ABSTRACT
Striae distensae (SD) are linear scar tissue in the dermis that arises from stretching the skin. There are two types of SD, striae rubrae and striae albae (SA) which is marked with a line hypopigmentation that cause a psychological problem, especially in the high skin type. The standard therapy is a 0.1% tretinoin cream, but it takes a long time to reach the collagen so it needs invasive measures to reach these targets. This study was comparing 0.1% tretinoin cream with combination therapy of fractional microneedle radiofrequency (FMR) and fractional CO2 laser for SA. The number of subjects in this study was 11 patients each group with Fitzpatrick skin types IV or V. Biopsy was taken before and after therapy. The clinical changes in SA lesions in this study were represented by measurements of the length and width. The percentage of collagen area is the amount of collagen fibers with Masson’s trichrome staining. The clinical changes of lesion in the combination therapy decreased. The percentage change in collagen area in the combination therapy group had a higher increase. The side effect experienced by all combination group subjects was postinflammatory hyperpigmentation, two subjects in 0.1% tretinoin cream group experienced irritation.
KEYWORDS:
Introduction
Striae distensae (SD) or stretch marks are linear scar tissue in the dermis that arises from stretching the skin beyond its elastic limit on weak connective tissue (Citation1). There are two types of SD, namely striae rubrae (SR) which is the initial phase and is marked by an erythematous line and striae albae (SA) which is marked with a line hypopigmentation, while the epidermis and dermis atrophy. The most common locations for SD include the stomach, breasts, upper arms, buttocks and thighs (Citation1,Citation2). Striae distensae prevalence is up to 88% in all races. Striae distensae is a skin condition that can cause significant distress and can become a psychological problem, especially for someone with a profession such as a model or actress and in the darker skin type, so that it can hinder work or social life. Stretching that occurs in the epidermis and dermis in SD which is characterized by atrophy can interfere the function of the skin barrier and even disrupt transepidermal water loss [Citation2,Citation3]. Although the causes for the emergence of SD are still not known with certainty, there are several theories explaining the causes and risk factors for SD. Causes of SD include rapid weight change, adolescent puberty growth, local and systemic use of corticosteroids, and Cushing’s syndrome (Citation2, Citation4). Rapid stretching of the skin that exceeds the elasticity limit results in mechanical stress and inflammation which causes an increase in proteolytic enzymes which results in decreased fibroblast activity and extracellular matrix (ECM) components, this affects the matrix in the dermis and results in reduced collagen and SD formation (Citation5,Citation6).
There are several SD therapy options that have had various results. Different modalities work with different targets. There are target modalities that serve to increase collagen in SD, increase melanin and reduce vascularity (Citation5). The standard therapy is a tretinoin 0,1% cream applied to the lesion and is a collagen-targeted therapy, but it takes a long time to reach the collagen target located in the dermis so it needs invasive measures to reach these targets (Citation1,Citation2).
Fractional microneedle radiofrequency (FMR) is a minimally invasive method that uses heat energy from rapidly penetrating microneedles to the target tissue (Citation7). After the damage reaches the reticular dermis layer, there will be a long-term dermal remodeling process, neoelastogenesis, and neocolagenesis along with the skin thickening process, so the use of FMR is currently being developed for SD therapy. The way FMR works is using microneedle penetration on a stamp or roller into the skin as deep as 0.5–2 mm. The small wound caused by the penetration of the microneedle will immediately close and can stimulate the wound healing process and the proliferation of fibroblasts and collagen production (Citation7,Citation8).
The CO2 laser technique has long been used for skin rejuvenation [Citation8, Citation9]. The laser uses a wavelength of 10,600 nm and generates heat which has a collagen denaturation effect. Currently, fractional CO2 laser therapy has been developed which is classified as safer because it is equipped with a system that will produce thermal damage to the micro-colum tissue around healthy tissue [Citation9,Citation10,Citation11,Citation12]. Fractional CO2 laser is often used for skin rejuvenation, scar acne and non-acne, as well as SD and gives satisfactory results [Citation7,Citation9]. The use of combination therapy with FMR and fractional CO2 laser resulted in an increase in the percentage of collagen area in the dermis layer due to increased expression of TGF-β1 and stratifin. Stratifin is an extracellular matrix modulating factor in dermal fibroblasts that induces matrix metalloproteinase-1 expression and activity of dermal fibroblasts which causes dermal remodeling. Stratifin also plays a role in epidermal interactions through the basal and mesenchymal stratum so that it will help the epidermal remodeling process and there will be thickening of the atrophic epidermal layer (Citation7). The aim of this study is to compare 0.1% tretinoin cream with combination therapy of fractional microneedle radiofrequency (FMR) and fractional CO2 laser for SA. Evaluation of this study by clinically and histopathology to know the collagen percentage.
