Abstract
Introduction: The intrapartum cardiotocography (CTG) classification system by FIGO in 2015 (FIGO2015) was introduced to simplify CTG interpretation, but it is not harmonized with the fetal ECG ST analysis (STAN) algorithm from 2007 (STAN2007), which is based on the FIGO CTG system from 1987. The study aimed to determine time courses and sensitivity between the systems in classifying CTG + ST events to indicate metabolic acidosis at birth.
Material and methods: Forty-four cases with umbilical cord artery metabolic acidosis were retrieved from a European multicenter database. CTG patterns and timing of the first occurring significant ST events were evaluated post hoc in consensus by an expert panel and sensitivity statistics were performed. Wilcoxon’s matched-pairs signed-ranks test and McNemar’s test were used with a two-tailed p < .05 regarded significant.
Results: STAN2007 had a higher sensitivity (73 versus 43%, p = .0002) and alarmed for metabolic acidosis in mean 34 min earlier than the FIGO2015 system did (p = .002). In every fourth case, the time difference was ≥20 min.
Conclusions: In this simulation study, surveillance with STAN2007 combined with fetal ECG ST analysis had a significantly higher sensitivity and would have alarmed for metabolic acidosis significantly earlier than the new FIGO system would have.
Brief rationale
We recently in a simulation study demonstrated that the new FIGO system from 2015 (FIGO2015) would classify cardiotocography (CTG) traces and ST events indicated by fetal ECG ST analysis (STAN) discrepantly from the current CTG classification system used in the STAN interpretation algorithm from 2007 (STAN2007). The new system then seems not exchangeable against the old system in the STAN interpretation algorithm. In the present simulation study, we investigated the performance of FIGO2015 versus STAN2007 in a retrospective series of 44 cases with umbilical cord blood arterial metabolic acidosis. CTG traces and ST events were classified post hoc in consensus by three CTG and STAN experts and the time from the first occurring significant CTG + ST event till delivery was calculated for both systems in each case. Other clinical information than metabolic acidosis were hidden. Of the 44 cases, STAN2007 first alarmed for metabolic acidosis in 32 cases (73%) and FIGO2015 in 19 cases (43%). This difference in sensitivity was significant (p = .0002). There was no case where FIGO2015 indicated a significant CTG + ST event and STAN2007 did not. In mean, STAN2007 alarmed 34 min earlier than FIGO2015 (p = .002), and in 25% of cases the time difference was more than 20 min. When the time aspect of significant CTG + ST events was not considered, the sensitivity of STAN2007 was still higher (73 versus 59%, p = .03). This simulation study then indicates that FIGO2015 cannot replace STAN2007 in the STAN interpretation algorithm because of being later in alarming for impending metabolic acidosis.
Key message
In this simulation study, the modified FIGO CTG classification system from 1987 combined with fetal ECG ST analysis (STAN) would have alarmed for metabolic acidosis significantly earlier than if combined with the new FIGO system from 2015.
Introduction
In 2015, the International Federation of Gynecology and Obstetrics (FIGO) presented an updated intrapartum cardiotocography (CTG) classification system (FIGO2015) [Citation1]. In a recent study [Citation2], we demonstrated that the new FIGO system would classify CTG traces and ST events indicated by fetal ECG ST analysis (STAN) discrepantly from the current CTG classification system used in the STAN interpretation algorithm (STAN2007) [Citation3], which is based on the original FIGO classification from 1987 [Citation4]. Hence, the new system seems not exchangeable against the old system in the STAN interpretation algorithm.
Since it remains to show the safety and accuracy of the new FIGO CTG classification system, we conducted the present study with the aim to investigate the performance of the new system in a retrospective series with verified adverse outcomes at birth, i.e. in cases with umbilical cord blood arterial metabolic acidosis. In a cohort from a large European observational multicenter study [Citation5], we classified CTG patterns and ST events with the old and the new classification systems post hoc, and assessed their respective sensitivity and time frame to anticipate metabolic acidosis. Based on our previous study [Citation2], we hypothesized that the systems would perform differently.
