Abstract
Background
Transcervical resection of adhesion (TCRA) and postoperative adjuvant estrogen and progestin are the main treatments for cavity adhesions, but the recurrence rate after surgery is still high. It was showed that aspirin could promote endometrial proliferation and repair after TCRA in patients with severe cavity adhesions, but the effect on reproduction was uncertain.
Objective
To assess the effect of aspirin on uterine arterial blood flow and endometrium in moderate and severe intrauterine adhesion after transcervical resection of adhesion.
Methods
The databases used included Cumulative Index to PubMed, EMBASE, Chinese National Knowledge Infrastructure (CNKI), and Wanfang database. Studies published before June 2022 were included. Each participant received an aspirin-based intervention aimed at improving uterine status, which was compared to a sham intervention. The primary outcome measure was a change in endometrium thickness. Secondary outcomes included uterine artery resistance index, blood flow index, and endometrial arterial resistance index.
Result
A total of 19 studies (n = 1361 participants) that met the inclusion criteria were included in this study. The aspirin-based intervention was strongly associated with better clinical outcome at second-look endometrium thickness (MD 0.81, CI 0.46–1.16; p < .00001) and blood flow Index (FI) (MD 4.1, CI 2.3–5.9; p < .00001). Besides, the analysis of arterial pulsatility index (PI) showed a significantly reduced after transcervical resection of adhesion (MD −0.9, CI −1.2 to 0.6; p < .00001); whereas no significant difference was found in endometrial arterial resistance index (RI) (95% CI, −0.30 to 0.01; p = .07).
Conclusion
Our study proved the effect of aspirin on uterine arterial blood flow and endometrium in moderate and severe intrauterine adhesion after transcervical resection of adhesion. However, the review requires evidence from additional randomized controlled trials and high-quality research. More strictly designed research studies are needed to assess the effectiveness of aspirin administration after transcervical resection of adhesion.
1. Introduction
As a result of damage to the basal layer of the endometrium caused by various factors, such as uterine surgery, cesarean section, endometrial tuberculosis, and uterine artery embolization, intrauterine adhesions (IUA) result in severe changes in the normal anatomy of the uterine cavity. Infertility, recurrent miscarriages, and decreased menstrual flow are some of the most common clinical symptoms of IUA. Currently, the main treatment method for IUA is hysteroscopic transcervical resection of adhesions. As well as direct visualization of the uterine cavity and scoring of uterine adhesions, hysteroscopic excision of scar tissue is also an effective treatment for IUA. This treatment method, however, is still associated with a high recurrence rate [Citation1]. According to a previous study, hysteroscopic adhesiolysis resulted in re-adhesion rates as high as 62.5%. Therefore, it is particularly important to prevent IUA following intrauterine operations.
Aspirin is anti-inflammatory and anti-rheumatic, inhibits platelet adhesion and aggregation, and prevents thrombosis. It was the first antiplatelet drug used in antithrombotic therapy that inhibits platelet aggregation effectively. Patients with adverse pregnancy and childbirth with a clear diagnosis of embolism-prone signs are the main candidates for this treatment, as well as those with abnormal uterine artery perfusion and abnormal placental perfusion. Inhibition of cyclooxygenase activity by aspirin can enhance uterine blood flow and promote tissue healing. In a recent study, aspirin was demonstrated to have a positive effect on the growth and repair of the endometrium following IUAs, suggesting that this may be related to the promotion of endometrial microvascular formation and an improvement in local blood circulation [Citation2]. Aspirin might thereby decrease the incidence of IUA recurrence, improve menstrual flow and increase pregnancy rates. The combination of Estradiol valerate and aspirin was shown to decrease the expression levels of TGF-β1 and PAI-1 in the endometrium tissue, whereas it increased the expression levels of NMP-9, which improved the IUA in rats [Citation3]. Additionally, it has been demonstrated that low-dose aspirin alters the expression of endometrial LIF and integrin β3 and that these changes may increase endometrial receptivity.
Currently, most articles describe the role of estrogen or progesterone-releasing IUD in TCRA instead of aspirin. And a limited number of studies have examined whether aspirin can improve local blood circulation to facilitate endometrial repair following severe IUA surgery. To test the effects of low-dose aspirin on uterine artery blood flow and endometrium after TCRA, this study used Meta-analysis to systematically evaluate the effects of low-dose aspirin on uterine artery blood flow and endometrium. The purpose of this article is to provide a scientific basis for the adjunctive use of aspirin therapy following clinical TCRA.
