?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Objective
In the present study, we sought to identify risk factors for umbilical cord prolapse (UCP) and adapt the multidisciplinary team (MDT) first-aid simulation training for UCP patients. We evaluated the usefulness of the MDT first-aid simulation by comparing delivery outcomes for UCP patients before and after its implementation.
Material and methods
A retrospective review was conducted on 149 UCP cases (48 overt and 101 occult) and 298 control deliveries that occurred at the Third Affiliated Hospital of Sun Yat-sen University from January 1998 to December 2022. Patient data were compared between the groups. One-way analysis of variance (ANOVA) was used for means comparison, and the chi-square test was used for categorical data. Univariate and multivariate logistic regression analyses were performed to identify factors significantly associated with UCP.
Results
Overt UCP was strongly associated with all adverse delivery outcomes. Both univariate and multivariate analyses identified multiparity, breech presentation, polyhydramnios, and low birth weight as independent risk factors for overt UCP (all odds ratios [OR] > 1; all p < 0.05). Preterm labor and abnormal placental cord insertion were identified as independent risk factors for occult UCP (all OR > 1; all p < 0.05). After 2014, when obstetrical staff received MDT first-aid simulation training, patients with overt UCP experienced shorter decision-to-delivery intervals due to more timely cesarean sections. They also had higher Apgar scores at 1, 5, and 10 min, and lower admission rates to the neonatal intensive care unit compared to patients before 2014 (all p < 0.05).
Conclusion
MDT first-aid simulation training for overt UCP can improve neonatal outcomes. However, medical simulation training efforts should initially focus on the early identification of risk factors for both overt and occult UCP.
KEY MESSAGE
Overt umbilical cord prolapse (UCP) is an obstetric emergency that can lead to adverse delivery outcomes. Early identification of risk factors for both overt and occult UCP is beneficial for facilitating early interventions. Multidisciplinary team first-aid simulation training specifically for overt UCP has been shown to effectively improve neonatal outcomes.
Introduction
Umbilical cord prolapse (UCP), encompassing both overt and occult presentations, is an uncommon obstetric emergency occurring in 0.1% to 0.6% of live birth deliveries over the past decades [Citation1,Citation2]. In overt UCP, cord compression leads to fetal hypoxia. Additionally, the cooler external temperature and exposure to the environment upon prolapse can cause vasospasms in the umbilical cord vessels, further compromising fetal oxygen supply [Citation3,Citation4]. In contrast, occult UCP presents with a non-palpable cord during pelvic examination and is typically suspected only when abnormal fetal heart rate tracings are observed [Citation5,Citation6].
Over the years, many studies have investigated risk factors associated with overt UCP. These factors can be classified into general categories (breech presentation, low birth weight, etc.) and those associated with labor management (artificial rupture of membranes with a high presentation, insertion of a large balloon catheter for induction of labor, etc.) [Citation7–Citation9]. However, risk factors specifically associated with occult UCP have been rarely reported.
When UCP occurs in deliveries among patients with the aforementioned risk factors, prompt and accurate management can significantly improve neonatal outcomes [Citation9]. Studies have shown that multidisciplinary team (MDT) first-aid simulation training can enhance teamwork awareness and clinical skills among clinicians and midwives, effectively reducing adverse neonatal outcomes [Citation10,Citation11].
The study aimed to evaluate the MDT first-aid simulation usefulness by comparing delivery outcomes for UCP patients before and after its implementation, and explore risk factors for UCP in order to adapt the MDT first-aid simulation to UCP patients.