Material and methods
A prerequisite for inclusion in the study was that a good quality CTG trace combined with STAN was available for of at least 30 min before the first occurring ST event, or before delivery in cases of no ST event appeared. Cases with umbilical cord blood metabolic acidosis at birth were retrieved from a database of a European multicenter study of 6999 deliveries performed during a 21-month period 2000–2002 [Citation5]. The study was performed at maternity units in Berlin, Copenhagen, Derby, Gothenburg, Lyon, Oslo, Perugia, Plymouth, Turku and Utrecht, to evaluate the clinical implementation of STAN. Oral informed consent from enrolled women and ethical approvals were obtained in those maternity units where STAN was not part of standard care.
The maternity units were equipped with STAN S21 monitors (Neoventa Medical, Mölndal, Sweden) following a 2–3 months educational process where two midwives and two doctors at each unit were trained by the manufacturer, and where these persons then educated and trained the rest of the staff.
STAN monitoring was used in singleton pregnancies ≥36 gestational weeks where a fetal scalp electrode was applied because of increased obstetric risk identified before or during labor. Monitoring was started in the first stage of labor and the clinical management was performed according to STAN clinical guidelines settled during the late 1990s [Citation6,Citation7]. In those guidelines, a modification of the 1987 FIGO CTG classification system [Citation4] was used; the STAN CTG classification system was republished in 2007 by Amer-Wåhlin et al. [Citation8] and in the present article therefore called STAN2007. ST data were open for the staff and fetal scalp blood sampling for determination of pH was performed at the discretion of the managing obstetrician. Immediately postpartum the umbilical cord was double-clamped and arterial and venous blood sampled for blood gas analyses. Umbilical cord blood metabolic acidosis was defined as an arterial pH < 7.05 in combination with a base deficit in extracellular fluid >12.0 mmol/L [Citation9].
The CTG traces were stored electronically for off-line analysis at a 1 cm/min paper speed with STAN Viewer computer software (Neoventa Medical, Mölndal, Sweden). Using a colored case report form [Citation2], the CTG traces were assessed and classified post hoc in consensus by two experienced CTG and STAN expert users (A.C. and H.N.). If consensus was not easily reached, a third expert (K.G.R.) settled. ST events and information about outcome (metabolic acidosis) were not hidden from the experts, but no other clinical information was revealed.
The fetal heart rate (FHR) patterns preceding ST events were classified according to the old and new FIGO CTG classification systems. The time of the first occurring ST event deemed significant by each of the classification systems were noted and for each system the time elapsing to birth was calculated. The sensitivity of each of the two systems was calculated twice, first at the time of the first ever significant ST event, and then for the whole CTG + ST trace until delivery. The time from end of FHR monitoring to birth was noted. For each individual case, two copies of the case report form were used, one for the first ever ST event and one for the time until delivery, where the time periods could be overlapping.
The classification of a CTG trace was in the STAN interpretation algorithm related to type of ST event to judge whether an ST event was significant or not [Citation8]. In cases of pre-terminal CTG patterns (variability <2 bpm, i.e. absent variability, silent pattern), the STAN clinical guidelines advocate immediate delivery irrespective of ST events or not. The pre-terminal CTG class is included in the STAN2007 system but not in the FIGO2015 system. In the FIGO2015 system such traces are deemed pathologic, suggesting a high probability of hypoxia and acidosis. We have summarized and displayed the two CTG classification systems in our recent article on agreements and discrepancies between the systems [Citation2].
Small-for-gestational-age was defined as a birthweight below the fifth gestational age- and fetal gender-adjusted percentile, appropriate-for-gestational-age as between the 5th and 95th percentile, and large-for-gestational-age as above the 95th percentile according to the World Health Organization multinational fetal growth Chart [Citation10].
Statistical analyses
Statistics were performed with aid of StatView® computer software (SAS Institute, version 5.0.1; Cary, NC). Comparison of continuous variables between groups was performed with Wilcoxon’s matched-pairs signed-ranks test, and of categorical variables with McNemar’s test. Sensitivity was expressed as (number of positives)/(number of positives + number of negatives), where positives were metabolic acidosis indicated by significant ST events and negatives where CTG + ST monitoring failed to indicate metabolic acidosis, or ST events were absent. Sensitivity with 95% confidence interval was calculated with software available on the web [Citation11]. A two-tailed p value of < .05 then indicated a significant discrepancy between the classifications compared.
