ABSTRACT
Introduction: Energy-based cosmetic devices offer an in-office treatment option, with minimal downtime, to non-invasively remove unwanted fat. We evaluated focused, pulsed ultrasound treatment to randomized flanks, compared to corresponding non-treated contralateral flanks. Material and Methods: Subjects were enrolled at three sites for a series of focused ultrasound treatments to a single flank, with the contralateral flank remaining untreated throughout the study. Success criteria included measureable fat thickness reduction on ultrasound imaging in the treated areas at 16 weeks after the final treatment session, and correct identification of the post-treatment photo and treated flank in at least 80% of evaluated images, as assessed by two blinded evaluators. Results: The post-treatment flank photo and treated flank side were correctly identified in 82% and 93% of cases, respectively. All study subjects demonstrated significant fat reduction in their treated area, as measured by ultrasound and skin caliper. Subjects expressed a high satisfaction from treatment outcomes. There were no complications with treatment. Conclusion: A series of three ultrasound treatments resulted in significant fat reduction in treated flanks. Although treatment results are more modest than with liposuction, non-invasive ultrasound treatment may provide an attractive alternative for patients seeking an in-office, nonsurgical procedure for fat reduction.
Introduction
A growing number of people in our modern society are seeking cosmetic solutions for the removal of excess and unwanted fat on the body to achieve a more pleasing body image. Adipose tissue is a loose connective tissue composed of adipocytes specialized to store lipids. The majority of lipids stored in adipose cells are triglycerides formed from imported free fatty acids and glycerol. Adipose tissue is not uniformly distributed throughout the body, with the majority of adipose tissue deposits being found in the subcutaneous fat layer, which composes approximately 80% of all body fat (Citation1). In men, subcutaneous fat normally represents about 15–20% of body weight, while in women, subcutaneous fat can range from 20 to 25% of total body weight. A minimal amount of body fat is necessary for normal female reproduction and general health. Subcutaneous adipose tissue helps to shape, cushion, and insulate the body, and provides padding for internal organs.
Body contouring is the targeted removal of limited amounts of adipose tissue to achieve a more aesthetically pleasing body shape. Non-invasive body contouring procedures have become very popular in the modern aesthetic practice as they can offer patients visually appreciable improvements in body shape and image, without more invasive surgical approaches and techniques. More invasive surgically oriented procedures are associated with inherent surgical risks as well as prolonged recovery times, and may not be the ideal treatment option for those patients who are anxious of and/or contraindicated for surgical approaches. Innovative energy-based cosmetic technologies such as laser, ultrasound, and radiofrequency (RF) have been developed for aesthetic medicine. These novel technologies have become very popular in fat reduction and body contouring procedures, as they offer patients an excellent treatment alternative to more traditional surgical body sculpting approaches.
Liposuction is a procedure used to sculpt body contour by surgically removing unwanted fat from specific targeted areas (Citation2–Citation4). The increasing popularity of this procedure has led to the evolution of techniques and equipment for fat removal, body reshaping, and cellulite treatments. Besides traditional suction-assisted lipoplasty, other technique options include ultrasound-assisted and external ultrasound-assisted liposuction, power-assisted liposuction, laser lipolysis as well as low-level laser-assisted liposculpture (Citation5).
The efforts in the search for alternative non-invasive or minimally invasive techniques and new tools aim mainly at reducing downtime and facilitating treatment for reduction of localized fatty tissue areas. New minimally invasive technologies include subcutaneous injection of phosphatidylcholine. This drug was initially used in emergencies and in the treatment of atheroma plaques in cardiac diseases. Recently, it has also been used in the treatment of localized fat deposits, especially in the submental area (Citation6).
Suboptimal treatment outcomes and limitations of past approaches and techniques have spurred continued research in this cosmetic niche, and led to the development of novel technologies that can be used for the non-invasive reduction of unwanted excess fat deposits including laser, cryotherapy, radiofrequency, and ultrasound (Citation7–Citation12). Previous studies have shown the therapeutic benefit of a focused ultrasound system, used for the treatment of unwanted excess adipose tissue and improvement of body contours (Citation7,Citation13–Citation18).
Focused ultrasound produces localized mechanical motion within fat tissues and cells for the purpose of producing cellular membrane disruption. In this clinical study, we evaluated the efficacy and safety of a non-thermal ultrasound device for non-invasive fat reduction treatment on the flanks with the goal of improving body shape and contour in this region.