Materials and methods
This study is an analytical experimental study using a randomized clinical trial method comparing 0.1% tretinoin cream with combination therapy of FMR and fractional CO2 laser in patients with striae albae in Dermatology and Venereology outpatient clinic, Dr. Soetomo general academic hospital, Surabaya, Indonesia. The number of subjects in this study was 11 patients each group and the inclusion criterias were female patients aged 14–60 years with striae albae at the stomach location with skin types Fitzpatrick IV or V, the general condition of the patient is good, willing to participate in the study and sign the informed consent. While the exclusion criteria were patients who had a history of keloids, patients with skin infections, diabetes mellitus, pregnant and breastfeeding, patients with systemic disease requiring immunosuppressive therapy, patients who have received topical retinoid therapy, laser and other SD therapy modalities within the last 3 months.
Biopsy was taken from the lesion area using a 4 mm punch biopsy. Prior to the biopsy, local anesthesia was performed first. Biopsy was performed 2 times, before and after therapy. Location of initial and final biopsy in the same lesion. Tretinoin is a vitamin A derivative that is thought to work through affinity fibroblasts and induction of collagen synthesis. This therapy is a standard therapy for SD given at Dr. Soetomo general academic hospital, Surabaya, Indonesia. The 0.1% tretinoin cream was applied to SA lesions once a day at night during 12 weeks. This study used fraxis duo ilooda FMR pass I: with a microneedle penetration depth of 2.5 mm, 40% intensity, 150 ms radiofrequency duration, pass II: with a microneedle penetration depth of 2 mm, 30% intensity, 150 ms radiofrequency duration. While the fractional CO2 laser fluence is 4.5 mJ, stack 3, distance is 0.7 mm. This study used a fluence 4.5 mJ fractional CO2 laser aimed at repairing epidermal damage, with the hope of minimizing the risk of Post Inflammatory Pigment Alteration (PIPA) side effects.
Initially the area to be performed action was cleaned with an alcohol swab, the patient was given topical anesthesia for 60 minutes. After 60 minutes, the area that would be given laser treatment was cleaned from topical anesthetic cream using gauze. The patient’s eyes were closed using dark glasses. Operators washed their hands and used gloves and face mask. After the duo fraxis has been prepared, FMR action can be started, after which the bleeding area can be cleaned using gauze, in the combined FMR and fractional CO2 laser treatment group, it can be continued with fractional CO2 laser work. The lesions were compressed with gauze and physiological NaCl for 10–20 minutes, then topical antibiotics were applied to the lesions. Each therapy was carried out 3 times with interval of 4 weeks, after 4 weeks from the last therapy a second biopsy was performed.
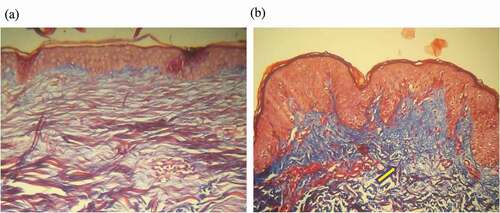
The clinical changes in SA lesions in this study were represented by measurements of the length and width of the SA lesions. These measurements were carried out by taking a photograph of the SA lesion before and after therapy, then one of the SA lesions on the photo was measured in length and width by drawing a straight line along the lesion using Image Meter software version 2.15.0. The software will measure the SA size digitally so that it will produce accurate numbers. The percentage of collagen area is the amount of collagen fibers from three fields of view of SD histopathological preparations with Masson’s trichrome staining through light microscopy with 10 times ocular enlargement and 10 times objective magnification. The collagen count is carried out using 100 squares measuring 20 × 20 μm. Each square is evaluated for collagen content in percentage units, then added together to produce the area of collagen in percentage units. Staining Masson’s trichrome will produce blue which indicates collagen, red which indicates muscle tissue and other connective tissue, while black color indicates the cell nucleus.
