Abstract
Background
During the lockdown due to COVID-19 pandemic, utilization of emergency care units has been reported to be reduced for obstetrical and gynaecological reasons. The aim of this systematic review is to assess if this phenomenon reduced the rate of hospitalizations for any reason and to evaluate the main reasons for seeking care in this subset of the population.
Methods
The search was conducted using the main electronic databases from January 2020 to May 2021. The studies were identified with the use of a combination of: “emergency department” OR “A&E” OR “emergency service” OR “emergency unit” OR “maternity service” AND “COVID-19” OR “COVID-19 pandemic” OR “SARS-COV-2” and “admission” OR “hospitalization”. All the studies that evaluated women going to obstetrics & gynecology emergency department (ED) during the COVID-19 pandemic for any reason were included.
Results
The pooled proportion (PP) of hospitalizations increased from 22.7 to 30.6% during the lockdown periods, in particular from 48.0 to 53.9% for delivery. The PP of pregnant women suffering from hypertensive disorders increased (2.6 vs 1.2%), as well as women having contractions (52 vs 43%) and rupture of membranes (12.0 vs 9.1%). Oppositely, the PP of women having pelvic pain (12.4 vs 14.4%), suspected ectopic pregnancy (1.8 vs 2.0), reduced fetal movements (3.0 vs 3.3%), vaginal bleeding both for obstetrical (11.7 vs 12.8%) and gynecological issues (7.4 vs 9.2%) slightly reduced.
Conclusion
During the lockdown, an increase in the proportion of hospitalizations for obstetrical and gynecological reasons has been registered, especially for labor symptoms and hypertensive disorders.
Introduction
In 2020, SARS-COV-2 infection spread from China to all over the world, causing a pandemic. The first and most important consequence had been that countries started to reorganize their health resources in order to face the increased request for care and management of COVID-19 ill people [Citation1]. In this regard, many subspecialty societies and expert consensus released guidelines and position papers with the aim both of evaluating the direct impact of the infection on specific diseases and of stating to stop all non-urgent medical and surgical treatments [Citation2–6]. The latter advice served to reduce the usual crowding of hospitals and healthcare settings, which were deemed as a potential route of contagion. Accordingly, governments decided on a strict lockdown, lasting differently among nations based on the local spread of SARS-COV-2 pandemic. As forecasted [Citation7], the impact on maternal-fetal wellness and obstetric care has been very tough, and pregnancy is considered a risk factor for a severe course of COVID-19 [Citation8,Citation9]. Moreover, SARS-COV-2 infection during pregnancy is associated with modifications in pregnancy management [Citation10,Citation11], an increase in adverse pregnancy outcomes [Citation12–14], the need for hospitalization [Citation15] and delivery in more than 50% of affected cases [Citation16]. In this scenario, we observed an important decrease in the number of Emergency Unit accesses for obstetric care in our university hospital of Naples during the first lockdown, as proof of previously excessive use of such healthcare resource settings by pregnant women [Citation17]. Thus, the pandemic raises the question of the importance of counseling in maternal-fetal medicine to allow pregnant women to learn when emergency care is needed [Citation18,Citation19]. The aim of this systematic review was to evaluate whether the hospitalization rate for obstetrics and gynecology conditions was changed during the pandemic and to assess the spectrum of conditions for which care was required.
Materials and methods
Study protocol
The review was performed according to a protocol recommended for systematic review. The study was reported according to the Preferred Reporting Item for Systematic Reviews and Meta-analyses (PRISMA) statement [Citation20]. The review protocol was designed a priori, defining methods for collecting, extracting and analyzing data. All review stages were conducted independently by three authors. In particular, three authors independently assessed electronic search, eligibility of the studies, inclusion criteria, risk of bias, data extraction and data analysis. Disagreements were resolved by discussion with senior authors.
Literature search and study selection
The literature search was conducted using MEDLINE, Embase, Web of Sciences, Scopus, ClinicalTrial.gov, OVID and Cochrane Library as electronic databases. The studies were identified with the use of a combination of the following text words from January 2020 to May 2021: “emergency department”; “A&E” OR “emergency service”; “emergency unit”; “maternity service”; “COVID-19”; “COVID-19 pandemic”; “SARS-COV-2”; “admission”; “hospitalization”. A review of articles also included the abstracts of all references retrieved from the search. Duplications were removed using Endnote online software and also manually.
