Abstract
Background
In an effort to prevent the spread of coronavirus disease 2019 (COVID-19), governments restricted outdoor activities and imposed lockdown quarantine. This change in lifestyle probably affected individuals’ eating habits and physical activity.
Objective
To examine the effect of lockdown due to the COVID-19 pandemic on maternal antenatal weight gain, neonatal macrosomia, and other maternal and neonatal outcomes of women delivering at an academic medical center in Israel.
Method
A retrospective, two-period cohort study conducted at a university teaching medical center in Afula, Israel. The study period was between April and September 2020. This period signifies worsening in pandemic situations, during which citizens experienced strict prolonged lockdown measures. The parallel unexposed period (control period) was between April and September 2019. Singleton pregnancies delivered at >24 weeks were eligible. Primary outcome was incidence of macrosomia. Secondary outcomes included gestational weight gain, body mass index (BMI) at delivery, rates of gestational diabetes mellitus (GDM), mode of delivery, postpartum hemorrhage (PPH), and neonatal outcomes reflecting neonatal birth weight and condition at delivery.
Results
A total of 4,765 women were included, 2,442 in the study group and 2,323 in the control group. The incidence of macrosomia was significantly higher in 2020 (6.2%) than in 2019 (4.9%), (p = .048; OR: 1.29; 95% CI: 1.002– 1.65). Women gained significantly more weight (median 1 kg more), weighed more at delivery (median 1 kg), and had higher BMI at delivery in 2020 compared with those in 2019 (p < .01). The incidence of GDM was 9.5% and 8.5% in the study and control groups respectively (p = .26; OR: 1.12; 95% CI: 0.92–1.37). Greater percentage of women did not perform the glucose challenge test in 2020 (9.9%) compared with those in 2019 (7.5%) (p = .003, OR: 1.36; 95% CI: 1.11–1.67). The incidence of any hypertension related to pregnancy was significantly higher in 2020 compared to 2019 (5.8% vs 4.4% respectively, (p = .042; OR: 1.32; 95% CI: 1.02–1.71). The proportion of women who smoked during pregnancy was also significantly higher in 2020 than in 2019 (5.1% vs 3.7%, respectively, p = .02; OR: 1.40; 95% CI: 1.06–1.86). Delivery mode did not differ, while the incidence of PPH was significantly higher in 2020 than in 2019 (5.6% vs 3.4%, respectively, p = .001; OR: 1.65; 95% CI: 1.25–2.19). Neonatal condition at delivery was comparable.
Conclusion
COVID-19-related lockdown was associated with the increased rate of macrosomic infants. This indirect effect of the pandemic is probably related to poorer maternal antenatal metabolic health status. Long-term consequences should be further examined.
Introduction
Since the outbreak of coronavirus disease 2019 (COVID-19), several studies have reported the consequences of direct maternal infection with COVID-19, including higher rates of preterm birth, low birth weight, meconium, preeclampsia, and other severe maternal morbidity and mortality among symptomatic hospitalized pregnant women [Citation1–4].
In an effort to prevent the spread of the disease, governments placed restrictions on social gatherings and outdoor activities and imposed collective lockdown quarantine in 2020. This sudden and dramatic change in lifestyle has led to indirect effects related to COVID-19, including changes in individuals’ eating habits and physical activity. According to a survey conducted in Poland during the COVID-19 pandemic among Polish women, 34% of the participants gained weight and nearly 65% of them increased their total food intake [Citation5]. In Denmark, the lockdown has led to a reduction in physical activities and exercise [Citation6].
The effect of lockdown on pregnancy outcomes is controversial, and the impact on metabolic health status is less known [Citation7,Citation8]. Maternal antenatal changes in eating habits and physical activity may lead to excessive gestational weight gain and therefore increase the risk of developing gestational diabetes mellitus (GDM) [Citation9]. The short-term consequences of these metabolic changes may lead to an increased risk of fetal macrosomia and higher cesarean delivery rates [Citation9–11]. High birth weight may predispose infants to an increased risk of short- and long-term adverse outcomes [Citation12–13].
In 2020, a number of periods of lockdowns and restrictions were forced in Israel in order to limit the spread of COVID-19. In the present study, we aimed to examine the effect of these consecutive lockdown periods on gestational weight gain, the incidence of GDM, and the related outcomes, mainly the rate of macrosomia, compared with the corresponding period in the previous year at an academic medical center in Israel.
