ABSTRACT
The aim of this study was to investigate if frontal plane knee and hip control in single-leg squats or vertical drop jumps with an overhead target were associated with future non-contact anterior cruciate ligament (ACL) injury in elite female athletes. Of the 429 handball and 451 football athletes (age 21.5 ± 4.0 years, height 169.6 ± 6.4 cm, body weight 67.1 ± 8.0 kg), 722 non-injured and 56 non-contact ACL injured participants were eligible for analysis. We calculated lateral pelvic tilt, frontal plane knee projection angle, medial knee position, and side-to-side asymmetry in these from 2D videos recorded at baseline, and recorded any new ACL injuries prospectively. None of the aforementioned variables in either screening task were different or could discriminate between injured and non-injured athletes (all p values >.05 and Cohen’s d values < .27). Two-dimensional video assessment of frontal plane knee and hip control during both a single-leg squat and vertical drop jump was unable to identify individuals at increased risk of non-contact ACL injury, thus should not be used for screening.
Introduction
Anterior cruciate ligament (ACL) injuries represent a significant concern in sports, due to the serious consequences for the injured athlete, with time lost from sport and decreased performance (Grindem et al., Citation2014). The long-term consequences may be even more severe, with increased risk of early osteoarthritis, reduced knee function and pain (Lie et al., Citation2019). While the practice has recently been questioned (Bahr, Citation2016), some practitioners and researchers still advocate the use of movement screening tests to identify athletes with increased risk for injury (Hewett et al., Citation2016). The assessment of frontal plane hip and knee motion in different movement tasks has been introduced based on the fact that excessive knee valgus motion has consistently been observed in video analyses of non-contact ACL injury situations (Koga et al., Citation2011, Citation2010; Krosshaug et al., Citation2007; Olsen et al., Citation2004; Waldén et al., Citation2015). Two-dimensional (2D) analyses, assessing frontal-plane projection angle (FPPA), are believed to represent a valid and reliable method to quantify knee-valgus motion during a number of screening tasks, including single-leg squats, single-leg landings, drop jump landings, side-steps and side jump manoeuvres (McLean et al., Citation1999, Citation2005; Munro et al., Citation2012; Stensrud et al., Citation2011; Willson & Davis, Citation2008). Filming screening tests using ordinary video cameras can easily be standardised and represents a time-efficient, low-cost assessment tool, compared to more advanced and expensive three-dimensional (3D) marker-based analysis, used in several previous studies (Hewett et al., Citation2005; Krosshaug et al., Citation2016; Leppänen et al., Citation2017). Video-based movement screening would therefore be well suited for large-scale screening. It is also worth noting that, although 3D analysis is believed to represent the gold standard research tool, surface markers can introduce large errors in valgus measurements due to landmark identification and soft tissue artefacts (Gasparutto et al., Citation2020; Mok et al., Citation2015; Stagni et al., Citation2005). Previous fluoroscopy studies (Myers et al., Citation2011) have revealed that while the true valgus angle will be less than 2 degrees in a jump landing, the measurement estimated from surface markers can be up to 30 degrees (Chappell & Limpisvasti, Citation2008; Ford et al., Citation2003). Simple 2D video measurements of frontal plane joint motion may therefore represent a good alternative to using sophisticated 3D motion capture systems to estimate true knee valgus angles. Importantly, even if a screening test may not be able to identify the athlete at risk with sufficient specificity and sensitivity, it could serve an important role in identifying potential risk factors related to movement characteristics at the group level.
Several prospective cohort studies have investigated whether a vertical drop jump (VDJ) can be used for screening purposes. Although a recent meta-analysis (Cronström et al., Citation2020) documents that frontal plane kinematics cannot be used to screen for ACL injury risk, it is worth noting that the initial study identifying knee valgus as a risk factor included an overhead target (Hewett et al., Citation2005), whereas later studies that failed to identify the same factors have not (Krosshaug et al., Citation2016; Leppanen et al., Citation2017; Smith et al., Citation2012). A previous study comparing vertical drop jumps with and without an overhead target concluded that using an overhead target can improve jump height and significantly alter knee biomechanics (Mok et al., Citation2017).
In contrast to what is observed in actual injury situations, the weight is distributed near evenly on both legs in a drop jump task. Thus, a two-leg test is not specific and may also mask potential deficits in either leg. Stensrud et al. (Citation2011) investigated hip and knee kinematics in vertical drop jumps, single-leg squats and single-leg drop jumps and found the two first tests to provide important information on knee control. The correlation between the single-leg squat and vertical drop jump tests was found to be low, suggesting that these tests identified different participants with poor knee control. However, the single-leg squat has so far only been used to assess risk factors for general lower extremity injury (Räisänen et al., Citation2018), but never included in a prospective cohort study on non-contact ACL injuries specifically. Hence, the purpose of this study was to investigate if frontal plane hip and knee kinematics based on 2D-video recordings of vertical drop jumps with an overhead target, or single-leg squats, were associated with increased ACL injury risk. The hypothesis was that greater frontal plane projection angles, medial knee displacement and lateral pelvic tilt, as well as greater leg asymmetry, would be associated with increased ACL injury risk.
