ABSTRACT
The photothermal effect of lasers is minimized and the photoacoustic effect is maximized as the pulse duration is shortened. Therefore, picosecond lasers with a short pulse and high peak power can be used to effectively treat various pigment disorders by reducing tissue damage. The first picosecond lasers were used for tattoo removal; they are also widely used for pigment treatment because of their reduced side effects compared with nanosecond lasers. Recently, picosecond lasers have been shown to be effective in the treatment of various skin conditions such as acne scars and large pores. There are many studies on picosecond lasers; however, there are no studies on a laser with a pulse duration of 300 ps. This report describes the use of a 300 ps Nd:YAG laser for treating pigment disorders and for skin rejuvenation in four Asians, with no side effects. Determining the clinical significance of the 300 ps pulse duration through comparative studies with various picosecond lasers is needed.
Introduction
In selective photothermolysis, lasers of specific wavelengths are used to achieve deep penetration and are absorbed selectively by a target chromophore. This process aims to treat skin lesions by rapidly, efficiently, and selectively dissolving the target chromophore while minimizing damage to the surrounding tissues. Therefore, the pulse duration of the laser should be shorter than the thermal relaxation time of the target chromophore to allow the effective destruction of the target while minimizing damage to the surrounding normal tissues (Citation1,Citation2).
Nanosecond domain Q-switched lasers have been widely used in tattoo removal and for treating various pigment disorders (Citation3). Picosecond lasers can reduce the side effects of epidermal damage and pigmentation because of their shorter pulse duration compared to nanosecond lasers (Citation4). Moreover, hyperpigmentation occurs frequently in the treatment of pigmentation disorders in Asian patients with dark skin. The use of picosecond laser has a lower risk of post-inflammatory hyperpigmentation than Q-switched laser and is therefore safer and more effective (Citation5). The reason is that the picosecond laser has a short pulse duration and high peak power; it has a higher photomechanical and lower photothermal effects, minimizing the tissue damage caused by heat (Citation6). The photomechanical effect is the primary effect of a picosecond laser on a target chromophore which successfully destroys tattoo particles. Essentially, a picosecond laser minimizes thermal damage, which leads to reduced side effects (Citation3,Citation7).
Initially, picosecond lasers were used for tattoo removal to provide better treatment results and reduce side effects compared to nanosecond lasers but, recently, they have also been effectively used to treat various pigment disorders, acne scars, and wrinkles (Citation8).
Currently, picosecond lasers commonly used in dermatology have a pulse duration of 300–900 ps (Citation9). A shorter pulse duration can reduce side effects and downtime, but there are no clinical cases reporting the use of lasers with a pulse duration of 300 ps. This study aimed to confirm whether a laser with a pulse duration of 300 ps is effective in treating skin lesions treated using other picosecond lasers. We report an effective treatment using a 1,064-nm neodymium-doped yttrium aluminum garnet (Nd:YAG) laser with a 300 ps pulse duration in four cases, including three types of pigment disorders and one type of skin rejuvenation, involving Asian patients.
Case presentation
Case 1
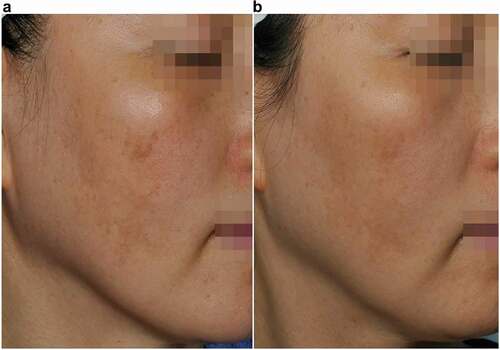
A 47-year-old man visited our clinic with complaints of dark-brown/black-colored, well-demarcated pigmented patches on both cheeks (). The patient had received intense pulsed light therapy and laser toning; but the treatment proved ineffective as the patches worsened. The pigmented lesions were visually diagnosed with the aid of a wood lamp (320–400 nm ultraviolet light, Cho Yang Medics, Co. LTD., Seongnam, Korea) as post-inflammatory hyperpigmentation (PIH) secondary to intense pulsed light therapy.