Materials and methods
This was a retrospective, two-period cohort study of women who gave birth at Emek Medical Center, a university teaching medical center in Afula, Israel. The first period (study group), was between April and September 2020. This period was selected since it signifies deterioration in the pandemic situation in Israel, during which citizens experienced two strict, consecutive, prolonged lockdowns. Health and fitness clubs were closed most of the time at the national level, and at the first-period citizens were prohibited from venturing more than 100 meters from their homes, apart from certain circumstances. The parallel unexposed period (control group) was between April and September 2019.
The study was approved in December 2020 by the local ethics committee of Emek Medical Center, Afula, Israel, in compliance with the Helsinki declaration ((#170-20-EMC). Signed informed consent was not required due to the type of research. After obtaining approval from the ethics committee, we located medical records through computerized labor charts and electronic records at admission and discharge. All of the records were manually and thoroughly reviewed to extract the required data.
Women with singleton pregnancies that gave birth after 24 weeks of gestation or later were eligible. Women with multiple gestations or termination of pregnancies were excluded. Gestational age was based on an ultrasonography scan performed during the first trimester and, if not available, according to the date of the last menstruation combined with the second-trimester ultrasonography. Macrosomia was defined as a neonatal birth weight of 4 kg or more. GDM was defined in accordance with the Carpenter–Coustan criteria [Citation14]. Postpartum hemorrhage (PPH) up to 24 h after delivery was defined as bleeding of at least 1000 ml, or a need for blood transfusion [Citation15]. Shoulder dystocia was recorded in cases of failed gentle traction and need for additional obstetric maneuvers in order to deliver the shoulders after delivery of the head [Citation16].
Primary outcome was the incidence of macrosomia during the two study periods. We hypothesized that lockdown may lead to a greater antenatal maternal weight gain and to a higher incidence of GDM, both of which are associated with higher rates of macrosomia. Secondary outcomes included gestational weight gain during pregnancy, body mass index (BMI) at delivery, smoking, incidences of GDM and gestational hypertension or preeclampsia, gestational age at delivery, mode of delivery and rate of PPH. Neonatal outcomes included neonatal birth weight, rates of neonatal birth weight ≥ 95th percentile according to birth weight standards in the live-born population in Israel [Citation17], low birth weight (<2500 g), shoulder dystocia, cord artery pH <7.1, and Apgar score < 7 at 1 and 5 min.
Statistical analysis
Differences between the years (2019 vs. 2020) were analyzed via Student’s t-test or the Mann–Whitney U test in case of non-normally distributed data for the continuous data. The chi-squared test or Fisher’s exact test was used to analyze intergroup differences in the categorical data. Odds ratios (ORs) with 95% confidence intervals (95% CIs) were computed for the categorical outcome data. Statistical significance was set at p < .05. All analyses were performed using SPSS Statistics for Windows, version 24.0. (ARMNOK, NY: IBM Corp).
Results
During the lockdown periods in 2020, there were a total of 2503 deliveries. We excluded 46 (1.8%) multiple gestations, 7 (0.3%) terminations of pregnancy, and 8 (0.3%) deliveries earlier than 24 weeks. In the parallel unexposed period in 2019, 2,402 deliveries occurred. We excluded 57 (2.4%) multiple gestations, 12 (0.5%) terminations of pregnancy, and 10 (0.4%) deliveries earlier than 24 weeks (). Overall, 4765 women were included in the final analysis, 2442 and 2323 in the study and control groups, respectively. presents the demographic and obstetric variables of each period. There were no significant differences in maternal age, pregestational weight and BMI, parity, pre-gestational diabetes, or macrosomia in previous pregnancies between the two groups.
Figure 1. Flow diagram describing all deliveries during the two periods in 2020 (Covid-19) and 2019 (unexposed), and number of deliveries included in the final analysis.
