ABSTRACT
Introduction
In the first months of the novel coronavirus (COVID-19) pandemic that begun in 2020, non-pharmaceutical interventions (NPIs) have been adopted worldwide. However, the effects of NPI implementation go beyond slowing the spread of COVID-19. Here, we review the non-intended effects that may have arisen from prolonged application of NPIs.
Areas covered
NPIs also affected the epidemiology of other infectious diseases, with unprecedentedly low circulation of several respiratory and gastrointestinal viruses being observed worldwide in 2020. While this was a welcome effect for already strained health-care systems, prolonged low exposure to pathogens may result in an increased pool of individuals susceptible to certain diseases. Out-of-season or unusually intense outbreaks of non-vaccine preventable diseases have already been documented as NPIs were gradually eased. In the context of widespread and important disruptions in national vaccination programs during the early phase of the pandemic, the risk of vaccine-preventable disease resurgence after NPIs are lifted cannot be excluded either.
Expert opinion
Awareness must be raised of the risk of vaccine-preventable disease resurgence, and efforts need to be made to mitigate this risk, where possible, by increasing vaccination coverage. Research and regulatory opportunities brought on by the COVID-19 pandemic should be seized.
Plain Language Summary
In the first months of the COVID-19 pandemic, the only methods available to slow the spread of the disease were non-pharmaceutical interventions, such as lockdowns, mask wearing, social distancing, school closures, and travel bans. Even after vaccines against COVID-19 became available, combinations of non-pharmaceutical interventions continued to be implemented by most countries, to various extents. Although these measures lowered the number of people who got sick before vaccines and therapies against COVID-19 were available, they also had other consequences for public health. The non-pharmaceutical interventions implemented worldwide have slowed or even stopped the spread of several infectious diseases: since 2020, fewer cases of flu, bronchiolitis, gastroenteritis, and other diseases were recorded compared to pre-pandemic times. This relatively long 2-year period during which people, especially children, were exposed to fewer infections might mean that their immune systems are less prepared to fight these diseases. In addition, vaccination against diseases other than COVID-19 dropped in the early months of the pandemic, meaning that the number of children and adults who are not protected against vaccine-preventable disease has potentially increased. Easing of COVID-19 restrictions has caused a comeback of some diseases against which no vaccine is available, sometimes with more cases than during the pre-pandemic years; there is a risk that this might happen with vaccine-preventable diseases as well. To prevent outbreaks, routine and catch-up vaccinations against other diseases besides COVID-19 should be encouraged and promoted.
1. Introduction
On the 11 March 2020, the newly described and rapidly spreading coronavirus disease (COVID-19) was declared a pandemic [Citation1]. In an attempt to mitigate the spread of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), almost all countries adopted a range of measures in the first months of the pandemic. Since specific treatments or vaccines were not available at that time, governments applied heterogeneous strategies involving combinations of non-pharmaceutical interventions (NPIs) that included lockdowns, movement restrictions, mask mandates, and school closures [Citation2]. Even after vaccines and pharmaceutical treatments became available, NPIs remained in place at various levels of stringency [Citation3,Citation4], to ‘flatten the curve’ and avoid overloading the healthcare system, and to allow time for reaching community protection through vaccination.
NPIs were largely successful in slowing the spread of SARS-CoV-2 worldwide [Citation5,Citation6], saving an estimated three million lives across 11 European countries alone in the first two months of the pandemic [Citation7] and an estimated 40 million lives globally [Citation8]. However, the effects of NPIs go well beyond their role in curbing SARS-CoV-2 transmission. Lockdowns, movement restrictions, and school closures can also translate into delayed access to health care, affecting prevention and treatment of acute and chronic diseases, increased incidence of depression and mental disease [Citation9]. In addition, marked economic impacts have been observed; whether these are positive or negative depends greatly on the extent of pandemic disease transmission at the time that NPIs are put into place [Citation10].
On the other hand, since NPIs are not pathogen-specific, their use can also affect the spread of other infectious agents [Citation11]. This effect is most prominently illustrated by the shortened or even absent influenza season in 2020/2021, and a shift in the seasonal peak of respiratory syncytial virus (RSV) cases, which was delayed by the implementation of strict NPIs, but rebounded in 2021 after the stringency of these measures was lowered [Citation12]. This change in dynamics raises concerns that following an increase of the susceptible population for these diseases, large future outbreaks could occur after all restrictions are lifted, further increasing the burden on health-care systems [Citation13].
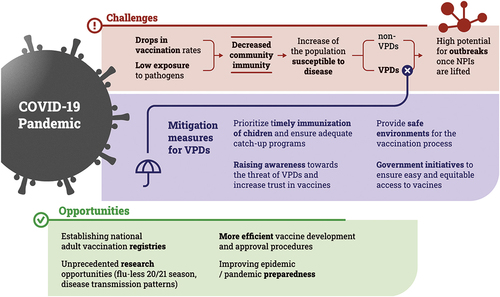
Here, we attempt to i) provide an overview of the effect NPIs adopted during the COVID-19 pandemic had on the epidemiology of other infectious diseases, both vaccine-preventable (VPD) and non-VPD and on the uptake of routine vaccines, ii) raise awareness of a potential rebound of infectious diseases after the lifting of NPIs, which could be minimized by focusing in a timely manner on other diseases besides COVID-19, and iii) identify opportunities provided by the COVID-19 pandemic for advancements in research and public health policies (). Opinions reflected in this manuscript are based on data from reliable sources (peer-reviewed publications, governmental websites or official documents issued by authorities). Data collection was started in December 2021, based on a core of publications and websites selected by the authors, which was expanded by adding additional relevant sources. These sources were identified by searching PubMed and the World Wide Web using combinations of various relevant keywords (including, but not limited to: ‘COVID-19 pandemic,’ ‘non-pharmaceutical interventions,’ ‘lockdown,’ ‘influenza,’ ‘respiratory syncytial virus,’ ‘RSV,’ ‘infectious diseases,’ ‘incidence,’ ‘decrease,’ ‘rebound,’ ‘outbreak’), and by reviewing the reference list of publications that were deemed relevant for the topic of the manuscript.
