Abstract
Objectives: To establish reference curves of normal fetal small bowel and colon diameters and to assess the clinical applicability.
Method: Serial longitudinal ultrasound examinations at 4-week intervals between 20 to 41 weeks of gestation in 39 low-risk fetuses. The largest loop of the small bowel and colon was identified. The bowel lumen short axis was measured. Linear mixed modeling was used to determine individual developmental trajectories. Twenty-eight fetuses with suspected bowel dilatation were analyzed relative to the reference curves.
Results: Development of the small bowel and colon diameters was best described by a linear and cubic model, respectively. The intraobserver and interobserver concordance were >0.94. In cases with suspected bowel dilatation, normal fetal outcome occurred if the bowel dilatation was transient. Progressive increase of fetal bowel diameter was associated with pathology after birth. Cases with small bowel pathology had a z-score >8 after 25 weeks of gestation.
Conclusion: We provided the first ultrasound reference curves for normal fetal small bowel and colon diameters. Progressive increase in the fetal bowel diameter z-score was highly predictive of intestinal abnormalities after birth. Longitudinal follow-up of dilated fetal bowel is important to distinguish normality from disease.
Introduction
The presence of dilated bowel loops on prenatal ultrasound may be a marker for fetal bowel obstruction and is found in various intestinal disorders, including bowel atresia, midgut volvulus, and meconium ileus [Citation1]. Prenatal diagnosis of these conditions provides an opportunity for parental counseling, close monitoring during pregnancy, and for delivery in a center with a pediatric surgery unit. Some cases may benefit from iatrogenic preterm delivery, for example, intestinal volvulus that may lead to severe bowel necrosis and fetal demise [Citation2]. However, prenatal bowel dilatation can also be transient and even if the dilatation persists until delivery it is possible that no abnormalities are found at postnatal evaluation [Citation3–6]. Parental counseling regarding fetal dilated bowel may therefore be challenging.
To identify pathologically dilated bowel, knowledge of the physiological and gestational age related increase in diameter of small bowel and colon is needed. To date there is no standardized method to assess the fetal bowel diameter. Furthermore, only limited data has been published on reference values for fetal intestinal measurements. None of these studies has used longitudinal data [Citation7–9] and some studies only used postmortem specimens [Citation10,Citation11].
The aim of our study was to establish reference curves of the normal fetal small bowel and colon diameters using longitudinal prospective data and to assess if these curves can be used to identify pathologically dilated bowel disease.
Materials and methods
Prospective longitudinal reference curves of fetal bowel diameter
To construct reference ranges of normal fetal bowel development, we included 39 healthy pregnant women in a prospective longitudinal study.
In all women, gestational age was determined by measurement of crown-rump length in the first trimester of pregnancy. A second trimester anomaly scan did not reveal any anomalies. We included only cases with an estimated fetal weight between the 10th and 90th percentiles [Citation12] in the absence of risk factors that might affect fetal growth, such as previous intrauterine growth restriction, maternal disease, or maternal use of medication. The study was reviewed and approved by the local Medical Ethics Committee of the University Medical Center Utrecht and informed consent was obtained from all participants.
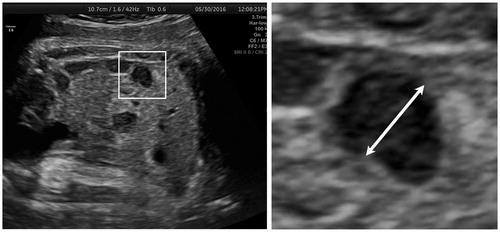
Ultrasound examinations were carried out at 4-week intervals starting at 20 weeks of gestation. All examinations were done by one observer (CL), using a General Electric Voluson 730 or E8 (General Electric Healthcare) ultrasound machine, with a 4–8 MHz transabdominal transducer. Biometry (including fetal head circumference, abdominal circumference, and femur length) was performed, followed by ultrasound evaluation of the fetal bowel. The largest loops of the small bowel and colon were identified in a coronal plane of the fetal abdomen. For both the colon and small bowel, the short axis of the bowel lumen was measured (from inner-to-inner bowel wall; ).
Figure 1. Identification of the largest loop of the colon (coronal plane) at 35 weeks of gestation. Measurement of the short axis of the bowel lumen (inner to inner bowel wall).
Data management and statistical analysis were performed with SPSS for Windows (version 21.0, IBM SPSS Inc., Chicago, IL, USA). The serial measurements available for each fetus were analyzed with multilevel (mixed-effects) modeling to determine the individual developmental trajectories of the small bowel and colon diameters. The first level comprises the variation between gestational ages within fetuses and the second level the variation between individual fetuses. We explored linear, quadratic, and cubic functions of gestational age for the two intestinal variables. The means and 95% prediction intervals (PIs) of the diameters of the small bowel and colon for consecutive gestational ages were calculated. The intraobserver agreement was calculated with intraclass correlation coefficient (ICC) based on two measurements in 39 cases by one observer and the interobserver agreement was calculated with ICC based on 39 repeated measurements by two observers (GM and LP) blinded for type of bowel and outcome.