Results
Fifty-one newborns with metabolic acidosis were identified in the database. In one case, the STAN Viewer document was damaged; in one case, the identification was unclear; in two cases, a poor ST signal disabled ST analysis; and in three cases, the CTG traces were pathologic at onset of STAN monitoring, which is a violation of STAN clinical guidelines [Citation8]. Thus, time courses and sensitivity of first ever significant ST events could be evaluated in 44 cases. Demographic characteristics of these cases are shown in . In six cases, the monitoring ended more than 20 min before delivery and the CTG patterns associated with cord blood metabolic acidosis could then be evaluated in 38 cases.
Table 1. Demographic characteristics of 44 deliveries with umbilical cord arterial metabolic acidosis at birth.
The overall classifications of CTG are shown in . Among the 44 cases available for both CTG and ST analysis, 32 showed significant ST events: first of STAN2007 alone in 13 cases, and STAN2007 and FIGO2015 simultaneously in 19 cases. The difference in sensitivity between the two systems was significant ().
Table 2. Distribution of 44 cardiotocograms between the cardiotocography classification systems.
Table 3. Comparison of sensitivity between cardiotocography classification systems combined with fetal ECG ST analysis to identify neonatal metabolic acidosis in umbilical cord blood at first ever occurring significant ST event in any of the systems.
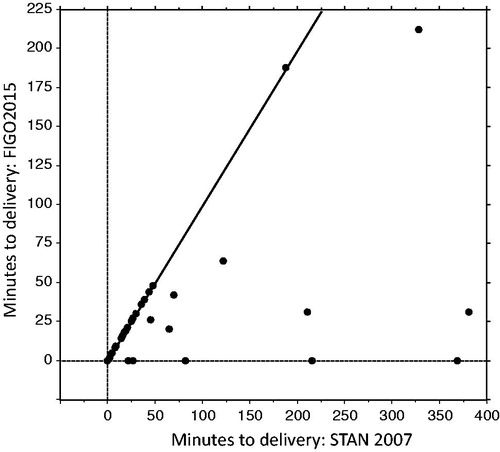
The time courses of the first significant ST event indicating metabolic acidosis by each of the two CTG classification systems are illustrated in . When the time to birth was set to nil minutes for cases with no ST events occurring and for those with non-significant ST events, the STAN2007 system indicated metabolic acidosis significantly earlier than the FIGO2015 system did (p = .002). The median time difference between the systems in showing the first significant ST event was nil minutes, and the mean time difference was 34 min (range 0–369 min). The STAN2007 system indicated significant ST events at least 20 min earlier than the FIGO2015 system in 11/44 (25%) of cases.
Figure 1. Scattergram showing the times from the first significant ST events occurring until delivery (n = 44). The times for the cardiotocography classification system currently used in the fetal ECG ST analysis (STAN) interpretation algorithm from 2007 (STAN2007) should be read on the x-axis, and the times for the new system by the International Federation of Gynecology and Obstetrics from 2015 (FIGO2015) on the y-axis. When no ST events occurred, or when ST events were non-significant, the time was set to nil minutes. The time difference was in mean 34 min (Wilcoxon’s signed-ranks matched-pairs test, p = .002).
The overall sensitivity, i.e. when the time aspect of significant ST events was not considered, was 72.7% (95% confidence interval: 57.0–84.5) for STAN2007 and 59.1% (43.3–73.3%) for FIGO2015 (p = .03).
The types of CTG patterns in cases with ongoing CTG and ST analysis until < 20 min before delivery are shown in . A baseline FHR within the range of 110–150 bpm occurred in 15/38 (39%) of cases and within 110–160 bpm in 26/38 (68%), a variability within the range of 5–25 bpm in 15/38 (39%), and decelerations lasting < 60 s in 13/37 (35%). The combination of baseline FHR 110–160 bpm and variability 5–15 bpm occurred in 13/38 (34%). Among four cases showing no ST event, none showed all CTG element categories normal according to the STAN2007 system. Among seven cases showing non-significant ST events, one showed all CTG element categories normal ().
