Abstract
Objectives
Few studies have assessed pregnancies and deliveries after traumatic brain injury (TBI). We report the incidence of TBIs and TBI-related surgeries in fertile-aged females and investigate subsequent pregnancy outcomes.
Methods
All fertile-aged (15–49) women with TBI diagnosis during our study period (1998–2018) were retrieved from the Care Register for Health Care and combined with data from the National Medical Birth Register. TBIs were categorized into three subgroups based on the length of the hospitalization period and the need for neurosurgery. Logistic regression was used to analyze preterm deliveries, cesarean sections (CS) and neonatal health. Results are reported as adjusted odds ratios (AOR) with 95% confidence intervals (CI).
Results
The incidence of TBIs increased from 103 per 100 000 person-years in 1998 to 257 per 100 000 (149.5%) in 2018. The incidence of TBI-related surgeries remained stable during our study period. The rate of preterm deliveries was 5.6% in the TBI group and 3.0% in the control group (AOR 1.23, CI 1.17–1.28). The CS rate in the TBI group was 19.2% and 15.9% in the control group (AOR 1.23, CI 1.18–1.29). The use of labor analgesia was higher among women with previous TBI. The rate of neonates requiring intensive care in the TBI group was 13.1% and 9.9% in the control group (AOR 1.30, CI 1.24–1.37).
Conclusion
The incidence of TBI hospitalizations increased during our study period, whereas the number of surgically treated TBI remained stable. Preterm deliveries, CS, instrumental vaginal deliveries and labor analgesia were more prevalent in women with previous TBI. Furthermore, more neonates required intensive care in this group. Therefore, a history of TBI should be acknowledged as a possible factor affecting the delivery and health of the neonate.
Introduction
Traumatic brain injury (TBI) has increasingly become an important global health problem [Citation1]. Indeed, more than 10 million people worldwide are affected annually by TBI [Citation2], with the most common causes being traffic accidents, falls and sports activities [Citation3]. An international study has estimated the incidence of TBI globally to be approximately 369 per 100 000 person-years. [Citation4] In Finland, the average incidence of hospitalized TBI for all women between 1991 and 2005 was 80 per 100 000 person-years. TBI patients are known to have higher mortality rates compared to the general population, although the mortality rate depends on the severity of injury [Citation5,Citation6]. In an earlier study, the mortality rate in Finland was estimated to be around 18 per 100 000 person-years, with a higher mortality rate among women [Citation7].
To date, the effects of TBI on the reproductive health of women have been sparsely studied. For fertile-aged women, TBI is reported to cause disorders in the menstrual cycle and nearly 50% of women report amenorrhea following TBI [Citation8,Citation9].
Interestingly, even though women who experience menstrual and/or sexual dysfunctions after a concussion are reported to have a decreasing incidence of pregnancy, previous studies have not assessed the effects of TBI on fertility [Citation10]. Moreover, only a few case reports have discussed the effects of TBI on deliveries in acute cases, where traumatic brain injury leads to the acute cesarean section after a craniotomy is performed to lower intracranial pressure [Citation11,Citation12]. The long-term effects of TBI on subsequent deliveries and neonatal health have not previously been studied, however. The aim of this nationwide register study is to report the incidence of TBI and surgeries related to TBI in fertile-aged females in Finland and to investigate the impact of TBI on subsequent pregnancies and deliveries
Materials and methods
In this nationwide retrospective register-based cohort study, data were retrieved from the Care Register for Health Care and combined with data retrieved from the National Medical Birth Register (MBR). Both registers are maintained by the Finnish Institute for Health and Welfare. The study period was from January 1, 1998 to December 31, 2018.
