Abstract
Objective
Transient Osteoporosis of the Hip is a self-limiting disorder of severe hip joint pain presenting in pregnancy or postpartum, of which magnetic resonance imaging (MRI) is the modality of choice for diagnosis. Clinical data regarding transient osteoporosis of the hip is limited, precluding evidence-based decision-making such as recommended mode of delivery. In this case-series retrospective study, we aim to describe the natural course of transient osteoporosis of the hip during pregnancy and the postpartum period including implications of the mode of delivery.
Methods
All women diagnosed with unilateral/bilateral transient osteoporosis of the hip by MRI during pregnancy or postpartum between 2010 and 2019 at a single tertiary medical center were retrospectively studied. All MRI scans were reviewed by an experienced radiologist at the same single tertiary medical center. Data obtained from patients’ electronic medical records and telephone questionnaires included maternal baseline characteristics, obstetric history, and current pregnancy obstetric and clinical outcome characteristics. Outcomes of normal vaginal delivery (NVD) and cesarean delivery (CD) were compared and analyzed.
Results
Thirty-four women were diagnosed with unilateral or bilateral transient osteoporosis of the hip during pregnancy (17 women) and postpartum (17 women). The mean maternal age was 34.18 ± 4.75 years. A family history of osteoporosis was reported in a rate of 29.4%. The rate of smokers was 47.1%, 32.4% of pregnancies were conceived by in-vitro fertilization (IVF), pre-pregnancy and term body mass index (BMI) were 22.03 and 27.6, respectively. No significant differences were found between NVD and CD in all parameters evaluated. Of 15 women with a sequential pregnancy, two were diagnosed with transient osteoporosis of the hip (13.3%)
Conclusion
Women diagnosed with transient osteoporosis of the hip had advanced maternal age, low BMI, family history of osteoporosis, prevalent smoking and IVF pregnancies. Transient osteoporosis of the hip was bilateral in 25% and presented postpartum in 50% of cases. There was no significant difference in maternal outcomes between NVD and CD. Higher awareness of this potential diagnosis during pregnancy and postpartum may improve patient management and outcomes.
Introduction
Transient Osteoporosis of the Hip (TOH) most commonly affects middle-aged men and pregnant women, mainly manifesting in the second or third trimesters or during the early postpartum period [Citation1,Citation2]. TOH is one of several conditions known as Pregnancy-related Pelvic Girdle Pain [Citation3–6]. It is a self-limiting disorder characterized by severe non-traumatic joint pain, normal radiographs or osteopenia of the affected femoral head and neck and normal laboratory panels. It usually presents with sudden-onset hip pain, extending to the groin and the thigh, causing limping and disability gradually subsiding over time [Citation7–12]. A definitive etiology for the disorder in not established, yet several etiologies have been suggested such as pelvic nerve compression, vascular insufficiency, hormonal changes of pregnancy and lactation (such as relaxin) or changes in the fibrinolytic system associated with pregnancy [Citation1,Citation13,Citation14]. Known risk factors for TOH include immobility, severe dental problems and lack of exercise in childhood, alcohol consumption, smoking and corticosteroid treatment [Citation15,Citation16]. Magnetic resonance imaging (MRI) is the modality of choice for early diagnosis in which diffuse bone marrow edema involving the head and neck of the involved femur can be detected at onset and help in differentiating this diagnosis from avascular necrosis, infection and pelvic bone insufficiency fractures [Citation17–20]. Treatment is mainly conservative, consisting of prevention of damage to the weakened bones by reducing weight-bearing activities, physiotherapy, acupuncture and analgesic agents [Citation21], as well as the use of other medications such as bisphosphonates, vitamin D and calcium supplements [Citation16]. Suppression of bone resorption or induction of bone formation were suggested to reduce further damage, promote recovery, or shorten the duration of recovery [Citation16]. Rarely, orthopedic-surgical intervention is required [Citation22].
Symptoms usually resolve within the first two months postpartum, although occasionally longer duration has been reported [Citation9,Citation23,Citation24]. Recurrence in subsequent pregnancies has not been reported [Citation9].