Assessment of clinical applicability
To assess the diagnostic applicability of the developed reference curves, we identified cases with suspected dilated bowel using the prenatal ultrasound database of the Wilhelmina Children’s Hospital, a Tertiary Referral Hospital. Ultrasound examinations were performed between 1 January 2007 and 31 December 2013. The suspicion of dilated bowel was based on the subjective assessment of the sonographer.
Fetuses with ultrasound findings suggestive of duodenal atresia (double bubble sign), additional extragastrointestinal anomalies, or with chromosomal abnormalities were excluded. Stored ultrasound images were reviewed for each patient. The short axis of the largest dilated bowel loop was remeasured in the images using ImageJ version 1.48 (NIH, Bethesda, MA, USA). If more examinations were available, serial ultrasound images were reviewed to assess whether the dilatation resolved, persisted, or increased over time. Hospital charts were reviewed for maternal, perinatal, and neonatal characteristics. If patients did not receive further care at our center, the referral hospitals were contacted in order to retrieve follow-up data. In each case we calculated z-scores of the small bowel or colon diameter relative to the study reference curves.
Results
Prospective longitudinal reference curves of fetal bowel diameter
A total of 198 ultrasound examinations were performed in 39 uneventful pregnancies. The first ultrasound was performed at 20 weeks of gestation. Repeat scans were performed at 4-week intervals (median 4.0; IQR 4.0–4.4 weeks) until labor. Delivery occurred at a median gestational age of 40 weeks 6 days (range 36 weeks 4 days-41 weeks 6 days). Median birth weight was 3520 g (range 2600–4700 g; Dutch reference curves z-scores [Citation13] mean 0.07 ± 0.96). None of the cases had bowel pathology diagnosed within the 1 month after birth. The median number of scans per pregnancy was 5 (range 4–6). Measurements of small bowel and colon diameters were obtained in 63% and 98% of cases, respectively. The intraobserver and interobserver ICC for small bowel was 0.94 and 0.96, respectively. For colon the ICC was 0.96 for both intra- and interobserver measurements.
The development of small bowel diameter and colon diameter was best described by a linear model and a cubic model, respectively, as shown in . The regression equations for the small bowel and colon modeled as a function of gestational age are given in Appendix A. At 40 weeks of gestation, mean small bowel diameter was 5.1 mm and mean colon diameter was 14.5 mm ().
Figure 2. Reference charts of small bowel diameter (A) and colon diameter (B) showing raw data (°) and fitted 50th percentile and 95% prediction ranges.
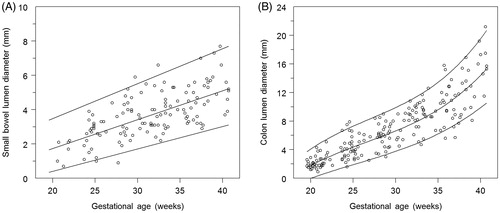
Table 1. Small bowel and colon diameters according to gestational age.
Assessment of clinical applicability
We identified 28 cases with suspected isolated dilated bowel loops. In z-scores of inner diameter of fetal bowel of these cases are presented relative to the study reference curves.
Figure 3. Fetal small bowel (A) and colon (B) inner diameter according to gestational age in fetuses with (box, n = 8) and without (circle, n = 20) bowel pathology. Z-scores were calculated relative to the study nomograms in each case. Upper and lower horizontal lines indicate z-scores of two and −2 respectively, that is, the range of ± two SDs from the mean values represented by a z-score of 0. Two cases (*) were antenatally suspected of colon dilatation and are presented in Figure 3(B) but turned out to have small bowel pathology after birth.
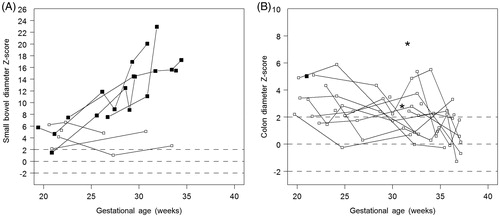
In , cases with suspected small bowel dilatation () and suspected colon dilatation () are presented. Only 26% of fetuses with suspected dilated bowel were found to have intestinal abnormalities shortly after birth.