Material and methods
Patients
Subjects with a body mass index of 22–30 and fat thickness of at least 1.5 cm in the treated area, as measured by calibrated caliper, were enrolled at three USA sites. Severe skin laxity or previous body contouring procedures within the past 12 months in the treated area excluded subjects from participation. The study was approved by the Chesapeake Institutional Review Board. All patients met the inclusion/exclusion criteria and provided written informed consent for participation in the study.
Device description
Treatments were performed using the UltraShape system (or Syneron Contour I V3.1) system (Syneron Medical Ltd., Yokneam, Israel). The focused ultrasonic technology emits acoustic sound waves of ultrasonic energy (200 ± 30 KHz frequency) that converge into a confined focal volume at a depth of 1.5 cm below the skin’s surface, targeting the subcutaneous fat at a controlled depth. Unlike traditional ultrasound technology, focused, pulsed ultrasound transmits bursts of pulsed ultrasound, allowing precision control over temperature elevation (less than 0.5°C increase) and enabling mechanical (non-thermal) selected fat destruction at a designated focal point in the subcutaneous fat layer. During treatment, the focused ultrasound causes rapid changes in pressure and creates bubbles in the interstitial fluid located between the adipocytes in the targeted area. These bubbles subsequently implode from the imposed quick pressure changes, leading to the rupture of the adipocyte walls.
In this study, a small 12-gram transducer was used to deliver the focused ultrasound energy to the flanks. Real-time optical and acoustic feedback on treatment was provided via the tracking and guidance system, ensuring that the treatment was performed only within the designated area in a homogenous manner. The in-office procedure was performed without anesthesia.
Study design
Subjects underwent three treatment sessions at 2-week intervals, with the ultrasound transducer in Single-Pass Mode on one randomized flank, with the contralateral flank remaining untreated throughout the study. Each subject was assessed at baseline and at each follow-up visit, which occurred at 4-, 8-, and 16-weeks after the final ultrasound treatment session.
Fat thickness at the flanks was measured by skin caliper and ultrasound imaging at baseline and at each follow-up visit. Clinical photographs were taken in a standardized manner at baseline and at each follow-up visit, and used for blinded evaluation of treatment outcome.
Study measurements
The primary endpoint was fat reduction in treated flanks, based on visual assessment by two blinded investigators of randomized photographs of before (baseline) versus after (16 weeks following last treatment), as well as treated versus untreated flanks. The primary endpoint was achieved when at least 80% of treated versus control flanks and pre- versus post-treatment photographs were correctly identified by the blinded reviewers.
Subjects assessed treatment comfort using a numerical pain scale (0 = no pain to 10). Investigator satisfaction assessment comparing before and after images was also reported, using a 5-point Likert Scale at 4 weeks, 8 weeks, and 16 weeks follow-up versus baseline for the treated flank.
Results
A total of 46 subjects (8 males, 38 females), with mean age 45 ± 10 years, Fitzpatrick Skin Types II–V and body mass index of 25 ± 2 (range 22–29), completed the three ultrasound treatments and were evaluated at follow-up clinic visits. In the study cohort, 45 flank pairs were available for blinded evaluation. One subject had poor-quality photographs that were not included in the evaluation. However, the subject did experience fat reduction measured by skin caliper and ultrasound imaging and data was included in the secondary endpoint analysis.
Treatment parameters included mean focal treatment zones of 2.7 ± 1 (range 1 to 6), as well as treatment durations of 18 ± 8, 15 ± 7, and 16 ± 10 min for the first, second, and third treatments, respectively.
Blinded evaluation results
For the primary endpoint, the post-treatment flank photos were correctly identified by the blinded investigators in 82% (37/45) of evaluations and the treated flank side for 93% (42/45) of evaluations. Correct identification of both the pre-/post-treatment photographs, as well as the treated/un-treated flanks, showed an 80% (36/45) success rate. An example of correct identification of baseline photo and treated flanks is shown in and .
Figure 1. (a) 33-year-old female subject with baseline BMI of 29. (b) 16-week follow-up: subject’s left flank was treated and correctly identified by both blinded reviewers. Subject reported on the 5-point Likert Scale that she was very satisfied with treatment outcome and that the results were highly visible.