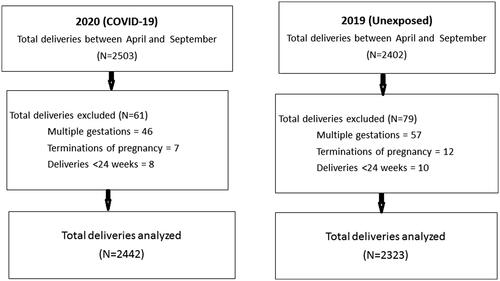
Table 1. Women demographic and obstetric variables during the COVID-19 lockdown period in 2020 compared to the control period in 2019.
shows neonatal outcomes. There was a significantly higher rate of macrosomia during the lockdown periods in 2020 (6.2%) compared with 2019 (4.9%) (p = .048; OR: 1.29; 95% CI: 1.002–1.65). Neonatal birth weight in 2020 was significantly higher than that in 2019, (p = .001). Rates of birth weight ≥ 95th percentile and low birth weight did not differ significantly between the two periods. The rates of shoulder dystocia, Apgar score < 7 at 1 and 5 min, and cord artery pH < 7.1, did not differ significantly between the groups, as well.
Table 2. Neonatal outcomes during the two study periods.
shows maternal outcomes. Pregnant women in 2020 gained significantly more weight (median 1 kg more), weighed more at delivery (median 1 kg), and had significantly higher BMI at delivery than those in 2019 (p < .01). Additionally, the proportion of women who smoked was significantly higher during the lockdown periods than in 2019 (5.1% compared with 3.7%, p = .02; OR: 1.40; 95% CI: 1.06–1.86). The incidence of GDM was 9.5% and 8.5% in the study and control groups, respectively (p = .26; OR: 1.12; 95% CI: .92–1.37). There was a significantly greater percentage of women who did not perform the glucose challenge test in 2020 than in 2019 (9.9% vs. 7.5%, respectively), (p = .003; OR: 1.36; 95% CI: 1.11–1.67). The incidence of any hypertension related to pregnancy, i.e. gestational or preeclampsia, was significantly higher in 2020 compared to 2019 (5.8% vs 4.4% respectively, p = .042; OR: 1.32; 95% CI: 1.02–1.71). Gestational age at delivery was greater in 2020 as compared to 2019 (p = .02), although the rates of preterm (gestational age <37 weeks) and late-term births (>41 weeks) were not significantly different. Mode of delivery did not differ between the groups, while the incidence of PPH was significantly higher in 2020 than in 2019 (5.6% vs 3.4% respectively, p = .001; OR: 1.65; 95% CI: 1.25–2.19) (). In the study group, 7 women were symptomatic and tested positive for COVID-19, during labor. All had mild disease. Their BMI ranged between 24.5 and 26.8 kg/m2. One woman (14.3%) had GDM.
Table 3. Maternal outcomes during the two study periods.
Discussion
The current study focused on the influence of COVID-19 lockdowns and restrictions on maternal and perinatal metabolic health outcomes. We found that the incidence of delivering a macrosomic infant increased by nearly 30%, from 4.9% to 6.2%, during the lockdown period.
Pregnant women during the COVID-19 lockdowns gained more weight, and also weighed more and had higher BMI at delivery. The proportion of women who smoked increased as well. The rate of GDM did not increase significantly; however, a greater percentage of women during the lockdowns did not perform GDM screening compared with their 2019 counterparts. The rates of gestational hypertension, or preeclampsia, and PPH increased as well during this period. The rates of preterm birth, low birth weight, and cesarean deliveries were not affected.
The impact of COVID-19-related mandatory lockdown on maternal antenatal metabolic health status and pregnancy outcomes is unclear. According to a position paper from the Academy of Nutrition and Dietetics, major components leading to a healthy pregnancy outcome include appropriate weight gain and physical activity during pregnancy [Citation18]. Concern about the spreading of COVID-19 infection led to forced lockdowns and restrictions on outdoor physical activities, which have created challenging conditions for maintaining a healthy antenatal lifestyle.
The results of our study might possibly reflect the change in lifestyle following the lockdown related to the pandemic. The association between reduced physical activity and weight gain in pregnancy might explain the higher incidence of macrosomia found in 2020. Two meta-analyses have found that the risk of macrosomia is significantly related to exercise intervention [Citation19,Citation20]. In addition, several studies have shown that gestational weight gain is an independent risk factor for macrosomia [Citation21–23]. Social isolation may induce depression, anxiety, and stress, all of which are associated with emotional eating. Emotional eating is characterized by overeating of high-sugar foods and beverages and is considered to be a learned response to coping with stress and emotions [Citation24,Citation25]. Zang et al. reported that COVID-19 may cause emotional eating, resulting in an increase in dietary intake and excess gestational weight gain [Citation26], which may explain the great maternal weight gain found in the current study. Similar findings were recently reported by others [Citation27,Citation28]. Furthermore, a positive relationship between cumulative exposure to lockdowns related to the pandemic and the risk of GDM has been reported [Citation28]. In contrast, the risk of macrosomia during the pandemic lockdown was reduced in one region in China [Citation29].