2. Materials and methods
2.1. Search strategy
This systematic review and meta-analysis was conducted according to the PRISMA guidelines. We perform a literature search using PubMed, EMBASE, Chinese National Knowledge Infrastructure (CNKI), and the Wanfang database. The following keywords were used: intrauterine synechiae, intrauterine adhesion, uterine synechiae, Transcervical resection of adhesion, TRCA, Aspirin, acetylsalicylic acid, uterine arterial blood flow, and endometrium. The search was limited to trials in humans, published in English or Chinese up to June 1, 2022.
2.2. Eligibility criteria and study selection
The inclusion criteria were the following: (1) type of studies: randomized controlled trials (RCTs) were included; (2) type of participants: participants should be clinically diagnosed with moderate and severe intrauterine adhesion and should be treated after transcervical resection of adhesion; (3) type of interventions: the treatment group could be treated by combined therapy with or without aspirin every day after transcervical resection of adhesion; (4) outcome measurements: Endometrial artery resistance index (RI), pulsatility index (PI), endometrial vascularization index (VI), flow index (FI) and vascularized flow index (VFI). If a study contained three or more groups, with just one group receiving aspirin and a control group not receiving aspirin and any medicine who were treated in the same way as the aspirin, the data from the treatment group and the control group were chosen for this study.
2.3. Data abstraction
Two reviewers independently extracted data from all eligible studies using a data extraction form containing characteristics and outcomes. Patients in the observation group were given aspirin treatment, while those in the control group were not given aspirin treatment. There was a comparison between the two groups in terms of clinical outcomes and reproductive outcomes. The statistics extracted from the eligible studies were analyzed using RevMan software, version 5.3 (Cochrane Collaboration, Copenhagen, the Netherlands).
In an unblinded standardized method, two investigators (LLN and LXD) reviewed the title and abstract information to select potential references. The full articles of all potentially relevant studies were retrieved. Both investigators independently reviewed the selected papers and made a final judgment on their selection. Any disagreements with a third author were resolved through discussion or consultation (DJ).
2.4. Quality assessment
According to the Newcastle-Ottawa Scale, two reviewers independently assessed the quality of the included studies, with a maximum possible score of nine points. Three items were assessed in this meta-analysis: selection of cases and controls, comparability of cases and controls, and outcome assessment. Evidence quality was rated using the GRADE approach, which grades recommendations based on assessment, development, and evaluation.
2.5. Data analysis
Cochrane RevMan software (version 5.3) was used to conduct statistical heterogeneity tests and combined data analyses. Count data were presented as odds ratios (OR) and measurement data as mean differences (MD). Studies with p ≥ .1 and I2 ≤ 50% were considered homogeneous and were analyzed using a fixed effect model. When p < .1 or I2 > 50%, the studies were considered heterogeneous, a random-effect model was adopted, and the research results were carefully interpreted. The 95% confidence interval (CI) was calculated and the difference was considered statistically significant when p < .05.
3. Results
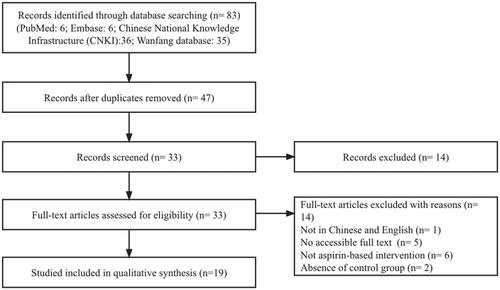
In the initial search, 83 articles were retrieved. 24 articles were excluded from consideration after titles and abstracts were screened. Additionally, 40 studies were excluded for the following reasons: the full text was not accessible, the full paper was not written in either English or Chinese, or the study was not controlled. There were two RCTs that met all other criteria, but both had to be excluded. One was because the control group was placed with an IUD after hysteroscopic surgery, and the other was an experimental design in which different doses of aspirin were used in different groups. Therefore neither of these articles could be included. Finally, 19 studies were included in our review. The flow diagram of the study selection was shown in .