Figure 1. Case 1: A 47-year-old man with post-inflammatory hyperpigmentation (right-side view). (a) Before treatment, (b) After treatment.
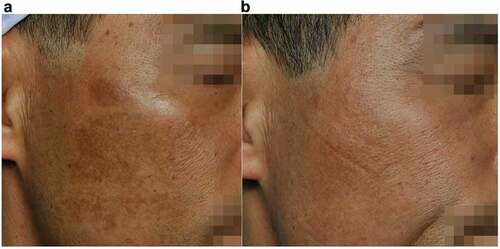
Figure 2. Case 1: A 47-year-old man with post-inflammatory hyperpigmentation (left-side view). (a) Before treatment, (b) After treatment.

The patient underwent 1,064-nm picosecond Nd:YAG laser treatment. Without administering any topical anesthetics, using a PICOHI device (Hironic Corp., Yongin, Korea), several pulses of a 1,064-nm Nd:YAG picosecond laser were administered to the pigmented lesions, with a spot size of 10 mm (collimated handpiece), fluence of 0.3 J/cm2, and pulse rate of 10 Hz until mild erythema appeared. The patient received this treatment a total of 8 times at 2 week intervals. Immediately after the procedure, the treated area was cooled with ice packs. No prophylactic antibiotics were prescribed. The patient received this treatment several times at intervals of 2 weeks. Moreover, Kligman’s formula, which is a combination of drugs that inhibit melanin synthesis (Melano cream, Dong-A ST Co., Seoul, Korea) and a topical corticosteroid cream (Titibe cream, Hanmi Pharmaceutical Co., Ltd., Seoul, Korea), was applied twice a day (day and night) for a period of 3 months. The patient was advised to avoid excessive exposure to sunlight and to apply sunscreen throughout the treatment period. The patient’s PIH lesions had almost disappeared without notable side effects ().
Case 2
A 30-year-old woman visited our clinic with complaints of brown-colored pigmented spots on both cheeks and the nose (). She had never been treated with any topical medications, laser, or light devices. The pigment disorders were diagnosed as combined pigmentary lesions of acquired bilateral nevus of Ota-like macules (ABNOM) and lentigo. She underwent 1,064-nm Nd:YAG picosecond laser treatment. Without using any topical anesthetics, the 1,064-nm picosecond Nd:YAG laser, using a PICOHI device (Hironic Corp.), was delivered to the pigmented lesions.
Figure 3. Case 2: A 30-year-old woman with acquired bilateral nevus of Ota-like macules and lentigo. (a) Before treatment, (b) After treatment.
For the treatment of ABNOM lesions, the parameters were set at a spot size of 10 mm (collimate handpiece), fluence of 0.6 J/cm2, and pulse rate of 10 Hz, using the pulse stacking technique for 2–3 s. In the same session, lentigo lesion treatment was administered, and the parameters were set at a spot size of 10 mm (collimated handpiece), fluence of 0.3 J/cm2, and pulse rate of 10 Hz. Using the sliding and circular technique, the laser beam was repeatedly passed over the lesions until mild erythema appeared. She received this treatment every 2 weeks for a total of 12 treatments. Immediately after treatment, an ice pack was applied to cool the treatment area; systemic or topical corticosteroids and antibiotics were not prescribed. The patient was advised to avoid exposure to sunlight and to apply sunscreen during the treatment period. The treated ABNOM lesions and lentigo had almost disappeared after laser treatment ().