Results
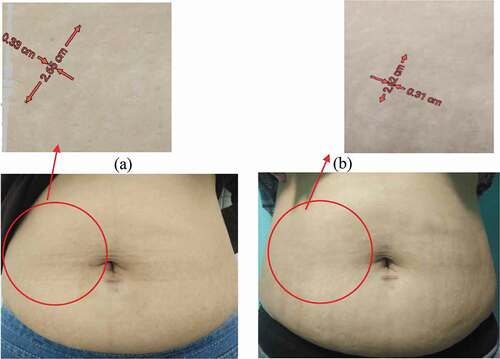
Eleven subjects each group were female patients, who met inclusion criteria were selected consecutively and enrolled this study. Subjects were 14–60 years with skin types Fitzpatrick IV or V. All subjects were informed about the study protocol and signed consent. All subjects had SA lesion in the stomach, clinical lesion was evaluated for the length and width as observed in . Baseline length and width in the 0.1% tretinoin cream group were 67.1 ± 41.2 cm and 5.2 ± 0.8 cm (mean ± SD) while in the FMR + fractional CO2 laser group were 45.0 ± 26.3 cm and 4.7 ± 2.0 (mean ± SD). The percentage of collagen area was evaluated histologically. Baseline collagen area in the 0.1% tretinoin cream group was 32.4 ± 7.5% (mean ± SD) and in the FMR + fractional CO2 laser group was 41.2 ± 8.8% (mean ± SD). The first evaluation was done before therapy. Later evaluation was after 4 weeks from the last therapy.
Table 1. Baseline characteristic
The clinical lesion that evaluated by length and width of the SA lesion in 0.1% tretinoin cream group showed no significant difference before and after therapy (p = .341) as seen in the . The length of SA lesions pre and post therapy in the combination FMR + Fractional CO2 laser group showed a decrease, but the difference was not significant (p = .075). Changes in the width of SA lesions in FMR + Fractional CO2 laser group showed a significant difference (p = .001) (). Percentage of collagen area also observed histologically and showed a significant difference between the percentage of collagen area pre and post therapy in each group. The tretinoin 0,1% cream group obtained p value 0.0001, as well as the FMR + Fractional CO2 laser group obtained p value < .0001 (). There was a significant difference in the change of the percentage of collagen area (%) between groups (p = .019).
Table 2. Comparison before and after therapy
Each group was evaluated for the side effects of each therapy. All subjects who received combination therapy FMR + Fractional CO2 laser obtained side effects of PIH (Post Inflammatory Hyperpigmentation) as many as 11 subjects in each group. In the 0.1% tretinoin cream group, 2 subjects experienced the irritation side effect that can be quickly relieved by topical steroid administration.
Discussion
The age of the study participants was determined to be in the range of 14–60 years, not younger than 14 years of age because it was feared that patients would not be able to work together for long research procedures in the form of skin biopsy and FMR + fractional CO2 laser procedures, not older than 60 years due to invasive procedures, it is feared that this study can affect the general condition of the patient. The age ranges were also selected according to WHO adult criteria (Citation13). The average age of the subjects in this study was 36 years. Crocco et al cited a complaint Striae alba can occur at any age, with the highest incidence between the ages of 23–49 years (Citation14).
The length and width of the SA lesion were examined as one of the basis for the evaluation of therapy measured before and after therapy. The width and the length of the SA lesions in the 0.1% tretinoin cream group showed a not significant difference between the pre and post therapy (). This is because tretinoin takes longer time to penetrates deep into the skin and requires a routine in applying to skin every day, so that in the single therapy 0.1% tretinoin cream takes a minimum of 6 months to produce clinical changes (Citation15–17). The length of SA lesions pre and post therapy in the combination therapy FMR + Fractional CO2 laser group showed a decrease, but the difference was not significant () meanwhile the width changes was significantly different the length and width of SA lesions before and after therapy were significantly different between groups with p < 0,0001. Changes in both the length and width of the SA lesion show varying results, but the size of the SA lesion has decreased in combination therapy of FMR + Fractional CO2 laser, according to the study of Naeini et al. [Citation9]. the changes obtained from invasive therapy resulted from the heat given during invasive therapy, causing a remodeling of the resulting wound [Citation9,Citation15, Citation18–20].