3.1. Baseline of characters
In total, 1361 patients of were included in the study. According to the included articles, the average age of the patients included in the study was 31.10 ± 9.91 (mean = 31.10, SD = 9.91). The average onset time of the patients included in the study is 6.59 ± 1.24 months (mean = 6.59, SD = 1.24) (see ). Besides, the mean BMI of all subjects mentioned in the study was 22.01 ± 3.2 kg/m2, and the dose and duration of treatment with aspirin was 100 mg/d for 14 d. Moreover, the mean dosage of estrogen and progestins in the two groups was 10 mg/d. The severity of adhesions included in the studies was mainly moderate to severe. The American Fertility Society was one of the most usual several classification systems to be used. All studies included in this review used complementary cyclical hormone therapy such as Estradiol Valerate. However, the duration and dose of hormone therapy, as well as the mean follow-up period, were not uniform. For the quality assessment of included articles. The results of the Newcastle-Ottawa Quality Assessment are given in . All studies scored between five and seven, out of a total of eight.
Table 1. Characteristics of Included Studies.
Table 2. Appraisal of methodological quality (Newcastle-Ottawa Scale) of included studies.
3.2 Meta-analysis outcome
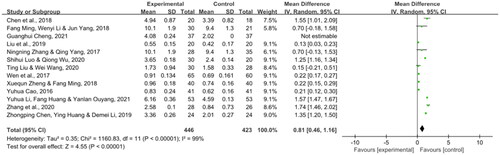
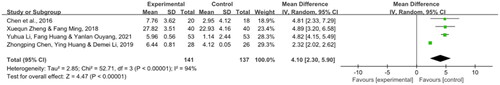
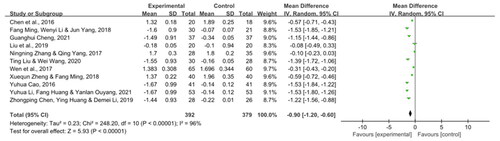
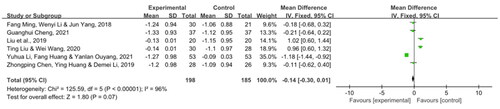
On the evaluation of the effectiveness of aspirin, three of the four outcome demonstrated a significant reduction. Thirteen articles reported the using of aspirin increased endometrium thickness (MD 0.81, CI 0.46–1.16; p < .00001) and FI (MD 4.1, CI 2.3–5.9; p < .00001) when compared with the beginning, which were shown in and . Besides, the analysis of PI showed significantly reduced after transcervical resection of adhesion (MD −0.9, CI −1.2 to −0.6; p < .00001), which was shown in . However, the mean effect size for the RI subgroup was −0.14 (95% CI, −0.30 to 0.01; p = .07, with high heterogeneity (I2 = 96%), which was shown in . Although the data show the effectiveness of aspirin, we are not certain that the effectiveness of aspirin leads to the possibility of another pregnancy for patients due to missing data or lack of data validity for re-pregnancy in the included articles.
4. Discussion
This study evaluated the effects of aspirin after hysteroscopic separation of uterine adhesions by searching databases using published clinical controlled trials, demonstrating that aspirin significantly improved Endometrium thickness, pulsatility index, and blood flow index. However, aspirin had no effect on the postoperative uterine artery resistance index. There were only three studies included in this study that used the 1988 American Fertility Society method for diagnosing uterine adhesions and had low homogeneity. In other words, oral aspirin is beneficial for endometrial regeneration and repair, which reduce the postoperative recurrence of IUA, improve menstruation, and finally improve the reproductive prognosis.
The terminal arterial branch of the uterine artery is the spiral uterine artery, which nourishes primarily the endometrium. The use of Color Doppler ultrasound can be used to monitor the blood flow in the uterine artery and endometrium, as well as to measure the PI and RI of the uterine artery and VI, FI, and VFI of the endometrium to reflect the perfusion of the uterine artery and endometrium [Citation22–24]. It is important to note that as the PI and RI of uterine arteries decrease, vascular resistance decreases, and local perfusion of uterine blood increases. As endometrial VI, FI, and VFI increase, endometrial perfusion increases and the endometrial repair process has a good blood supply, thereby promoting growth and repair. A poor endometrial blood supply, on the other hand, will adversely affect endometrial repair, resulting in a poor postoperative outcome. It is important to mention that aspirin contains active ingredients such as acetylsalicylic acid. Aspirin can reduce platelet activity, reduce micro thrombosis, improve local blood circulation, and also increase blood flow to the uterus and ovaries. By improving uterine morphology, one can increase endometrial receptivity and facilitate embryonic implantation, leading to an increase in fertility. Accordingly, aspirin may improve the long-term reproductive prognosis in IUA due to its ability to improve endometrial thickness and prevent IUA.