Methods
Study design and participants
The current study was based on a prospective cohort study aimed at investigating risk factors for non-contact ACL injuries in female elite handball and football athletes (Krosshaug et al., Citation2016; Sivertsen et al., Citation2019; Steffen et al., Citation2016, Citation2017). In 2007, we invited all teams in the Norwegian female handball premier league to a comprehensive pre-season baseline screening examination. From 2008 to 2013, new teams and athletes advancing to the premier league were invited to the same tests. From 2009 to 2014, we also included football athletes from the female premier league. A total of 880 athletes were included for testing (Football: 451; handball: 429).
The study was approved by the Regional Committee for Medical Research Ethics; South-Eastern Norway Regional Health Authority, and by the Norwegian Social Science Data Services, Norway. Athletes signed a written informed consent form before inclusion, including parental consent for athletes aged <18 yrs.
Screening tests
Athletes attended 1 day of screening during the preseason. Frontal plane video analyses of single-leg squats and vertical drop jumps were part of the screening test battery. The athletes wore shorts, a sports bra and indoor training shoes, and first completed a standardised warm-up procedure, then the single-leg squat, and, finally, the vertical drop jump. The screening tests have been described in detail by Stensrud et al. (Citation2011).
Single-leg squat
The athletes performed a single-leg squat to 90° of knee flexion for each leg, standing on a metal plate. To ensure 90° of knee flexion, two-legged squat depth was measured with a standard goniometer (GYMNA, Berlin, Germany), and a string with a small metal weight was attached to the lateral aspect of the proximal thigh, so that the weight touched the metal plate. The anterior superior iliac spines (ASIS) and tibial tuberosities were marked with a small piece of white tape to facilitate 2D analyses of hip and pelvis position. During the trials, the athletes performed a single-leg squat until the metal weight made contact with the plate and provided feedback to return to the starting position. The athletes held their hands on the waist and were instructed to look forward during the squat. A trial was invalid if they held the opposite leg in front of the body during the squat, if the opposite leg touched the stance leg or the ground, if hands were removed from the waist, or the player lost balance during the performance. Right and left leg performance were analysed separately. We used a digital camera (digital consumer camcorders with SD resolution until 2012 and HD resolution from 2013, both cameras recording at 25 Hz), which was positioned on a tripod, approximately 1 m above the ground and 4.5 m in front of the metal plate, to record all trials for further analyses (Stensrud et al., Citation2011).
Vertical drop jump with overhead target
The athletes performed a vertical drop jump from a 30-cm box, and we used the same digital camera setup as for the single-leg squat. Starting on top of the box, athletes were instructed to drop off the box using a symmetrical 2-foot landing strategy, immediately followed by a maximal vertical jump. To ensure that athletes performed the jump with maximal effort and with an external focus of attention, a ball was attached to a string hanging 260 cm above the floor, of which the athletes were encouraged to touch. A trial was judged invalid if the athletes jumped rather than dropped off the box or failed to perform a maximal effort vertical jump after the first landing. Athletes were allowed three practice trials before the test and completed three valid trials.
2D video analyses
We included three valid trials for each leg from the single-leg squat, and three valid trials from the vertical drop jump test and analysed the deepest position of each trial. For the vertical drop jump, we also analysed the frame of initial heel contact, i.e. when the foot was flat on the ground. We used a Java-based computer software (ImageJ, Version 1.50, National Institutes of Health, USA) to identify joint centres using digital markers and to calculate joint kinematics. All testers underwent a structured training programme, involving a thorough description of the procedures, followed by two rounds of practice analyses. After each round, we had consensus meetings where we discussed the selection of frames and marker placements. After the final consensus meeting, we conducted independent analyses of 20 participants, to determine the inter-rater reliability.
Joint centre estimation
Due to differences in body anthropometrics, technique and video quality, estimating joint centres was the part requiring most discussions and training. To estimate joint centres as accurate as possible, we used a Model-Based Imaged-Matching technique described in Krosshaug and Bahr (Citation2005) to visualise hip, knee and ankle joints as a part of the structured training program ().
Figure 1. Superimposed skeleton model during a single-leg squat to estimate joint centres, using the method of Krosshaug and Bahr (Citation2005).