Figure 2. (a) 53-year-old female subject with baseline BMI of 22. (b) 16-week follow-up: subject’s left flank was treated and correctly identified by both blinded reviewers. Subject reported on the 5-point Likert Scale that she was neutral with treatment outcome and that the results were slightly visible.

Secondary objectives
Study subjects showed minimal weight change throughout the study (averaging less than 0.41%). As measured on ultrasound imaging, absolute fat thickness reduction following ultrasound treatment compared to baseline was statistically significant (p < 0.05, t-test) before the third treatment and at all follow-up evaluations, with a mean reduction of 2.2 mm at the 16-week follow-up. Ultrasound imaging measurements of treated flanks are shown in and . In contrast, fat reduction of the untreated flank (control) compared to baseline was not significant at any evaluation assessment (p > 0.05). Fat thickness reduction for the treated flanks was also statistically significantly greater than the results for the untreated flanks at all evaluations (p < 0.05), reaching a high level of significance (p < 0.001) at the 16-week follow-up.
Figure 3. (a) Ultrasound image for 33-year-old female subject () prior to treatment. (b) 16-week follow-up: measurement showed 4.2 mm reduction (from 13.8 mm at baseline to 9.6 mm at follow-up).
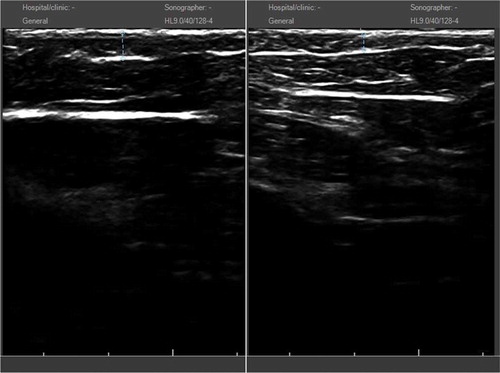
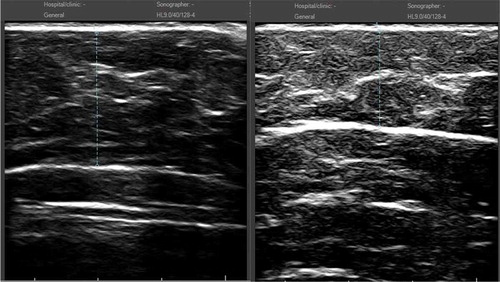
Figure 4. (a) Ultrasound image for 53-year-old female subject () prior to treatment. (b) 16-week follow-up: measurement showed 7.0 mm reduction (from 21.2 mm at baseline to 14.2 mm at follow-up).
As measured by skin caliper, fat thickness reduction of the treated flank also tended to be consistently greater compared to the control flank at each follow-up visit, reaching statistical significance in absolute fat thickness reduction at the 16-week follow-up.
At the 4-week follow-up, investigator satisfaction measured 70%. Subsequent results reflected lower satisfaction with increasing time from treatment (53% at 8 weeks follow-up, 43% at 16 weeks follow-up). Similarly, subject satisfaction decreased with time.
Ultrasound treatment to the flanks was accompanied by little or no discomfort, with subjects reporting a mean pain level of 0.38 ± 0.84 out of 10 (range 0–6) over all treatments. Data showed that 98% of treatments were associated with no to minimal discomfort. There were no treatment complications, and immediate responses of erythema and edema were mild and transient in nature, completely resolving within days without any intervention.
Discussion
There are several different technologies currently available in aesthetic medicine specifically engineered to non-invasively remove unwanted subcutaneous adipose tissue with the purpose of achieving an improved body shape and contour. Focused ultrasound technology was developed to be a non-thermal method to selectively destroy fat cells beneath the skin without surgery, discomfort or downtime. The outcomes of this multicenter clinical study demonstrated significant results, a favorable safety profile and subject tolerability with focused ultrasound treatment for fat reduction of the flanks.
We present the results of a multicenter, randomized, controlled clinical study in which 46 healthy male and female subjects were treated with focused ultrasound for fat reduction in a randomized flank compared with the untreated contralateral flank. Success criteria included the correct identification of the post-treatment photo and treated flank at the 16-week follow-up visit in at least 80% of evaluated images as assessed by two blinded evaluators (primary endpoint), as well as measureable fat thickness reduction in the treated areas (secondary endpoint). The study success criterion was met with 80% (36/45) of evaluations correctly identified by the blinded investigators.