Information regarding TOH, both in the field of gynecology and that of orthopedics, is scarce and mainly described in case reports and small case series. Literature regarding clinical implications and evidence-based decision-making is even more scarce. No previous research or review has evaluated the preferred mode of delivery for women with TOH, although some have reported that elective cesarean delivery (CD) was indicated due to severe hip pain and joint functional limitation and has been thought to protect women from birth-related injuries [Citation8,Citation9,Citation25].
In the current study, we aim to describe the natural course of TOH during pregnancy and postpartum in a large case series from a single tertiary center.
Methods
This retrospective case series study consists of all women diagnosed with unilateral or bilateral TOH by MRI scans during pregnancy or postpartum (up to 12 weeks from birth) between 2010 and 2019 at a single tertiary medical center.
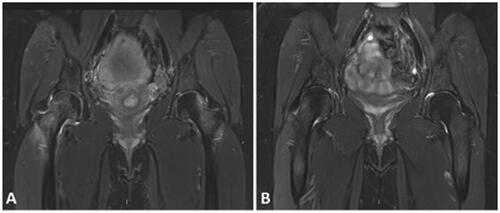
All MRI scans were reviewed by an experienced musculoskeletal radiologist for the presence of TOH as per the following definition – high signal intensity on T2 weighted (T2-w) with fat suppression sequences and low signal intensity on T1-weighted sequences of the femoral head and neck reaching the per-trochanteric area (an example is shown in ).
Figure 1. Coronal T2-W sequences of the pelvis of a 32 years old female, 1 week after vaginal delivery, with severe bilateral hip pain (A) and a follow-up image performed after 3 months (B). On presentation, there is bilateral bone marrow edema of the femoral head and neck (more severe on the right) compatible with bilateral transient osteoporosis (A). After 3 months there is almost complete resolution of the bone marrow edema with minor residual bone marrow edema on the right femoral head (B).
Patients in which alternative MRI diagnosis such as avascular necrosis, pelvic stress fracture, or symphysiolysis was given and patients who were lost to follow-up or had missing medical records were excluded.
Data were obtained from the medical center’s electronic health record and via telephone questionnaire in order to obtain postpartum medical information. Institutional review board approval for this retrospective review of the MRI images and medical records as well as for conducting a telephone interview was obtained (5888-19-SMC).
Baseline characteristics included maternal age, body mass index (BMI) before pregnancy and at term, comorbidities, past history of TOH, family history of osteoporosis (defined according to the World Health Organization, the WHO, criteria [Citation26]), exercise before puberty and dental problems in childhood (both defined as less than normal/normal/more than normal), smoking before and during pregnancy (defined as smoking at least one cigarette (or equivalent) per day) and alcohol consumption before and during pregnancy (for women, consuming more than 3 drinks on any day or more than 7 drinks per week - as defined by the National Institute of Alcohol Abuse and Alcoholism, the NIAAA [Citation27]).
Obstetric history characteristics included gravidity, parity, number of past CDs and number of past abortions. Current pregnancy obstetric history included mode of conception, gestational diabetes mellitus (GDM), gestational hypertensive disease (GH), mode of delivery, birth weight and neonatal complications (Apgar score lower than 5 < 7, need of mechanical ventilation, neonatal intensive care unit admissions). Clinical outcome characteristics included timing and gestational age of MRI and diagnosis of TOH, modality of treatment including the use of anticoagulants (Low-molecular-weight heparin (LMWH)), time for resolution of symptoms, and complications such as venous thromboembolism and edema or inflammation of lower limb. The necessity of treatment and the chosen modalities were decided upon by each patient-treating physician.
A comparison between patients who had a normal vaginal delivery (NVD) and those who underwent CD was performed. The comparative analysis included maternal demographics, gestational age of TOH diagnosis, treatment, duration of symptoms, complications, and rates of TOH in recurrent pregnancies.