Another explanation for the increased macrosomia rate during the pandemic can be attributed to delays in medical appointments due to the fear of contracting the infection, which can result in a prolonged pregnancy [Citation30–32]. A recent study in Israel has reported that women admitted to the obstetrical emergency department were at a more advanced gestational age during the pandemic outbreak [Citation33]. Similarly, in the current study, gestational age at delivery was more advanced in the study group, which may also explain, at least in part, the higher neonatal birth weight.
The impact of these metabolic changes has been well described. Maternal excess gestational weight gain is associated with an increasing risk of postpartum weight retention, obesity in future pregnancies, type 2 diabetes, cardiovascular disease, and even premature death. Additionally, an infant of an obese mother and a macrosomic infant are at an increased risk of developing metabolic syndrome, obesity, asthma, childhood poor cognitive behavior, neurodevelopmental disorders, and even some childhood cancers [Citation12,Citation13,Citation34].
Reduced physical activity and high dietary intake are risk factors for the development of GDM [Citation9]. Nevertheless, the increase in the rate of GDM during lockdown found in the current study was not significant. This may be partly explained by an increase in missed GDM diagnoses during the lockdown periods. Indeed, a greater percentage of women did not perform the screening test during the pandemic compared with their 2019 counterparts. It has been reported that fear of contracting the COVID-19 infection often leads to the reduction or suspension of antenatal medical appointments [Citation35,Citation36]. A missed diagnosis of GDM, and as a result untreated GDM, is related to numerous maternal and perinatal adverse outcomes [Citation9]. Additionally, there is a universal argument concerning the diagnostic thresholds for GDM, and diagnostic criteria vary globally [Citation37]. Therefore, different criteria from the ones we used may lead to different results, and possibly to a significant increase in the rate of GDM.
The increased rate of gestational hypertension and preeclampsia observed during the lockdown period in the present study is not widely described in the literature. It is possible that the substantial weight gain found during the pandemic contributed, at least in part, to this increase.
Macrosomia is a risk factor for PPH; indeed, there was a higher incidence of PPH in 2020. PPH accounts for 8% of maternal deaths in developed countries and 20% in developing regions [Citation38]. The increased risk of developing PPH reinforces the necessity of changing attitude toward the indirect effects of the COVID-19 pandemic on women’s health.
The effects of lockdowns can be found across the world, including various consequences to daily life and negative metabolic changes in the non-pregnant population similar to those observed in pregnant population in the present study [Citation39]. Among non-pregnant smokers, an increase in the number of daily cigarettes was reported during the COVID-19 pandemic [Citation40]. It has been reported that, for some individuals, smoking serves to relieve stress [Citation41]. Little is known on the impact of the COVID-19 pandemic on smoking habits during pregnancy, and the available data are controversial [Citation6,Citation42]. In the current study, the proportion of smokers increased significantly during the lockdown periods though the number of cigarettes smoked per day was not examined. Smoking during pregnancy is associated with several adverse maternal and perinatal outcomes [Citation43].
The strengths of our study include its cohort study design and large sample size. Furthermore, we examined the first 6 months of the COVID-19 pandemic in Israel. This period was characterized by two repeated lockdown periods with extreme restrictions on the population. The limitations of this study include missing data on individual participants’ physical activities and dietary habits before and during the pandemic, which resulted from its retrospective nature. Additionally, compared with multicenter studies, results from a single institution may be less generalizable.
In conclusion, COVID-19 lockdowns affected maternal metabolic health status and smoking habits and also led to the non-execution of essential screening tests. Lockdown was also associated with a higher incidence of delivering macrosomic infants, possibly resulting in an increase in PPH occurrence. The long-term medical and economic burdens of these changes are worth examining as well. This burden is global; in 2020, over 100 countries worldwide implemented lockdown measures, affecting billions of citizens [Citation44]. Although lockdown is a tool for reducing the spread of pandemics, governments and medical authorities should consider their secondary effects on public health. When a lockdown is unavoidable, healthcare providers should provide professional counseling regarding the impact of lockdown on social habits and on adverse maternal and perinatal outcomes.
Acknowledgment
The authors thank Paula S. Herer, biostatistician, MSc., MPH, for statistical guidance and assistance.
