Abstract
Background
The usefulness of cervical length (CL) measurement in asymptomatic pregnancies in the third trimester of pregnancy is not certain. Therefore, the objective of this study was to assess the performance of CL measurement at 31–34 gestational weeks for the prediction of spontaneous late preterm birth (PTB).
Materials and Methods
This was a prospective study of women with a singleton pregnancy, who had their routine third-trimester scan at 31–34 weeks. The CL was measured transvaginally and was tested, together with maternal demographic and obstetric parameters, for the prediction of late PTB (34 to 36 weeks), using logistic regression and ROC curve analysis.
Results
Overall, from a population of 1003 women that consented to participate in the study, 42 (4.2%) delivered at 34–36 gestational weeks. A significant association was identified between gestational age at birth and CL (rho = 0.182, p < .001), and there were significant differences in the CL between cases of late preterm and term births (p < .001). Cervical length alone could predict 17% of late PTB for a 10% false positive rate, corresponding to 22 mm. A model combining CL with parity and method of conception can identify 35% of pregnancies resulting in late PTB, at a false positive rate of 10% (AUC: 0.750; 95% CI: 0.675–0.824).
Conclusions
CL assessment at 31–34 gestational weeks may contribute to the prediction of late PTB when combined with maternal characteristics.
Introduction
The rates of preterm birth (PTB) in Europe are as high as 11%, and the majority of them are late preterm births (34–36 weeks) [Citation1]. Compared to term, late preterm neonates have higher morbidity rates including hypothermia, hypoglycemia, respiratory distress, hyperbilirubinemia, and longer duration of hospitalization [Citation2]. Moreover, late preterm neonates have higher mortality rates and increased risk of death in the first year of life, compared to term neonates [Citation3]. Regarding the causes of late PTB, several modifiable and non-modifiable risk factors have been identified to date, including multiple pregnancies, increasing maternal age, or medical and obstetric conditions that may lead to iatrogenic late PTB [Citation1].
Iams et al. first showed that cervical length (CL) may be an accurate predictor of PTB [Citation4]. Since then, different sonographic techniques have been reported for CL evaluation [Citation5,Citation6], with transvaginal measurement being the gold standard [Citation4]. A large prospective study that studied the contribution of CL to the prediction of PTB in the first trimester of pregnancy found that a combination of CL measurement and maternal characteristics may provide effective first-trimester screening for spontaneous early PTB, but is a relatively poor predictor of late PTB [Citation7].
In women identified with a short CL (<25mm) at mid-trimester, vaginal progesterone treatment is effective in reducing the risk of PTB, when administered for up to 36 weeks [Citation8]. In the same sense, if a short CL measured at 32 weeks can predict late PTB, then treatment with progesterone up to 36 weeks may theoretically be useful in reducing the rate of late prematurity. To date, there are no high-quality studies that have evaluated the contribution of CL in the third trimester of pregnancy to the PTB rate. Hence, the aim of this study was to evaluate the role of CL measurement at 31–34 gestational weeks for the prediction of spontaneous late PTB.
Materials and methods
Study design, setting and participants
A prospective study was conducted between May 2018 and January 2020 at the 3rd Academic Department of Obstetrics and Gynecology, Aristotle University of Thessaloniki, Greece. This is a tertiary care center that covers a population of more than 2 million people in Greece. All low-risk pregnancies are offered three ultrasound scans, at 11–14, 20–4 and 31–34 gestational weeks, as part of their routine antenatal care.
This study included pregnant women with a singleton pregnancy between 31 and 34 gestational weeks, who received routine antenatal care in our department. The gestational age (GA) was estimated according to the crown-rump length measurement at 11–14 weeks. The exclusion criteria were: (1) missed previous scans (11–14 or 20–24 weeks); (2) preterm prelabor rupture of membranes before the 31–34 weeks’ scan; (3) treatment with progesterone, cervical cerclage, or pessary due to short cervix in the second trimester of pregnancy (≤25mm); (4) congenital defects of the fetus, congenital uterine anomalies, history of cervical conization; (5) iatrogenic PTB for any indication or PTB before 34 weeks.
The measurement of the CL was performed according to the FMF specifications, as described by Kagan et al. [Citation9]; a 4–9 MHz transducer was used (Voluson S6, GE Healthcare, Austria). All CL measurements were acquired by a single operator (I.T.), under the supervision of fetal-maternal medicine specialist consultants (T.D. and A.A).