Subjects demonstrated significant fat reduction in their treated area, as measured by ultrasound and skin caliper. At each of the follow-up visits, the fat thickness reduction in the treated flank was statistically significantly greater compared to baseline pre-treatment measurements by ultrasound imaging. Interestingly, although fat reduction in the treated flank increased with treatment and time, with best results observed at the 16-week follow-up, investigator and subject satisfaction decreased with time. This aspect of clinical outcome warrants further study and a better understanding of patient expectations. The controlled study design included an untreated control. In clinical practice, both flanks, as well as the abdomen, would likely be treated, resulting in improved clinical outcome and higher patient satisfaction.
Treatments were found to be very well tolerated by study subjects, with 98% of flank treatments associated with none to minimal discomfort. These results were further reflected in the mean pain level scores of 0.38 ± 0.84 out of 10 for treated flanks. None of the study subjects experienced complications with treatments, and the only immediate responses observed were mild erythema and edema that were transient in nature, completely resolving within days without any intervention.
There are several limitations with the study that should be noted. Ultrasound imaging is user-dependent on the force applied to the ultrasound transducer. Applying pressure to the transducer will result in a decreased fat layer measurement. This was addressed in the study by detailed training and instructing the operators to apply minimal pressure to the transducer. Two repeated measurements were taken at each flank area and then averaged. Additionally, due to the study design, the contralateral flank was left untreated, so circumference measurements were not available for comparison with baseline. Finally, it is difficult to visualize improvement on photography with just the one flank treated. Treatment outcomes to a larger area to include the abdomen or both flanks are more visible to the patient and on clinical photographs.
Pulsed, focused non-thermal ultrasound treatment has demonstrated non-invasive fat reduction, leading to improvements in body contour, as reported in several previous clinical studies (Citation7,Citation13–Citation18). A recent multicenter, randomized, controlled clinical study (Citation18) similarly demonstrated significant circumference reduction in the abdomen. In that study, 150 healthy male and female patients presenting with excess subcutaneous fat deposits in the abdominal region were randomly assigned to Group 1 for a 4-week control phase before undergoing three abdominal ultrasound treatments, at 2-week intervals, or to Group 2 for immediate treatment. Data collection included patient’s weight, abdominal circumference, treatment tolerability, and patient satisfaction, as well as adverse event reporting. Results showed that the average reduction in the midline circumference was 2.5 ± 2.1 cm in Group 1 and 3.5 ± 2.7 cm in Group 2 in the final follow-up visit at Week 22. In addition, the effect of multiple treatments was found to be cumulative, as a trend for a steady decrease in abdominal circumferences throughout the study was seen. The authors suggest that successive focused ultrasound treatments can significantly reduce treatment area circumference, while providing the patient with a comfortable, non-invasive treatment option.
Novel treatment techniques and technologies that can noninvasively address the excess and unwanted subcutaneous fat deposits have become very popular in the aesthetic field, with each modality having a varying efficacy, efficiency, and safety. Ultrasound has become a cornerstone modality in medicine and is widely used for diagnostic, as well as therapeutic applications. Therapeutic ultrasound is known to induce a vast range of biological effects at very different acoustic parameters. While low levels of ultrasound can produce beneficial but reversible cellular effects, higher levels (such as high-intensity focused ultrasound) can cause instantaneous cell necrosis. Most therapeutic ultrasound-based devices use heating to achieve a desired effect. In contrast, pulsed, focused ultrasound technology achieves its intended effect of adipocyte destruction in a non-thermal fashion. The non-thermal focused ultrasound technology results in the destruction of adipocytes via cavitation or mechanical acoustic effect, while controlling the temperature elevation (less than 0.5°C increase) in the targeted tissues. Therefore, typical side effects associated with thermal-based devices such as pain, dysesthesia, bruising, swelling, and downtime are not commonly associated with focused ultrasound treatment.
In conclusion, a series of three ultrasound treatments resulted in significant fat reduction in treated flanks compared to untreated controls. Treatments were reported as comfortable, and with no treatment complications. Although results are more modest than with liposuction, non-invasive ultrasound treatment may provide an attractive alternative to patients seeking an in-office, non-surgical procedure for fat reduction.