Table 4. Relations between baseline fetal heart rate, variability and decelerations in 38 newborns with metabolic acidosis at birth and cardiotocography and ST analysis monitoring ongoing until <20 min before birth.
Discussion
This simulation study showed that fetal surveillance with the STAN2007 CTG classification system combined with ST analysis would have alarmed for metabolic acidosis at birth significantly earlier than the corresponding combination with the FIGO2015 system would. In every fourth case, the FIGO2015 system lagged behind with more than 20 min.
The differences between the systems in time courses of when significant ST events occurred were also reflected in the sensitivity analyses. In all, metabolic acidosis was indicated by significant ST events in 32 cases, where STAN2007 alone was the earliest indicator in 13 cases and simultaneous with FIGO2015 in 19 cases. There was no case where FIGO2015 indicated a significant ST event and STAN2007 did not. STAN2007 then showed an estimated sensitivity of 73% while the sensitivity of FIGO2015 was significantly lower, 43%. By progress of labor, new ST events occurred and the sensitivity of FIGO2015 then increased to 59%, but the difference to STAN2007 remained significant. This is an important finding, implicating that in comparative studies of methods for intrapartum fetal monitoring, the time courses of when FHR abnormalities occur must be considered.
Not only the STAN2007 system, but also the FIGO2015 system, alarmed for action hours before delivery at some occasions. This is a worrisome finding, because a delay in action will expose the fetus to graver hypoxia than necessary. The European multicenter study [Citation6], from which the study series was retrieved, was performed during the clinical introduction of ST analysis and digressions from STAN clinical guidelines might have happened, as has been experienced by others despite user certification and thorough training of the staff [Citation12]. By continuous staff support, feedback, and experts and opinion leaders on the floor, Norén & Carlsson [Citation13] managed to gradually reduce the rate of metabolic acidosis in their hospital from 0.72 to 0.19% after 4–6 years.
It is a strength of the study that the CTG and ST evaluations were performed by three expert clinicians in consensus. They had experience of applying the new classification systems from our previous study [Citation2], but they had no clinical experience in using them. To facilitate their work, a detailed colored case report form was created. A weakness of the study was that the experts had knowledge about the clinical outcome, which possibly could have influenced the classification of CTG from what it would have been without the knowledge, or what it would have been in the clinical situation. A simulation study like this cannot perfectly conform to a study performed in reality. Performing CTG classifications post hoc might idealize what a monitoring system is capable of. On the other hand, that does not disqualify fair comparisons between different systems in a simulation study like ours.
We also attempted to elucidate the types of CTG patterns associated with metabolic acidosis. Ingemarsson & Ingemarsson [Citation14] have stated that it is difficult to correlate the CTG pattern in the second stage of labor to Apgar score and cord blood acidemia because of influence of other factors. They particularly emphasize attention to decreasing variability as a first sign of worsening hypoxia, eventually leading to absent variability and silent pattern. In parallel, tachycardia and changes in shape and duration of variable decelerations occur and then a fall in baseline FHR to an end-stage bradycardia. In addition to these observations, an acute increase in variability has been suggested as a specific marker of metabolic acidosis when lasting for more than 20 min [Citation15].
In our analysis of CTG patterns preceding cord artery acidemia, only one fetus showed a normal CTG pattern, but one-third of fetuses had normal variability together with a baseline FHR of 110–160 bpm. Cases with no ST events or non-significant ST events showed mostly less serious decelerative patterns and mostly a normal baseline and normal variability. To identify these fetuses before they develop severe hypoxia and metabolic acidosis constitutes an important challenge. So far, CTG interpretation is based on a matrix assessment based on clinical experience gathered over the last 50 years, but by the present results it appears necessary to more precisely identify acutely evolving specific FHR changes that in connection with ST events signify the rapid conversion from compensated to uncompensated hypoxia and development of metabolic acidosis. Thus, Rosén et al. [Citation16] have recently suggested a more physiologically oriented approach to FHR assessment in connection with ST events.
