Abstract
Background
Some newborns require acute transport to a Neonatal Intensive Care Unit (NICU) due to unpredicted or unpredictable reasons.
Objective
To describe the activity of the Neonatal Emergency Transport Service (NETS) in Northeast Italy.
Methods
An observational retrospective study was performed between 1 January 2018, and 31 December , 2019.
Results
A total of 133 transports were collected, with a neonatal transport index of 1.4%. Infants ≤2500 grams were more frequently transferred by NETS than those in the normal group (n = 34/563, 6.0% vs. n = 99/8,437, 1.2%; p < .001). The incidence of preterm birth among transferred newborns was 42/133 (31.6%). For the newborns with >2500 grams, there was a low incidence of a cesarean birth compared to vaginal delivery (23.2% versus 63.5%; p = .001), while the percentages were reversed in the group of infants ≤2500 grams (67.7% versus 20.6%) (p = .001). Infant stabilization time was higher in the underweight group compared to those weighed >2500 grams (31.5 versus 23.0 min; p < .001), as well as the median length of stay in NICU (18.0 versus 8.0 days, respectively, p < .001). The group of infants ≤2500 grams received more intravenous therapy (47.1% vs. 26.2%) and invasive ventilation (26.5% vs. 8.1%), compared to the group of infants who weighed >2500 grams.
Conclusions
This study described a local reality by showing the characteristics of the neonatal transports that took place in a metropolitan area in Northeast Italy. Wider database is necessary to achieve a better knowledge in the field of perinatal outcomes.
Introduction
Neonatal transport is required when a newborn needs care that cannot be provided in the referral center. Since it represents an additional risk factor for a critically ill neonate, it should be performed, when possible, by a well-organized neonatal transport service.
In utero transfer is universally recognized as the most effective and safe way to guarantee both the pregnant woman and the newborn the most qualified assistance so as to minimize risks for both the mother and the neonate [Citation1–5]. Although maternal antenatal transport is the preferred option, this method is not always feasible and some infants inevitably need urgent transport to a Neonatal Intensive Care Unit (NICU) after birth [Citation1,Citation4–6]. Data suggest that about 30% of serious pathologies arising during labor are not preventable and that 1-2% of births require a neonatal resuscitation and intensive or sub-intensive care in a completely unexpected way [Citation4]. On these grounds, there will always be a number of neonates who need to be transferred due to unpredicted or unpredictable reasons [Citation1].
At global level, the major causes of neonatal deaths are infections, prematurity, asphyxia (birth asphyxia) and congenital anomalies [Citation7–11]. Although neonatal transport represents an additional risk factor for a critically ill neonate, especially for very preterm infants [Citation1], the ability to safely transfer a sick newborn to a health facility with a higher level of care could avoid many neonatal deaths and reduce neonatal morbidity [Citation9,Citation12]. Furthermore, the timely activation of the Neonatal Emergency Transport Service (NETS) allows the newborn, on the one hand, to receive already at birth and on-site specialist care and, on the other hand, to be transferred in the very first hours of life to appropriate facilities for intensive neonatal care [Citation1,Citation5]. Patient stabilization is an essential condition for adequate transport, regardless of transport time or distance [Citation13]. The optimal stabilization time, including waiting times at referral sites, can be quite variable [Citation14]. This is due to the fact that stabilization periods in neonatal transports depend on several factors including illness severity, need for procedures, and availability of local resources as well as the capacity of the appropriate care facility [Citation15].
The presence of a well-organized NETS is mandatory for a perinatal regional network since it represents the link between birth centers and NICUs and can reduce the risks associated with transportation, especially for very preterm infants [Citation1]. The aim of this study is to describe NETS in a regional metropolitan area by showing the characteristics of the neonatal transports that took place from 2018 to 2019.
