Dear Editor,
We have read with great interest a case report on a resolution of acute cervical insufficiency after antibiotic treatment in a case presented by Yeo et al. [Citation1]. The described case is similar to our patient and analyzing them both together raises several questions, discussed below.
36-year-old primigravida was referred to the Department of Obstetrics, Perinatology and Neonatology Center of Postgraduate Medical Education due to high risk of preterm delivery and intraamniotic infection at 31 + 1 weeks of gestation. The prior course of pregnancy was uneventful with normal cervical length measurement of 32 mm at 21 weeks of gestation. Gestational age was verified during the first trimester ultrasound examination. 2 years earlier the patient had hysteroscopic uterine polypus removal performed.
On admission the patient denied cramping, bleeding, or leaking of fluid. The fetal weight was estimated to be 1304 g (10.8 percentile) with normal uterine and umbilical arteries doppler. On transvaginal ultrasound the cervical canal length was 6 mm with funneling (). Digital exam revealed fetal membranes visible at the external os on the diameter of 2 cm (). In the laboratory tests normal C-reactive protein level (2.19 mg/L) and white blood count (12.4x109/mL) were found. The urine culture was negative and in the vagino-cervical swab only Lactobacillus spp. were identified. The patient was informed about the high risk of imminent preterm delivery and the risk of intraamniotic infection and inflammation. She was administered betamethasone (two doses of 12 mg intramuscularly, 24 h apart) and vaginal progesterone (200 mg). The patient was offered an amniocentesis to verify if the intraamniotic infection and inflammation were present, however she did not consent to the procedure. She was informed about an antibiotic treatment which was successful in cervical insufficiency in a study by Oh et al. and agreed to this treatment [Citation2]. A regimen of 3 antibiotics was administered: ceftriaxone 1 gram IV every 24 h, clarithromycin 500 mg oral every 12 h and metronidazole 500 mg IV every 8 h. This treatment was continued for 7 days with no side effects. No bed rest was recommended.
Figure 1. (a) Sonographic cervical evaluation at 31 0/7 gestational weeks. The cervical length is 6.1 mm with funneling; (b) Fetal membranes visible at the external os; (c) Sonographic cervical evaluation at 32 0/7 gestational weeks. The cervical length is 21.9 mm.
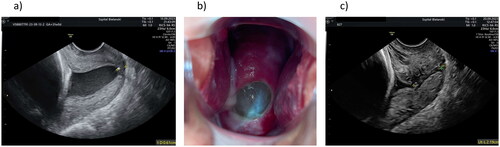
During the following 7 days she did not report any adverse symptoms. The CTG was normal. The ultrasound performed after 7 days of antibiotics treatment revealed a closed cervical canal measuring 21 mm (). The patient was discharged home with recommendation to continue vaginal progesterone. She was counseled afterwards at the Outpatient Clinic and the cervix remained closed with cervical canal measurement of 20 mm at 33 + 0 and 34 + 0 weeks, 12 mm at 35 + 0 weeks and 10 mm at 36 + 0 weeks. Finally, she delivered vaginally at 38 weeks a heathy girl weighting 2240 g in a good general condition.
In both cases – the one described by Yeo et al. and ours, a resolution of advanced cervical insufficiency after antibiotic and progesterone treatment was observed. In our case no direct proof of intraamniotic infection or inflammation was available as the patient did not consent to amniocentesis. The urine and vagino-cervical swabs were normal. In the case presented by Yeo et al. no pathogens were identified in amniotic fluid. The glucose level in amniotic fluid was normal, while interleukin-6 concentration elevated [Citation1]. This may indicate intraamniotic inflammation. The patient received antibiotic treatment for 11 days. In our case the therapy was continued for 7 days with no bed rest and spontaneous closure of cervical canal was observed. Therefore, we assumed that in our patient intraamniotic inflammation could have been present as well.
The effectiveness of antibiotic treatment in intraamniotic infection/inflammation was observed by other researchers [Citation2–5]. Cervical insufficiency, preterm rupture of membranes and preterm delivery may be symptoms of intraamniotic infection or inflammation. Is it possible to eradicate pathogens and eliminate inflammation inside amniotic cavity? Is ceftriaxone with clarithromycin and metronidazole the best treatment option? For how long should the therapy be continued? In our case treatment lasting 7 days was efficient, while other authors recommended a longer therapy. Further randomized trials on large study groups on the efficacy of antibiotics are urgently needed.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data on the presented case are available from the corresponding author. The patient gave written consent to this publication.
Additional information
Funding
References
- Yeo L, Romero R, Chaiworapongsa T, et al. Resolution of acute cervical insufficiency after antibiotics in a case with amniotic fluid sludge. J Matern Fetal Neonatal Med. 2022;35(25):5416–5426. doi: 10.1080/14767058.2021.1881477.
- Oh KJ, Romero R, Park JY, et al. Evidence that antibiotic administration is effective in the treatment of a subset of patients with intra-amniotic infection/inflammation presenting with cervical insufficiency. Am J Obstet Gynecol. 2019;221(2):140.e1–140.e18. doi: 10.1016/j.ajog.2019.03.017.
- Hatanaka AR, Franca MS, Hamamoto TENK, et al. Antibiotic treatment for patients with amniotic fluid "sludge" to prevent spontaneous preterm birth: a historically controlled observational study. Acta Obstet Gynecol Scand. 2019;98(9):1157–1163. doi: 10.1111/aogs.13603.
- Yoon BH, Romero R, Park JY, et al. Antibiotic administration can eradicate intra-amniotic infection or intra-amniotic inflammation in a subset of patients with preterm labor and intact membranes. Am J Obstet Gynecol. 2019;221(2):142.e1-142–e22. doi: 10.1016/j.ajog.2019.03.018.
- Lee J, Romero R, Kim SM, et al. A new antibiotic regimen treats and prevents intra-amniotic inflammation/infection in patients with preterm PROM. J Matern Fetal Neonatal Med. 2016;29(17):2727–2737. doi: 10.3109/14767058.2015.1103729.
