA. Therapeutics for COVID-19 and post COVID-19 complications: An update. Curr Res Pharmacol Drug Discov [Internet]. 2022;100086. Internet: https://www.sciencedirect.com/science/article/pii/S2590257122000062.
- Callaway E. Heavily mutated Omicron variant puts scientists on alert [Internet]. Nat News. 2021 [cited 2021 Nov 30];600:21. p. Update 27 November 2021. Available from: https://www.nature.com/articles/d41586-021-03552-w.
- Variant Technical Group (UK Health Security Agency). SARS-CoV-2 variants of concern and variants under investigation in England [Internet]. 2021. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1036501/Technical_Briefing_29_published_26_November_2021.pdf.
- Kumar S, Thambiraja TS, Karuppanan K, et al. Omicron and delta variant of SARS-CoV-2: a comparative computational study of spike protein. bioRxiv [Internet]. 2021;2021.12.02.470946. Available from: http://biorxiv.org/content/early/2021/12/03/2021.12.02.470946.abstract
- Wang L, Berger NA, Kaelber DC, et al. Comparison of outcomes from COVID infection in pediatric and adult patients before and after the emergence of Omicron. medRxiv [Internet]. 2022:2021.12.30.21268495. Available from: http://medrxiv.org/content/early/2022/01/02/2021.12.30.21268495.abstract
- Flemming A. Omicron, the great escape artist. Nat Rev Immunol [Internet]. 2022;22:75.
- Zhao H, Lu L, Peng Z, et al. SARS-CoV-2 Omicron variant shows less efficient replication and fusion activity when compared with delta variant in TMPRSS2-expressed cells. Emerg Microbes Infect [Internet]. 2021:1–18. Available from: https://doi.org/https://doi.org/10.1080/22221751.2021.2023329
- Chavda VP, and Apostolopoulos V. Omicron Variant (B.1.1.529) of SARS-CoV-2: Threat for the elderly? Maturitas [Internet]. 2022; Internet: https://doi.org/10.1016/j.maturitas.2022.01.011.
- Chavda VP, Kapadia C, and Soni S, et al. A global picture: therapeutic perspectives for COVID-19. Immunotherapy [Internet]. 2022; Internet: https://doi.org/10.2217/imt-2021-0168
- Garcia-Beltran WF, St. Denis KJ, Hoelzemer A, et al. mRNA-based COVID-19 vaccine boosters induce neutralizing immunity against SARS-CoV-2 Omicron variant. Cell [Internet]. 2022;185:457–466.e4.