Material and methods
Design
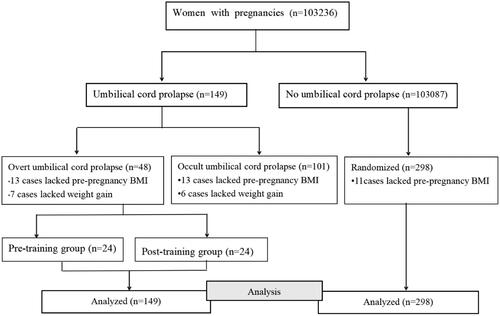
Cases of UCP that occurred between January 1998 and December 2022 were retrospectively reviewed at the Department of Obstetrics, Third Affiliated Hospital of Sun Yat-sen University. Inclusion criteria included confirmed UCP and neonatal survival. Exclusion criteria were deliveries before 28 weeks, intrauterine fetal death, and deliveries outside the hospital. A randomized code was generated using the random number generator of SPSS 20.0 statistical software. Two deliveries without UCP were matched to each delivery with UCP (2:1 control-to-case ratio) [Citation12]. A flow diagram of patient inclusion is shown in .
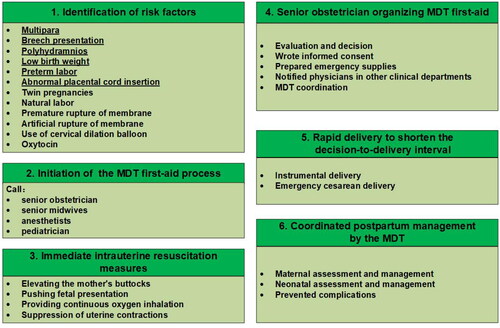
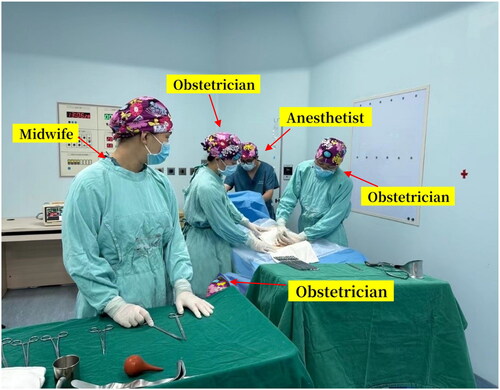
Implemented after 2014, MDT first-aid simulation training for overt UCP was held every two months for all staff. The training encompassed various scenarios of overt UCP, led by experienced instructors in emergency UCP management. The training emphasized key steps: (a) identification of risk factors, (b) initiation of the MDT first-aid process, and (c) immediate intrauterine resuscitation measures, including elevating the mother’s buttocks, pushing the fetal presentation, suppressing uterine contractions to relieve pressure on the cord, and providing continuous oxygen to the mother. (d) A senior obstetrician then organizing the MDT first-aid, prioritizing (e) rapid delivery to shorten the decision-to-delivery interval (DDI), followed by (f) coordinated postpartum management by the MDT (as illustrated in ).
Data sources and participants
Data were collected from the medical records of the Third Affiliated Hospital of Sun Yat-sen University. Diagnoses of UCP were identified by searching for the corresponding description in the patient’s medical record and the relevant International Classification of Diseases (ICD) code (O69.001). A total of 149 patients with confirmed UCP were identified. Additionally, we collected data from a control group of 298 patients who did not experience UCP.
Variables
Umbilical cord prolapse: UCP was defined as the descent of the umbilical cord through the cervix, either occult or overt, preceding the presenting part in the presence of ruptured membranes [Citation13,Citation14].
Maternal data included maternal age, pre-pregnancy body mass index (BMI), weight gain during pregnancy, presence of a uterine scar, and any pregnancy complications such as gestational diabetes mellitus and hypertensive disorders of pregnancy.
Delivery outcomes included mode of delivery, DDI, postpartum hemorrhage, puerperal morbidity (defined as a maternal body temperature ≥38 °C on two occasions within 24 h to 10 days after delivery) [Citation14], length of postpartum hospitalization, fetal distress (identified by cardiotocography monitoring of fetal heart rate and uterine contractions during labor) [Citation14,Citation15], and 1, 5, and 10-min Apgar scores, and admission to the neonatal intensive care unit (NICU).