We included in our systematic review all randomized and non-randomized studies that evaluated the population of women going to Obstetrics & Gynecology Emergency Department during the period of COVID-19 pandemic for any reasons; studies considering specifically obstetrical and delivery outcomes without mentioning the rate of admissions/hospitalization were excluded.
Risk of bias assessment
The risk of bias and quality assessment of the included studies were performed using the Newcastle-Ottawa Scale (NOS) [Citation21]. The NOS score was used to evaluate the included studies, and judgment on each one was passed according to three issues: selection of the study group, comparability between groups, and ascertainment of exposed/not exposed cohorts.
Data extraction and analysis
Data were extracted from the included studies without modifications. The main data extracted for our systematic review were: obstetrical and or gynecological emergency department access rate; hospitalization rate; any reasons (indications) for seeking emergency obstetrical or gynecological consultation.
The proportion of hospitalizations and any reasons for seeking emergency obstetrical or gynecological consultation was calculated for both lockdown and control periods. In particular, each proportion was calculated as the number of events by the total access to the obstetrical and or gynecological emergency department. Proportions were calculated for each included study as a pooled estimate and graphically reported on forest plots with 95% confidence interval (CI). All analyses were performed by adopting the random effect model of DerSimonian and Laird. Quantitative analysis was carried out only when at least three studies considered one of the variables of interest.
Statistical heterogeneity among included studies was evaluated by the inconsistency index I2, as previously described [Citation22–24]. In detail, heterogeneity was classified as: null for I2 = 0%, minimal for I2 b 25%, low for I2 b 50%, moderate for I2 b 75% and high for I2 ≥ 75%. Comprehensive Meta-Analysis (Biostat,14 North Dean Street, Englewood, NJ 07631, USA) and Review Manager 5.3 (Copenhagen: The Nordic Cochrane Center, Cochrane Collaboration, 2014) were used as data analysis software.
Results
Study selection and study characteristics
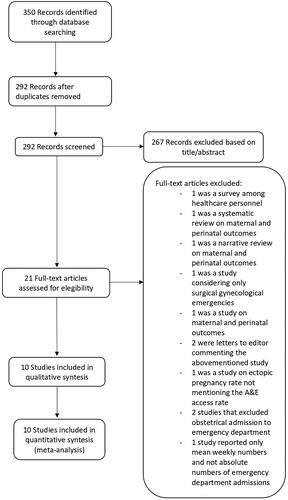
A total of 350 articles were initially identified by the search; of these, 58 articles were duplications and thus removed. The titles and abstracts of 292 articles were scrutinized and ultimately 21 were selected for full-text retrieval and eligibility assessment. After the exclusion of studies not meeting the selection criteria, 10 studies [Citation17,Citation25–33] were included in the systematic review and meta-analysis analyses ().
The general features of the studies and the risk of bias are illustrated in . Two studies were performed in the USA [Citation25,Citation33], one in France [Citation26], one in India [Citation30], two in Israel [Citation31,Citation32] and four in Italy [Citation17,Citation27–29]. Apart from the study by Goyal et al. [Citation30], which was prospective, the others were retrospective case-control analyses. Athiel et al. [Citation26] performed a multicenter study considering almost 40 thousand women. The time periods considered varied across countries, according to local pandemic waves, and the observations were of around one month for 4 studies [Citation27,Citation28,Citation32,Citation33], around two months for 2 studies [Citation25,Citation31], three months for 2 studies [Citation17,Citation26], and five months for other 2 studies [Citation29,Citation30].
Table 1. Features of the included studies.
Synthesis of the results
Evaluable outcomes from included studies are reported in , while pooled proportions are detailed in . The pooled proportion of hospitalizations for any obstetrical or gynecological issue increased from 22.7% to 30.6% during the lockdown periods and in particular from 48.0% to 53.9% for delivery. In detail, looking at the main indications for seeking emergency care, we observed that the pooled proportion of pregnant women suffering from hypertensive disorders increased (2.6% vs 1.2%), as well as women having impending labor (52% vs 43%) and premature rupture of membranes (12.0% vs 9.1%). Oppositely, we found that the proportion of women having pelvic pain (12.4% vs 14.4%), suspected ectopic pregnancy (1.8% vs 2.0%), reduced fetal movements (3.0 vs 3.3%) slightly reduced, as well as vaginal bleeding both for obstetrical (11.7%vs 12.8%) and gynecological issues (7.4% vs 9.2%).