All cases with small bowel pathology after birth (n = 7) had a z-score >8 after 25 weeks of gestation. In cases with two or more consecutive ultrasound examinations progressive dilatation was found in all cases with postnatal bowel pathology. In cases without bowel pathology after birth, the bowel diameter decreased to a z-score below 4 after 35 (weeks of gestation; ). The cases with suspected colon dilatation are presented in . In 10 cases with repeated measurements the colon diameter was not progressive. None of these cases presented with intestinal abnormalities after birth. Additional polyhydramnios was seen in seven cases. In five cases bowel pathology was diagnosed after birth.
The antenatal and postnatal findings of the cases with postnatal bowel pathology are described in . Five out of eight cases had additional polyhydramnios. Two cases (, cases 3 and 7) were antenatally suspected of colon dilatation and are presented in , but turned out to have small bowel pathology after birth. There was one case (, case 8) that was suspected of colon dilatation before birth and this was confirmed postnatally. Unfortunately there were no consecutive measurements of these three cases. Seven cases had small bowel obstructions. There was one intrauterine fetal death at 31 weeks’ gestation (case 1). Autopsy showed dysmorphic facial features (depressed nasal bridge and downward slanting palpebral fissures) and a duodenal web, causing severe dilatation of the proximal duodenum. The cause of death could not be established. Cases 2 and 3 presented with meconium ileus at birth and were diagnosed with cystic fibrosis. Case 4 was born with a jejunal atresia and had concomitant congenital biliary atresia. Surgical porto-enterostomy was not successful and she died at 15 months of age awaiting liver transplantation. Case 5, an infant born with jejunal and ileal atresia and antenatal volvulus, had multiple anastomotic leaks after primary surgery. Adequate intestinal function could not be established and he died at 4 months of age. Case 6 had intrauterine small bowel perforations resulting in meconium peritonitis. Postnatal surgery showed extended bowel necrosis. Despite surgical attempts to preserve bowel function, she died 18 h after birth. A monochorionic twin pregnancy with one child (case 7) with antenatal suspected bowel dilatation and polyhydramnios presented with atresia, volvulus, and peritonitis. Successful ileostomy with end-to-end anastomosis was performed. There was only one case with colon pathology after birth; case 8 had a blind-ending ascending colon in which surgical anastomosis was successful. In the group without neonatal bowel pathology, one infant was diagnosed with biliary atresia at 3 weeks of age. She had a successful liver transplantation and is doing well now at 5 years of age.
Table 2. Summary of cases with bowel pathology.
Discussion
We provide the first ultrasound reference curves of the fetal small bowel and colon diameters based on repeated measurements on individuals. The charts were derived from longitudinal data obtained from prospective investigations between 20 and 40 weeks of gestation. The mean colon diameter at 40-week gestation was 14.5 mm, with a maximum of 19.4 mm. For small bowel the mean diameter at 40-week gestation was 5.1 mm with a maximum of 7.6 mm.
Our results for colon diameter are in line with the findings of two other studies in which a maximal inner diameter of 18 mm was found [Citation7,Citation9]. In one of these studies an increase in mean colon diameter from 3.5 to 13.5 mm between 20 and 40 weeks of gestation was found [Citation9]. We are aware of only one study on ultrasound assessment of the small bowel diameter across gestation [Citation8]. These authors reported an increase from 1 to 4.4 mm in the course of gestation, with a maximum of 8 mm at term. Neither standard deviations nor PIs were given. All previous reference charts for small bowel and colon diameter were constructed using cross-sectional data [Citation7–9]. Malas et al. studied the development of colon, jejunum, and ileum in a postmortem series of 131 fetuses [Citation10,Citation11]. The authors only provided the outer-to-outer bowel wall diameters. For colon diameter they found an increase from 3 to 15 mm between 20 and 40 weeks of gestation. The diameter of the small intestine was determined as an average of 7 mm at term, which is higher than in our series. This difference may be explained by the fact that the postmortem measurement of a loop of bowel without smooth muscle tone can be significantly different from the diameter of a loop of bowel in a living fetus.
In our retrospective study only 26% of fetuses with suspected dilated bowel were found to have intestinal abnormalities at birth. Our study shows that fetal intestinal dilatation can resolve during gestation; 56% of fetuses with repeated measurements had a resolution of intestinal dilatation on consecutive ultrasound examinations. Resolution of dilated bowel should be considered reassuring for normal neonatal outcome, since none of those fetuses were found to have intestinal pathology after birth. In the cases with transient bowel dilatation there was one infant diagnosed with biliary atresia; a condition only seen in 1 in 19.000 livebirths [Citation14]. To our knowledge transient antenatal bowel dilatation has not been described in association with biliary atresia and this may therefore be a coincidental finding.
In all cases with progressive dilatation of the small bowel, pathology of the small bowel was confirmed after birth. A large small bowel diameter (z-score >8) after 25 weeks of gestation was also associated with small bowel pathology. The type of bowel disease diagnosed after birth varied however. In all these cases surgical treatment was necessary in early postnatal life. This stresses the importance of antenatal diagnosis of bowel pathology to ensure immediate pediatric (surgical) care after birth.