Materials and methods
Study design
An observational retrospective study was adopted; it included all newborns who were treated by the NETS from 1 January 2018, to 31 December 2019. This period was chosen as preexisting data were available, even if originally collected for reasons other than research. Data were reported here according to the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) statements to improve truthfulness and ensure clarity [Citation16].
Setting and study population
Friuli Venezia Giulia, a region in the northeast of Italy, is an area of 1,215,000 inhabitants (1 January 2020). As the Italian National Health System is highly decentralized, significant regional differences in access to and quality of healthcare services have been reported in the past years [Citation1]. However, the agreement of the State-Regions Conference in December 2010 (also known as “Birth Pathway”) provided guidance to standardize pregnancy and childbirth practices at the regional level, including the adoption of perinatal networks based on the hub and spoke organizational model that guarantees the presence of maternal and NETS [Citation3]. Information regarding NETS organization is reported in .
Table 1. NETS organization.
As part of the regional routine prenatal service, all symptomless women with low-risk pregnancies are registered for a planned delivery at any hospital in the Friuli Venezia Giulia Region. Those who experience complications at childbirth (e.g. premature rupture of membranes, abruptio placentae) need transporting the newborn infant to the NICU. In the Region, two NICUs are available in two centers. These hospitals are formally recognized second level maternity units (defined by the Italian Ministry of Health as facilities with >1000 annual births and equipped with a NICU) [Citation17]. About 130 miles outside the Region is a third-level hospital with highly skilled personnel and advanced technical tools that serves as the national standard for neonatal treatment.
The researchers of this study conducted a retrospective analysis of data available in the second-level facility in Udine, whose NICU targets over 600,000 inhabitants with a total of about 4500 births/year.
Data collection and outcome measures
Study data were obtained from the internal database of the NETS, which was hosted by the NICU of Udine Academic Hospital, where every neonatal transport is registered. The NICU medical director extracted the pertinent data that were stored on a weekly basis by the head nurse. Additional demographic data were also obtained from governmental sources (ISTAT, Istituto Nazionale di Statistica – the Italian Statistics Institute, available at http://www.istat.it/).
The outcome measures of the study included variables at a) infant-level, such as low birth weight, that is to say infants whose weigh was 2500 grams or less at birth, gestational age (GA) at birth (weeks), the reason for transport (e.g. respiratory failure), Apgar score (at 1- and 5-min), type of birth (e.g. vaginal delivery), length of stay (LOS) in NICU (days) and NICU survival; and b) transport-level, such as NETS response time interval (defined as the time lag between an initial emergency call and arrival of the transport team at the patient’s bedside, in minutes), infant stabilization time (minutes), return time (minutes), overall transport time (minutes), and intervention(s) during the transport (e.g. intravenous therapy).
The worldwide standard cutoff weight for identifying low birth weight infants at high mortality risk is 2500 grams [Citation18].
Statistical analysis
Data from all transports were entered in a Microsoft Excel® spreadsheet and then analyzed using the R Statistical Software (version 3.4.1, Foundation for Statistical Computing, Vienna, Austria). Continuous variables were reported as mean, standard deviation (SD) and median (I quartile and III quartile), and discrete parameters were reported as absolute value (percentage). Differences in data distribution between infants ≤2500 grams and infants >2500 grams were explored through the chi-squared test and the t-test. A p value of <.05 was considered significant for all tests.
Ethical issues
According to the local rules, parental written consent was required before each transport and procedure performed on a newborn. The study was approved by the Regional Ethics Committee of Friuli Venezia Giulia, Italy (as per document CEUR-2022-Os-13). Data regarding patients and their relatives were extracted and then anonymized. Privacy, rights, and confidentiality of the available data were ensured throughout the study in strict accordance with Italian law. Additionally, each step of this study was carried out in agreement with the Helsinki Declaration.