All fertile-aged (15–49 years) women with a TBI diagnosis during our study period were retrieved from the Care Register for Health Care. TBI was defined as a hospitalization period following TBI based on ICD-10 (International Classification of Diseases 10th revision) codes. After a one-year wash-out period, each TBI diagnosis was classified as a new separate TBI, as hospital follow-up appointments for TBI rarely occur later than one-year post-injury in the majority of cases. In subgroup analysis, TBIs with a hospitalization period lasting more than one day were considered as admitted TBI, and TBIs with a hospitalization period lasting less than one day were considered as non-admitted TBI. Patients who underwent surgery were identified by NOMESCO (Nordic Medico-Statistical Committee) classification procedure codes. Only procedure codes with one of the TBI diagnosis codes during the same hospitalization period were included because these operations are also performed for reasons other than TBI. ICD-10 codes and NOMESCO classification procedure codes included in this study are shown in Supplementary Table 1.
The incidences of TBIs and TBI surgeries were calculated using the whole population of fertile-aged (15–49 years) women in Finland at the end of a particular year, which was obtained from Statistics Finland (Stat.fi). During our study period, the size of the study population in Finland decreased from 1 389 409 in 1998 to 1 285 100 in 2018 [Citation13].
Data retrieved from the Care Register for Health Care were combined with data from the National Medical Birth Register (MBR) using the pseudonymised identification number of the mother. The MBR contains information on all pregnancies, delivery statistics and the perinatal outcomes of births with a birthweight of ≥500 grams or a gestational age ≥22 + 0. The MBR has a coverage of nearly 100% [Citation14,Citation15]. In the present study, we use the standard variables used in the MBR, which are defined in the register description [Citation16].
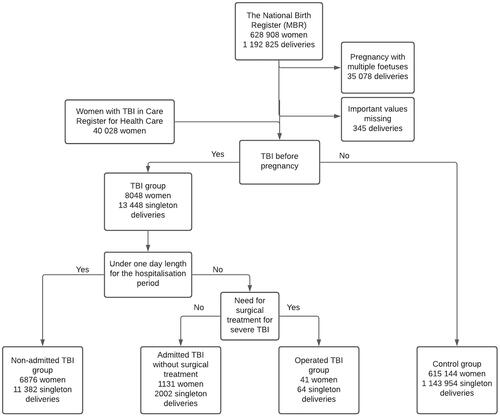
A flowchart of the study population is presented in . All deliveries of women with previous TBI were compared with a control group without previous TBI, which consisted of 615 144 women with 1 143 954 singleton deliveries. In subgroup analysis, non-admitted admitted and operated TBIs were analyzed separately. The identification of women with previous TBI with subsequent deliveries was based on the date of the TBI or operation in the Care Register for Health Care and the start date of the pregnancy in the MBR. Deliveries with missing information on the mode of delivery were excluded. In the MBR, cesarean section (CS) was classified as elective or urgent until 2004, and in order to have uniform coding throughout the study period, we used this instead of the current three-stage classification (elective, urgent and emergency). This means that each emergency and urgent CS is considered as an unplanned CS in our current report. The results of this study are reported according to the STROBE guidelines (Supplementary Table 1) [Citation17].
Figure 1. Flowchart of the study population. Data from the MBR were combined with data on the diagnosed TBI and TBI-related surgical operations in the Care Register for Health Care.
Ethics
Both the National Medical Birth Register (MBR) and the Care Register for Health Care have the same unique pseudonymised identification number for each patient. The pseudonymisation was made by the Finnish data authority Findata. The authors did not have access to the pseudonymisation key, as it is maintained by Findata. In accordance with Finnish regulations, no informed written consent was required because of the retrospective register-based study design and because the patients were not contacted. Permission for use of this data was granted by Findata after evaluation of the study protocol (Permission number: THL/1756/14.02.00/2020)
Statistics
Continuous variables were interpreted as mean with standard deviation or as median with interquartile range based on variable distribution. Categorized variables were presented as absolute numbers and percentages. Student’s t-test, Mann-Whitney U-test and Chi-Squared tests were used for group comparisons. Multivariable logistic regression was used to assess the primary outcomes (preterm delivery, mode of delivery and neonatal health). The need for intensive care for the neonate was used as an indicator for neonatal health in logistic regression analyses. Maternal smoking during pregnancy, maternal diabetes during pregnancy and the socioeconomic status of the mother was used as adjusting variables. Details of maternal smoking status during pregnancy are collected during visits to maternity clinics and can be either nonsmoker, smoking during the first semester, smoker or unknown. The socioeconomic status of the mother is recorded in the MBR during pregnancy. Odds ratios (OR) and adjusted odds ratios (AOR) with 95% confidence intervals (CI) were calculated for the main outcomes. P-value under .05 was considered statistically significant. Adjustments were made by choosing the variables for a multivariate model using directed acyclic graphs (DAGs) constructed using the free online software DAGitty (dagitty.net). The variables included in the DAGs were chosen based on known risk factors and by hypothesized causal pathways [Citation18,Citation19]. DAGs are presented as supplementary files (Supplementary Figures 1–3). Statistical analysis was performed using R version 4.0.3.