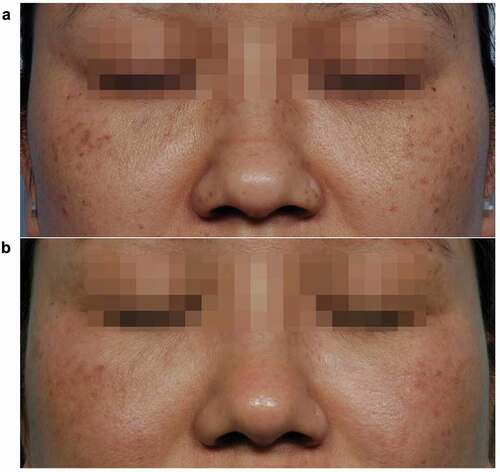
Case 3
A 38-year-old woman visited our clinic with complaints of light-brown-colored, poorly demarcated pigmented patches on both cheeks (). She had not received any treatment with topical agents or laser/light devices. After examining the pigmented lesions, we made a clinical diagnosis of melasma. The patient then underwent 1,064-nm picosecond Nd:YAG laser treatment. Without applying any topical anesthetics, using a PICOHI device (Hironic Corp.), several pulses of the 1,064-nm picosecond Nd:YAG laser were delivered to the pigmented lesions with the parameters set at a spot size of 10 mm (collimate handpiece), fluence of 0.3–0.4 J/cm2, and pulse rate of 10 Hz using a sliding and circular technique until mild erythema appeared. She underwent treatment every 2 weeks for a total of 12 treatments. Immediately after treatment, an ice pack was applied to cool the treated area; no prophylactic topical corticosteroids and antibiotics were prescribed. The patient was advised to avoid excessive exposure to sunlight and to apply broad-spectrum sunscreens during the treatment period. After laser treatment, the melasma became brighter without notable side effects ().
Case 4
A 27-year-old man visited our clinic with complaints of multiple depressed scars on both cheeks and temporal areas (). The patient had not received any treatment using laser/light devices. After examining the lesions, we diagnosed the patient with acne scars (ice pick and boxcar scars).
A topical anesthetic was applied, and using a PICOHI device (Hironic Corp.), the 1,064-nm picosecond Nd:YAG laser was delivered to the scar lesions, with a spot size of 13 mm (variable microlens array fractional handpiece), fluence of 0.20–0.25 J/cm2, and pulse rate of 10 Hz. For mild lesions, the sliding technique was used until erythema and petechia appeared, and for severe lesions, the stacking technique was used for 2–3 s. The treatments were performed at 2 to 3 week intervals depending on the patient’s condition for a total of 14 treatments. Immediately after treatment, an ice pack was applied to cool the treated area; prophylactic systemic or topical corticosteroids were not prescribed. To control the acne skin lesions, the patient was prescribed 200 mg of doxycycline daily for 1 month. The patient was advised to avoid excessive exposure to sunlight and to use broad-spectrum sunscreens during the treatment period. After laser treatment, the patient’s scars improved without notable side effects ().
Discussion
There are several reports regarding the clinical use of picosecond lasers, with pulse durations ranging from 450–750 ps (Citation3,Citation9). The current report is meaningful in that a laser with a shorter pulse duration (i.e., 300 ps) was used rather than a conventional picosecond laser. This study was initiated because although other picosecond lasers have been used for pigmented lesion treatment and skin regeneration, there are no case reports about similar effects when using a 300 ps laser for these purposes.
In four patients (three types of pigment disorders and one type of skin rejuvenation), a 300 ps pulse duration Nd:YAG laser was used for 4–8 months, and the clinical outcomes and side effects were assessed by comparing the images before and after treatment.
A comparison of the pictures taken before and after treatment showed improvement in the four clinical cases, and no side effects were noted. Although the 300 ps laser has a different pulse duration compared with the conventional picosecond laser, the results showed that it can be safely and effectively used for pigment disorders and skin rejuvenation treatment.