The hip joint centres were estimated when the player was standing upright, using a frame prior to the analysed frames, and was defined using the method of Bell (Bell et al., Citation1990). ImageJ allowed us to keep the same, fixed distance between the hip joint centres in all the analysed frames. The hip joint centres were estimated when the player was standing upright and was defined using the method of Bell (Bell et al., Citation1990). ImageJ allowed us to keep the same, fixed distance between the hip joint centres in all the frames analysed. Both joint centres were moved simultaneously using the left/right/down/up keys as the participant descended towards the greater hip and knee flexion, to ensure a fixed width between the hip joint centres. We estimated the hip joint centres based on thigh and trunk segment movements using the observations learned during the training sessions to guide positioning. In case of an observed lateral pelvic tilt, we naturally allowed a height difference in the hip joint centres, and kept the horizontal distance fixed. The knee joint centres were defined as the mid-point between the femur condyles (Davis et al., Citation1991). The ankle joint centres were defined as the mid-point between the lateral and medial malleoli, while at the same time taking into consideration the possible internal or external rotation of the tibia (Eng & Winter, Citation1995). When all joint centres were identified using the digital markers, we extracted the x and y coordinates for each marker to calculate knee and hip joint kinematics.
Variables
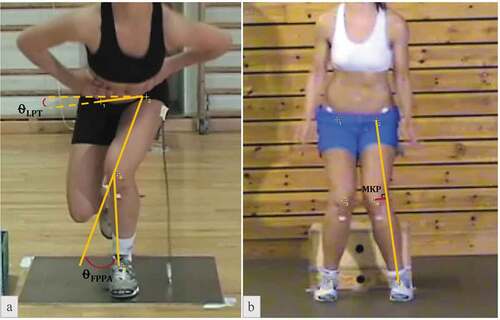
For the single-leg squat, we calculated the frontal plane projection angle (FPPA), medial knee position (MKP), and the lateral pelvic tilt (LPT) for both sides, as well as asymmetry in these variables between sides. For the vertical drop jump test, we calculated FPPA, MKP, and medial knee displacement (MKD) at initial contact and peak knee flexion, as well as the asymmetry between legs. The FPPA was defined as the angle set by the line connecting the hip and knee joint, and the line connecting the knee and ankle joint ()). FPPA <0 represents knee valgus, whereas values >0 correspond to knee varus. LPT was defined as the angle between the line drawn between right and left hip joint centres and a horizontal line through the hip joint centre of the squatting leg ()). LPT >0 represents a contralateral drop of the pelvis, whereas LPT <0 represents a contralateral hike (elevation) of the pelvis. MKP was defined as the perpendicular distance from the knee joint centre to the line joining the ankle and hip joint centres, projected onto the frontal plane ()). We calculated the distance in pixels, normalised for leg length, where leg length was defined as the pixel distance between the hip and ankle joint centre at initial heel contact of the drop jump. MKP <0 corresponds to knee valgus, whereas MKP >0 corresponds to knee varus. MKD was calculated as the difference between MKP at initial contact and peak knee flexion.
Figure 2. The single-leg squat (a) and the vertical drop jump (b) tests, visually presenting the calculation of the lateral pelvic tilt (LPT) and frontal plane projection angle (FPPA) in 2A, and the medial knee position (MKP) in 2B. The FPPA angle and Medial Knee Position seen in these athletes would have a negative sign due to the valgus joint position.
Injury registration
We recorded all complete ACL injuries among the tested athletes through March 2015 (eight years/seasons), primarily through semi-annual contact with the participating teams (manager, coach, medical staff), or monthly during the competitive season. If any acute knee injuries occurring during regular team training or competition were reported, we contacted the injured player by phone to obtain detailed medical data and a description of the injury situation. All ACL injuries were verified by MRI and/or arthroscopy as complete ruptures. Direct contact related injuries were excluded from the analysis (N = 9). In addition, we obtained information about previous ACL injuries through questionnaires administrated as part of the screening test battery.
Statistical procedures
To determine differences in 2D kinematics between future non-contact ACL injured and non-injured athletes, independent Welch’s t-tests were used to compare means given the unequal sample sizes (Delacre et al., Citation2017) as well as measures of effect size using Cohen’s d. Area under the receiver operating characteristics curve (AUC) was also performed for each variable to determine the prognostic characteristics. Area under the curve values were characterised as: outstanding (0.90–1), excellent (0.80–0.89), acceptable (0.70–0.79), poor (0.51–0.69), and no discrimination (0.50) (Hosmer et al., Citation2013). Finally, we performed logistic regression analyses for each variable to control for variables that may influence injury risk such as previous ACL injury to either side and sport type (Annesi et al., Citation1989; Janes & Pepe, Citation2008). For the non-injured athletes, we selected a random side/limb to be included in the analysis. Data were analysed using R (Team, Citation2018) with pROC to perform the receiver operating characteristic (ROC) and area under the curve (AUC) analysis.
To assess inter-rater reliability for marker positioning and calculation of variables between raters, we calculated intraclass correlation coefficients (ICC) and standard error of measurements (SEM). Based on the 95% confident interval of the ICC estimate, values less than 0.50 are indicative of poor, between 0.50 and 0.75 as moderate, between 0.75 and 0.90 as good, and greater than 0.90 are defined as excellent reliability (Koo & Li, Citation2016). The alpha level was set at p < .05 for all analyses.