Results
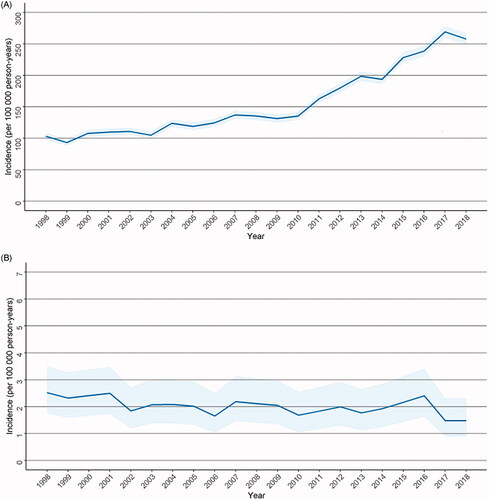
A total of 40 028 women with a TBI hospitalization were retrieved from the Care Register for Health Care. During our study period, the incidence of TBI hospitalization in fertile-aged women increased over two-fold (149.5%) from 103 per 100 000 person-years in 1998 to 257 per 100 000 person-years in 2018 (). The incidence of TBI requiring surgical treatment, however, decreased slightly during our study period from 2.5 to 1.5 per 100 000 person-years ().
Figure 2. (A) Incidence of traumatic brain injury hospitalization among fertile-aged (15–49 years) women during the study period. (B) Incidence of traumatic brain injury surgeries among fertile-aged (15–49 years) women during the study period.
The majority of patients with TBI suffered concussion trauma (S06.0) (n = 36 703, 85.3%), with focal traumatic brain injury (S06.3) (n = 1126, 2.6%) and traumatic subdural hemorrhage (S06.5) (n = 1119, 2.6%) being the second most common types of trauma. The mean age of patients was highest among patients with traumatic subdural hemorrhage (S06.5) (37.6, SD 10.0). Among patients with other TBIs, the mean age was lower, ranging from 29.8 to 33.8 years. A total of 5890 women (13.4%) had a hospitalization period of more than one day (Supplementary Table 2).
During our study period, 8048 women gave birth after TBI. In the TBI group, a notably higher number of fetuses were exposed to maternal smoking during pregnancy when compared to the control group (27.7% vs 14.5%, p < .001). The rate for deliveries requiring induction was higher among women with previous TBI when compared to the control group (25.4% vs 18.9%, p < .001) (). Moreover, a higher rate of women in the TBI group underwent elective CS as a mode of delivery (7.8% vs 6.6%, p < .001). After elective CS was excluded, the rate of unplanned CS was higher in the TBI group (12.5% vs 9.9%, p < .001) when only attempted vaginal deliveries were included. Moreover, the rates of different labor analgesia were higher in the TBI group. In particular, the proportional amount of epidural analgesia (50.8% vs 43.4%, p < .001) and spinal analgesia (15.8% vs 11.4%, p = .292) were higher in the TBI group when compared with the control group ().
Table 1. Background information on the deliveries and perinatal characteristics in the traumatic brain injury group and the control group.
Table 2. Proportions of obstetric variables in attempted vaginal deliveries in the traumatic brain injury group and control group.