Statistical analysis
The statistical analysis is mainly descriptive, with variables presented using the accepted method – quantitative variables by mean, standard deviation, minimum-maximum and interquartile range and ordinal variables by percentage and absolute number. A univariate analysis was performed by Chi-square for categorical variables. Normally distributed quantitative variables were compared by using independent-t-test and non-normally distributed quantitative variables were compared with non-parametric tests such as the Mann–Whitney test and Spearman test. Statistical analysis was performed using the SPSS Statistics 25v program (SPSS Inc., Chicago, IL), where the value of α > 0.05 was considered statistically significant.
Results
Between 2010 and 2019 a total of 131 women underwent hip or pelvic MRI due to pelvic girdle pain during pregnancy (27 women) or postpartum (104 women). Out of these, 49 women were diagnosed by MRI with TOH. After applying exclusion criteria, 34 women were diagnosed by MRI with TOH either during pregnancy (17 women, 50%) or postpartum (17 women, 50%). Nine women (26.5%) were diagnosed with bilateral TOH and 25 with unilateral TOH (73.5%).
Mean follow-up time after TOH diagnosis was 36 months.
Maternal characteristics are presented in . Mean maternal age was 34.18 ± 4.75 years, BMI, before pregnancy was 22.03 ± 3.18 kg/m2 and BMI at term, was 27.60 ± 5.02 kg/m2. 47.1% of women smoked and 2.9% of the women consumed alcohol.
Table 1. Demographic variables.
Medical history is shown in . A family history of osteoporosis was reported in 29.4% of cases. There was no notable prevalence of any co-morbidities or chronic medication use. Of note, none of the women in the cohort were breastfeeding at the time of the diagnosis and only one woman had previous hip trauma.
Table 2. Medical history.
Obstetric and neonatal characteristics are shown in . 64.7% of women conceived spontaneously and 32.4% by In-vitro fertilization (IVF). Pregnancy complications such as GDM or GH were rare (less than 5%). 47.1% of births were vaginal, including 35% NVD and 11.8% vacuum extraction (VE), and 47.1% of the births were CD. Of all CD’s, 31.2% were elective due to TOH, 18.8% were elective due to malpresentation and 50% were non-elective during a trial of vaginal birth. There were two cases (5.8%) of termination of pregnancies that were conducted after TOH diagnosis and were unrelated to TOH.
Table 3. Obstetric and neonatal variables.
TOH medical status is shown in . The MRI for diagnosis of TOH was performed during pregnancy in 50% and partum in 50% of cases. The mean gestational age for MRI performed during pregnancy was 29 weeks and 5 days. Treatment for TOH included physiotherapy (67.6% of all women), acupuncture (44.1%), analgesic medications (70.6%), Vitamin D (52.9%) and Calcium (38.2%). Anticoagulation medications (anti-thrombotic prophylaxis due to reduced mobilization) were used in 29.4% of patients. The mean length of treatment was 1.2 months during pregnancy and 2.9 months during the post-partum period. The mean timing of resolution of symptoms was 3.6 months after delivery. Of note, two women had symptoms for 12 months and one woman had symptoms for 24 months after delivery. A follow-up MRI confirming the resolution of findings was performed in 8 patients (23.5%). Complications were reported in 32.4% of the women − 2.9% had venous thromboembolism and 26.5% had edema or inflammation of a lower limb. In a mean follow-up of 36 months after TOH diagnosis, 15 women (44.1%) had a subsequent pregnancy, out of which two women (13.3%) were diagnosed with TOH in the sequential pregnancy.
Table 4. TOH clinical status.
A univariable sub-analysis regarding the timing of the resolution of symptoms was performed. The timing of resolution of symptoms was not significantly different whether TOH was unilateral or bilateral (p = .465), if physiotherapy or acupuncture was performed (p = .077 and p = .515, respectively), and was not affected by BMI at term (p = .536). A univariable sub-analysis regarding the mode of delivery was performed. The mode of delivery (NVD or CD) was not significantly different whether TOH was unilateral or bilateral (p = .220).