Variables and data sources
For every pregnant woman, a complete medical and obstetric history was acquired. Apart from the CL, maternal age, GA at the scan, parity, smoking, method of conception (spontaneous or ART), height (cm), pre-pregnancy weight (kg), BMI, GA at birth and neonatal birthweight were collected.
Statistical analysis
Continuous variables were described as mean ± standard deviation (SD) or median (range) for those not following normal distribution, while absolute (n) and relative (%) frequencies were estimated for qualitative variables. Τhe Spearman correlation coefficient was used for the regression between GA at birth and CL. The Pearson’s Chi-square test was used to identify differences between categorical variables, while the Independent-samples t-test and the Mann-Whitney U test were used to identify differences in PTB for continuous variables. Moreover, univariate logistic regression models, followed by multivariate logistic regression analyses were employed to identify risk factors for the prediction of late PTB, which was the outcome in the model. The prediction models were tested for their predicting ability of PTB using the receiver operating characteristic (ROC) curve; an area under the curve of 1 corresponds to perfect performance, whereas 0.5 is the minimum. The performance of screening was determined by the area under the curve (AUC).
All reported p values were two-tailed. Statistical significance was set at p < .05. All data analyses were performed with the statistical package SPSS v.25.0.
Ethics
All participants were informed regarding the aim of the study and no incentives were provided. The research related to human use complied with all the relevant national regulations, institutional policies, and the tenets of the Helsinki Declaration, while the study protocol was approved by the ethics committee of the Aristotle University of Thessaloniki (3.188/2-5-2018) and a written informed consent was obtained in order to take part in the survey.
Results
In total, 1229 women were approached and 1201 (97.7%) consented to participate in the study. Among these, 198 were excluded (28 due to iatrogenic PTB, 9 due to PTB before 34 weeks and 161 due to other exclusion criteria); thus, the final sample population consisted of 1003 women (median GA: 32– range: 31–34 weeks) (Supplementary Table 1, Supplementary Table 2). The median CL was 31 mm (range: 7–45 mm) ().
Figure 1. Boxplots of third trimester cervical length measurements according to late preterm birth. The top of the box represents the 75th centile, the bottom the 25th centile, and the horizontal line in the box represents the median. The T-bars represent the maximum and minimum values, excluding outliers; the latter are shown as separate circles and asterisks.
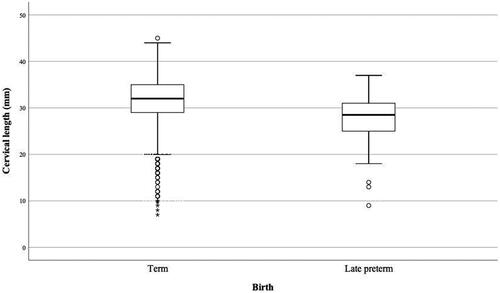
For the group of late PTB, the median CL was 28 mm (range: 9–37), 45.2% (n = 19) were nulliparous, 11.9% (n = 5) reported conception through ART, 14.3% (n = 6) were current smokers and the median BMI was 24.4 kg/m2 (range: 15.6–40.5). The median GA at birth was 35 weeks, the median neonatal birthweight was 2320 g and the median birthweight centile was 28. There were no significant differences in the mean maternal age between women with or without late PTB (Mean Difference: 0.035; 95% CI: −1.543 to 1.614; p = .965), however, the PTB group had higher median BMI than term deliveries (24.4 kg/m2 versus 22.8 kg/m2; p = .027).
A significant association was identified (rho = 0.182; p < .001) between GA at birth and CL. There was a significant difference in the median CL between the cases with late preterm and term deliveries (28 mm versus 32 mm; p < .001) ().
In the univariate analyses, women with a short CL (OR: 0.915; 95% CI: 0.877–0.955) and multiparous (OR: 2.123; 95% CI: 1.140–3.953) had a higher incidence of late PTB, whereas maternal age, BMI, method of conception and smoking were not associated with PTB. In the multivariate analysis, CL (OR: 0.912; 95% CI: 0.874–0.951), multiparity (OR: 2.624; 95% CI: 1.370–5.027) and conception through ART (OR: 2.988; 95% CI: 1.070–8.344) were identified as independent predictors for late PTB.