Among women with TBI before pregnancy, a slightly higher proportion of neonates were born with low birthweight (birthweight < 2500 grams, LBW) (3.8% vs 3.0%, p < .001) and born preterm (5.6% vs 4.6%, p < .001). Furthermore, the need for neonatal intensive care was slightly higher in the TBI group (13.1% vs 9.9%, p < .001) (). The probability for preterm deliveries in the TBI group was also slightly higher (AOR 1.23, CI 1.17–1.28). The odds for all CS, including both elective and unplanned CS, were slightly higher in the TBI group when compared to the control group (AOR 1.23, CI 1.18–1.29). The odds for impaired health of the neonate showed a small increase in the TBI group when compared with the control group (AOR 1.30, CI 1.24–1.37) (). When compared to the non-admitted and admitted TBI groups in subgroup analysis, patients with operated TBI had a notably higher rate of instrumental vaginal deliveries (21.9% vs 9.3% and 8.8%, p = .015). (Supplementary Table 3)
Table 3. Univariable and adjusted Odds ratios (OR) with 95% confidence intervals (CI) for the main variables.
Discussion
The main finding of this study was the two-fold increase in the incidence of TBI hospitalizations among fertile-aged women within the last two decades. The incidence of TBI-related surgeries remained stable or had decreased slightly during this period. Women with previous TBI had a lower rate of spontaneous vaginal deliveries and higher use of labor analgesia. Women in the TBI group had a higher rate of neonates requiring intensive care.
The overall increased incidence of TBI hospitalizations during our study period, combined with the stable incidence of TBI-related surgeries, indicates that the increase in incidence is predominantly among milder injuries. According to previous systematic reviews, the incidence of TBI among fertile-aged women in Finland has increased to the same level as that seen in the general European population [Citation20–22]. The high increase in TBI hospitalizations among Finnish fertile-aged women can be partly explained by indirect temporal factors and phenomena such as (i) lower patient-based threshold to seek medical care due to mild head injuries, (ii) better access to CT imaging and (iii) improved awareness of TBIs and TBI-related health issues. Furthermore, the foundation of joint emergency service in 2011 may have led to improvements in acute TBI diagnostics. Notably, TBI hospitalizations among Finnish fertile-aged women began to increase more rapidly after 2011.
Women with a history of TBI had a higher rate of complications during delivery, which was indicated by a higher rate of instrumental vaginal deliveries, unplanned CS and labor analgesia. There are no national guidelines for pregnancies/deliveries after TBI in Finland. Most of the time, the mode of delivery after TBI is chosen based on obstetric indications, maternal preference is taken into account, without any particular recommendation from neurosurgeons. Neurosurgeons are consulted during pregnancy about the preferred mode of delivery when deemed necessary. To date, no previous studies have investigated the effects of TBI before pregnancy on obstetric outcomes, although head trauma during pregnancy is known to cause complications for the mother and for the health of the fetus [Citation23]. Interestingly, the rate of instrumental vaginal deliveries among operated TBI patients, where the need for neurosurgery usually indicates more severe neurotrauma, was notably higher. This higher rate of instrumental vaginal deliveries accompanied by a higher rate of labor analgesia could be related to a slower progression of labor. Nevertheless, the rate of unplanned CS and the need for intensive care unit treatment was lower in this group than in the other non-surgical TBI groups. The low number of women in the operated TBI group may have affected these results. Based on our findings, it appears that women with previous TBI experience more challenges related to delivery (lower rate of spontaneous vaginal deliveries) than other groups. Due to the crude nature of the data, however, solid conclusions cannot be made. Furthermore, it remains unknown whether the higher rate of instrumental vaginal deliveries and CS is caused by TBI or by other factors. Additional research on this topic is therefore needed.