2. Challenges of the COVID-19 pandemic
2.1. Changing dynamics of VPDs and non-VPDs due to NPI implementation
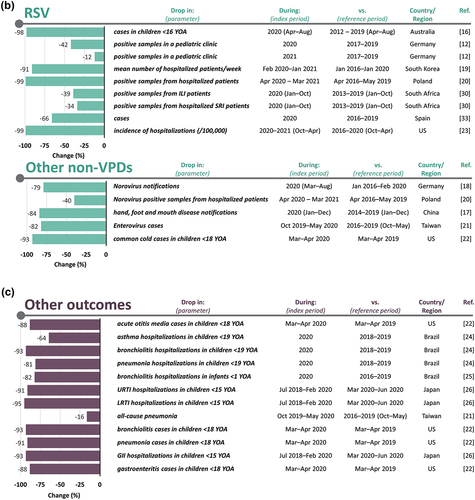
There is a considerable body of evidence indicating that implementation of NPIs to control the COVID-19 pandemic, including mask mandates, lockdowns, physical distancing, and overseas travel restrictions, have affected the spread of other infectious diseases [Citation14]. Worldwide, the burden of respiratory infections, such as influenza, RSV, pertussis, measles Neisseria meningitidis infections, and even common cold, has markedly decreased () [Citation11,Citation12,Citation15–29]. Dynamics of infectious diseases with a seasonal pattern, such as influenza and RSV, were affected differently. Influenza circulation decreased sharply after NPI implementation in countries from the Northern hemisphere, where the start of the COVID-19 pandemic coincided with the seasonal influenza peak, and influenza activity remained low throughout the 2020/2021 season [Citation12,Citation18,Citation20,Citation30]. In countries from the southern hemisphere, where NPI implementation preceded the influenza season, circulation of the virus was virtually absent, with the exception of an out-of-season outbreak in South Africa [Citation19,Citation31–33]. RSV circulation was also markedly impacted, with very low detection observed during the usual autumn-winter peaks in both hemispheres [Citation33–35]; however, in some countries, delayed RSV peaks were observed [Citation12,Citation36–39]. In addition to respiratory diseases, gastrointestinal or enteroviral diseases declined as well (), especially during the early phases of the pandemic, when NPIs were more stringent [Citation11,Citation17,Citation18,Citation20]. Although the decrease in disease burden was documented across all age groups, it does appear to be strongly driven by the reductions occurring in children [Citation17,Citation18]. There are studies suggesting that the impact of NPIs on disease transmission, albeit significant in most reports, could have been less marked in the case of non-enveloped viruses, such as rhinovirus, adenoviruses, and norovirus [Citation20,Citation40,Citation41], suggesting that these pathogens may have maintained a certain degree of circulation even during lockdowns.
Figure 2. Drops in burden caused by vaccine-preventable and non-vaccine preventable diseases due to the implementation of NPIs. a) VPDs; b) Non-VPDs; c) Etiology not determined.
It has been hypothesized that frequent stimulation of the innate immune system by viral infections can result in a functional reprogramming process that would enhance its effectiveness in the long term [Citation42], leading to what is called ‘trained’ immunity. This process is thought to be common in children during their first years of life but continues throughout the life-course as people are exposed to new pathogens or re-exposed to those they have encountered before. A reduction of exposure to infectious agents resulting from the NPIs imposed by the pandemic may have led to a less potent trained immunity in children; this drop in heterologous protection against infections might result in greater overall susceptibility to infections in the future [Citation43].
Lack of exposure to microbial agents may also lead to a decrease in the pathogen-specific natural protection of the population, even in adults, especially when non-VPDs are concerned. For example, partial and transient immunity to RSV, an infectious disease against which no vaccine is available, is spontaneously achieved each year by infection or, in the case of new-borns, transplacental transfer of maternal antibodies [Citation43]. With an absent or low level of RSV transmission over a prolonged period, the achievement of this transient immunity would be suboptimal, thus increasing the proportion of susceptible individuals in a population; this may translate into higher infection rates affecting even older age groups when RSV circulation is resumed [Citation36,Citation44]. This mechanism is also valid for VPDs with relatively low vaccination rates, such as influenza: prolonged lack of exposure to the pathogen contributes to a decreased community immunity of the population [Citation45].
2.2. Effects of decreased community immunity
In the context of the already strained health-care systems, reductions in the incidence of other infectious diseases represent a welcome byproduct of the NPIs employed to reduce the spread of COVID-19. However, some of the diseases that were impacted by the introduction of stringent NPIs rebounded after the restrictions were lifted or eased, sometimes reaching incidence rates higher than those documented during the pre-pandemic years. Such a dynamic has already been described for RSV [Citation20,Citation36,Citation46], norovirus [Citation47] and rhinovirus infections [Citation12,Citation18,Citation19,Citation34,Citation41], or hand, foot, and mouth disease [Citation11], and is expected to continue into 2022 as well [Citation13,Citation48].
Based on the data currently available, rebounds or outbreaks that appeared after NPIs were eased were first observed in children [Citation18,Citation20,Citation34,Citation36,Citation47] and were all caused by non-VPDs; however, future outbreaks of VPDs could also occur when NPIs are completely lifted, and social dynamics return to normal. Unusual outbreaks, such as the recent cases of severe acute hepatitis of unknown etiology, might also be related to increased pathogen circulation against a background of decreased community immunity [Citation49], although the evidence for such an assumption is still lacking. These outbreaks also highlight the scientific community’s current limitations in understanding the circulation of pathogens and community immunity.
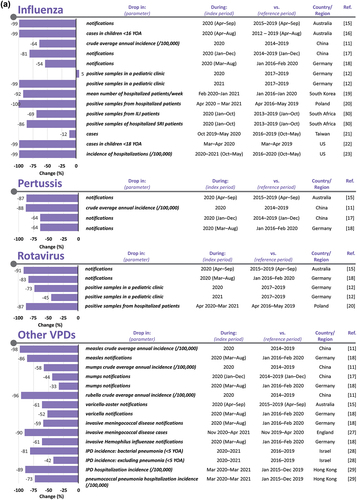
2.3. Disruptions of national vaccination programs
In the early days of the COVID-19 pandemic, the World Health Organization (WHO) recommended continuing to prioritize immunizations where feasible, adapting immunization strategies when needed, but to temporarily suspend mass vaccination programs [Citation50]. Despite this recommendation, national vaccination programs in more than 60 countries were significantly impacted in 2020, due to loss of funding, vaccine shortages, lack of medical personnel and concerns of the public regarding the possibility of contracting COVID-19 at vaccination clinics or doctor’s offices [Citation51,Citation52]. This problem has affected developed and developing countries alike, albeit to somewhat different extents [Citation53–63], as illustrated in . As a consequence, the number of children under the age of one year at risk of diphtheria, measles, and poliomyelitis was estimated to be over 80 million; vaccination programs against poliomyelitis and measles were the most severely affected [Citation64]. The impact of missed vaccinations is likely to be the highest when primary vaccinations are concerned, or in vaccines with a limited window of administration, such as the rotavirus vaccine or maternal pertussis vaccinations. Although gaps in vaccine coverage tended to reduce in the second part of 2020, a WHO-conducted survey assessing the continuity of essential health services during the COVID-19 pandemic reported that more than one-third of 112 countries included in the survey (37%) still struggled with some degree of disruption in their immunization services [Citation65]. Despite the rebound in vaccination rates seen in certain parts of the world, this vaccination gap has not been fully closed in 2021 [Citation66,Citation67].
Figure 3. Drops in vaccination during the early phases of the COVID-19 pandemic.
Declines in routine vaccination rates have led to an increase of the population susceptible to VPDs, placing the global community at increased risk of outbreaks, as previously documented for rotavirus gastroenteritis [Citation68] and measles [Citation69]. In children, diseases such as poliomyelitis, pertussis, and measles are associated with a much higher morbidity and mortality than COVID-19, especially in the developing world [Citation51]; it was estimated that in Africa, for each excess COVID-19 death attributable to SARS-CoV-2 infection acquired during a vaccination clinic visit, up to 84 vaccine-preventable deaths could be averted [Citation70].
Effects of the COVID-19 pandemic on influenza vaccination campaigns differed across countries. While in Ireland, Italy, and the United Kingdom (UK), influenza vaccine acceptance and uptake increased for the 2020/2021 season [Citation71–73], Australia witnessed a significant decline in flu vaccinations for adults over 65 years of age at the start of the 2021 season compared with the previous year, although similar levels were eventually reached following public awareness efforts [Citation74]. There is a possibility that based on the unprecedentedly low number of influenza cases recorded over the last two seasons, the risk of contracting influenza might be perceived as minimal by the public; whether and to what extent this will affect influenza vaccine coverage for the next flu season remains to be seen.