Among the articles we included was one in which different doses of aspirin were used in different groups, thereby comparing their differences in effectiveness [Citation2]. Despite the fact that the results of the study showed that the disease improved significantly after the use of aspirin compared with the control group. However, no difference in efficacy was observed when different dosages were compared. In experimental studies, aspirin has been shown to inhibit the synthesis of prostacyclin (PGI2) and thromboxane (TXA2) by inhibiting the first synthesis enzyme of prostaglandin synthesis, cyclooxygenase [Citation25–27]. Aspirin at low doses (75–100 mg/d) suppresses the synthesis of thrombin A2, thus inhibiting platelet aggregation, preventing microthrombus formation, and improving circulation [Citation28]. Aspirin may also inhibit endometrial fibrosis by suppressing the TGFβ1-Smad2/Smad3 pathway [Citation21]. Aspirin is more sensitive to platelet cyclooxygenase than to vascular endothelial cyclooxygenase, and a small dose of aspirin can effectively inhibit platelet TXA2 synthesis. By inhibiting inflammation, it improves the local blood circulation in the uterus and ovaries. Furthermore, the majority of literature that was included in this article used estrogens simultaneously with aspirin in a number of studies. As a result of estrogen promoting the growth of the endometrium and progesterone promoting the transformation of the endometrium into the secretory phase, a regular menstrual cycle is produced [Citation29,Citation30]. The simultaneous administration of estrogen and aspirin can therefore improve the uterine cavity morphology and improve the menstrual recovery of the patient [Citation3].
It is important to consider the potential limitations of this meta-analysis. There were differences in postoperative adjuvant therapies (artificial cycle, intrauterine balloons, and intrauterine devices, among others) between the experiment and control groups. As a result of the limitations in the existing literature, we were unable to examine the curative effects of different instruments for the treatment of IUA because of the limitations in the existing literature. Besides, the type of surgery (and pre-surgery) wasn’t considered and it represents a big bias. There is also the possibility that other details (operators’ techniques) contributed to the bias as well. Thirdly, the dose of aspirin used was different in different studies, which could also create a problem of bias. Fourth, judging by the lack of strong evidence, we need to conduct more high-quality RCTs in the future, considering the lack of stronger evidence.
5. Conclusion
Based on available evidence, this meta-analysis showed that aspirin was effective on uterine arterial blood flow and endometrium. Further high-quality trials are required to assess the efficacy and safety of aspirin.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Bosteels J, Weyers S, Kasius J, et al. Anti‐adhesion therapy following operative hysteroscopy for treatment of female subfertility. Cochrane Database Syst Rev. 2015;11(11):CD011110.
- Chen Y, Liu L, Luo Y, et al. Effects of aspirin and intrauterine balloon on endometrial repair and reproductive prognosis in patients with severe intrauterine adhesion: a prospective cohort study. Biomed Res Int. 2017;2017:1–8.
- Liu J. Improvement effect of estradiol valerate combined with aspirin on intrauterine adhesion in rats. J Jilin Univ. 2019;45:830–835.
- Cheng G-H. Study on the application of aspirin combined with detroterone after separation of severe uterine adhesions in the reproductive age. Pract Integr Chinese Western Med Clin. 2021;22:81–82.
- Li Y, Huang F, Ouyang Y. Aspirin adjuvant therapy after severe uterine adhesions. Chinese J Mod Med. 2021;10:61–63.
- Xue P, Ruoyu L. Effects of estrogen combined with climen and aspirin to prevent recurrence of intrauterine adhesions after hysteroscopy. China J Fam Plan Obstet Gynecol. 2020;11:82–84.
- Liu T, Wang W. Effect of low-dose aspirin application on endometrium after hysteroscopic electrosurgery. Chinese J Mod Med. 2020;5:65–67.
- Shihui L, Qiong W. Clinical effect analysis of aspirin on patients with moderate or severe intrauterine adhesion after surgery. J Jinzhou Med Univ. 2020;1:64–67.
- Liu J, Zheng Y, Wang Y, et al. Efects of aspirin combined with electrical stimulation of pelvic floor smooth muscle on MVD and VEGF expresion in endometrium of patients after hysteroscopic adhesiolysis and its clinical significance. Journal of Jilin Univ. 2019;6:1408–1414.