Disclosure statement
No potential conflict of interest was reported by the author(s). The auteurs declare no competing of interests (financial or non-financial).
Additional information
Funding
References
- DeBolt CA, Bianco A, Limaye MA, et al. Pregnant women with severe or critical coronavirus disease 2019 have increased composite morbidity compared with nonpregnant matched controls. Am J Obstet Gynecol. 2021;224(5):510.e1-12–510.e12.
- Dashraath P, Wong JLJ, Lim MXK, et al. Coronavirus disease 2019 (COVID-19) pandemic and pregnancy. Am J Obstet Gynecol. 2020;222(6):521–531.
- Knight M, Bunch K, Vousden N, et al. Characteristics and outcomes of pregnant women admitted to hospital with confirmed SARS-CoV-2 infection in UK: national population based cohort study. BMJ. 2020;369:m2107.
- Jering KS, Claggett BL, Cunningham JW, et al. Clinical characteristics and outcomes of hospitalized women giving birth with and without COVID-19. JAMA Intern Med. 2021;181(5):714–717.
- Drywień ME, Hamulka J, Zielinska-Pukos MA, et al. The COVID-19 pandemic lockdowns and changes in body weight among polish women. A cross-sectional online survey PLifeCOVID-19 study. Sustainability. 2020;12(18):7768.
- Hegaard HK, Rom AL, Christensen KB, et al. Lifestyle habits among pregnant women in Denmark during the first COVID-19 lockdown compared with a historical period-a hospital-based cross-sectional study. IJERPH. 2021;18(13):7128.
- Kirchengast S, Hartmann B. Pregnancy outcome during the first covid 19 lockdown in Vienna, Austria. IJERPH. 2021;18(7):3782.
- Du M, Yang J, Han N, et al. Association between the COVID-19 pandemic and the risk for adverse pregnancy outcomes: a cohort study. BMJ Open. 2021;11(2):e047900.
- ACOG practice bulletin no. 190: gestational diabetes mellitus. Obstet Gynecol. 2018;131:e49-64.
- Goldstein RF, Abell SK, Ranasinha S, et al. Association of gestational weight gain with maternal and infant outcomes: a systematic review and meta-analysis. JAMA. 2017;317(21):2207–2225.
- Ehrenberg HM, Durnwald CP, Catalano P, et al. The influence of obesity and diabetes on the risk of cesarean delivery. Am J Obstet Gynecol. 2004;191(3):969–974.
- American college of obstetricians and gynecologists’ committee on practice bulletins–obstetrics. Obesity in Pregnancy: ACOG Practice Bulletin, Number 230. Obstet Gynecol. 2021;137:e128-44.
- Scifres CM. Short- and Long-Term outcomes associated with large for gestational age birth weight. Obstet Gynecol Clin North Am. 2021;48(2):325–337.
- Carpenter MW, Coustan DR. Criteria for screening tests for gestational diabetes. Am J Obstet Gynecol. 1982;144(7):768–773.
- Committee on Practice Bulletins-Obstetrics Practice bulletin no. 183: postpartum hemorrhage. Obstet Gynecol. 2017;130:e168-86.
- Hansen A, Chauhan SP. Shoulder dystocia: definitions and incidence. Semin Perinatol. 2014;38(4):184–188.
- Dollberg S, Haklai Z, Mimouni FB, et al. Birth weight standards in the live-born population in Israel. Isr Med Assoc J. 2005;7:311–314.
- Procter SB, Campbell CG. Position of the academy of nutrition and dietetics: nutrition and lifestyle for a healthy pregnancy outcome. J Acad Nutr Diet. 2014;114(7):1099–1103.
- Wiebe HW, Boulé NG, Chari R, et al. The effect of supervised prenatal exercise on fetal growth. Obstet Gynecol. 2015;125(5):1185–1194.
- Davenport MH, Meah VL, Ruchat SM, et al. Impact of prenatal exercise on neonatal and childhood outcomes: a systematic review and meta-analysis. Br J Sports Med. 2018;52(21):1386–1396.
- Black MH, Sacks DA, Xiang AH, et al. The relative contribution of prepregnancy overweight and obesity, gestational weight gain, and IADPSG-defined gestational diabetes mellitus to fetal overgrowth. Diabetes Care. 2013;36(1):56–62.