Results
The NETS dealt with a total of 133 transports in the 1 January 2019–31 December 2020 period, with a neonatal transport index of 1.4% out of 9000 births in the area during the same period. Infants ≤2500 grams were more frequently transferred by the NETS than those who weighed >2500 grams (n = 34/563, 6.0% vs. n = 99/8437, 1.2%; p < .001). Among the 133 newborns transferred, the incidence of preterm birth (PTB, with GA equal to or less than 34 weeks) was 42/133 (31.6%).
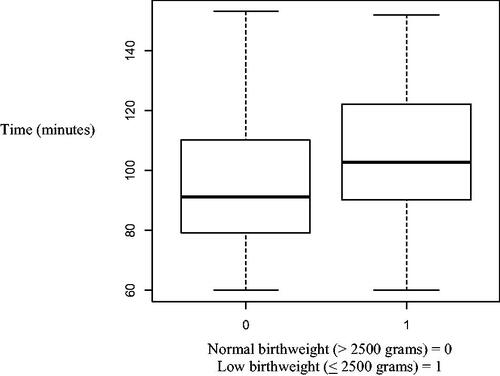
Comparisons of clinical characteristics of infants with a low birth weight with infants who weighed more than 2500 grams at birth are presented in . For the newborns with >2500 grams, there was a low incidence of cesarean birth compared to vaginal delivery (23.2% versus 63.5%; p = .001), while the percentages were reversed in the group of infants ≤2500 grams (67.7% versus 20.6%) (p = .001). The median NETS response time interval was similar between the two groups (p = .857), as well as the time of returning (p = .310). Infant stabilization time was higher in the underweight group compared to those who weighed >2500 grams (31.5 min; I–III quartile 23.0–45.0 versus 23.0 min; I–III quartile 17.0–30.0; p < .001). Total transport time was significantly different between normal- and low-birthweight groups (91.0 min; I–III quartile 79.0–110.0 versus 102.5 min; I–III quartile 90.5–121.2; p = .029, respectively) (). Regarding the interventions performed during transport, the group of infants ≤2500 grams received more intravenous therapy (47.1% vs. 26.2%) and invasive ventilation (26.5% vs. 8.1%), compared to the group of infants who weighed >2500 grams. The median NICU LOS was 18.0 days (I–III quartile 13.0–27.7) in the group of infants ≤2500 grams and 8.0 (I-III quartile 6.0-12.0) in the normal weight group (p < .001). The patients who stayed in the NICU less than 72 h were two in the low-birthweight group and nine in the normal-birthweight group (p = .343). There were two deaths in the underweight group, while no deaths occurred within those neonates who weighed >2500 grams (p < .001).
Table 2. Comparison of clinical characteristics of infants with a low birthweight (less than 2500 grams) and infants who weighed more than 2500 grams at birth.
Discussion
This study described a local reality by showing the characteristics of the neonatal transports that took place in the metropolitan area of Udine, Italy. These data may have several uses. From an epidemiological point of view, this research gives a contribution to knowledge on perinatal care by describing NETS activity, thus promoting comparisons between different healthcare systems and geographical contexts. The information obtained may well be used to perform better decision-making processes and to improve awareness of resource allocation [Citation19]. In addition, the neonatal transport index of 1.4% was found to be in line with the national trends [Citation1]. According to the literature, the neonatal transport index may be a useful tool for evaluating regionalization programs, and a range of 1–1.5% should be used [Citation20].