Data reflecting the effect of the COVID-19 pandemic on the uptake of maternal pertussis vaccination, although scarce, suggests a drop in vaccination coverage. In a low-income population of pregnant women from the United States, uptake of the tetanus-diphtheria-acellular pertussis (Tdap) vaccine during the pandemic was 11 percentage points lower compared to pre-pandemic values [Citation63]. In England, maternal pertussis vaccination coverage was around seven percentage points lower in the last trimester of 2021 than in the corresponding pre-pandemic period in 2019, which represents a further drop of about three percentage points compared to 2020 [Citation75]. However, these numbers might have been influenced by underreporting [Citation75]; a survey revealed that in general, pregnant women in the UK considered that the COVID-19 pandemic increased awareness regarding the importance of maternal vaccination [Citation76].
2.4. Potential implications on VPDs
In the context of decreased community immunity, coupled with the disruption of vaccination programs, similar trends of rebound as those seen for non-VPDs might be expected for VPDs as well.
Before the 2021–2022 influenza season in the Northern hemisphere, concerns were expressed over its potentially increased severity following the previous season of low influenza circulation [Citation77]. However, the 2021–2022 influenza season proved to also be mild; although the number of cases were higher compared to the 2020–2021 season, they remained below pre-pandemic levels [Citation78,Citation79]. Other particularities of the 2021–2022 influenza season included a prolonged duration and delayed peak, and the continued absence of B/Yamagata lineage [Citation78–81]. Whether these particularities will persist, as well as their potential influence on the severity of upcoming seasons, is still unclear.
Global eradication efforts of VPDs have been hampered by the disruption in vaccination programs seen during the COVID-19 pandemic. The resulting increase of susceptible populations could result in outbreaks of VPDs, such as poliomyelitis and measles. However, this scenario is more likely for measles due to its increased transmissibility, higher vaccination coverage needed to reach community immunity, and ongoing transmission in several parts of the world [Citation82]. Against the background of disruptions in vaccination caused by the COVID-19 pandemic, measles cases in 2022 have been rising worldwide [Citation83], presumably accelerated by the lifting of restrictions and resuming of international travel [Citation82].
Poliomyelitis is still considered endemic in two countries, Afghanistan and Pakistan [Citation84]; from there, wild poliovirus can be carried over long distances by travelers and introduced into vulnerable populations, as proven by the recent poliomyelitis outbreaks in Malawi and Mozambique [Citation85,Citation86]. While the potential for outbreaks in Europe and Northern America is lower, due to the still relatively high vaccination coverage, findings suggesting possible community transmission of vaccine-derived poliovirus were recently observed in London, UK [Citation87]. Although no cases of paralysis have been reported until now [Citation87], this finding may suggest that vaccine coverage has dropped below the threshold needed to achieve community immunity.
A rising trend could also be expected for diseases with exclusively human reservoirs, such as pertussis. Once movement restrictions and social distancing are no longer in place, adolescents, adults, and older school-age children, who represent important reservoirs for Bordetella pertussis [Citation88], could be the source of infection for infants with decreased immunity to the pathogen due to missed maternal or childhood vaccinations.
Lower circulation of certain respiratory viruses like RSV and influenza can have implications that go beyond a drop in the number of disease cases caused by these viruses, affecting the incidence of infectious diseases caused by other pathogens. Following the introduction of NPIs, an overall decrease in invasive pneumococcal disease (IPD), including pneumococcal pneumonia, was a common finding in several countries [Citation89]. This was presumed to be the result of the breaks in transmission chains caused by NPIs; however, a study conducted in children under 5 years of age in Israel revealed that changes in pneumococcal carriage rates compared to the pre-pandemic period were minimal, and the substantial decrease in IPD cases was instead associated with the absence of certain respiratory viruses acting as co-pathogens [Citation28]. Based on this observation, an increase in IPD cases, including pneumococcal pneumonia, could occur once the circulation of respiratory viruses intensifies again [Citation90]. Whether this is also true for older adults is not yet confirmed; regardless, return of social mixing to normal levels might result in increased number of IPD cases in this age group.
3. Conclusions
In the early days of the COVID-19 pandemic, implementation of NPIs was the only available method to delay the spread of SARS-CoV-2, one that also affected the epidemiology of other infectious diseases in the process and decreased the pressure on already strained health-care systems. However, there are also potential side effects of this fortunate byproduct of NPIs; among others, it translates into lack of natural exposure to pathogens and a subsequent increase of susceptible individuals, as confirmed by the resurgence of several non-VPDs once restrictions were eased. While not documented so far, a similar scenario for VPDs cannot be excluded, considering that the disruption of vaccination programs during the COVID-19 pandemic is likely to have caused a decrease in community immunity. To avoid an imminent resurgence of VPDs after NPIs introduced during the COVID-19 pandemic are lifted completely, awareness of these other diseases besides COVID-19 must be maintained among physicians and the general public alike.
4. Expert opinion
4.1. How can the potential rebound of VPDs be minimized?
A high proportion of individuals susceptible to disease, regardless of whether it results from a lack of naturally acquired or vaccine-induced immunity, could translate into increased risk of future outbreaks once all NPIs are lifted [Citation43]. In case of VPDs, this risk can be partially mitigated by vaccinations. In the face of an increasing threat of VPDs as NPIs against the COVID-19 pandemic are being lifted, all efforts should be made to maximize the number of individuals protected by vaccines, including catch-up programs to vaccinate those who have missed previously scheduled vaccinations. Catch-up vaccination strategies should be adapted to specific populations, while keeping disease- and vaccine-specific particularities in mind; in some cases, the window of opportunity for catch-up vaccination is very narrow (e.g. with maternal immunization or rotavirus vaccination in infants). Health-care providers might be hesitant about administering catch-up vaccinations (i.e. vaccinations outside the well-established routine vaccination schedules) in the absence of clear guidance. To address this potential barrier, national health authorities and relevant professional societies could issue guidelines on how to perform catch-up vaccinations, and the existing ones [Citation91–93] should be popularized among the medical personnel involved in immunizations. In case of limited resources, prioritization of catch-up vaccination might be warranted, starting with the diseases that pose the greatest risk (e.g. measles).
To stimulate vaccination programs to return to or even go above their pre-pandemic levels, barriers to successful immunization programs need to be identified, and comprehensive actions that involve multiple stakeholders of the immunization process need to be taken to overcome them [Citation94]. This topic has understandably sparked a great interest recently, with several comprehensive publications providing overviews and suggestions for successful interventions [Citation53,Citation94,Citation95].
The COVID-19 pandemic resulted in impaired access to medical care, including diagnosis, treatment, and immunization. When infectious diseases are concerned, the negative effects of the first two are already demonstrated by the worrying increase of deaths due to tuberculosis and the reversal of years of progress in the fight against this disease [Citation96]. The risks deriving from impaired access to immunization might be just starting to materialize in the form of VPD outbreaks. Ensuring that the population has safe and easy access to medical care is an essential step toward the goal of increasing vaccine coverage; raising awareness of the risk that VPDs still represent is at least as important [Citation95], especially in the current context of decreased community immunity and the likely increase in risk once the protective NPIs are completely lifted. Vaccine hesitancy was cited in 2019 by the WHO as one of the top 10 global health threats [Citation97], and this has likely not changed during the COVID-19 pandemic. On the other hand, vaccine acceptance was demonstrated to be higher if a trusted health-care provider recommended immunization [Citation98,Citation99]; this was also true for maternal immunizations [Citation100,Citation101]. Focusing on high-risk populations and groups identified as having higher vaccine hesitancy is warranted.