- Shi Y, Peng DH, Gao YX, et al. Evaluation of the effectiveness of tonic jalapeno combined with fentanyl and aspirin in preventing recurrence of moderate-severe uterine adhesions after HEOS cold knife surgery. J Southeast Univ. 2019;5:873–876.
- Zhong-Ping C, Ying H, De-Mei LI. The effect of small dose aspirin on endometrial and blood flow changes in patients with uterine adhesion electric resection. Drugs Clinic. 2019;12:37–39.
- Xiang Y, Ding Y. Effect analysis of three drug treatment regimens after the transcervical resection of adhesion of moderate and severe intrauterine adhesion. Xinjiang Med. 2018;10:1106–1110.
- Zheng X, Ming F. Effect of low-dose aspirin on uterine artery blood flow and endometrium after uterine adhesions surgery. Contemp Med. 2018;18:146–148.
- Ming F, Li WY, Yang J. Efficacy of low-dose aspirin for patients undergoing hysteroscopic transcervical resection of adhesion. Guangxi Med J. 2018;11:1221–1223.
- Zhang N-N, Yang Q. Effect of aspirin combined with femoston on endometrial repair after operation in severe intrauterine adhesion. Pract Pharma Clin Remedies. 2017;10:1159–1162.
- Wen Y, Chi Y-G, Liu L-B, et al. Effect of low-dose aspirin on endometrial receptivity and pregnancy outcome of severe intrauterine adhesion after surgery. J Chongqing Med Univ. 2017;04:449–452.
- Chen Q, Liang C, Li X, et al. Effect of transcervical resection of adhesion combined with low-dose aspirin on uterine artery blood flow and Smad2/3in endometrial tissue. J Hainan Med Univ. 2016;22:2657–2660.
- Cao Y. Effect of low-dose aspirin on the endometrium after uterine adhesions surgery. J Math Med. 2016;7:1034–1035.
- Chi Y, Lei L, Liu L-B, et al. The effect of low-dose aspirin on endometrium after transcervical resection for severe intrauterine adhesions. Chongqing Med. 2015;28:3944–3946.
- Chi Y, He P, Lei L, et al. Transdermal estrogen gel and oral aspirin combination therapy improves fertility prognosis via the promotion of endometrial receptivity in moderate to severe intrauterine adhesion. Mol Med Rep. 2018;17(5):6337–6344.
- Zhang Z, Li S, Deng J, et al. Aspirin inhibits endometrial fibrosis by suppressing the TGF-β1-Smad2/Smad3 pathway in intrauterine adhesions. Int J Mol Med. 2020;45(5):1351–1360.
- Monk C, Newport DJ, Korotkin JH, et al. Uterine blood flow in a psychiatric population: impact of maternal depression, anxiety, and psychotropic medication. Biol Psychiatry. 2012;72(6):483–490.
- Zhang K, Wang E, Li Y, et al. Role of low-molecular-weight heparin in altering uterine artery blood flow in recurrent spontaneous abortion: a prospective study. J Int Med Res. 2020;48(8):300060520945558.
- Miccò M, Sala E, Lakhman Y, et al. Imaging features of uncommon gynecologic cancers. AJR Am J Roentgenol. 2015;205(6):1346–1359.
- Burch JW, Stanford N, Majerus PW. Inhibition of platelet prostaglandin synthetase by oral aspirin. J Clin Invest. 1978;61(2):314–319.
- Jaffe EA, Weksler BB. Recovery of endothelial cell prostacyclin production after inhibition by low doses of aspirin. J Clin Invest. 1979;63(3):532–535.
- Macchi L, Sorel N, Christiaens L. Aspirin resistance: definitions, mechanisms, prevalence, and clinical significance. Curr Pharm Des. 2006;12(2):251–258.
- Di Francesco L, Lopez Contreras LA, Sacco A, et al. New insights into the mechanism of action of aspirin in the prevention of colorectal neoplasia. Curr Pharm Des. 2015;21(35):5116–5126.
- Roy KK, Negi N, Subbaiah M, et al. Effectiveness of estrogen in the prevention of intrauterine adhesions after hysteroscopic septal resection: a prospective, randomized study. J Obstet Gynaecol Res. 2014;40(4):1085–1088.
- Chen L, Zhang H, Wang Q, et al. Reproductive outcomes in patients with intrauterine adhesions following hysteroscopic adhesiolysis: experience from the largest women’s hospital in China. J Minim Invasive Gynecol. 2017;24(2):299–304.