Figure 1. Clinical SA lesions in study subjects in 0.1% tretinoin single-therapy, pre-therapy (A) and post-therapy (B)
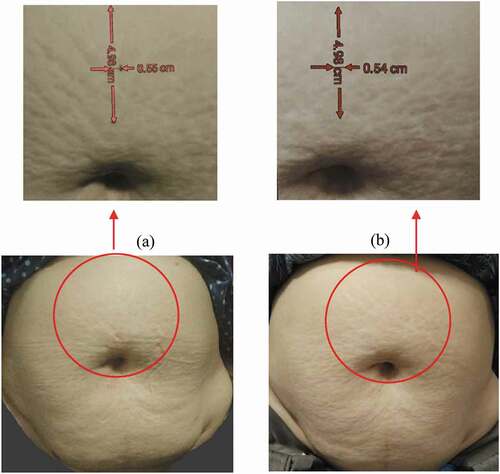
Figure 2. Clinical SA lesions in study subjects in the combination therapy group FMR + fractional CO2 laser, pre therapy (A) and post therapy (B)
Changes in the percentage of collagen area before (pre) and after (post) showed a significant difference between pre and post therapy in each group ( and ). An increase in collagen is also obtained in the 0.1% tretinoin cream after 3 months of therapy, that is faster than previous studies that took time minimum of 6 months (Citation15, Citation21). This is also in accordance with the research of Ryu et al, who conducted a study on patients with striae distensae using FMR and fractional CO2 laser, there was an increase in collagen in SA lesions after research subjects received 3x FMR and fractional CO2 laser therapy (Citation7). Data on differences in changes in the percentage of collagen area (%) results showed a significant difference in changes in the percentage of collagen area (%) between groups (p = .019).
Figure 3. Histopathology of the percentage area of collagen (100x magnification) in the study subjects in the 0.1% tretinoin cream group, pre therapy (A) and post therapy (B). Yellow arrows indicate an increase in the amount of collagen
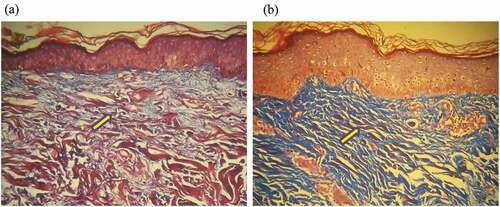
Figure 4. Histopathology of the percentage area of collagen (100x magnification) in the study subjects in the combination therapy group FMR + fractional CO2 laser, pre therapy (A) and post therapy (B). Yellow arrows indicate an increase in the amount of collagen
All subjects who received combination therapy FMR + Fractional CO2 laser obtained side effects of PIH as many as 11 subjects in each group while in the 0.1% tretinoin cream group, there were 2 subjects who experienced irritation that can be quickly resolved by topical steroids. In accordance with the study of Ryu et al., The side effects of patients in the combination FMR and fractional CO2 group were PIH. The PIH results from an inflammatory process caused by heat energy supplied by either the FMR or the fractional CO2 laser. Patients with fitzpatrick skin types IV, V have a greater risk of developing PIH than fitzpatrick skin types I and II (Citation7).
Conclusion
Length and width of SA lesions in the 0.1% tretinoin cream group did not decrease significantly, meanwhile the percentage of collagen area experienced a significant increase. The length of the SA lesion in the combination FMR and Fractional CO2 laser group did not decrease significantly, but the width of the SA lesion decreased significantly. The percentage of collagen area in both group experienced a significant increase. The percentage change in collagen area in the combination FMR and fractional CO2 laser therapy group had a higher increase than the increase in collagen in the 0.1% tretinoin cream monotherapy group. The side effect experienced by all subjects in the combination FMR and fractional CO2 laser group was PIH, meanwhile in the 0.1% tretinoin single therapy group only 2 subjects who experience irritation side effects. The CO2 fractional laser action in this study is aimed at repairing the epidermis. Both treatments can significantly increase collagen (Citation9, Citation22).
Acknowledgments
There’s nothing to declare.
References
- Ud-Din S, McGeorge D, Bayat A. Topical management of striae distensae (stretch marks): prevention and therapy of striae rubrae and albae. JEADV. 2016;30:211–22.
- J-orh R, Titapant V, Chuenwattana P, Tontisirin P.Prevalence and associate factors for striae gravidarum. J Med Assoc Thai. 2008;91(4):445–51.
- Farahnik B, Park K, Kroumpouzos G, Murase J.Striae gravidarum: risk factors, prevention, and management. International Journal of Women’s Dermatology. 2017;3(2):77–85.doi:https://doi.org/10.1016/j.ijwd.2016.11.001.