But how can health-care providers and members of the general public be made aware of the risk VPD resurgence represents, and that optimal vaccination coverage is needed to mitigate this risk? A relatable analogy for immunity with how we physically train our body for strength and endurance could help reach that goal [Citation102]. Adequate exposure to pathogenic stimuli (either via natural infection or vaccination) is the equivalent of daily training to our immune systems; during the COVID-19 pandemic, the scarcity of those stimuli likely caused missed opportunities for our immune systems to keep full readiness for future interactions with pathogens. But the seemingly inevitable resurgence of some non-VPDs and, more worryingly, possible VPD outbreaks should not find us unprepared. Vaccination can provide the necessary training for our immune systems so that we are ready to return to our normal lives as safely as possible.
4.2. What are the opportunities for advancement of vaccines and vaccination?
The unprecedented challenges faced by the global community during the COVID-19 pandemic have come with a few opportunities that are worth exploring.
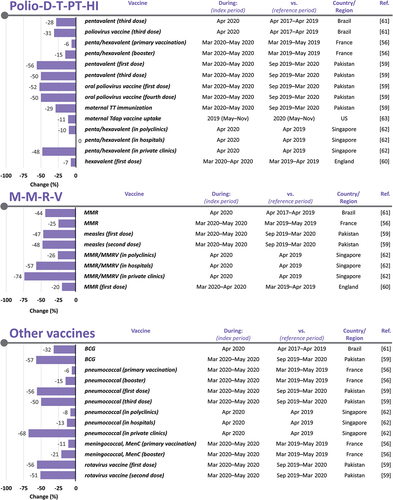
The virtually absent 2020/2021 influenza season provides unique opportunities for large-scale studies of long-term immunity to influenza, both naturally acquired, and vaccine-induced. Studies on the transmission patterns of RSV and influenza after such a prolonged period of transmission bottleneck can reveal valuable details on how these infections spread in a community [Citation38]. Limited data is available on whether different non-VPDs and VPDs will (or will not) rebound after the easing or lifting of NPIs [Citation27,Citation103–109]; we can only speculate on how the characteristics of the infectious agent, transmission patterns within the community and country-specific particularities of NPI implementation/lifting will influence such a rebound () [Citation110]. The reason why rebounds were seen for some infectious diseases, but not for others remains unclear; the degree of environmental stability or transmission route alone do not appear to constitute plausible explanations [Citation34]. It could be hypothesized that highly contagious diseases might rebound more quickly, as they spread with more ease through the pool of susceptible individuals. This would be consistent with why RSV, norovirus, rhinovirus or hand, foot and mouth disease, with basic reproductive number (R0) values of around 4.5 [Citation111], 2 [Citation112], 1.5–2.7 [Citation111] and 2.5–5.5 [Citation113], respectively, have reappeared faster compared to influenza, which has an R0 value of around 1.3 [Citation114]. Highly contagious VPDs such as measles or pertussis might make a similar comeback, as indicated by recent data on measles outbreaks [Citation83]. Such outbreaks can be used as early warning signs of suboptimal vaccine coverage. Continued surveillance of infectious diseases, including genomic surveillance, is of upmost importance for timely detection of outbreaks and their mitigation.
Table 1. Evolution of different infectious diseases during the COVID-19 pandemic.
The COVID-19 pandemic has reinforced the importance of vaccination for infectious disease control and the knowledge gained from the fast pace at which COVID-19 vaccines were created and approved could be used to streamline vaccine development and approval processes for other VPDs as well. The clinical development process of COVID-19 vaccines has provided learning opportunities on a wide array of subjects, from the ethical perspectives of conducting clinical trials [Citation115] to collaboration between academia, industry and regulatory authorities [Citation116].
Lessons learned from the large-scale COVID-19 vaccination campaigns conducted in adults include the need to establish adult vaccination registries, an important pre-requisite for increasing the uptake of primary and booster vaccines recommended to adults [Citation95]. The collective experience gained in scaling up vaccine manufacturing capacity, establishing and maintaining global vaccine supply chains, or setting up and operating mass vaccination centers should be used to improve and advance preparedness toward future outbreaks, epidemics, or pandemics.
The large-scale deployment of messenger ribonucleic acid (mRNA) vaccines against COVID-19 has been one of the most prominent scientific breakthroughs brought on by the pandemic. Despite the enthusiasm that followed the first-time approval in humans of a vaccine developed using mRNA technology, expectations on how this will shape the future of vaccine development process must be kept reasonable. While mRNA vaccines do have some advantages over vaccines developed using other platforms, such as rapidity of adaptation to mutations of the target pathogen or rapid and scalable production [Citation117], the unprecedentedly fast development and approval process of mRNA COVID-19 vaccines might not be easily replicated for other vaccines in the near future. Scientists have started working on the mRNA platform well before the COVID-19 pandemic, and knowledge accumulated over time enabled them to develop mRNA COVID-19 vaccines in record time. The pandemic context, which translated into an urgent need for effective and safe vaccines and practically unlimited funding allocated for finding such a vaccine, has also a great contribution. Although we will see more mRNA vaccines in the future, it is unlikely that they will replace well-established vaccines based on other platforms. Challenges that persist include optimizing vaccine uptake (by developing effective and trust-building communication with the public on topics concerning vaccination and finding ways to successfully combat misinformation), and ensuring equitable access to new and existing vaccines, as set forth by the WHO’s Global Immunization Agenda 2030 [Citation118].
In the 200 years that have passed since the discovery of the first vaccine, immunization has come a long way; the benefits of vaccination in preventing morbidity and mortality have been repeatedly proven by the successful eradication of smallpox and substantial decreases in the burden of other infectious diseases worldwide. However, for this progress to be sustained, and to avoid an imminent resurgence of VPDs after all NPIs introduced during the COVID-19 pandemic are eliminated, awareness of other diseases besides COVID-19 must be maintained. Learnings from the COVID-19 pandemic could provide unprecedented opportunities for vaccination, from research and development to implementation. Properly seized, these opportunities could help us closer to milestones, such as eradication of poliomyelitis or discovery of new vaccines against yet unconquered infectious diseases.
Article highlights
Non-pharmaceutical interventions (NPIs) such as lockdowns, movement restrictions, mask mandates and school closures, adopted during the COVID-19 pandemic, also led to unusually low burdens of both vaccine-preventable and non-vaccine preventable (VPDs and non-VPDs) infectious diseases, including influenza, respiratory syncytial virus (RSV), pertussis, measles, rotavirus, and norovirus
While this effect of NPIs was beneficial for already strained health-care systems, it also translated into reduced opportunities for natural boosting of immunity against those pathogens, potentially leading to an increased pool of individuals susceptible to diseases
In addition, transient disruptions of varying magnitude in vaccination programs have been documented in several countries, which could further contribute to the decreased community immunity elicited by prolonged low exposure to pathogens
Activity of influenza and other VPDs continues to be low at the beginning of the third pandemic year, while for non-VPDs, such as RSV and norovirus, out-of-season outbreaks of high intensity have been documented following easing of NPIs, suggesting that infectious diseases might resurge once restrictions are lifted
VPD outbreaks could be prevented by increasing vaccination coverage, unless awareness of health-care providers and the general public regarding the risk of infectious diseases is lowered following long periods of low disease burden in the pandemic era
The COVID-19 pandemic has also brought on several opportunities that should be seized; these include the possibility to establish adult vaccination registries, to conduct research on long-term immunity against influenza, to streamline the vaccine development and regulatory approval processes, and to perfect strategies of epidemic/pandemic preparedness for the future
Author contribution
All authors contributed to the interpretation of the data and a critical review of the paper for important intellectual content. All authors are in agreement with the content of the final article and have approved it for submission and publication.