A sub-analysis of the comparison between NVD and CD is shown in . There were no significant differences between the groups in maternal demographics, gestational age of TOH diagnosis, treatment, length of symptoms, complications and rates of TOH in recurrent pregnancies.
Table 5. Comparison between normal vaginal delivery and cesarean delivery.
Discussion
This retrospective case-series study reports the maternal, obstetric and clinical characteristics and outcomes of 34 pregnant women diagnosed with TOH during pregnancy or postpartum.
The major findings of our study include the relatively advanced maternal age (mean maternal age was 34.18 ± 4.75 years), the high prevalence of family history of non-pregnancy related osteoporosis (29.4%), the high rates of smokers (47.1%) and pregnancies conceived by IVF (32.4%), as well as low BMI of the women pre-pregnancy and at term (22.03 and 27.60, accordingly). Nine women (26.5%) were diagnosed with bilateral TOH. Clinical outcomes were not significantly different between NVD and CD. Two women (13.3%) were diagnosed with TOH in a sequential pregnancy.
In our results, the mean maternal age was 34.18 ± 4.75 years, which is significantly more advanced than the mean maternal age of 30.5 years at delivery in the general population in Israel [Citation28]. In the review by Quaresima et al. [Citation9], the mean maternal age was 32.10 ± 5.50 years. However, Hadji et al. [Citation15] described 33 cases of TOH in which the mean maternal age was 35.20 ± 4.10 years.
Family history of osteoporosis (not pregnancy related) was reported in 29.4% of cases, much higher than the reported prevalence of osteoporosis in the Israeli population [Citation26], which was reported as 13.6% in 2003 [Citation29]. A family history of osteoporosis was not described in existing literature as a risk factor for TOH. This finding in our cohort is surprising considering the pathophysiology of both conditions is completely different, thus the relation between the two is unclear.
The proportion of smokers (47.1%) was remarkably high compared with known rates of smoking during pregnancy of only 6.7% in the United States in 2017 [Citation30]. Accordingly, smoking may be considered a major risk factor for TOH as shown in previous publications [Citation16].
The proportion of pregnancies conceived by IVF in our cohort (32.4%) is relatively high. In comparison, in 2018 only 5.1% of all births in Israel were conceived by IVF [Citation31]. This factor is yet to be reported or considered as a risk factor for TOH. Possible explanations for this finding may be the relatively high mean maternal age (34.18 ± 4.75 years) in our cohort and the medications used in IVF treatments, such as gonadotropins that have been previously described as risk factors for TOH [Citation8].
The BMI of the women in our cohort, both pre-pregnancy and at term (22.03 and 27.6, respectively), is relatively low compared to mean BMI values in the population (24.7 and 29.7, respectively) [Citation32–34]. This finding is contradictory to existing literature regarding increased body weight as a risk factor for TOH. Previous publications showed women with TOH presented with a 2 kg higher average body weight compared to women without TOH [Citation15]. Previous publications regarding non-transient osteoporosis have concluded that a higher BMI improves bone mineral density and thus reduces the risk of fractures, while a low BMI is a well-documented risk factor for osteoporotic fractures [Citation35].
Nine women (26.5%) were diagnosed with bilateral TOH. This high prevalence of bilateral TOH is of considerable clinical importance, meaning that recommendations such as weight-bearing reduction may be applicable to both limbs and thus early imaging and diagnosis are important.