Results
Of the 429 handball and 451 football athletes (age 21.5 ± 4.0 years, height 169.6 ± 6.4 cm, body weight 67.1 ± 8.0 kg) included, 86 athletes had a previous ACL injury, of which 14 suffered a new ACL injury. In total, we recorded 74 new ACL injuries. Some had to be excluded from the analyses for the following reasons: 1) contact related ACL injury (n = 9), 2) incomplete or invalid tests, 3) video recording errors. The sample size for each variable is reported in . The median time from testing to injury was 434 days, and 25 (39%) of those injuries occurred within 1 year after testing.
Table 1. Frontal plane kinematic descriptive and statistical tests for differences between injured and non-injured.
None of the variables within the single-leg squat or drop vertical jump could discriminate between athletes who sustained a future non-contact ACL injury or the non-injured athletes (). The results of the logistic regression analyses and corresponding adjusted odds ratios corroborated the univariable analyses. For the variables shown in the table, we also calculated side-to-side differences as a measure of asymmetry. None of the asymmetry variables differed between groups, nor could they discriminate between injured and non-injured (p values >.54).
Inter-rater reliability
Due to the vast amount of work involved in analysing all trials of nearly 800 players, we had two teams (team 1: four analysts, and team 2: three analysts), responsible for the handball and football cohorts, respectively. We calculated intra-rater reliability for each team individually, based on analyses of 20 randomly selected athletes from the cohort. Inter-rater reliability was found to be good to excellent, in all but two variables, with intraclass correlation coefficients (ICC) ranging from 0.60 to 0.95 for all variables, also confirmed by the standard error of measurements (SEM) for both sessions ().
Table 2. Summary of the inter-rater reliability from two separate sessions.
Discussion and implications
The purpose of this study was to investigate if frontal plane knee and hip kinematics in single-leg squats, or vertical drop jumps with an overhead target, are associated with future ACL injury risk. However, none of the variables in either tests were associated with an increased risk for ACL injury.
The vertical drop jump test
Although we included an overhead target for the VDJ test, the result did not deviate from the recent meta-analysis of Cronström et al. (Citation2020). We found only minor, non-significant, differences in group means, and all effect sizes were smaller than 0.3, suggesting that even if we would have identified statistically significant differences, these would likely be of minor importance. In other words, even if we had more than 100 injury cases, there are no indications suggesting that the conclusion would change. Although some past VDJ studies, based on smaller samples, have suggested that we may be able to identify risk factors in some cohorts, the results are inconsistent and the factors identified differ between each study (Hewett et al., Citation2005; Leppänen et al., Citation2017; Padua et al., Citation2015). Even if the VDJ test could be useful in certain cohorts, higher-powered studies have revealed that the VDJ test failed to provide any information on future injury risk in female elite handball and football athletes, in high school and college athletes or in combat soldiers (Krosshaug et al., Citation2016; Schwartz et al., Citation2020; Smith et al., Citation2012). These studies cover different age groups, playing levels and sexes.
The single-leg squat test
Based on previous investigations, we know that the single-leg squat test can detect poor knee control, i.e. greater valgus motion, in athletes who demonstrate good control in the VDJ test. Therefore, we wanted to examine whether such a single-leg test could detect injury-related movement characteristics. However, the results clearly demonstrated this to not be the case. If anything, the tendencies were towards valgus movement being higher in the non-injured group. Although these two tests failed to detect movement-related risk factors, two studies suggest that single-leg drop jumps may be more suitable to detect movement-related risk factors. In a study by Numata et al. (Citation2018), 27 non-contact ACL injuries in high-school basketball and handball athletes were recorded after baseline testing; they were compared to 27 randomly selected uninjured knees. Greater valgus measures were identified in athletes who later were injured. In an even smaller cohort, with seven ACL injuries, Dingenen et al. (Citation2015) found a combination of increased knee valgus and ipsilateral trunk motion during a single-leg drop jump to be a risk factor. These findings should be considered as preliminary evidence for valgus as a risk factor for ACL injury, and need to be replicated in a variety of larger cohorts before we can make firm conclusions. They also suggest that a one-leg drop jump may be a more appropriate task than two-leg drop jumps or single-leg squats to identify injury-related movement characteristics. A one-leg landing is clearly more sport-specific and, importantly, more injury-specific, compared to the two tests used in our study. One may speculate that a cutting test might provide even higher predictive power compared to one-leg drop jumps. Recently, Nedergaard et al. (Citation2020) reported poor correlations between single-leg drop/jump tasks and a cutting manoeuvre. Numata et al. (Citation2018) reported a 2.5 times greater number of cutting-related injury situations compared to single-leg landings. However, there are currently no prospective cohort studies using cutting manoeuvre biomechanics as the prognostic variable.