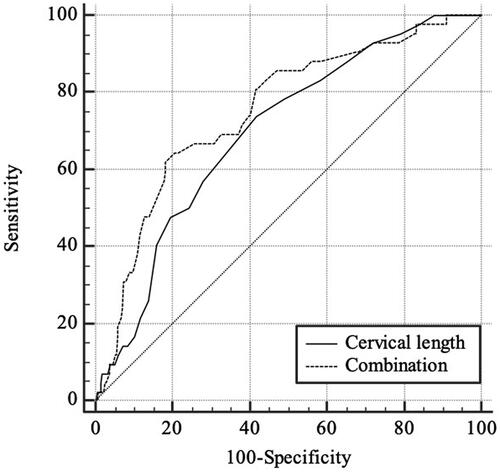
The AUC for CL alone was 0.700 (95% CI: 0.627–0.773; p < .001). When CL was combined with parity and method of conception from the multivariate model, the AUC significantly improved for the prediction of late PTB (AUC: 0.750; 95% CI: 0.675–0.824; p < .001) ( and Supplementary Table 3). Moreover, the CL cutoffs at 5% and 10% false positive rates were 19 mm and 22 mm, respectively.
Discussion
Main findings
The main findings of this study were that in singleton pregnancies at 31–34 weeks: i) the CL was shorter in women that delivered between 34–36 weeks compared to those that delivered later ii) an algorithm combining CL with maternal characteristics may identify 35% of those delivering late preterm at a 10% false positive rate.
Interpretation of the findings
The rationale for investigating the potential value of CL screening at the third trimester is that most cases of PTB occur after 34 gestational weeks [Citation1], PTB at this stage is associated with significant morbidity [Citation2], and the detection rate of screening with CL both in the first and the second trimester is significantly lower for late- than for PTB before 34 weeks [Citation7,Citation10]. Therefore, we conducted this study hypothesizing that CL could be more accurate in predicting PTB if measured closer to the event (birth).
We found that the CL cutoffs for the prediction of late PTB at 5% and 10% false positive rates were 19 mm and 22 mm, respectively, which is similar to that of Esplin et al. where the CL cutoff at 22–30 gestational weeks was 25 mm at a false positive rate of 6% [Citation11]. The CL was shorter in the late preterm compared to the term group, and there was a relationship between the CL at 31–34 weeks and the duration of pregnancy, similar to previously published data that examined the usefulness of CL between 28 and 32 gestational weeks [Citation12].
In addition, we found that as in the first- and second trimesters of pregnancy [Citation7,Citation10], the addition of maternal factors to CL improved the accuracy of the model to a 35% detection rate for a 10% false-positive rate. The maternal factors in the model included parity and conception through ART; the effect of these factors on the incidence of PTB has been previously reported. Regarding parity, there are still controversies about its effect on PTB rate. In particular, nulliparous and grand-multiparous pregnant women (>3 births) appear to be at higher risk for pregnancy complications, including PTB, compared to multiparous (≤3 births) [Citation13]. Additionally, several theories exist on the pathophysiology of spontaneous PTB in cases of ART, including procedure-related effects (e.g. medication or culture media), special characteristics of the infertile populations, and the implementation of more intensive care with associated interventions; however, the exact mechanisms remain to be determined [Citation14]. Theoretically, women at increased risk for late PTB, as identified in the third trimester, could receive modified antenatal care, including the timely administration of antenatal corticosteroids or the administration of progesterone up to 36 weeks, according to specific guidelines [Citation8,Citation15]. However, special considerations are needed for false positive cases following third-trimester screening, which could lead to maternal anxiety and unnecessary admissions or administration of corticosteroids at the late preterm period [Citation15].
About one in 20 women delivered spontaneously at 34–36 gestational weeks. This proportion is lower than in other countries, however, it may be explained by the fact that our population consisted of low-risk singleton pregnant women and all cases of iatrogenic PTB were excluded [Citation1]. To date, CL measurement in the third trimester of pregnancy would increase the examination time, as well as women’s discomfort; currently, implementation of the method would be justified only for research purposes.