Additional information
Funding
References
- Arner P. Regional adipocity in man. J Endocrinol. 1997;155:191–92. doi:10.1677/joe.0.1550191.
- Flynn TC, Coleman WP III, Field LM, Klein JA, Hanke CW. History of liposuction. Dermatol Surg. 2000;26:515–20. doi:10.1046/j.1524-4725.2000.00066.x.
- Hanke W, Cox SE, Kuznets N, Coleman WP III, Tumescent liposuction report performance measurement initiative: national survey results. Dermatol Surg 2004; 30:967–77.
- Adamo C, Mazzocchi M, Rossi A, Scuderi N. Ultrasonic liposculpturing, extrapolations from the analysis of in vivo sonicated adipose tissue. Plast Reconstr Surg. 1997;100:220–26.
- Goldman A. Submental Nd: YAG Laser-assisted liposuction. Lasers Surg Med. 2006;38:181–84. doi:10.1002/(ISSN)1096-9101.
- Hexsel D, Serra M, Mazzuco R, Dal’Forno T, Zechmeister D. Phosphatidylcholine in the treatment of localized fat. J Drugs Dermatol. 2003;2;511–18.
- Moreno-Moraga J, Valero-Altés T, Riquelme AM, Isarria-Marcosy MI, de la Torre JR. Body contouring by noninvasive transdermal focused ultrasound. Lasers Surg Med. 2007;39:315–23. doi:10.1002/(ISSN)1096-9101.
- Weiss RA. Noninvasive radiofrequency for skin tightening and body contouring. Semin Cutan Med Surg. 2013;32:9–17.
- Adatto MA, Adatto-Neilson RM, Morren G. Reduction in adipose tissue volume using a new high-power radiofrequency technology combined with infrared light and mechanical manipulation for body contouring. Lasers Med Sci. 2014;29:1627–31. doi:10.1007/s10103-014-1564-x.
- Brightman L, Weiss E, Chapas AM, Karen J, Hale E, Bernstein L, Geronemus RG. Improvement in arm and post-partum abdominal and flank subcutaneous fat deposits and skin laxity using a bipolar radiofrequency, infrared, vacuum and mechanical massage device. Lasers Surg Med. 2009;41:791–98. doi:10.1002/lsm.20872.
- Winter ML. Post-pregnancy body contouring using a combined radiofrequency, infrared light and tissue manipulation device. J Cosmet Laser Ther. 2009;11:229–35. doi:10.3109/14764170903134334.
- Brown SA, Greenbaum L, Shtukmaster S, Zadok Y, Ben-Ezra S, Kushkuley L. Characterization of nonthermal focused ultrasound for noninvasive selective fat cell disruption (lysis): Technical and preclinical assessment. Plast Reconstr Surg. 2009;124:92–101.
- Ascher B. Safety and efficacy of UltraShape Contour I treatments to improve the appearance of body contours: Multiple treatments in shorter intervals. Aesthet Surg J. 2010;30:217–24. doi:10.1177/1090820X09360692.
- Chang SL. Combination therapy of focused ultrasound and radiofrequency for noninvasive body contouring in Asians with MRI photographic documentation. Lasers Med Sci. 2014;29:165–72. doi:10.1007/s10103-013-1301-x.
- Coleman KM, Coleman WP 3rd, Benchetrit A. Noninvasive, external ultrasonic lipolysis. Semin Cut Med Surg. 2009;28:263–67. doi:10.1016/j.sder.2009.10.004.
- Teitelbaum SA, Burns JL, Kubota J, Matsuda H, Otto MJ, Shirakabe Y, Suzuki Y, Brown SA. Noninvasive body contouring by focused ultrasound: Safety and efficacy of the contour I device in a multicenter, controlled, clinical study. Plast Reconstr Surg. 2007;120:779–89.
- Hota TA. Nonsurgical body contouring with focused ultrasound. Plast Surg Nurs. 2010;30:77–82.
- Coleman, 3rd WP, Coleman W 4th, Weiss RA, Kenkel JM, Ad-El DD, Amir R. A multicenter controlled study to evaluate multiple treatments with nonthermal focused ultrasound for noninvasive fat reduction. Dermatol Surg. 2017;43:50–57.