Anticoagulation medications (anti-thrombotic prophylaxis due to reduced mobilization) were used in 29.4% of patients in our study. The anticoagulant used by these patients was LMWH, which is recommended as a first-line agent for the prevention of venous thromboembolism [Citation36]. Data regarding the osteopenic effect of this treatment is somewhat contradicting. Long-term LMWH prophylaxis in pregnancy for at least 3 months was associated with bone loss and fractures in some reports [Citation37,Citation38], although others have showed that the absolute risk of fracture in this population was small (1%–2%) [Citation39] and that decreases in bone mineral density of 2%–4% caused by the prophylactic doses of LMWH or unfractionated heparin were similar to the bone loss that occurs physiologically during pregnancy [Citation40,Citation41]. Research regarding longer use of LMWH on non-pregnant patients concluded that the use of LMWH for 3–6 months did not increase the risk of fractures, but longer exposure for up to 24 months was associated with a decrease in bone mineral density and thus higher risk of fractures [Citation41]. This data suggests that the use of LMWH for only several months, as used by the patients in our study, is not supposed to expose the patients to a higher risk of fractures. Nevertheless, the pros and cons of LMWH treatment, especially if intended for an extended period should be carefully evaluated before deciding to begin treatment.
Interestingly, when comparing NVD with CD, our results show there were no significant differences between the groups in maternal demographics, gestational age of TOH diagnosis, treatment, duration of symptoms, complications and rates of TOH in recurrent pregnancies. To the best of our knowledge, this is the first report of such a comparison. Hadji et al. [Citation15] reported that women with TOH had higher rates of elective CD compared with healthy women. Quaresima et al. [Citation9] showed that more than 70% of women with TOH were advised to undergo elective CD. In our cohort only 5 women (31.2%) were advised to undergo elective CD due to TOH, as the other cases of CD were either elective for reasons not related to TOH (maternal/obstetric) or were emergent CD’s during a trial of vaginal birth. CD rates were 50% of all reported deliveries in the review by Quaresima et al. [Citation9], similar to our cohort (47.1%). However, TOH was the reason for elective CD in 74.2% of all CDs in that report. This, perhaps, may be attributed to the accumulated experience with TOH patients in our medical center, along with high MRI scan availability, allowing NVD trials based on expert opinion. Our results may give clinicians the reassurance to allow pregnant women with TOH to try to deliver vaginally.
In regards to the timing of diagnosis, Quaresima et al. [Citation9] described only five cases (4%) diagnosed postpartum, whereas in our cohort there were 17 cases (50%). This may be attributed to high awareness for TOH diagnosis during postpartum in our medical center. Clinicians should be aware of hip joint pain in the postpartum period, especially considering that medical surveillance at this period is considerably lesser than during pregnancy, and consider performing an MRI scan in cases of severe ongoing pain.
Our study’s retrospective nature is an inherent limitation, restricting our ability to control for confounding factors. Another limitation is the lack of a respectively healthy control group. However, the aim of this study was not to compare women with TOH to healthy women but to understand the clinical and outcome trends within this cohort of pregnant women diagnosed with TOH.
To the best of our knowledge, this is the largest cohort of women diagnosed with TOH at a single medical center by a single experienced team of MRI radiologists. Furthermore, we obtained highly detailed clinical data regarding symptoms, treatment and outcome that may allow the drawing of clinical conclusions such as preferred mode of delivery.
Conclusion
Transient Osteoporosis of the Hip is a self-limiting disorder seen during pregnancy and postpartum.
Our cohort of women diagnosed with TOH was characterized by advanced maternal age and low BMI, a family history of osteoporosis, prevalent smoking and a high rate of pregnancies conceived by IVF. TOH was diagnosed bilaterally in 25% of cases and was diagnosed postpartum period in 50% of the cases. The mean resolution of symptoms was 3.6 months after delivery.
A trial of vaginal birth may be a valid option that does not expose pregnant women with TOH to negative outcomes compared with CD. Awareness of this potential diagnosis during pregnancy and postpartum is required. Further studies are needed in order to ratify the recommendations for ideal follow-up, treatment and clinical management of pregnancies complicated by TOH.
Ethical approval
Informed consent to participate in the study was obtained from all participants. The study was approved by the Sheba medical center Institutional review board - approval 5888-19-SMC.
Acknowledgements
The authors would like to thank Dr. Amit Meitus for her assistance in writing, reviewing and editing of this manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Sachsanidis P, Tartagni MV, Graf U. Recurrent transient osteoporosis during pregnancy and treatment with oral bisphosphonates: a case report. Open J Obstet Gynecol. 2017;7:1044–1051.