In summary, this study showed that in a series of deliveries with umbilical cord blood metabolic acidosis, intrapartum surveillance with the STAN2007 CTG classification system combined with fetal ECG ST analysis would have alarmed for metabolic acidosis significantly more often and significantly earlier than the FIGO2015 system would have. Metabolic acidosis was in all indicated by significant ST events in 32 cases, of which STAN2007 alone was the earliest indicator in 13 cases and simultaneous with FIGO2015 in the other 19 cases. The sensitivity of 73% with STAN2007 was significantly better than 43% by FIGO2015. However, the shortcomings of CTG monitoring to indicate metabolic acidosis in some cases, even in combination with ST analysis, prove the need to refine the method.
Acknowledgements
Neoventa Medical AB is acknowledged for providing the STAN Viewer computer software for offline analyses.
Disclosure statement
K.G.R. is a founder of Neoventa Medical AB and holds < 1% of shares, but has no current financial relation. P.O. is consulting Global Medical Adviser to Neoventa Medical AB. H.N. and A.C. declare no conflicts of interest.
References
- Ayres-de-Campos D, Spong CY, Chandraharan E. FIGO consensus guidelines on intrapartum fetal monitoring: cardiotocography. Int J Gynecol Obstet. 2015;131:13–24.
- Olofsson P, Norén H, Carlsson A. New FIGO and Swedish intrapartum cardiotocography classification systems incorporated in the fetal ECG ST analysis (STAN) interpretation algorithm: agreements and discrepancies in cardiotocography classification and evaluation of significant ST events. Acta Obstet Gynecol Scand. 2018;97:219–228.
- Rosén KG, Mårtendal A. The physiology of fetal surveillance. The green book of Neoventa Part I. Göteborg: Neoventa Medical AB; 2014.
- FIGO Subcommittee on Standards in Perinatal Medicine. Guidelines for the use of fetal monitoring. Int J Gynecol Obstet 1987;25:159–167.
- Luttkus AK, Norén H, Stupin JH, et al. Fetal scalp pH and ST analysis of the fetal ECG as an adjunct to CTG – a multi-centre, observational study. J Perinat Med. 32:486–494.
- Sundström A-K, Rosén D, Rosén KG. Fetal surveillance. Göteborg: Neoventa Medical AB; 2000.
- Amer-Wåhlin I, Hellsten C, Norén H, et al. Intrapartum fetal monitoring: cardiotocography versus cardiotocography plus ST analysis of the fetal ECG. A Swedish randomized controlled trial. Lancet. 2001;358:534–538.
- Amer-Wåhlin I, Arulkumaran S, Hagberg H, et al. Fetal electrocardiogram: ST waveform analysis in intrapartum surveillance. BJOG. 2007;114:1191–1193.
- Wiberg N, Källén K, Olofsson P. Base deficit estimation in umbilical cord blood is influenced by gestational age, choice of fetal fluid compartment, and algorithm for calculation. Am J Obstet Gynecol. 2006;195:1651–1656.
- Kiserud T, Piaggio G, Carroli G, et al. The World Health Organization fetal growth charts: a multinational longitudinal study of ultrasound biometric measurements and estimated fetal weight. PLOS Med. 2017;14:e1002220.
- VassarStats [Internet]. Website for statistical computation. Available from: http://vassarstats.net
- Amer-Wåhlin I, Källén K, Herbst A, et al. Implementation of new medical techniques: experience from the Swedish randomized controlled trial on fetal ECG during labor. J Matern Fetal Neonatal Med. 2005;18:93–100.
- Norén H, Carlsson A. Reduced prevalence of metabolic acidosis at birth: an analysis of established STAN usage in the total population of deliveries in a Swedish district hospital. Am J Obstet Gynecol. 2010;202:546.e1–546.e7.
- Ingemarsson I, Ingemarsson E. Fosterövervakning Med CTG. [Fetal Surveillance with CTG]. Lund: Studentlitteratur; 2006.
- Nunes I, Ayres-de-Campos D, Kwee A, et al. Prolonged saltatory fetal heart rate pattern leading to newborn metabolic acidosis. Clin Exp Obstet Gynecol. 2014;41:507–511.
- Rosén KG, Norén H, Carlsson A. FHR patterns that become significant in connection with ST waveform changes and metabolic acidosis at birth. J Matern Fetal Neonatal Med. 2018 [Apr 18]; [1–6].