Methodological considerations
The present study represents a major undertaking with more than 800 elite female handball and football athletes assessed using a screening task over a 7-year period, with 15 included test sessions in total. The current analyses included 56 non-contact ACL injuries, more than twice the size of most other cohorts. This is important, as most other published studies are simply too small to be conclusive. According to Bahr and Holme, strong to moderate associations can only be detected if the study includes 20–50 injury cases, and the measurement tool has high reliability. Unfortunately, high movement variability and less than optimal measurement reliability place most studies in the low end of this interval, and at least those which have less than 20 injury cases are highly susceptible to drawing spurious conclusions.
For the video analyses, we dedicated substantial time and effort to optimising validity and reliability before conducting thorough analyses. The many iterations of ‘calibrating’ the video analysts were time-consuming, but resulted in good to excellent reliability for all variables, except for left leg MKP. Moreover, to ensure high validity, we used sophisticated methods (Krosshaug & Bahr, Citation2005) to visualise the joint centres so that the assessors would be precise in identifying joint centres, even in difficult scenarios where the player displayed excessive forward lean. The reliability between testers in this study is comparable with previous studies investigating test–retest reliability within the same tester (Gwynne & Curran, Citation2014; Munro et al., Citation2012; Warner et al., Citation2019). Hence, we can be fairly confident in the results of this study, despite having several assessors.
Due to different light conditions and advances in video camera technology, the video sequences from the last years were noticeably improved over the first years. However, importantly, although picture quality was less optimal in the first years, we do not believe that we would be able to identify the ankle and knee joint centres more precise with higher quality, as long as the boundaries of the leg were clearly identifiable even in the older recordings. Furthermore, we included both new and old videos for our reliability tests, making them representative of the data material as a whole. Unfortunately, in some test sessions (7 handball sessions and 6 football sessions overall), video cameras were not levelled, as can be seen in ). This may have impacted our measurements of lateral pelvic tilt and may have impacted our risk factor estimates. For this reason, we conducted an additional regression analysis correcting for this variable, including a test session as an adjustment factor. However, the results were virtually identical to the un-adjusted statistical model.
Although we calculated several different movement variables to thoroughly characterise frontal plane knee control, it is possible that other movement-related variables than the ones we have investigated could be more important. However, in a recent online video analysis study, more than 200 sports medicine professionals aimed to rate injury risk, based on a vertical drop jump test from 101 players (Mørtvedt et al., Citation2020). Twenty of these players would later sustain an ACL injury. The sports medicine practitioners were allowed to assess these videos repeatedly to identify any risk factor that may be present. The study clearly demonstrated that none of these practitioners, many with higher education and extensive clinical experience, were able to detect any movement-related factors relevant to ACL injury.
Conclusion
The current study found no association between frontal plane hip and knee kinematics in single-leg squats or vertical drop jumps with overhead target and ACL injury risk in elite female handball and football athletes. Future prospective studies may need to utilise other movement tasks, with a closer resemblance to injury situations, to identify risk factors associated with ACL injury.
Acknowledgments
We thank Maya Rosvoll, Sólveig Þórarinsdóttir, Camilla Christensen and Jørn Erik Strand for their contributions to the video analyses. A special thanks to Inge Dehli Andersen for valuable help with data acquisition. We also acknowledge all athletes in the Norwegian female soccer and handball premier league for their participation in the study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Annesi, I., Moreau, T., & Lellouch, J. (1989). Efficiency of the logistic regression and cox proportional hazards models in longitudinal studies. Statistics in Medicine, 8(12), 1515–1521. https://doi.org/10.1002/sim.4780081211