Declaration of interest
KB Oh, TM Doherty and V Vetter are employees of the GSK group of companies and hold shares in the GSK group of companies as part of their employee remuneration and they have no non-financial competing interest to declare. P Bonnani declares payment and support from the GSK group of companies, MSD, Pfizer, Seqirus, Astra Zeneca, Janssen, and Sanofi Pasteur. Authors declare no other relevant financial and non-financial conflict of interest that the ones disclosed above.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Acknowledgments
Authors thank Modis for editorial assistance, manuscript coordination, and design support on behalf of GSK. Timea Kiss provided medical writing support, Gil Costa provided design support, and Emilie Mak Fan coordinated manuscript development.
Additional information
Funding
References
- World Health Organization [Internet]. WHO; c2022. Timeline: WHO’s COVID-19 response; 2020 [updated 28 Mar 2022; cited 13 Dec]; [ about 2 screens]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline?gclid=CjwKCAjwkdL6BRAREiwA-kiczOSDJ1iAFGB74uYaWtY33SRgkrzMfOaE5JrFZXlCOF58SVAW_QdT7xoCzlkQAvD_BwE#event-71
- Shen Y, Powell G, Ganser I, et al. Monitoring non-pharmaceutical public health interventions during the COVID-19 pandemic. Sci Data. 2021;8(1):225.
- Hale T, Angrist N, Goldszmidt R, et al. A global panel database of pandemic policies (Oxford COVID-19 government response tracker). Nat Hum Behav. 2021;5(4):529–538.
- Our World in Data [Internet]. OurWorldInData.org. Covid-19 Stringency Index; 2021 [cited 2021 Dec 10]; [ about 1screen]. Available from: https://ourworldindata.org/grapher/covid-stringency-index?tab=chart
- Askitas N, Tatsiramos K, Verheyden B. Estimating worldwide effects of non-pharmaceutical interventions on COVID-19 incidence and population mobility patterns using a multiple-event study. Sci Rep. 2021;11(1):1972.
- Mendez-Brito A, El Bcheraoui C, Pozo-Martin F. Systematic review of empirical studies comparing the effectiveness of non-pharmaceutical interventions against COVID-19. J Infect. 2021;83(3):281–293.
- Flaxman S, Mishra S, Gandy A, et al. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. 2020;584(7820):257–261.
- Walker P, Whittaker C, Watson O, et al. Report 12: the global impact of COVID-19 and strategies for mitigation and suppression. Imperial College London; 2020. 2020 Mar 26.
- Müller O, Razum O, Jahn A, Effects of non-pharmaceutical interventions against COVID-19 on the incidence of other diseases. Lancet Reg Health Eur. 2021;6:100139.
- International Monetary Fund. Chapter 2: dissecting the economic effects. In: World economic outlook, October 2020: a long and difficult ascent. Washington (DC): International Monetary Fund; 2020. p. 65–84.
- Geng M-J, Zhang H-Y, L-J Y, et al., Changes in notifiable infectious disease incidence in China during the COVID-19 pandemic. Nat Commun. 2021;12(1):6923.
- Maison N, Peck A, Illi S, et al., The rising of old foes: impact of lockdown periods on “non-SARS-CoV-2” viral respiratory and gastrointestinal infections. Infection. 2022;50(2):519–524.
- Baker RE, Park SW, Yang W, et al. The impact of COVID-19 nonpharmaceutical interventions on the future dynamics of endemic infections. Proc Natl Acad Sci U S A. 2020;117(48):30547–30553.
- Cohen R, Pettoello-Mantovani M, Somekh E, et al. European pediatric societies call for an implementation of regular vaccination programs to contrast the immune debt associated to COVID-19 pandemic in children. J Pediatr. 2022;242:260–261.e3.
- Adegbija O, Walker J, Smoll N, et al. Notifiable diseases after implementation of COVID-19 public health prevention measures in Central Queensland, Australia. Commun Dis Intell (2018). 2021;45.
- Yeoh DK, Foley DA, Minney-Smith CA, et al. Impact of coronavirus disease 2019 public health measures on detections of influenza and respiratory syncytial virus in children during the 2020 Australian winter. Clin Infect Dis. 2021;72(12):2199–2202.
- Xiao J, Dai J, Hu J, et al. Co-benefits of nonpharmaceutical intervention against COVID-19 on infectious diseases in China: a large population-based observational study. Lancet Reg Health West Pac. 2021;17:100282.
- Ullrich A, Schranz M, Rexroth U, et al. Impact of the COVID-19 pandemic and associated non-pharmaceutical interventions on other notifiable infectious diseases in Germany: an analysis of national surveillance data during week 1-2016 - week 32-2020. Lancet Reg Health Eur. 2021;6:100103.
- Kim JH, Roh YH, Ahn JG, et al. Respiratory syncytial virus and influenza epidemics disappearance in Korea during the 2020-2021 season of COVID-19. Int J Infect Dis. 2021;110:29–35.
- Grochowska M, Ambrożej D, Wachnik A, et al., The impact of the COVID-19 pandemic lockdown on pediatric infections-a single-center retrospective study. Microorganisms. 2022;10(1):178.
- Chiu NC, Chi H, Tai YL, et al. Impact of wearing masks, hand hygiene, and social distancing on influenza, enterovirus, and all-cause pneumonia during the coronavirus pandemic: retrospective national epidemiological surveillance study. J Med Internet Res. 2020;22(8):e21257.
- Hatoun J, Correa ET, Donahue SMA, et al. Social distancing for COVID-19 and diagnoses of other infectious diseases in children. Pediatrics. 2020;146(4):e2020006460.
- Olsen SJ, Winn AK, Budd AP, et al. Changes in influenza and other respiratory virus activity during the COVID-19 pandemic-United States, 2020-2021. Am J Transplant. 2021;21(10):3481–3486.
- Chiapinotto S, Sarria EE, Mocelin HT, et al. Impact of non-pharmacological initiatives for COVID-19 on hospital admissions due to pediatric acute respiratory illnesses. Paediatr Respir Rev. 2021;39:3–8.
- Friedrich F, Ongaratto R, Scotta MC, et al. Early impact of social distancing in response to coronavirus disease 2019 on hospitalizations for acute bronchiolitis in infants in Brazil. Clin Infect Dis. 2021;72(12):2071–2075.
- Kishimoto K, Bun S, Shin JH, et al. Early impact of school closure and social distancing for COVID-19 on the number of inpatients with childhood non-COVID-19 acute infections in Japan. Eur J Pediatr. 2021;180(9):2871–2878.