Table 2. Outcomes of the included studies.
Table 3. Pooled proportions for the outcomes of interest.
Discussion
Main findings
During the lockdown periods, despite a reduction was noticed in the overall number of people seeking care for obstetrical and/or gynecological reasons, access to the obstetrical and gynecological emergency unit led to more frequent hospitalizations, especially for delivery, with either uterine contractions or rupture of membranes, and especially for hypertensive disorders which were found increased in comparison to the previous year or control periods.
Strength and limitations
As far as we know, this represents the first pooled analysis for the evaluation of hospitalizations for obstetrical and/or gynaecological reasons during the lockdown for COVID-19. The main strengths of our analysis are the adherence to PRISMA guidelines and the large number of outcomes considered. Limitations of our study may be the retrospective designs and wide heterogeneity among studies, both in the outcomes evaluated and in the definitions for different outcomes, because of which sometimes it was not possible to cumulate the data. In fact, populations from different countries in the included studies might have different variances; this might underlie the wide heterogeneity among the studies which we found.
Interpretation of the study findings, clinical and research implications
In a previous study, we observed an overall reduction in the number of obstetrics and gynecology emergency visits during the lockdown period [Citation17]. Moreover, we demonstrated that pregnant women refused to perform prenatal invasive diagnosis procedures, despite the number of deliveries remaining constant and even increasing during the lockdown, as proof that women were coming to the hospital when there were no other options [Citation10]. In line with the latter observation, we found the same phenomenon in this pooled analysis, with an increase in the number of hospitalizations, especially for labour symptoms and hypertensive disorders during pregnancy. Considering that contractions and vaginal discharge are among the most common reasons for seeking emergency visits, the finding of increased hospitalizations for these conditions during the lockdown might be explained as proof of an overall reduction in the number of unnecessary visits for unclear conditions, which were the cause of overwhelming of emergency units. Therefore, patients requested medical attention only when labor symptoms were truly specific and the need was real. Hypertensive disorders were found to increase by the studies which analyzed this item, and an explanation could be found in the more sedentary lifestyle imposed during the lockdown, as well as in the eventual reduction in the antenatal care appointments, with the consequence of missed antenatal screenings, although this has not been directly demonstrated. Vaccinal programs are now in place to reduce the burden of SARS-CoV-2 infection, although the propensity seems not very high, especially among obstetrical populations [Citation34–37]. Blakeway et al. [Citation38] observed that less than one-third accepted COVID-19 vaccination during pregnancy, with similar pregnancy outcomes compared with unvaccinated pregnant women, and a recent meta-analysis confirmed these results [Citation39]. Given that time is still needed to reduce the spread of the SARS-CoV-2 infection and the achievement of herd immunity, it is very important to control people's anxiety [Citation40,Citation41] with continuous information regarding the safety of vaccines against SARS-CoV-2 and proper utilization of healthcare resources, starting from seeking care when truly needed, both avoiding to go to the hospital for non-urgent conditions and not underestimating symptoms of illness due to fear of contagion, therefore risking a worsening of the disease. In this regard, more data are awaited on the safety of vaccines in pregnant women to help the decision-making process. In the meanwhile, many guidelines have been released on the management of COVID-19-affected pregnant women [Citation42]. Also, the role of general practitioners appears of utmost importance, being the first medical resource to which usually people refer before going to hospitals.
Conclusion
During the lockdown, an increase in the proportion of hospitalizations for obstetrical and gynecological reasons has been registered, especially for labour symptoms and hypertensive disorders. Further studies on the safety of vaccines against SARS-CoV-2 would probably help to normalize the unnecessary request for medical care and access to emergency units.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Jardine J, Relph S, Magee LA, et al. Maternity services in the UK during the COVID-19 pandemic: a national survey of modifications to standard care. BJOG. 2021;128(5):880–889.
- Franchi M, Bosco M, Garzon S, et al. Management of obstetrics and gynaecological patients with COVID-19. Italian J Obstet Gynecol. 2020;32(1):6–19.
- Carbone IF, Conforti A, Farina A, et al. A practical approach for the management of obstetric and infertile women during the phase two of the novel coronavirus disease 2019 (COVID-19) pandemic. Eur J Obstet Gynecol Reprod Biol. 2020;251:266–267.