Limitations
This study has certain limitations. First, the measurement of the CL was limited to specific gestational weeks during the third trimester (31–34 weeks). This period was selected as it is the time at which a universal growth scan is offered in Greece. Second, women with a short cervix identified and treated in the second trimester were excluded from the study and this may have reduced the actual performance of screening. Third, the self-reported data may be associated with recall bias, mostly regarding medical and obstetric history. Finally, our findings were based on a sample of pregnant women that received antenatal care in a single Academic Department; nevertheless, the latter covers a large population in Northern Greece and the study sample was large, so the results could probably be generalized to the entire Greek population. Of note, the predictive ability of CL alone or when combined with maternal characteristics remains lower than in the second trimester, after excluding women with CL ≤ 25mm in the second trimester.
Conclusions
Our study showed that women who deliver preterm have a shorter CL in the third trimester and that late PTB can be predicted by a combination of CL with maternal characteristics at 3134 weeks. The economic burden of PTB on the health system is so severe that should further alert health policy planners in order to encourage the development and implementation of more efficient screening methods in the pregnant population. The addition of other biomarkers, along with CL, may improve the predictive value and may encourage the investigation of interventions such as progesterone for the prevention of late PTB.
Supplemental Material
Download Zip (45.9 KB)Acknowledgments
None.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Martin JA, Hamilton BE, Osterman MJK, et al. Births: final data for 2017. Natl Vital Stat Rep. 2018;67(8):1–50.
- Leone A, Ersfeld P, Adams M, et al. Neonatal morbidity in singleton late preterm infants compared with full-term infants. Acta Paediatr. 2012;101(1):e6-10–10.
- Teune MJ, Bakhuizen S, Gyamfi Bannerman C, et al. A systematic review of severe morbidity in infants born late preterm. Am J Obstet Gynecol. 2011;205(4):374 e1-9–374.e9.
- Iams JD, Goldenberg RL, Meis PJ, et al. The length of the cervix and the risk of spontaneous premature delivery. National institute of child health and human development maternal fetal medicine unit network. N Engl J Med. 1996;334(9):567–572.
- Tsakiridis I, Mamopoulos A, Athanasiadis A, et al. Comparison of transabdominal and transvaginal ultrasonography for the assessment of cervical length in the third trimester of pregnancy. Taiwan J Obstet Gynecol. 2019;58(6):784–787.
- Tsakiridis I, Dagklis T, Mamopoulos A, et al. Cervical length at 31-34 weeks of gestation: transvaginal vs. transperineal ultrasonographic approach. J Perinat Med. 2019;47(8):817–821.
- Greco E, Gupta R, Syngelaki A, et al. First-trimester screening for spontaneous preterm delivery with maternal characteristics and cervical length. Fetal Diagn Ther. 2012;31(3):154–161.
- Society for Maternal-Fetal Medicine Publications Committee waoVB Progesterone and preterm birth prevention: translating clinical trials data into clinical practice. Am J Obstet Gynecol. 2012; 206(5):376–386.
- Kagan KO, Sonek J. How to measure cervical length. Ultrasound Obstet Gynecol. 2015; 45(3):358–362.
- Celik E, To M, Gajewska K, et al. Cervical length and obstetric history predict spontaneous preterm birth: development and validation of a model to provide individualized risk assessment. Ultrasound Obstet Gynecol. 2008; 31(5):549–554.
- Esplin MS, Elovitz MA, Iams JD, et al. Predictive accuracy of serial transvaginal cervical lengths and quantitative vaginal fetal fibronectin levels for spontaneous preterm birth among nulliparous women. JAMA. 2017;317(10):1047–1056.
- Benshalom-Tirosh N, Tirosh D, Aricha-Tamir B, et al. The clinical utility of sonographic cervical length in the management of preterm parturition at 28–32 weeks of gestation. J Matern Fetal Neonatal Med. 2015;28(16):1929–1933.
- Bai J, Wong FW, Bauman A, et al. Parity and pregnancy outcomes. Am J Obstet Gynecol. 2002;186(2):274–278.
- Dagklis T, Tsakiridis I, Mamopoulos A, et al. Modifiable risk factors for spontaneous preterm birth in nulliparous women: a prospective study. J Perinat Med. 2020;48(2):96–101.
- Tsakiridis I, Mamopoulos A, Athanasiadis A, et al. Antenatal corticosteroids and magnesium sulfate for improved preterm neonatal outcomes: a review of guidelines. Obstet Gynecol Surv. 2020;75(5):298–307.