- UK Health Security Agency. Invasive meningococcal disease in England: annual laboratory confirmed reports for epidemiological year 2020 to 2021. UK Health Security Agency; 2022. ( Health Protection Report; Volume 16 Number 1).
- Danino D, Ben-Shimol S, van der Beek BA, et al. Decline in pneumococcal disease in young children during the coronavirus disease 2019 (COVID-19) pandemic in Israel associated with suppression of seasonal respiratory viruses, despite persistent pneumococcal carriage: a prospective cohort study. Clin Infect Dis. 2021;30. DOI:10.1093/cid/ciab1014.
- Chan KF, Ma TF, Ip MS, et al. Invasive pneumococcal disease, pneumococcal pneumonia and all-cause pneumonia in Hong Kong during the COVID-19 pandemic compared with the preceding 5 years: a retrospective observational study. BMJ Open. 2021;11(10):e055575.
- Chan CP, Wong NS, Leung CC, et al. Positive impact of measures against COVID-19 on reducing influenza in the Northern Hemisphere. J Travel Med. 2020;27(8):taaa087.
- Olsen SJ, Azziz-Baumgartner E, Budd AP, et al. Decreased influenza activity during the COVID-19 pandemic - United States, Australia, Chile, and South Africa, 2020. MMWR. 2020;69(37):1305–1309.
- Tempia S, Walaza S, Bhiman JN, et al. Decline of influenza and respiratory syncytial virus detection in facility-based surveillance during the COVID-19 pandemic, South Africa, January to October 2020. Euro Surveill. 2021;26(29):2001600.
- Varela FH, Scotta MC, Polese-Bonatto M, et al. Absence of detection of RSV and influenza during the COVID-19 pandemic in a Brazilian cohort: likely role of lower transmission in the community. J Glob Health. 2021;11:05007.
- Oh DY, Buda S, Biere B, et al. Trends in respiratory virus circulation following COVID-19-targeted nonpharmaceutical interventions in Germany, January - September 2020: analysis of national surveillance data. Lancet Reg Health Eur. 2021;6:100112.
- Torres-Fernandez D, Casellas A, Mellado MJ, et al. Acute bronchiolitis and respiratory syncytial virus seasonal transmission during the COVID-19 pandemic in Spain: a national perspective from the pediatric Spanish Society (AEP). J Clin Virol. 2021;145:105027.
- Foley DA, Yeoh DK, Minney-Smith CA, et al. The interseasonal resurgence of respiratory syncytial virus in Australian children following the reduction of coronavirus disease 2019-related public health measures. Clin Infect Dis. 2021;73(9):e2829–e2830.
- Delestrain C, Danis K, Hau I, et al. Impact of COVID-19 social distancing on viral infection in France: a delayed outbreak of RSV. Pediatr Pulmonol. 2021;56(12):3669–3673.
- Williams TC, Sinha I, Barr IG, et al. Transmission of paediatric respiratory syncytial virus and influenza in the wake of the COVID-19 pandemic. Euro Surveill. 2021;26(29):2100186.
- Centers for Disease Control and Prevention [Internet]. Atlanta (GA): Centers for Disease Control and Prevention. Increased interseasonal respiratory syncytial virus (RSV) activity in parts of the southern United States; 2021 [cited 14 Dec 2021]; [about 5 screens]. Available from: https://emergency.cdc.gov/han/2021/han00443.asp
- Giraud-Gatineau A, Kaba L, Boschi C, et al. Control of common viral epidemics but not of SARS-CoV-2 through the application of hygiene and distancing measures. J Clin Virol. 2022;150-151:105163.
- Rodgers L, Sheppard M, Smith A, et al. Changes in seasonal respiratory illnesses in the United States during the coronavirus disease 2019 (COVID-19) pandemic. Clin Infect Dis. 2021;73(Suppl 1):S110–S117.
- Netea MG, Giamarellos-Bourboulis EJ, Domínguez-Andrés J, et al. Trained immunity: a tool for reducing susceptibility to and the severity of SARS-CoV-2 infection. Cell. 2020;181(5):969–977.
- Cohen R, Ashman M, Taha MK, et al. Pediatric Infectious Disease Group (GPIP) position paper on the immune debt of the COVID-19 pandemic in childhood, how can we fill the immunity gap? Infect Dis Now. 2021;51(5):418–423.
- Fourgeaud J, Toubiana J, Chappuy H, et al. Impact of public health measures on the post-COVID-19 respiratory syncytial virus epidemics in France. Eur J Clin Microbiol Infect Dis. 2021;40(11):2389–2395.
- Together Against Flu [Internet]. IFPMA; c2022. What are the main issues concerning the next flu season?; 2021 [cited 15 Dec 2021]; [about 6 screens]. Available from: https://togetheragainstflu.com/news/interview-richard-webby
- Ujiie M, Tsuzuki S, Nakamoto T, et al. Resurgence of respiratory syncytial virus infections during COVID-19 pandemic, Tokyo, Japan. Emerg Infect Dis. 2021;27(11):2969–2970.
- Yasmin F, Ali SH, Ullah I. Norovirus outbreak amid COVID-19 in the United Kingdom; priorities for achieving control. J Med Virol. 2021;94(3):1232–1235.
- O’Reilly KM, Sandman F, Allen D, et al. Predicted norovirus resurgence in 2021-2022 due to the relaxation of nonpharmaceutical interventions associated with COVID-19 restrictions in England: a mathematical modelling study. BMC Med. 2021;19(1):299.
- World Health Organization [Internet]. WHO; c2022. Severe acute hepatitis of unknown aetiology in children - Multi-country; 2022 [cited 2022 Jul 11]; [ about 18 screens]. Available from: https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON394
- World Health Organization. Guiding principles for immunization activities during the COVID-19 pandemic. WHO; 2020. (Interim guidance; 2020 Mar 26).
- Feldman AG, O’Leary ST, Danziger-Isakov L. The risk of resurgence in vaccine-preventable infections due to coronavirus disease 2019-related gaps in immunization. Clin Infect Dis. 2021;73(10):1920–1923.
- Bonanni P, Angelillo IF, Villani A, et al. Maintain and increase vaccination coverage in children, adolescents, adults and elderly people: let’s avoid adding epidemics to the pandemic: appeal from the board of the vaccination calendar for life in Italy: maintain and increase coverage also by re-organizing vaccination services and reassuring the population. Vaccine. 2021;39(8):1187–1189.
- Dembiński Ł, Huss G, Radziewicz-Winnicki I, et al. EAP and ECPCP statement risks for children’s health during the COVID-19 pandemic and a call for maintenance of essential pediatric services. Front Pediatr. 2021;9:679803.
- Wong YJ, Lee SWH. COVID-19: a call for awareness or mandatory vaccination even in pandemics? J Glob Health. 2021;11:03005.
- Santos VS, Vieira SCF, Barreto IDC, et al. Effects of the COVID-19 pandemic on routine pediatric vaccination in Brazil. Expert Rev Vaccines. 2021;20(12):1661–1666.
- Taine M, Offredo L, Drouin J, et al. Mandatory infant vaccinations in France during the COVID-19 pandemic in 2020. Front Pediatr. 2021;9:666848.
- Din M, Ali H, Khan M, et al. Impact of COVID-19 on polio vaccination in Pakistan: a concise overview. Rev Med Virol. 2021;31(4):e2190.
- Saitoh A, Okabe N. Changes and remaining challenges for the Japanese immunization program: closing the vaccine gap. Vaccine. 2021;39(22):3018–3024.