It has been found that male gender represented around 60% of the infants considered. The study of Al-Qaraghouli and Fang showed that the reported effects of male gender on the course of pregnancy and delivery included higher incidence of preterm labor in singletons and twins [Citation21]. Male patients predominated also in the study of Henry and Trotman on neonatal transport in Jamaica [Citation10], as well as in the study of Romanzeira and Sarinho in Brazil [Citation13]. Xu et al. showed that critically ill newborns transferred to NICUs were predominantly male infants whose average gestational age was 32.63 weeks and body weight was 1828.7 grams [Citation22]. This study demonstrated that transported newborns incidence was similar to our findings in terms of gender distribution (60.9% male), gestational age (68.4% term infants with a median of 39 weeks) and body weight (2997 grams). Other studies found that 63.6% of infants had a gestational age between 37 and 42 weeks and 60.6% of neonates had a body weight at transport >2500 grams (mean weight 2438 ± 946 grams) [Citation13]. Similar findings were seen in the study conducted by Baidya et al. [Citation7]. This study revealed that term neonates (66.2%) were more than preterm neonates, with a mean admission weight of 2300 ± 600 grams. Comparable findings were seen in our study. In fact, full-term gestational age (68.4%) and body weight at NICU admission >2500 grams (74.4%, with a mean of 2997 grams) were prevalent.
Regarding Apgar scoring, it was found that infants ≤2500 grams had a lower score (6 at 1 min, 8 at 5 min) than those >2500 grams (9 at 1 min, 9 at 5 min). The association of factors such as low Apgar score and birth defects reflected a higher acuity of illness and needed specialty services; it was to be expected that these factors would be associated with a higher likelihood of transport [Citation23]. Regarding the type of birth, the analysis showed that for infants who weighed less than 2500 grams, 20.6% was a vaginal delivery and 67.7% was urgent cesarean delivery; on the other hand, for those whose weight was more than 2500 grams, 63.5% was a vaginal delivery and 23.2% was urgent cesarean delivery. In the literature, there were no data on the association between type of birth and neonatal transportation.
Regarding infants ≤2500 grams, it was found that the main causes of transport were respiratory distress (44.2%), followed by prematurity (20.5%) and neurological disorders (11.8%). Even for infants ≥2500 grams the most frequent reasons for transfer request remained respiratory distress (49.4%). Scientific evidence confirmed that the main cause of transport request was respiratory distress syndromes (meconium aspiration, respiratory distress syndrome, pneumonia and pneumothorax) [Citation2,Citation14]. Also Henry and Trotman found that half of all neonatal transports were due to respiratory disorders [Citation10]. The growing fluid-filled fetal lungs must adjust to the extrauterine environment, which puts the newborns at risk for a variety of respiratory disorders, many of which are specific to this stage of early life [Citation24]. Regardless the causes (e.g. preterm, low first- and five-minute APGAR), early diagnosis and management of the main newborn respiratory disorders can reduce linked infant mortality and short- and long-term consequences. As a result, neonatal intensive care was required, and in certain cases, a relatively short LOS was sufficient to guarantee a patient’s recovery from illness. Previous research reported a median recovery time from respiratory distress of seven days (I–III quartile 3–13) [Citation25].
Other situations requiring transfer to specialized neonatal units were preterm births requiring special care (gestational age <32 weeks and/or birth weight <1500 g), severe hypoxia, suspected heart disease, seizures, perinatal infections (sepsis), and the surgical situation/congenital malformations [Citation2,Citation13,Citation14]. Kempley et al. in their study on neonatal transport in England [Citation12] showed that the most urgent reasons for neonatal transfer were the need for surgery, intensive neonatal surveillance and cardiac or neurological problems. Neurological disorders represented 18.8% of the transports while prematurity 6%; the last data could be explained by a timely maternal or in utero transfer.