- Bahr, R. (2016). Why screening tests to predict injury do not work-and probably never will … : A critical review. British Journal of Sports Medicine, 50(13), 776–780. https://doi.org/10.1136/bjsports-2016-096256
- Bell, A. L., Pedersen, D. R., & Brand, R. A. (1990). A comparison of the accuracy of several hip center location prediction methods. Journal of Biomechanics, 23(6), 617–621. https://doi.org/10.1016/0021-9290(90)90054-7
- Chappell, J. D., & Limpisvasti, O. (2008). Effect of a neuromuscular training program on the kinetics and kinematics of jumping tasks. The American Journal of Sports Medicine, 36(6), 1081–1086. https://doi.org/10.1177/0363546508314425
- Cronström, A., Creaby, M. W., & Ageberg, E. (2020, August 20). Do knee abduction kinematics and kinetics predict future anterior cruciate ligament injury risk? A systematic review and meta-analysis of prospective studies. BMC Musculoskeletal Disorders, 21(1), 563. PMID: 32819327; PMCID: PMC7441716. https://doi.org/10.1186/s12891-020-03552-3
- Davis, R. B., III, Ounpuu, S., Tyburski, D., & Gage, J. R. (1991). A gait analysis data collection and reduction technique. Human Movement Science, 10(5), 575–587. https://doi.org/10.1016/0167-9457(91)90046-Z
- Delacre, M., Lakens, D., & Leys, C. (2017). Why psychologists should by default use Welch’s t-test instead of student’s t-test. International Review of Social Psychology, 30(1), 92. https://doi.org/10.5334/irsp.82
- Dingenen, B., Malfait, B., Nijs, S., Peers, K. H., Vereecken, S., Verschueren, S. M., & Staes, F. F. (2015). Can two-dimensional video analysis during single-leg drop vertical jumps help identify non-contact knee injury risk? A one-year prospective study. Clinical Biomechanics (Bristol, Avon), 30(8), 781–787. https://doi.org/10.1016/j.clinbiomech.2015.06.013
- Eng, J. J., & Winter, D. A. (1995). Kinetic analysis of the lower limbs during walking: What information can be gained from a three-dimensional model? Journal of Biomechanics, 28(6), 753–758. https://doi.org/10.1016/0021-9290(94)00124-M
- Ford, K. R., Myer, G. D., & Hewett, T. E. (2003). Valgus knee motion during landing in high school female and male basketball players. Med Sci Sports Exerc, 35(10), 1745–1750. https://doi.org/10.1249/01.MSS.0000089346.85744.D9
- Gasparutto, X., Wegrzyk, J., Rose-Dulcina, K., Hannouche, D., & Armand, S. (2020). Can the fusion of motion capture and 3D medical imaging reduce the extrinsic variability due to marker misplacements? PloS One, 15(1), e0226648. https://doi.org/10.1371/journal.pone.0226648
- Grindem, H., Eitzen, I., Engebretsen, L., Snyder-Mackler, L., & Risberg, M. A. (2014). Nonsurgical or surgical treatment of ACL injuries: Knee function, sports participation, and knee reinjury: The Delaware-Oslo ACL cohort study. The Journal of Bone and Joint Surgery. American Volume, 96(15), 1233–1241. https://doi.org/10.2106/JBJS.M.01054
- Gwynne, C. R., & Curran, S. A. (2014). Quantifying frontal plane knee motion during single limb squats: Reliability and validity of 2-dimensional measures. International Journal of Sports Physical Therapy, 9(7), 898–906. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4275194/
- Hewett, T. E., Myer, G. D., Ford, K. R., Heidt, R. S., Jr, Colosimo, A. J., McLean, S. G., Van den Bogert, A. J., Paterno, M. V., & Succop, P. (2005, April). Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: A prospective study. The American Journal of Sports Medicine, 33 (4), 492–501. Epub 2005 Feb 8. PMID: 15722287. https://doi.org/10.1177/0363546504269591
- Hewett, T. E., Myer, G. D., Ford, K. R., Paterno, M. V., & Quatman, C. E. (2016). Mechanisms, prediction, and prevention of ACL injuries: Cut risk with three sharpened and validated tools. Journal of Orthopaedic Research: Official Publication of the Orthopaedic Research Society, 34(11), 1843–1855. https://doi.org/10.1002/jor.23414
- Hosmer Jr, D. W., Lemeshow, S., & Sturdivant, R. X. (2013). Applied logistic regression (Vol. 398). John Wiley & Sons.
- Janes, H., & Pepe, M. S. (2008). Adjusting for covariates in studies of diagnostic, screening, or prognostic markers: An old concept in a new setting. American Journal of Epidemiology, 168(1), 89–97. https://doi.org/10.1093/aje/kwn099
- Koga, H., Bahr, R., Myklebust, G., Engebretsen, L., Grund, T., & Krosshaug, T. (2011). Estimating anterior tibial translation from model-based image-matching of a noncontact anterior cruciate ligament injury in professional football: A case report. Clinical Journal of Sport Medicine: Official Journal of the Canadian Academy of Sport Medicine, 21(3), 271–274. https://doi.org/10.1097/JSM.0b013e31821899ec