- Holzer I, Snir N, Ben-Galim P, et al. Transient osteoporosis of the hip: long-term outcomes in men and nonpregnant women. Curr Orthop Pract. 2009;20(2):161–163.
- Keriakos R, Bhatta SR, Morris F, et al. Pelvic girdle pain during pregnancy and puerperium. J Obstet Gynaecol. 2011;31(7):572–580.
- Kanakaris NK, Roberts CS, Giannoudis PV. Pregnancy-related pelvic girdle pain: an update. BMC Med. 2011;9:15.
- Geith T, Stellwag AC, E Müller P, et al. Is bone marrow edema syndrome a precursor of hip or knee osteonecrosis? Results of 49 patients and review of the literature. Diagn Interv Radiol. 2020;26(4):355–362.
- Curtiss PH, Kincaid WE. Transitory demineralization of the hip in pregnancy. A report of three cases. J Bone Joint Surg Am. 1959;41-A:1327–1333.
- Kyoko Kasahara NK, Kawasaki T, Morisaki S, et al. Bilateral femoral neck fractures resulting from pregnancy-associated osteoporosis showed bone marrow edema on magnetic resonance imaging. J Obstet Gynaecol Res. 2017;43(6):1067–1070.
- Kovacs CS, Ralston SH. Presentation and management of osteoporosis presenting in association with pregnancy or lactation. Osteoporos Int. 2015;26(9):2223–2241.
- Quaresima P, Angeletti M, Luziatelli D, et al. Pregnancy associated transient osteoporosis of the hip (PR-TOH): a non-obstetric indication to caesarean section. A case report with literature review. Eur J Obstet Gynecol Reprod Biol. 2021;262:28–35.
- Ververidis AN, Drosos GI, Kazakos KJ, et al. Bilateral transient bone marrow edema or transient osteoporosis of the knee in pregnancy. Knee Surg Sports Traumatol Arthrosc. 2009;17(9):1061–1064.
- Malizos KN, Zibis AH, Dailiana Z, et al. MR imaging findings in transient osteoporosis of the hip. Eur J Radiol. 2004;50(3):238–244.
- Emad Y, Ragab Y, El-Shaarawy N, et al. Transient osteoporosis of the hip, complete resolution after treatment with alendronate as observed by MRI description of eight cases and review of the literature. Clin Rheumatol. 2012;31(11):1641–1647.
- Goldsmith LT, Weiss G, Steinetz BG. Relaxin and its role in pregnancy. Endocrinol Metab Clin North Am. 1995;24(1):171–186.
- Kovacs CS, Kronenberg HM. Maternal-fetal calcium and bone metabolism during pregnancy, puerperium, and lactation. Endocr Rev. 1997;18(6):832–872.
- Hadji P, Boekhoff J, Hahn M, et al. Pregnancy-associated transient osteoporosis of the hip: results of a case-control study. Arch Osteoporos. 2017;12(1):11.
- Asadipooya K, Graves L, Greene LW. Transient osteoporosis of the hip: review of the literature. Osteoporos Int. 2017;28(6):1805–1816.
- Klontzas ME, Vassalou EE, Zibis AH, et al. MR imaging of transient osteoporosis of the hip: an update on 155 hip joints. Eur J Radiol. 2015;84(3):431–436.
- Yamaguchi R, Yamamoto T, Motomura G, et al. Radiological morphology variances of transient osteoporosis of the hip. J Orthop Sci. 2017;22(4):687–692.
- Bloem JL. Transient osteoporosis of the hip: MR imaging. Radiology. 1988;167(3):753–755.
- Hayes CW, Conway WF, Daniel WW. MR imaging of bone marrow edema pattern: transient osteoporosis, transient bone marrow edema syndrome, or osteonecrosis. Radiographics. 1993;13(5):1001–1011; discussion 1012.
- Cohen I, Melamed E, Lipkin A, et al. Transient osteoporosis of pregnancy complicated by a pathologic subcapital hip fracture. J Trauma. 2007;62(5):1281–1283.