For patient safety, reaction time (time lag between the initial emergency call and arrival of the transport team at the patient’s bedside) should be as short as possible [Citation2]. A comparison between the two groups, that is infants who weighed ≤2500 grams and those who weighed > 2500 grams, showed that the median reaction time was higher for the first group (33.5 min) than for the second (31 min). This could be explained by all practices and procedures that were needed for these critically ill infants. Regarding infant stabilization time, it was observed that the infant stabilization time for infants ≤2500 grams (median 31.5 min) was longer than for those >2500 grams (median 23 min). The study conducted by Lee demonstrated that neonates with a higher severity illness (defined as ventilated and on inotropes) had longer stabilization times compared with non-ventilated neonates (median stabilization time 125 vs 63 min) [Citation14]. In addition, McEvoy et al. found a median stabilization time of 45 min [Citation2], observing longer intervals in hospitals with a lower level of care. Abdul Wahab et al. demonstrated that the increase in stabilization times was associated with the need for interventions [Citation15], partly because of the technical complexity of the procedure partly due to the related measures taken to ensure that the procedure was successful and safe. They observed that 30% of neonatal transports did not require procedural or therapeutic interventions before mobilization for admission to the receiving unit. In the remaining 70% of the transfers, one or more interventions were required. A similar result was seen in this present study for infants >2500 grams (68.9% one or more interventions during transport). Instead for those ≤2500 grams, one or more interventions were required in 82.4% of the transports. This may be due to the criticality and instability of these infants. Abdul Wahab et al. suggested that if the staff at referring hospital can perform the required interventions/procedures before the arrival of the transport team, the time spent by the transport team at the referring hospital could be reduced significantly [Citation15].
Limitations
There are some limitations mainly due to the retrospective nature of the research. First, the maternal characteristics were not available as well as the obstetric history, which could potentially have influenced PTB incidence [Citation26]. This research only evaluated a part of the regional neonatal transport activity due to the data’s origin from one metropolitan area that is served by a dedicated NICU. As a result, this research might not have the rigor needed to support broad changes in practice. The risk of a single center conducting the study, in this case, lay in the data quantity (number of transports) and the limited external validity. Data from a nationwide network may make it possible to compare transport outcomes at the national level and remove the limitations of previous research with a single center and limited sample sizes. Third, it would have also been of interest to explore some other variables related to the transport (e.g. body temperature), in-hospital LOS, the follow-up, or the procedures provided by the referring hospital (e.g. blood gas analysis). It may be helpful to explore the risk factors for those requiring neonatal transport by comparing specific patient characteristics, such as maternal obstetric history, with newborns admitted to the same NICU at the same time who did not require neonatal transport. However, a data set for intended for managerial purposes only was accessed, hence restricted as far as the nature of information concerning the research goals.
Conclusion
A neonatal transport index of 1.4% out of 9000 births was found. The study revealed that many newborns had multiple reasons for the transfer request. It was confirmed that the main reason for newborn transfer was respiratory distress syndromes. The second main cause of transfer was prematurity in infants ≤2500 grams and neurological disorders in those >2500 grams. It was observed that infant stabilization time for infants ≤2500 grams was longer than that for infants >2500 grams. Increased stabilization time could be associated with the criticality and instability of said infants and their need for one or more interventions.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Gente M, Aufieri R, Agostino R, et al. Nationwide survey of neonatal transportation practices in Italy. Ital J Pediatr. 2019;45(1):51.
- McEvoy CG, Descloux E, Barazzoni MS, et al. Evaluation of neonatal transport in Western Switzerland: a model of perinatal regionalization. Clin Med Insights Pediatr. 2017;11:117955651770902.
- Health Italian Minister. Comitato percorso nascita nazionale. Linee di indirizzo sull’organizzazione del sistema di trasporto materno assistito (stam) e del sistema in emergenza del neonato (sten). https://www.salute.gov.it/imgs/C_17_pagineAree_4483_listaFile_itemName_4_file.pdf. 2015. Accessed October 16, 2021.
- Alberico S, Antonaglia V, Cattarossi L, et al. Procedura organizzazione del trasporto in emergenza perinatale: servizio di trasporto in emergenza neonatale (STEN) servizio di trasporto assistito materno (STAM). Regional guideline. https://www.regione.fvg.it/rafvg/export/sites/default/RAFVG/salute-sociale/sistema-sociale-sanitario/FOGLIA135/allegati/21122016_STEN-STAM-pubblicazione.pdf. 2016. Accessed June 162021.