- Lisa R, Henk H, Ali P, Filip S, Stan M.Microneedling: where do we stand now? a systematic review of the literature. J Plast Reconstr Aesthet Surg. 2017;6815(17):30250–54.
- Hague A, Bayat A.Therapeutic targets in the management of striae distensae: a systematic review. J Am Acad Dermatol. 2017;77(3):559–68.doi:https://doi.org/10.1016/j.jaad.2017.02.048.
- Naeini FF, Behfar S, Naeini BA, Keyvan S, Pourazizi M. Promising option for treatment of striae alba: fractionated microneedle radiofrequency in combination with fractional carbon dioxide laser. Dermatology Research and Practice. 2016;2016:1–7.doi:https://doi.org/10.1155/2016/2896345.
- Ryu HW, Kim SA, Jung HR, Ryoo YW, Lee KS, Cho JW. Clinical improvement of striae distensae in korean patients using a combination of fractionated microneedle radiofrequency and fractional carbon dioxide laser. Dermatol Surg. 2013;11(12): 12108–17.
- Khater MH, Khattab FM, Abdelhaleem MR.Treatment of striae distensae with needling therapy versus CO2 fractional laser. J Cosmet Laser Ther. 2016;18(2):75–79.doi:https://doi.org/10.3109/14764172.2015.1063665.
- Naeini FF, Nikyar Z, Mokhtari F, Bahrami A. Comparison of the fractional CO2 laser and the combined use of a pulsed dye laser with fractional CO2 laser in striae alba treatment. Adv Biomed Res 2014;3:184–6.
- Gonzales DFM, Navalta JTP. The efficacy and safety of fractional ablative resurfacing using 10,600nm CO2 pulse wave in the treatment of striae distensae among filipino women with skin types III-V, a preliminary investigation and initial results. Am J Clin Dermatol. 2012;19(3):405–23.
- Naeini FF, Soghrati M. Fractional CO2 laser as an effective modality in treatment of striae alba in skin types III and IV. J Res Med Sci. 2012;17(10):928–33.
- Yang YJ, Lee GY. Treatment of striae distensae with nonablative fractional laser versus ablative CO2 fractional laser: a randomized controlled trial. Ann Dermatol. 2011;23(4):481–9.
- World Health Organization. (2011) International statistical classification of diseases and related health problems 10th revision. 4th ed. Geneva: WHO Press.
- Crocco EI, Mantovani PA, Volpini BMF. In search of treatments for striae rubra and striae alba: a dermatologists’ challenge. Surg Cosmet Dermatol. 2012;4(4):332–7.
- Al-Himdani S, Ud-Din S, Gilmore S, Bayat A.Striae distensae: a comprehensive review and evidence-based evaluation of prophylaxis and treatment. British Journal of Dermatology. 2014;170(3):527–47.doi:https://doi.org/10.1111/bjd.12681.
- Bogdan C, Iurian S, Tomuta I, Moldovan M. Improvement of skin condition in striae distensae: development, characterization and clinical efficacy of a cosmetic product containing Punica granatum seed oil and Croton lechleri resin extract. Drug Des Devel Ther. 2017;11:521–31.doi:https://doi.org/10.2147/DDDT.S128470.
- Moore J, Kelsberg G, Safranek S.Do any topical agents help prevent or reduce stretch marks? J Fam Practice. 2012;12(61):757–58.
- El-Khalafawy GMK. Comparative study between intense pulsed light “IPL” and pulsed dye laser in the treatment of striae distensae. J Cutan Laser Ther. 1. 2013;95–100.
- El Taieb MA, Ibrahim AK.Fractional CO2 laser versus intense pulsed light in treating striae distensae. Indian J Dermatol. 2016;61(2):174–80.doi:https://doi.org/10.4103/0019-5154.177774.
- Liu L, Ma H, Li Y.Interventions for the treatment of stretch marks: a systematic review. Cutis. 2014;94(2):66–72.
- Lung PW, Tippavajhala VK, de Oliveira Mendes T, Téllez-Soto CA, Schuck DC, Brohem CA, Lorencini M, Martin AA. Lasers Med Sci. 2018;33(3):609–17. Epub 2018 Jan 7. doi:https://doi.org/10.1007/s10103-017-2431-3.PMID: 29308552
- Ud-Din S, Bayat A.New insights on keloids, hypertrophic scars, and striae. Dermatologic Clinics. 2014;32(2):193–209.doi:https://doi.org/10.1016/j.det.2013.11.002.