- Alberico S, Montico M, Barresi V, et al. The role of gestational diabetes, pre-pregnancy body mass index and gestational weight gain on the risk of newborn macrosomia: results from a prospective multicentre study. BMC Pregnancy Childbirth. 2014;14:23.
- Bowers K, Laughon SK, Kiely M, et al. Gestational diabetes, pre-pregnancy obesity and pregnancy weight gain in relation to excess fetal growth: variations by race/ethnicity. Diabetologia. 2013;56(6):1263–1271.
- Macht M. How emotions affect eating: a five-way model. Appetite. 2008;50(1):1–11.
- Kuijer RG, Boyce JA. Emotional eating and its effect on eating behaviour after a natural disaster. Appetite. 2012;58(3):936–939.
- Zhang J, Zhang Y, Huo S, et al. Emotional eating in pregnant women during the covid-19 pandemic and its association with dietary intake and gestational weight gain. Nutrients. 2020;12(8):2250.
- La Verde M, Torella M, Riemma G, et al. Incidence of gestational diabetes mellitus before and after the covid-19 lockdown: a retrospective cohort study. J Obstet Gynaecol Res. 2022;48(5):1126–1131.
- He Z, Lv Y, Zheng S, et al. Association of COVID-19 lockdown with gestational diabetes mellitus. Front Endocrinol. 2022;13:824245.
- Wen J. Impact of COVID-19 pandemic on birth outcomes: a retrospective cohort study in nanjing, China. Front Public Health. 2022;10:923324.
- Coxon K, Turienzo CF, Kweekel L, et al. The impact of the coronavirus (COVID-19) pandemic on maternity care in Europe. Midwifery. 2020;88:102779.
- Goyal M, Singh P, Singh K, et al. The effect of the COVID-19 pandemic on maternal health due to delay in seeking health care: experience from a tertiary center. Int J Gynaecol Obstet. 2021;152(2):231–235.
- Justman N, Shahak G, Gutzeit O, et al. Lockdown with a price: the impact of the COVID -19 pandemic on prenatal care and perinatal outcomes in a tertiary care center. IMAJ. 2020;22:533–537.
- Kugelman N, Lavie O, Assaf W, et al. Changes in the obstetrical emergency department profile during the COVID-19 pandemic. J Matern Neonatal Med. 2022;35(21):4116–4122.
- McAuliffe FM, Killeen SL, Jacob CM, et al. Management of prepregnancy, pregnancy, and postpartum obesity from the FIGO pregnancy and non-communicable diseases committee: a FIGO (international federation of gynecology and obstetrics) guideline. Int J Gynecol Obstet. 2020;151(S1):16–36.
- De Curtis M, Villani L, Polo A. No title. Arch Dis Child Fetal Neonatal Ed. 2021;106(4):456.
- Khalil A, von Dadelszen P, Draycott T, et al. Change in the incidence of stillbirth and preterm delivery during the COVID-19 pandemic. JAMA. 2020;324(7):705–706.
- Crowther CA, Samuel D, McCowan L, et al. Lower versus higher glycemic criteria for diagnosis of gestational diabetes. N Engl J Med. 2022;387(7):587–598.
- Say L, Chou D, Gemmill A, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014;2(6):e323-33–e333.
- Rubio-Tomás T, Skouroliakou M, Ntountaniotis D. Lockdown due to COVID-19 and its consequences on diet, physical activity, lifestyle, and other aspects of daily life worldwide: a narrative review. IJERPH. 2022;19(11):6832.
- Guignard R, Andler R, Quatremère G, et al. Changes in smoking and alcohol consumption during COVID-19-related lockdown: a cross-sectional study in France. Eur J Public Health. 2021;31(5):1076–1083.
- Fidler JA, West R. Self-perceived smoking motives and their correlates in a general population sample. Nicotine Tob Res. 2009;11(10):1182–1188.
- Tsakiridis I, Dagklis T, Mamopoulos A, et al. Antenatal depression and anxiety during the COVID-19 pandemic: a cross-sectional study in pregnant women from routine health care contact in Greece. J Perinat Med. 2021;49(6):656–663.
- Pineles BL, Hsu S, Park E, et al. Systematic review and meta-analyses of perinatal death and maternal exposure to tobacco smoke during pregnancy. Am J Epidemiol. 2016;184(2):87–97.
- Dunford D, Dale B, Stylianou N, et al. The Coronavirus: world in lockdown in maps and charts2020. https://www.bbc.com/news/world-52103747.