- Chandir S, Siddiqi DA, Mehmood M, et al. Impact of COVID-19 pandemic response on uptake of routine immunizations in Sindh, Pakistan: an analysis of provincial electronic immunization registry data. Vaccine. 2020;38(45):7146–7155.
- McDonald HI, Tessier E, White JM, et al. Early impact of the coronavirus disease (COVID-19) pandemic and physical distancing measures on routine childhood vaccinations in England, January to April 2020. Eurosurveillance. 2020;25(19):2000848.
- Silveira MF, Tonial CT, Goretti KMA, et al. Missed childhood immunizations during the COVID-19 pandemic in Brazil: analyses of routine statistics and of a national household survey. Vaccine. 2021;39(25):3404–3409.
- Zhong Y, Clapham HE, Aishworiya R, et al. Childhood vaccinations: hidden impact of COVID-19 on children in Singapore. Vaccine. 2021;39(5):780–785.
- Cotter SB, Taylor LL, Grace R, et al. Effects of the COVID-19 pandemic on routine maternal vaccine uptake <Q176/>. Obstetrics Gynecol. 2022;139(139):51S.
- World Health Organization [Internet]. WHO; c2022. At least 80 million children under one at risk of diseases such as diphtheria, measles and polio as COVID-19 disrupts routine vaccination efforts, warn Gavi, WHO and UNICEF; 2020 [cited 13 Dec 2021]; [about 9 screns]. Available from: https://www.who.int/news/item/22-05-2020-at-least-80-million-children-under-one-at-risk-of-diseases-such-as-diphtheria-measles-and-polio-as-covid-19-disrupts-routine-vaccination-efforts-warn-gavi-who-and-unicef
- World Health Organization. Pulse survey on continuity of essential health services during the COVID-19 pandemic. WHO; 2021. ( Quarter 1 2021).
- Skolnik A, Bhatti A, Larson A, et al. Silent consequences of COVID-19: why it’s critical to recover routine vaccination rates through equitable vaccine policies and practices. Ann Fam Med. 2021;19(6):527–531.
- GAVI. 2022. Routine immunisation worldwide holds firm despite the pandemic; 2021 [cited 8 Apr 2022]; [ about 8 screens]. Available from: https://www.gavi.org/vaccineswork/routine-immunisation-worldwide-holds-firm-despite-pandemic
- Martinón-Torres F, Aramburo A, Martinón-Torres N, et al. A reverse evidence of rotavirus vaccines impact. Hum Vaccin Immunother. 2013;9(6):1289–1291.
- van den Hof S, Meffre CM, Conyn-van Spaendonck MA, et al. Measles outbreak in a community with very low vaccine coverage, the Netherlands. Emerg Infect Dis. 2001;7(3 Suppl):593–597.
- Abbas K, Procter SR, van Zandvoort K, et al. Routine childhood immunisation during the COVID-19 pandemic in Africa: a benefit-risk analysis of health benefits versus excess risk of SARS-CoV-2 infection. Lancet Glob Health. 2020;8(10):e1264–e1272.
- O’Sullivan N, O’Sullivan G, Van Harten M. The impact of the COVID-19 pandemic on the uptake of the seasonal influenza vaccine. Ir Med J. 2021;114(2):269.
- Bertoni L, Roncadori A, Gentili N, et al. How has COVID-19 pandemic changed flu vaccination attitudes among an Italian cancer center healthcare workers? Hum Vaccin Immunother. 2022;18(1):1978795.
- Bachtiger P, Adamson A, Chow -J-J, et al. The impact of the COVID-19 pandemic on the uptake of influenza vaccine: UK-wide observational study. JMIR Public Health Surveill. 2021;7(4):e26734.
- Morris T, Tate J. Influenza vaccination during the COVID-19 pandemic. Planning and delivering vaccination programs to protect the most vulnerable people. London: The Health Policy Partnership; 2021.
- UK Health Security Agency. Pertussis vaccination programme for pregnant women update: vaccine coverage in England, October to December 2021. UK Health Security Agency; 2022. ( Health Protection Report; Volume 16 4).
- Anderson E, Brigden A, Davies A, et al. Maternal vaccines during the Covid-19 pandemic:A qualitative interview study with UK pregnant women. Midwifery. 2021;100:103062.
- Bellizzi S, Panu Napodano CM, Pinto S, et al. COVID-19 and seasonal influenza: the potential 2021-22 “Twindemic” Vaccine. 2022;40(24):3286–3287.
- Melidou A, Ködmön C, Nahapetyan K, et al. Influenza returns with a season dominated by clade 3C.2a1b.2a.2 A(H3N2) viruses, WHO European Region, 2021/22. Euro Surveill. 2022;27(15):2200255.
- Centers for Disease Control and Prevention [Internet]. Atlanta (GA): Centers for Disease Control and Prevention. 2021-2022 U.S. Flu season: preliminary in-season burden estimates; 2022 updated 17 Jun 2022; cited 11 Jul 2022]; [about 5 screens. Available from: https://www.cdc.gov/flu/about/burden/preliminary-in-season-estimates.htm
- European Centre for Disease Prevention and Control [Internet]. Stockholm: ECDC; c2022. Influenza virus characterisation - Summary Europe, March 2022; [updated 21 Apr 2022; cited 11 Jul 2022]; [about 3 screens]. Available from: https://www.ecdc.europa.eu/en/publications-data/influenza-virus-characterisation-summary-europe-march-2022
- Martínez-Baz I, Casado I, Miqueleiz A, et al. Effectiveness of influenza vaccination in preventing influenza in primary care, Navarre, Spain, 2021/22. Euro Surveill. 2022;27(26):2200488.
- World Health Organization [Internet]. WHO; c2022. UNICEF and WHO warn of perfect storm of conditions for measles outbreaks, affecting children; 2022 cited 02 May 2022]; [about 7 screens]. Available from: https://www.who.int/news/item/27-04-2022-unicef-and-who-warn-of–perfect-storm–of-conditions-for-measles-outbreaks–affecting-children
- UNICEF [Internet]. UNICEF. Measles cases are spiking globally; 2022 cited 10 Jul 2022]; [about 6 screens]. Available from: https://www.unicef.org/stories/measles-cases-spiking-globally
- The Global Polio Eradication Initiative [Internet]. Swizerland: WHO; 2016. Endemic countries; 2022 [cited 2022 Jul 10; [ about 3 screens]. Available from: https://polioeradication.org/where-we-work/polio-endemic-countries
- United Nations [Internet]. United Nations. First polio outbreak in 30 years declared in Mozambique; 2022 [cited 2022 Jul 11]; [ about 5 screens]. Available from: https://news.un.org/en/story/2022/05/1118502
- World Health Organization [Internet]. WHO; c2022. Disease Outbreak News; Wild poliovirus type 1 (WPV1) - Malawi; 2022 [cited 2022 Jul 11]; [ about 5 screens]. Available from: https://www.who.int/emergencies/disease-outbreak-news/item/wild-poliovirus-type-1-(WPV1)-malawi
- UK Health Security Agency [Internet]. UK Health Security Agency. Poliovirus detected in sewage from North and East London; 2022 cited 2022 Jul 11; [ about 5 screens]. Available from: https://www.gov.uk/government/news/poliovirus-detected-in-sewage-from-north-and-east-london
- Havers FP, Moro PL, Hariri S, et al. Pertussis. In: Hall E, Wodi AP, Hamborsky J, et al. editors. Epidemiology and prevention of vaccine-preventable diseases. 14th. Washington (DC): Public Health Foundation; 2021. p. 239–254.