- Koga, H., Nakamae, A., Shima, Y., Iwasa, J., Myklebust, G., Engebretsen, L., Bahr, R., & Krosshaug, T. (2010). Mechanisms for noncontact anterior cruciate ligament injuries: Knee joint kinematics in 10 injury situations from female team handball and basketball. The American Journal of Sports Medicine, 38(11), 2218–2225. https://doi.org/10.1177/0363546510373570
- Koo, T. K., & Li, M. Y. (2016). A guideline of selecting and reporting intraclass correlation coefficients for reliability research. Journal of Chiropractic Medicine, 15(2), 155–163. https://doi.org/10.1016/j.jcm.2016.02.012
- Krosshaug, T., & Bahr, R. (2005). A model-based image-matching technique for three-dimensional reconstruction of human motion from uncalibrated video sequences. Journal of Biomechanics, 38(4), 919–929. https://doi.org/10.1016/j.jbiomech.2004.04.033
- Krosshaug, T., Nakamae, A., Boden, B. P., Engebretsen, L., Smith, G., Slauterbeck, J. R., Hewett, T. E., & Bahr, R. (2007). Mechanisms of anterior cruciate ligament injury in basketball: Video analysis of 39 cases. The American Journal of Sports Medicine, 35(3), 359–367. https://doi.org/10.1177/0363546506293899
- Krosshaug, T., Steffen, K., Kristianslund, E., Nilstad, A., Mok, K. M., Myklebust, G., Andersen, T. E., Holme, I., Engebretsen, L., & Bahr, R. (2016, April). The vertical drop jump is a poor screening test for ACL injuries in female elite soccer and handball players: A prospective cohort study of 710 athletes. The American Journal of Sports Medicine, 44 (4), 874–883. Epub 2016 Feb 11. Erratum in: The American Journal of Sports Medicine. 2017 Jul;45(9):NP28-NP29. PMID: 26867936. https://doi.org/10.1177/0363546515625048
- Leppänen, M., Pasanen, K., Kujala, U. M., Vasankari, T., Kannus, P., Äyrämö, S., Krosshaug, T., Bahr, R., Avela, J., Perttunen, J., & Parkkari, J. (2017, February). Stiff landings are associated with increased ACL injury risk in young female basketball and floorball players. The American Journal of Sports Medicine, 45 (2), 386–393. Epub 2016 Oct 1. PMID: 27637264. https://doi.org/10.1177/0363546516665810
- Lie, M. M., Risberg, M. A., Storheim, K., Engebretsen, L., & Øiestad, B. E. (2019). What’s the rate of knee osteoarthritis 10 years after anterior cruciate ligament injury? An updated systematic review. British Journal of Sports Medicine, 53(18), 1162–1167. https://doi.org/10.1136/bjsports-2018-099751
- McLean, S. G., Neal, R. J., Myers, P. T., & Walters, M. R. (1999). Knee joint kinematics during the sidestep cutting maneuver: Potential for injury in women. Medicine and Science in Sports and Exercise, 31(7), 959–968. https://doi.org/10.1097/00005768-199907000-00007
- McLean, S. G., Walker, K., Ford, K. R., Myer, G. D., Hewett, T. E., & Van Den Bogert, A. J. (2005). Evaluation of a two dimensional analysis method as a screening and evaluation tool for anterior cruciate ligament injury. British Journal of Sports Medicine, 39(6), 355–362. https://doi.org/10.1136/bjsm.2005.018598
- Mok, K. M., Bahr, R., & Krosshaug, T. (2017). The effect of overhead target on the lower limb biomechanics during a vertical drop jump test in elite female athletes. Scandinavian Journal of Medicine & Science in Sports, 27(2), 161–166. https://doi.org/10.1111/sms.12640
- Mok, K. M., Kristianslund, E. K., & Krosshaug, T. (2015). The effect of thigh marker placement on knee valgus angles in vertical drop jumps and sidestep cutting. Journal of Applied Biomechanics, 31(4), 269–274. https://doi.org/10.1123/jab.2014-0137
- Mørtvedt, A. I., Krosshaug, T., Bahr, R., & Petushek, E. (2020). I spy with my little eye … a knee about to go ‘pop’? Can coaches and sports medicine professionals predict who is at greater risk of ACL rupture? British Journal of Sports Medicine, 54(3), 154–158. https://doi.org/10.1136/bjsports-2019-100602
- Munro, A., Herrington, L., & Carolan, M. (2012). Reliability of 2-dimensional video assessment of frontal-plane dynamic knee valgus during common athletic screening tasks. Journal of Sport Rehabilitation, 21(1), 7–11. https://doi.org/10.1123/jsr.21.1.7
- Myers, C. A., Torry, M. R., Peterson, D. S., Shelburne, K. B., Giphart, J. E., Krong, J. P., Woo, S. L., & Steadman, J. R. (2011). Measurements of tibiofemoral kinematics during soft and stiff drop landings using biplane fluoroscopy. The American Journal of Sports Medicine, 39(8), 1714–1722. https://doi.org/10.1177/0363546511404922
- Nedergaard, N. J., Dalbø, S., Petersen, S. V., Zebis, M. K., & Bencke, J. (2020). Biomechanical and neuromuscular comparison of single-and multi-planar jump tests and a side-cutting maneuver: Implications for ACL injury risk assessment. The Knee, 27(2), 324–333. https://doi.org/10.1016/j.knee.2019.10.022