- Wright EV, Naqvi AZ, Syed S, et al. Transient osteoporosis of the hip in pregnancy: the orthopaedic management of bilateral neck of femur fractures in the third trimester. BMJ Case Rep. 2021;14(3):e238659.
- Paiva F, Simões N, Pereira D, et al. Idiopathic transient osteoporosis during pregnancy – report of a clinical case. J Orthop Case Rep. 2020;9(6):54–57.
- Bircher C, Afors K, Bircher M. Transient osteoporosis of the hip in pregnancy resulting in bilateral fracture of the neck of the femur. Int J Gynaecol Obstet. 2012;116(2):176–177.
- Venturella R, Quaresima P, Micieli M, et al. Non-obstetrical indications for cesarean section: a state-of-the-art review. Arch Gynecol Obstet. 2018;298(1):9–16.
- Salari N, Ghasemi H, Mohammadi L, et al. The global prevalence of osteoporosis in the world: a comprehensive systematic review and meta-analysis. J Orthop Surg Res. 2021;16(1):609.
- NIAAA. NIAAA – Drinking levels defined; 2020. Available from: https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking
- Statistics CBo. Births and fertility in Israel, 2020; 2022. Available from: https://www.cbs.gov.il/he/mediarelease/DocLib/2022/062/01_22_062b.pdf
- Nitzan-Kaluski D, Chinich A, Ifrah A, et al. Correlates of osteoporosis among Jewish and Arab women aged 45–74 in Israel: national women’s health interview survey. J Gend Specif Med. 2003;6(1):17–23.
- Azagba S, Manzione L, Shan L, et al. Trends in smoking during pregnancy by socioeconomic characteristics in the United States, 2010-2017. BMC Pregnancy Childbirth. 2020;20(1):52.
- Health IMo. In vitro fertilization (IVF) treatments in Israel 1990–2018; 2018. Available from: https://www.health.gov.il/PublicationsFiles/IVF1990-2018.pdf
- Keinan-Boker L, Noyman N, Chinich A, et al. Overweight and obesity prevalence in Israel: findings of the first national health and nutrition survey (MABAT). Isr Med Assoc J. 2005;7(4):219–223.
- Hochner H, Friedlander Y, Calderon-Margalit R, et al. Associations of maternal prepregnancy body mass index and gestational weight gain with adult offspring cardiometabolic risk factors: the Jerusalem perinatal family follow-up study. Circulation. 2012;125(11):1381–1389.
- Kundu S, Kaukemueller L, von Kaisenberg C, et al. Influence of maternal BMI and maternal weight gain during pregnancy on maternal and perinatal outcome – a retrospective data analysis of pregnancies during 2004 and 2014. Int J Womens Health Wellness. 2019;5:095.
- Cummings SR, Nevitt MC, Browner WS, et al. Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med. 1995;332(12):767–773.
- Garcia DA, Baglin TP, Weitz JI, et al. Parenteral anticoagulants: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141(2 Suppl):e24S–e43S.
- Ensom MH, Stephenson MD. Low-molecular-weight heparins in pregnancy. Pharmacotherapy. 1999;19(9):1013–1025.
- Greer IA, Nelson-Piercy C. Low-molecular-weight heparins for thromboprophylaxis and treatment of venous thromboembolism in pregnancy: a systematic review of safety and efficacy. Blood. 2005;106(2):401–407.
- Le Templier G, Rodger MA. Heparin-induced osteoporosis and pregnancy. Curr Opin Pulm Med. 2008;14(5):403–407.
- Backos M, Rai R, Thomas E, et al. Bone density changes in pregnant women treated with heparin: a prospective, longitudinal study. Hum Reprod. 1999;14(11):2876–2880.
- Gajic-Veljanoski O, Phua CW, Shah PS, et al. Effects of long-term low-molecular-weight heparin on fractures and bone density in non-pregnant adults: a systematic review with meta-analysis. J Gen Intern Med. 2016;31(8):947–957.