- Brueggemann AB, Jansen van Rensburg MJ, Shaw D, et al. Changes in the incidence of invasive disease due to streptococcus pneumoniae, haemophilus influenzae, and Neisseria meningitidis during the COVID-19 pandemic in 26 countries and territories in the invasive respiratory infection surveillance initiative: a prospective analysis of surveillance data. Lancet Digit Health. 2021;3(6):e360–e370.
- Amin-Chowdhury Z, Bertran M, Sheppard CL, et al. Does the rise in seasonal respiratory viruses foreshadow the return of invasive pneumococcal disease this winter? Lancet Respir Med. 2022;10(1):e1–e2.
- Commission for Infectious Diseases and Vaccination Issues of the DAKJ (German Academy for Pediatric and Adolescent Medicine). Medizinische Maßnahmen bei immigrierenden Kindern und Jugendlichen – aktualisierung vom 07.10.2013. Stellungnahme der Kommission für Infektionskrankheiten und Impffragen [Medical measures for immigrant children and young people – updated 07.10.2013. Opinion of the Commission on Infectious Diseases and Vaccination]. Monatsschr Kinderheilkd. 2014;162:56–61. In German.
- Haute Autorité de Santé.Catch-up vaccination for newly arrived migrants in the event of unknown, incomplete or incompletely known immunisation status. Haute Autorité de Santé; 2019.
- Centers for Disease Control and Prevention [Internet]. Centers for Disease Control and Prevention. Catch-up immunization schedule for children and adolescents who start late or who are more than 1 month behind; updated 17 Feb 2022; cited 11 Jul 2022]; [about 38 screens]. Available from: https://www.cdc.gov/vaccines/schedules/hcp/imz/catchup.html
- Privor-Dumm LA, Poland GA, Barratt J, et al. A global agenda for older adult immunization in the COVID-19 era: a roadmap for action. Vaccine. 2021;39(37):5240–5250.
- Nam LH, Chiu C-H, Heo JY, et al. The need for pertussis vaccination among older adults and high-risk groups: a perspective from advanced economies of the Asia pacific region. Expert Rev Vaccines. 2021;20(12):1603–1617.
- World Health Organization. Global tuberculosis report 2021. Geneva: WHO; 2021.
- World Health Organization [Internet]. WHO; c2022. Ten threats to global health in 2019; 2019 cited 13 Dec 2021]; [about 18 screens. Available from: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019
- Bayliss J, Randhawa R, Oh KB, et al. Perceptions of vaccine preventable diseases in Australian healthcare: focus on pertussis. Hum Vaccin Immunother. 2021;17(2):344–350.
- Menzies RI, Leask J, Royle J, et al. Vaccine myopia: adult vaccination also needs attention. Med J Aust. 2017;206(6):238–239.
- Wilson RJ, Paterson P, Jarrett C, et al. Understanding factors influencing vaccination acceptance during pregnancy globally: a literature review. Vaccine. 2015;33(47):6420–6429.
- Cavaliere AF, Zaami S, Pallottini M, et al. Flu and tdap maternal immunization hesitancy in times of COVID-19: an Italian survey on multiethnic sample. Vaccines (Basel). 2021;9(10):1107.
- Laupèze B, Del Giudice G, Doherty MT, et al. Vaccination as a preventative measure contributing to immune fitness. NPJ Vaccines. 2021;6(1):93.
- European Centre for Disease Prevention and Control. Communicable disease threats report. Week 7, 13-19 February 2022. ECDC; 2022.
- Government of Western Australia [Internet]. Government of Western Australia. Pertussis notifications. Notifiable infectious diseases reports, WA Department of Health; 2022 cited 2022 Apr 12; [ about 4 screens]. Available from: https://ww2.health.wa.gov.au/Articles/N_R/Notifiable-infectious-disease-report?report=pertussis
- Communicable Disease Control Branch [Internet]. Government of South Australia. Rotavirus chart; 2022 [cited 2022 Apr 12; [ about 1 screen]. Available from: https://www.sahealth.sa.gov.au/wps/wcm/connect/281a3d8042fb3067bb9abb9d0fd82883/Item+9_Rotavirus.pdf?MOD=AJPERES&CACHEID=ROOTWORKSPACE-281a3d8042fb3067bb9abb9d0fd82883-o0sqhvG
- UK Health Security Agency [Internet]. UK Helath Security Agency. Pneumococcal disease: cases caused by strains covered by Prevenar 13 vaccine; 2022 cited 2022 Apr 11; [ about 4 screens]. Available from: https://www.gov.uk/government/publications/pneumococcal-disease-cases-caused-by-strains-covered-by-prevenar-13-vaccine/pneumococcal-disease-cases-caused-by-strains-covered-by-prevenar-13-vaccine
- UK Health Security Agency. National norovirus and rotavirus bulletin: routine norovirus and rotavirus surveillance in England 2021 to 2022 season. 2021. (Week 40 report: data to week 38; 2021 Sept 26.
- Government of Western Australia [Internet]. Rotavirus notifications. Notifiable infectious diseases reports, WA Department of Health; 2022 [cited 2022 Apr 18]; [ about 3 screens]. Available from: https://ww2.health.wa.gov.au/Articles/N_R/Notifiable-infectious-disease-report?report=rotavirus
- Clark S, Campbell H, Mensah AA, et al. [Internet]. Elsevier. An increase in group B invasive meningococcal disease among adolescents and young adults in England following easing of COVID-19 containment measures; 2021 [cited 2022 Apr 11; [about 3 screens]. Available from: http://dx.doi.org/10.2139/ssrn.3998164
- Zheng Z, Pitzer VE, Shapiro ED, et al. Estimation of the timing and intensity of reemergence of respiratory syncytial virus following the COVID-19 pandemic in the US. JAMA Network Open. 2021;4(12):e2141779.
- Reis J, Shaman J. Simulation of four respiratory viruses and inference of epidemiological parameters. Infect Dis Model. 2018;3:23–34.
- Gaythorpe KAM, Trotter CL, Lopman B, et al. Norovirus transmission dynamics: a modelling review. Epidemiol Infect. 2018;146(2):147–158.
- Ma E, Fung C, Yip SH, et al. Estimation of the basic reproduction number of enterovirus 71 and coxsackievirus A16 in hand, foot, and mouth disease outbreaks. Pediatr Infect Dis J. 2011;30(8):675–679.
- Chowell G, Miller MA, Viboud C. Seasonal influenza in the United States, France, and Australia: transmission and prospects for control. Epidemiol Infect. 2008;136(6):852–864.
- Rid A, Lipsitch M, Miller FG. The ethics of continuing placebo in SARS-CoV-2 vaccine trials. JAMA. 2021;325(3):219–220.
- Moll N. The research-based industry response to COVID-19; collaboration and innovation. Eur Pharm Rev. 2021;26(4):34–36.
- Machado BAS, Hodel KVS, Fonseca L, et al. The importance of RNA-based vaccines in the fight against COVID-19: an overview. Vaccines (Basel). 2021;9(11):1345.
- World Health Organization. Immunization Agenda 2030. WHO; 2020.