Interestingly, the rate of neonates requiring intensive care was higher in the group of mothers with previous TBI. This can partly be explained by the slightly higher rate of CS in this group, as the procedure is usually associated with an increased need for intensive care for the neonate [Citation24,Citation25]. Moreover, a notably higher rate of smokers in the TBI group partly explains the increase, but adjusted analysis with smoking status still showed higher odds for the need for intensive care for the neonate. We are unaware of previous studies that have examined the effects of a mother’s previous TBI on her offspring. TBIs are known to affect the menstrual cycle and severe head traumas during pregnancy are related to increased risk for fetal deaths [Citation9,Citation26]. Overall, high-energy traumas during pregnancy increased the risk for placental abruption and direct fetal injuries, which partly explains the increased risk for fetal deaths associated with TBI [Citation27]. The exact reason for the higher rate of neonatal intensive care in the group of mothers with previous TBI remains unknown.
The strength of our study is the large nationwide study population with a long study period, making it possible to compare large patient groups. The register data used in our study are routinely collected with structured forms with national instructions, which ensures good coverage and reduces possible reporting and selection bias [Citation28]. Furthermore, the coverage of both registers included in this study is high [Citation28,Citation29]. The advantage of this study compared to previous ones is the large national research material in a country with uniform delivery-related guidelines and attitudes.
The main limitation of our study is the missing clinical information on TBIs (e.g. radiological findings and TBI severity indices). As this information is not recorded to the registers, we could only use ICD-10 coding, which means that the severity of trauma-based on the length of the hospitalization period (non-admitted and admitted TBI patients) is only directive. It has to be kept in mind that TBI management has improved during the last two decades. This improvement in turn has ultimately reflected the diagnostic threshold of especially mild MTBI. Currently, mild injuries are identified more frequently among healthcare professionals and also the public has been sensitized to the possible lingering problems related to mild head injuries. This shift in clinical practice has most likely increased the number of reported TBI cases in Finland. Thus, the increasing TBI incidence among fertile-aged women can be partly explained by the alterations in national practice. Further, the contents of the birth register were updated in 2004 and 2017, and 5-min Apgar scores, durations of labor stages, body mass index and the chronic disease diagnosis of the mother were only included after 2004. Therefore, these clinical parameters were not analyzed in our study. Furthermore, since cases of CS were classified as elective or urgent prior to 2004, we have used the same classification in the present study instead of the newer three-stage classification (elective, urgent and emergency). In addition, the indications behind CS or instrumental vaginal delivery are not registered in the MBR, which means that indications for these remain unknown. Thus, it is unknown whether the patient had planned elective CS or attempted vaginal delivery before undergoing unplanned CS.
Conclusion
The incidence of TBI hospitalizations among fertile-aged women increased during our study period, whereas the incidence of TBI-related surgical operations remained stable. Preterm birth, CS, instrumental vaginal delivery and the use of labor analgesia were more frequent among mothers with a history of TBI. Furthermore, a slightly increased rate of neonates with impaired health was observed among women with previous TBI. Therefore, maternal history of TBI should be acknowledged as a possible factor affecting the delivery and health of the neonate.
Supplemental Material
Download Zip (353.1 KB)Disclosure statement
The authors have no conflicts of interest to report.
References
- Maas AIR, Menon DK, Adelson PD, et al. Traumatic brain injury: integrated approaches to improve prevention, clinical care, and research. Lancet Neurol. 2017;16(12):987–1048.
- Hyder AA, Wunderlich CA, Puvanachandra P, et al. The impact of traumatic brain injuries: a global perspective. NeuroRehabilitation. 2007;22(5):341–353.
- Ng SY, Lee AYW. Traumatic brain injuries: pathophysiology and potential therapeutic targets. Front Cell Neurosci. 2019;13:528.
- GBD 2016 Traumatic Brain Injury and Spinal Cord Injury Collaborators. Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990-2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol. 2019;18(1):56–87.
- Groswasser Z, Peled I. Survival and mortality following TBI. Brain Inj. 2018;32(2):149–157.