Polyhydramnios is a risk factor for fetal bowel obstruction, especially when found in combination with fetal bowel dilatation [Citation5]. In our case series of patients with fetal bowel dilatation, five out of eight cases with postnatal bowel pathology had polyhydramnios. However, polyhydramnios was also seen in two cases without bowel pathology after birth. Hence polyhydramnios is not a reliable indicator for bowel obstruction.
The incidence of abnormalities after birth in our retrospective series is lower than that reported in a previous study by Ruiz et al. [Citation3]. They described postnatal bowel pathology in 8 out of 15 fetuses (53%) with bowel dilatation on prenatal ultrasound. This difference is possibly explained by underreporting of cases with normal postnatal outcome, since there were five cases lost to follow-up in their series.
The strength of our study of normal reference curves is its prospective and longitudinal design. The bowel measurements were performed according to a strict protocol. We are aware that distinguishing the small bowel from colon can be difficult. However, the coronal plane of the fetal abdomen helps to distinguish the small bowel from the colon by its anatomic position. In addition, identification of haustra of the colon becomes easier in the third trimester. This confirms – again – the importance of repeated measurements.
The cohort used to test the applicability of our study was limited by retrospective design. The measurements were performed before the prospective study was done and therefore not standardized. Identification of small bowel or colon was not preformed according to our proposed protocol. However, we remeasured the bowel dilatation and calibrated the images in order to improve the standardization of measurements. Unfortunately, repeated measurements were not available for all cases with postnatal colon pathology. Therefore, no definite conclusions can be drawn about the development of colon dilatation over time. Further research in cases with suspected colon dilatation using the normal colon curves is necessary in order to test the clinical applicability of the reference curves of the colon.
In conclusion, we have provided ultrasound reference curves for the normal fetal small bowel and colon diameters. These reference curves may be useful in the prenatal counseling of parents carrying a fetus with dilated bowel loops. Transiently dilated bowel on prenatal ultrasound predicts a normal fetal outcome. Progressive increase in the fetal bowel diameter, on the other hand, is highly predictive of intestinal abnormalities after birth. Longitudinal follow-up of dilated bowel is important to distinguish normality from disease.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Shawis R, Antao B. Prenatal bowel dilatation and the subsequent postnatal management. Early Hum Dev. 2006;82:297–303.
- Takacs ZF, Meier CM, Solomayer EF, et al. Prenatal diagnosis and management of an intestinal volvulus with meconium ileus and peritonitis. Arch Gynecol Obstet. 2014;290:385–387.
- Ruiz MJ, Thatch KA, Fisher JC, et al. Neonatal outcomes associated with intestinal abnormalities diagnosed by fetal ultrasound. J Pediatr Surg. 2009;44: 71–74; discussion: 74–75.
- Borsellino A, Zaccara A, Nahom A, et al. False-positive rate in prenatal diagnosis of surgical anomalies. J Pediatr Surg. 2006;41:826–829.
- Virgone C, D'Antonio F, Khalil A, et al. Accuracy of prenatal ultrasound in detecting jejunal and ileal atresia: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2015;45:523–529.
- Orgul G, Soyer T, Yurdakok M, et al. Evaluation of pre- and postnatally diagnosed gastrointestinal tract obstructions. J Matern Fetal Neonatal Med. 2018;12:1–6.
- Nyberg DA, Mack LA, Patten RM, et al. Fetal bowel. Normal sonographic findings. J Ultrasound Med. 1987;6:3–6.
- Parulekar SG. Sonography of normal fetal bowel. J Ultrasound Med. 1991;10:211–220.
- Zalel Y, Perlitz Y, Gamzu R, et al. In-utero development of the fetal colon and rectum: sonographic evaluation. Ultrasound Obstet Gynecol. 2003;21:161–164.
- Malas MA, Aslankoç R, Ungör B, et al. The development of jejunum and ileum during the fetal period. Early Hum Dev. 2003;74:109–124.
- Malas MA, Aslankoç R, Ungör B, et al. The development of large intestine during the fetal period. Early Hum Dev. 2004;78:1–13.
- Verburg BO, Steegers EA, De Ridder M, et al. New charts for ultrasound dating of pregnancy and assessment of fetal growth: longitudinal data from a population-based cohort study. Ultrasound Obstet Gynecol. 2008;31:388–396.
- Perinatale Zorg in Nederland. Utrecht, Netherlands: Stichting Perinatale Registratie Nederland. 2006.
- Hartley JL, Davenport M, Kelly DA. Biliary atresia. Lancet. 2009;374:1704–1713.