The first case was PIH, which was treated with laser toning for 4 months, and it was confirmed that the pigment area became bright (). For the treatment of PIH, nanosecond Q-switched ruby and Q-switched Nd:YAG lasers have been the most widely used (Citation10). Hydroquinone-containing topical therapy is routinely combined with lasers to treat pigmentation disorders as it improves clinical results and patient satisfaction compared to lasers treatment alone. In case 1, a topical agent was used to induce better results as hyperpigmentation had not improved with light-based treatment. Based on this, it is difficult to attribute the entirety of the result to the picosecond laser, as the effects of topical agent may have also played a role in the resolution of the patient’s PIH lesions. However, cases of successful PIH treatment using picosecond lasers have been reported; although further research is needed to clarify the effectiveness and natural healing potential after picosecond laser therapy, these lasers may be an effective treatment option for PIH (Citation11).
In the second case, ABNOM lesions with lentigo were treated using a 300 ps laser 12 times every 2 weeks, and the lesions improved and reduced in number (). When using picosecond lasers rather than traditional Q-switched lasers, better ABNOM treatment results with lower fluence, fewer treatments and complications, and shorter downtime have been obtained (Citation12).
In the third case (melasma), the dark color of the lesion was slightly improved by applying the laser treatment 10 times (). The greatest drawback of the photothermal effect caused by Q-switch lasers for melasma treatment is that PIH occurs after treatment. The picosecond laser may serve as a new treatment method for melasma using the photoacoustic mechanism (Citation13).
In the fourth case, a fractional beam of the microlens array method was used for acne scars. The photograph after 12 weeks of treatment showed that the depth of the scar was changed, and the area was narrowed (). The technology that allows the formation of new collagen based on the laser-induced optical breakdown principle enables safe skin rejuvenation with a short downtime without damaging the epidermis (Citation14). But Acne scars and acne-related hyperpigmentation may resolve with doxycycline treatment, as it reduces the occurrence of acne. In this case, of the laser treatment did have an effect on the patient’s scars; however, the doxycycline treatment may have played an adjuvant role.
Based on this study, it is not unreasonable to state that a laser with a pulse duration of 300 ps can be safely and effectively used to treat various skin lesions. Since the picosecond laser selectively reacts only to the target tissue, it is advantageous for the treatment of pigmentation disorders while minimizing damage to the surrounding normal tissue. In particular, the 300 ps laser used in this study has a lower photothermal effect than the 450–700 ps laser, so it is considered to be safer for Asian patients with dark skin as it reduces the amount of collateral thermal damage. However, it is difficult to assess the differences of the clinical results and/or side effects according to each picosecond lasers with different pulse durations. Comparative studies on picosecond lasers with different pulse durations under the same clinical conditions are required to clearly confirm the clinical significance of the 300 ps pulse duration.
In conclusion, 300 ps lasers can be safely and effectively used in the treatment of various skin lesions. To the best of our knowledge, this is the first report on the effective treatment of skin lesions using a picosecond laser with a pulse duration of 300 ps.
Ethical approval
The study follows the principles of the Declaration of Helsinki.
Informed consent
All the patients provided written informed consent for the publication of this report, including the images.
Data availability
Jiehoon Kim has full access to all the data related used in this study, but said data cannot be made publicly available for reasons of patient privacy.
Acknowledgments
The authors would like to thank Adonai (Editage, Seoul, Korea) for his help with the editing of this manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Anderson RR, Parrish JA. Selective photothermolysis: precise microsurgery by selective absorption of pulsed radiation. Science. 1983;220(4596):524–27. doi:https://doi.org/10.1126/science.6836297. Cited in: PMID: 6836297.
- Ho SG, Goh CL. Laser tattoo removal: a clinical update. J Cutan Aesthet Surg. 2015;8(1):9–15. doi:https://doi.org/10.4103/0974-2077.155066. Cited in: PMID: 25949017.