- Miller GF, Daugherty J, Waltzman D, et al. Predictors of traumatic brain injury morbidity and mortality: examination of data from the national trauma data bank: predictors of TBI morbidity & mortality. Injury. 2021;52(5):1138–1144.
- Koskinen S, Alaranta H. Traumatic brain injury in Finland 1991-2005: a nationwide register study of hospitalized and fatal TBI. Brain Inj. 2008;22(3):205–214.
- Ripley DL, Harrison-Felix C, Sendroy-Terrill M, et al. The impact of female reproductive function on outcomes after traumatic brain injury. Arch Phys Med Rehabil. 2008;89(6):1090–1096.
- Colantonio A, Mar W, Escobar M, et al. Women's health outcomes after traumatic brain injury. J Womens Health. 2010;19(6):1109–1116.
- Anto-Ocrah M, Cafferky V, Lewis V. Pregnancy after concussion: a clarion call for attention? J Head Trauma Rehabil. 2021.
- Tawfik MM, Badran BA, Eisa AA, et al. Simultaneous cesarean delivery and craniotomy in a term pregnant patient with traumatic brain injury. Saudi J Anaesth. 2015;9(2):207–210.
- Neville G, Kaliaperumal C, Kaar G. Miracle baby': an outcome of multidisciplinary approach to neurotrauma in pregnancy. BMJ Case Rep. 2012.
- Statistics Finland. History of official statistics of Finland – tilastolaitoksen historiaa. http://www.stat.fi/org/tilastokeskus/historia.html.
- Vuori EG. Perinatal statistics: Parturients, deliveries and newborns 2015. national institute of health and welfare; 2016.
- Gissler M, Teperi J, Hemminki E, et al. Data quality after restructuring a national medical registry. Scand J Soc Med. 1995;23(1):75–80.
- Perinatal statistics – parturients, delivers and newborns – THL. https://Thl.fi/fi/tilastot-ja-data/tilastot-aiheittain/seksuaali-ja-lisaantymisterveys/synnyttajatsynnytykset-ja-vastasyntyneet/perinataalitilasto-synnyttajat-synnytykset-ja-vastasyntyneet.
- von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–349.
- Greenland S, Pearl J, Robins JM. Causal diagrams for epidemiologic research. Epidemiology. 1999;10(1):37–48.
- VanderWeele TJ, Staudt N. Causal diagrams for empirical legal research: a methodology for identifying causation, avoiding bias and interpreting results. Law Probab Risk. 2011;10(4):329–354.
- Tagliaferri F, Compagnone C, Korsic M, et al. A systematic review of brain injury epidemiology in Europe. Acta Neurochir. 2006;148(3):255–268. discussion 268.
- Peeters W, van den Brande R, Polinder S, et al. Epidemiology of traumatic brain injury in Europe. Acta Neurochir. 2015;157(10):1683–1696.
- Brazinova A, Rehorcikova V, Taylor MS, et al. Epidemiology of traumatic brain injury in Europe: a living systematic review. J Neurotrauma. 2021;38(10):1411–1440.
- Legros B, Aesch B, Fournier P, et al. Head injury and pregnancy. Neurochirurgie. 2000;46(2):110–116.
- Kamath BD, Todd JK, Glazner JE, et al. Neonatal outcomes after elective cesarean delivery. Obstet Gynecol. 2009;113(6):1231–1238.
- Khasawneh W, Obeidat N, Yusef D, et al. The impact of cesarean section on neonatal outcomes at a university-based tertiary hospital in Jordan. BMC Pregnancy Childbirth. 2020;20(1):335–332.
- Kho GS, Abdullah JM. Management of severe traumatic brain injury in pregnancy: a body with two lives. Malays J Med Sci. 2018;25(5):151–157.
- Brown HL. Trauma in pregnancy. Obstet Gynecol. 2009;114(1):147–160.
- https://Thl.fi/en/web/thlfi-en/statistics/information-on-statistics/register-descriptions/newborns.
- Sund R. Quality of the Finnish hospital discharge register: a systematic review. Scand J Public Health. 2012;40(6):505–515.