- Rasmussen SA, Smulian JC, Lednicky JA, et al. Coronavirus disease 2019 (COVID-19) and pregnancy: what obstetricians need to know. Am J Obstet Gynecol. 2020; 222(5):415–426.
- Picarelli S, Conforti A, Buonfantino C, et al. IVF during coronavirus pandemic: who comes first? The POSEIDON viewpoint. It Journ Gyn Obs. 2020;32(04):223–228.
- Alviggi C, Esteves SC, Orvieto R, et al. COVID-19 and assisted reproductive technology services: repercussions for patients and proposal for individualized clinical management. Reprod Biol Endocrinol. 2020; 18(1):45.
- Putra M, Kesavan M, Brackney K, et al. Forecasting the impact of coronavirus disease during delivery hospitalization: an aid for resource utilization. Am J Obstet Gynecol MFM. 2020;2(3):100127.
- Oakes MC, Kernberg AS, Carter EB, et al. Pregnancy as a risk factor for severe coronavirus disease 2019 using standardized clinical criteria. Am J Obstet Gynecol MFM. 2021; 3(3):100319.
- Sakowicz A, Ayala AE, Ukeje CC, et al. Risk factors for severe acute respiratory syndrome coronavirus 2 infection in pregnant women. Am J Obstet Gynecol MFM. 2020;2(4):100198.
- Carbone L, Raffone A, Sarno L, et al. Invasive prenatal diagnosis during COVID-19 pandemic. Arch Gynecol Obstet. 2022;305 (3):797–801.
- Carbone L, Esposito R, Raffone A, et al. Proposal for radiologic diagnosis and follow-up of COVID-19 in pregnant women. J Matern Fetal Neonatal Med. 2022;35:(15):3002–3003.
- WAPM (World Association of Perinatal Medicine) Working Group on COVID-19. Maternal and perinatal outcomes of pregnant women with SARS-CoV-2 infection. Ultrasound Obstet Gynecol. 2021; 57(2):232–241.
- Di Girolamo R, Khalil A, Alameddine S, et al. Placental histopathology after SARS-CoV-2 infection in pregnancy: a systematic review and meta-analysis. American Journal of Obstetrics & Gynecology MFM. 2021;3(6):100468.
- Carbone L, Conforti A, LA Marca A, et al. The negative impact of most relevant infections on fertility and assisted reproduction technology. Minerva Obstet Gynecol. 2022;74(1):83–106.
- Vega M, Hughes F, Bernstein PS, et al. From the trenches: inpatient management of coronavirus disease 2019 in pregnancy. Am J Obstet Gynecol MFM. 2020;2(3):100154.
- Pierce-Williams RAM, Burd J, Felder L, et al. Clinical course of severe and critical coronavirus disease 2019 in hospitalized pregnancies: a United States cohort study. Am J Obstet Gynecol MFM. 2020;2(3):100134.
- Carbone L, Raffone A, Travaglino A, et al. Obstetric A&E unit admission and hospitalization for obstetrical management during COVID-19 pandemic in a third-level hospital of Southern Italy. Arch Gynecol Obstet. 2022;305:(4):859–867.
- Kaimal A, Norton ME, Society for Maternal-Fetal Medicine (SMFM). Electronic address: [email protected] for Maternal-Fetal medicine consult series #55: counseling women at increased risk of maternal morbidity and mortality. Am J Obstet Gynecol. 2021;224(4):B16–B23.
- Di Mascio D, Buca D, Berghella V, et al. Counseling in maternal-fetal medicine: SARS-CoV-2 infection in pregnancy. Ultrasound Obstet Gynecol. 2021; 57(5):687–697.
- Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700.
- Wells G, Shea B, O’Connell D, et al. Quality assessment scales for observational studies. Ottawa Health Research Institute. 2004. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm
- Travaglino A, Raffone A, Mollo A, et al. TCGA molecular subgroups and FIGO grade in endometrial endometrioid carcinoma. Arch Gynecol Obstet. 2020; 301(5):1117–1125.
- Travaglino A, Raffone A, Saccone G, et al. Congruence between 1994 WHO classification of endometrial hyperplasia and endometrial intraepithelial neoplasia system. Am J Clin Pathol. 2020;153(1):40–48.