- Numata, H., Nakase, J., Kitaoka, K., Shima, Y., Oshima, T., Takata, Y., Shimozaki, K., & Tsuchiya, H. (2018). Two-dimensional motion analysis of dynamic knee valgus identifies female high school athletes at risk of non-contact anterior cruciate ligament injury. Knee Surgery, Sports Traumatology, Arthroscopy: Official Journal of the ESSKA, 26(2), 442–447. https://doi.org/10.1007/s00167-017-4681-9
- Olsen, O. E., Myklebust, G., Engebretsen, L., & Bahr, R. (2004). Injury mechanisms for anterior cruciate ligament injuries in team handball: A systematic video analysis. The American Journal of Sports Medicine, 32(4), 1002–1012. https://doi.org/10.1177/0363546503261724
- Padua, D. A., DiStefano, L. J., Beutler, A. I., De La Motte, S. J., DiStefano, M. J., & Marshall, S. W. (2015). The landing error scoring system as a screening tool for an anterior cruciate ligament injury-prevention program in elite-youth soccer athletes. Journal of Athletic Training, 50(6), 589–595. https://doi.org/10.4085/1062-6050-50.1.10
- Räisänen, A. M., Arkkila, H., Vasankari, T., Steffen, K., Parkkari, J., Kannus, P., Forsman, H., & Pasanen, K. (2018). Investigation of knee control as a lower extremity injury risk factor: A prospective study in youth football. Scandinavian Journal of Medicine & Science in Sports, 28(9), 2084–2092. https://doi.org/10.1111/sms.13197
- Schwartz, O., Talmy, T., Olsen, C. H., & Dudkiewicz, I. (2020). The landing error scoring system real-time test as a predictive tool for knee injuries: A historical cohort study. Clinical Biomechanics (Bristol, Avon), 73, 115–121. https://doi.org/10.1016/j.clinbiomech.2020.01.010
- Sivertsen, E. A., Haug, K., Kristianslund, E. K., Trøseid, A. S., Parkkari, J., Lehtimäki, T., Mononen, N., Pasanen, K., & Bahr, R. (2019). No association between risk of anterior cruciate ligament rupture and selected candidate collagen gene variants in female elite athletes from high-risk team sports. The American Journal of Sports Medicine, 47(1), 52–58. https://doi.org/10.1177/0363546518808467
- Smith, H. C., Johnson, R. J., Shultz, S. J., Tourville, T., Holterman, L. A., Slauterbeck, J., Vacek, P. M., & Beynnon, B. D. (2012). A prospective evaluation of the landing error scoring system (LESS) as a screening tool for anterior cruciate ligament injury risk. The American Journal of Sports Medicine, 40(3), 521–526. https://doi.org/10.1177/0363546511429776
- Stagni, R., Fantozzi, S., Cappello, A., & Leardini, A. (2005, March). Quantification of soft tissue artefact in motion analysis by combining 3D fluoroscopy and stereophotogrammetry: A study on two subjects. Clinical Biomechanics (Bristol, Avon), 20 (3), 320–329. PMID: 15698706. https://doi.org/10.1016/j.clinbiomech.2004.11.012
- Steffen, K., Nilstad, A., Kristianslund, E. K., Myklebust, G., Bahr, R., & Krosshaug, T. (2016). Association between lower extremity muscle strength and noncontact ACL injuries. Medicine and Science in Sports and Exercise, 48(11), 2082–2089. https://doi.org/10.1249/MSS.0000000000001014
- Steffen, K., Nilstad, A., Krosshaug, T., Pasanen, K., Killingmo, A., & Bahr, R. (2017). No association between static and dynamic postural control and ACL injury risk among female elite handball and football players: A prospective study of 838 players. British Journal of Sports Medicine, 51(4), 253–259. https://doi.org/10.1136/bjsports-2016-097068
- Stensrud, S., Myklebust, G., Kristianslund, E., Bahr, R., & Krosshaug, T. (2011). Correlation between two-dimensional video analysis and subjective assessment in evaluating knee control among elite female team handball players. British Journal of Sports Medicine, 45(7), 589–595. https://doi.org/10.1136/bjsm.2010.078287
- Team, R. C. (2018). R: A language and environment for statistical computing. R Foundation for Statistical Computing. Austria: Vienna.
- Waldén, M., Krosshaug, T., Bjørneboe, J., Andersen, T. E., Faul, O., & Hägglund, M. (2015). Three distinct mechanisms predominate in non-contact anterior cruciate ligament injuries in male professional football players: A systematic video analysis of 39 cases. British Journal of Sports Medicine, 49(22), 1452–1460. https://doi.org/10.1136/bjsports-2014-094573
- Warner, M. B., Wilson, D. A., Herrington, L., Dixon, S., Power, C., Jones, R., Heller, M. O., Carden, P., & Lewis, C. L. (2019). A systematic review of the discriminating biomechanical parameters during the single leg squat. Physical Therapy in Sport: Official Journal of the Association of Chartered Physiotherapists in Sports Medicine, 36, 78–91. https://doi.org/10.1016/j.ptsp.2019.01.007
- Willson, J. D., & Davis, I. S. (2008). Utility of the frontal plane projection angle in females with patellofemoral pain. The Journal of Orthopaedic and Sports Physical Therapy, 38(10), 606–615. https://doi.org/10.2519/jospt.2008.2706