- Chang ASM, Berry A, Jones LJ, et al. Specialist teams for neonatal transport to neonatal intensive care units for prevention of morbidity and mortality. Cochrane Database Syst Rev. 2015;2015(10):CD007485.
- Trevisanuto D, Cavallin F, Loddo C, et al. Trends in neonatal emergency transport in the last two decades. Eur J Pediatr. 2021;180(2):635–641.
- Baidya M, Shirin M, Saha L. Transport factors affecting the outcome of referred neonates admitted in a tertiary care hospital. Bangladesh J Child Health. 2018;41(3):159–164.
- Jena D, Tripathy R, Srabani P, et al. Assessment of socio-clinical profile of neonates admitted in sick neonatal care unit of tertiary care hospital: Odisha. Int J Res Med Sci. 2017;5(9):4077.
- Niermeyer S, Domek G. Neonatal transport in developing country settings: a systematic review. Pan American Health Organisation, Montevido 2016. Available online: https://iris.paho.org/handle/10665.2/31317. Accessed October 16, 2021.
- Henry S, Trotman H. Challenges in neonatal transport in Jamaica: a resource-limited setting. J Trop Pediatr. 2017;63:307–313.
- Kempley ST, Sinha AK, Census of neonatal transfers in London and the South East of England. Arch Dis Child Fetal Neonatal Ed. 2004;89(6):F521–F526.
- Mouskou S, Troizos-Papavasileiou P, Xanthos T, et al. Neonatal transportation through the course of history. J Pediatr Neonatal Care. 2015;3:00104.
- Romanzeira JCF, Sarinho SW. Quality assessment of neonatal transport performed by the mobile emergency medical services (SAMU). J Pediatr (Rio J). 2015;91(4):380–385.
- Lee K-S. Neonatal transport metrics and quality improvement in a regional transport service. Transl Pediatr. 2019;8(3):233–245.
- Abdul Wahab MG, Thomas S, Murthy P, et al. Factors affecting stabilization times in neonatal transport. Air Med J. 2019;38(5):334–337.
- von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–1499.
- Cegolon L, Mastrangelo G, Heymann WC, et al. A systematic evaluation of hospital performance of childbirth delivery modes and associated factors in the Friuli Venezia Giulia region (North-Eastern Italy), 2005–2015. Sci Rep. 2019;9(1):19442.
- Hughes MM, Black RE, Katz J. 2500-g low birth weight cutoff: history and implications for future research and policy. Matern Child Health J. 2017;21(2):283–289.
- Fairchild G, Tasseff B, Khalsa H, et al. Epidemiological data challenges: planning for a more robust future through data standards. Front Public Health. 2018;6:336.
- Bellini C, Ramenghi LA. The neonatal transport index could be used as a reference tool for the italian perinatal care regionalisation plan. Acta Paediatr. 2018;107(5):902–902.
- Al-Qaraghouli M, Fang YMV. Effect of fetal sex on maternal and obstetric outcomes. Front Pediatr. 2017;5:144.
- Xu X-J, Shi Z-G, Li L-N, et al. Importance of stabilization of the neonatal transport network in critically ill neonates. J Int Med Res. 2019;47(8):3737–3744.
- Akula VP, Gould JB, Kan P, et al. Characteristics of neonatal transports in California. J Perinatol. 2016;36(12):1122–1127.
- Brennan G, Colontuono J, Carlos C. Neonatal respiratory support on transport. Neoreviews. 2019;20(4):e202–e212.
- Enyew EF, Bitew DA, Gelagay AA. Incidence, time to recovery and predictors among neonates admitted with respiratory distress to the neonatal intensive care unit at the University of Gondar comprehensive specialized hospital, northwest Ethiopia, 2021. PLOS One. 2022;17(12):e0278887.
- Turienzo CF, Rayment-Jones H, Roe Y, et al. A realist review to explore how midwifery continuity of care may influence preterm birth in pregnant women. Birth. 2021;48(3):375–388.