- Torbeck RL, Schilling L, Khorasani H, Dover JS, Arndt KA, Saedi N. Evolution of the picosecond laser: a review of literature. Dermatol Surg. 2019;45(2):183–94. doi:https://doi.org/10.1097/DSS.0000000000001697. Cited in: PMID: 30702447.
- Negishi K, Akita H, Matsunaga Y. Prospective study of removing solar lentigines in Asians using a novel dual-wavelength and dual-pulse width picosecond laser. Lasers Surg Med. 2018;50(8):851–58. doi:https://doi.org/10.1002/lsm.22820. Cited in: PMID: 29608215.
- Kung KY, Shek SY-N, Yeung CK, Chan HH. Evaluation of the safety and efficacy of the dual wavelength picosecond laser for the treatment of benign pigmented lesions in Asians. Lasers Surg Med. 2019;51(1):14–22. doi:https://doi.org/10.1002/lsm.23028. Cited in: PMID: 30357871.
- Ross V, Naseef G, Lin G, Kelly M, Michaud N, Flotte TJ, Raythen J, Anderson R. Comparison of responses of tattoos to picosecond and nanosecond Q-switched neodymium: YAG lasers. Arch Dermatol. 1998;134(2):167–71. doi:https://doi.org/10.1001/archderm.134.2.167. Cited in: PMID: 9487208.
- Ho DDM, London R, Zimmerman GB, Young DA. Laser-tattoo removal–a study of the mechanism and the optimal treatment strategy via computer simulations. Lasers Surg Med. 2002;30(5):389–97. doi:https://doi.org/10.1002/lsm.10065. Cited in: PMID: 12116333.
- Forbata E, Al-Niaimi F. The use of picosecond lasers beyond tattoos. J Cosmet Laser Ther. 2016;18(6):345–47. doi:https://doi.org/10.1080/14764172.2016.1188209. Cited in: PMID: 27183360.
- Douglas CW, Goldman MP, Wat H, Chan HHL. A systematic review of picosecond laser in dermatology: evidence and recommendations. Lasers Surg Med 2020; doi:https://doi.org/10.1002/lsm.23244. Cited in: PMID: 32282094.
- Cho SB, Park SJ, Kim JS, Kim MJ, Bu TS. Treatment of post-inflammatory hyperpigmentation using 1064-nm Q-switched Nd: YAGlaser with low fluence: report of three cases. J Eur Acad Dermatol Venereol. 2009;23(10):1206–07. doi:https://doi.org/10.1111/j.1468-3083.2009.03123.x. Cited in: PMID: 19453798.
- Lee HJ, Lee SH, Yoon SY, Lee JW, Kim YK, Choi EH. 2018. Postinflammatory hyperpigmentation successfully treated with 1,064-nm picosecond-domain neodymium: yttrium-aluminum-garnetlaser. Medical Lasers. 7(1):52–54. doi:https://doi.org/10.25289/ML.2018.7.1.52
- Yu W, Zhu J, Yu W, Lyu D, Lin X, Zhang Z. A split-face, single-blinded, randomized controlled comparison of alexandrite 755-nm picosecond laser versus alexandrite 755-nm nanosecond laser in the treatment of acquired bilateral nevus of Ota-like macules. J Am Acad Dermatol. 2017;79:479–86. doi:https://doi.org/10.1016/j.jaad.2017.12.053. Cited in: PMID: 29288102.
- Trivedi MK, Yang FC, Cho BK. A review of laser and light therapy in melasma. Int J Women’s Dermatol. 2017;3:11–20. doi:https://doi.org/10.1016/j.ijwd.2017.01.004. Cited in: PMID: 28492049.
- Habbema L, Verhagen R, Van Hal R, Liu Y, Varghese B. Minimally invasive non-thermal laser technology using laser-induced optical breakdown for skin rejuvenation. J Biophotonics. 2012;5(2):194–99. doi:https://doi.org/10.1002/jbio.201100083. Cited in: PMID: 22045580.