- Travaglino A, Raffone A, Stradella C, et al. Impact of endometrial carcinoma histotype on the prognostic value of the TCGA molecular subgroups. Arch Gynecol Obstet. 2020;301(6):1355–1363.
- Abel MK, Alavi MX, Tierney C, et al. Coronavirus disease 2019 (COVID-19) and the incidence of obstetric and gynecologic emergency department visits in an integrated health care system. Obstet Gynecol. 2021;137(4):581–583.
- Athiel Y, Civadier MS, Luton D, et al. Impact of the outbreak of SARS-CoV-2 infection on urgent gynecological care. J Gynecol Obstet Hum Reprod. 2020;49(8):101841.
- Salsi G, Seidenari A, Diglio J, et al. Obstetrics and gynecology emergency services during COVID-19 pandemic. Am J Obstet Gynecol. 2020;2(4):100214.
- Grandi G, Del Savio MC, Caroli M, et al. The impact of COVID-19 lockdown on admission to gynecological emergency departments: results from a multicenter Italian study. Int J Gynecol Obstet. 2020;151(1):39–42.
- Dell’Utri C, Manzoni E, Cipriani S, et al. Effects of SARS cov-2 epidemic on the obstetrical and gynecological emergency service accesses. What happened and what shall we expect now? European J Obstet Amp 2020;254:64–68.
- Goyal M, Singh P, Singh K, et al. The effect of the COVID‐19 pandemic on maternal health due to delay in seeking health care: experience from a tertiary center. Int J Gynaecol Obstet. 2021;152(2):231–235.
- Meyer R, Levin G, Hendin N, et al. Impact of the COVID-19 outbreak on routine obstetrical management. Isr Med Assoc J. 2020;22(8):483–488.
- Kugelman N, Lavie O, Assaf W, et al. Changes in the obstetrical emergency department profile during the COVID-19 pandemic. J Matern Fetal Neonatal Med. 2022;35:(21):4116–4122.
- Spurlin EE, Han ES, Silver ER, et al. Where have all the emergencies gone? The impact of the COVID-19 pandemic on obstetric and gynecologic procedures and consults at a New York city hospital. J Minim Invasive Gynecol. 2021;28(7):1411–1419.e1.
- Carbone L, Mappa I, Sirico A, et al. Pregnant women perspectives on SARS-COV-2 vaccine: condensation: most of Italian pregnant women would not agree to get the SARS-COV-2 vaccine, irrespective of having features of high risk themselves, or being high-risk pregnancies. Am J Obstet Gynecol MFM. 2021;3(4):100352.
- Mappa I, Luviso M, Distefano FA, et al. Women perception of SARS-CoV-2 vaccination during pregnancy and subsequent maternal anxiety: a prospective observational study. J Matern Fetal Neonatal Med. 2022;35(25):6302–6305.
- Sutton D, D'Alton M, Zhang Y, et al. COVID-19 vaccine acceptance among pregnant, breastfeeding, and nonpregnant reproductive-aged women. Am J Obstet Gynecol MFM. 2021; 3(5):100403.
- Carbone L, Di Girolamo R, Mappa I, et al. Worldwide beliefs among pregnant women on SARS-CoV-2 vaccine: a systematic review. Eur J Obstet Gynecol Reprod Biol. 2022;268:144–164.
- Blakeway H, Prasad S, Kalafat E, et al. COVID-19 vaccination during pregnancy: coverage and safety. Am J Obstet Gynecol. 2022;226(2):236.e1–236.e14.
- Carbone L, Trinchillo MG, Di Girolamo R, et al. COVID-19 vaccine and pregnancy outcomes: a systematic review and meta-analysis. Intl J Gynecology & Obste. 2022;159(3):651–661.
- Esposito V, Rania E, Lico D, et al. Influence of COVID-19 pandemic on the psychological status of infertile couples. Eur J Obstet Gynecol Reprod Biol. 2020;253:148–153.
- Di Mascio D, Saccone G, D'Antonio F, et al. Psychopathology associated with coronavirus disease 2019 among pregnant women. Am J Obstet Gynecol MFM. 2021;3(1):100290.
- Di Girolamo R, Khalil A, Rizzo G, et al. Systematic review and critical evaluation of quality of clinical practice guidelines on the management of SARS-CoV-2 infection in pregnancy. Am J Obstet Gynecol MFM. 2022;4(5):100654.