Data extracted with respect to risk factors of UCP included gestational age at delivery, the number of past pregnancies (primigravida or multipara), abnormal placental cord insertion, breech presentation, twin pregnancy, polyhydramnios, natural labor (the spontaneous presence of uterine contractions of sufficient frequency, duration, and intensity, to cause demonstrable effacement and dilation of the cervix) [Citation14,Citation16], use of cervical dilation balloon, use of oxytocin, low birth weight (newborn’s birth weight was less than 2500 grams) [Citation14,Citation17], premature rupture of membranes and artificial rupture of membranes (the latter two items were not collected for occult UCP).
Statistical analysis
Data were presented as mean ± standard deviation (SD) for continuous variables and as counts (percentages) for categorical variables. One-way analysis of variance (ANOVA) was used to compare means between groups for normally distributed continuous data. Categorical data were compared using the chi-square test. Fisher’s exact test was employed when appropriate, such as for small sample sizes. For pairwise comparisons following significant ANOVA results, the least significant difference (LSD) method was utilized. Univariate and multivariate logistic regression analyses were performed to identify factors significantly associated with UCP. A p-value of less than 0.05 was considered statistically significant. All statistical analyses were conducted using SPSS version 20.0 statistical software.
Results
Maternal and newborn characteristics
A total of 149 deliveries with UCP occurred at the Department of Obstetrics, Third Affiliated Hospital of Sun Yat-sen University. Of these, 48 cases involved overt UCP (one fetus was stillborn and excluded from analysis). The remaining 101 cases were occult UCP. The overall UCP incidence was 0.15%, with overt UCP at 0.05% and occult UCP at 0.10%.
Compared to the control group, the overt UCP group had the highest rates of cesarean section, puerperal disease, fetal distress, and NICU admission. Additionally, they had the lowest 1, 5, and 10-min Apgar scores (all p < 0.05). The occult UCP group only showed significant differences in the cesarean delivery rate and 1-min Apgar score compared to the control group (all p < 0.05). Detailed results are summarized in .
Table 1. Comparison of basic data and clinical data in three groups.
Risk factors for UCP
The final multivariate regression analysis revealed significant correlations (all odds ratio [OR] > 1; all p < 0.05) between overt UCP and multipara labor, breech presentation, polyhydramnios, and low birth weight (). Conversely, occult UCP showed significant associations (all odds ratio [OR] > 1; all p < 0.05) with preterm labor and abnormal placental cord insertion ().
Table 2. Analysis of risk factors for overt umbilical cord prolapse.
Table 3. Analysis of risk factors for occult umbilical cord prolapse.
Cesarean section was the delivery mode for a significant portion of occult UCP patients (n = 101). Indications included UCP diagnosed by ultrasound (n = 12, where the mother requested a C-section upon learning of the condition), fetal distress (n = 26), unsuccessful labor induction or abnormal labor (n = 19), and other indications (n = 44).
UCP risk factors and delivery outcomes before and after MDT first-aid simulation training in the overt UCP group
Interestingly, no significant differences in risk factors for overt UCP were observed between patients before 2014 and those after ().
Table 4. Risk factors, maternal and infant outcomes of overt UCP before and after MDT first aid simulation training.
However, delivery outcomes did differ. Patients with overt UCP who delivered after 2014 had significantly higher cesarean section rates and 1, 5, and 10-min Apgar scores compared to those before 2014 (all p < 0.05). Additionally, the DDI was shorter, and the admission rate to the NICU was lower in the group delivering after 2014 (all p < 0.05) ().
Discussion
UCP is detrimental to maternal and neonatal outcomes
Compared to the control group, both the overt UCP and occult UCP groups in this study experienced higher cesarean section rates and longer postpartum hospital stays, attributed to the need for cesarean delivery in both groups to improve fetal outcomes. Additionally, overt UCP often necessitates emergency cesarean delivery during labor, which can lead to increased postpartum complications, as evidenced by previous researches [Citation8,Citation18,Citation19]. Supporting this notion, other studies have identified overt UCP as an independent risk factor for perinatal death (OR = 6.4, 95% CI: 4.5–9.0) [Citation20]. Our study confirms these adverse outcomes in the overt UCP group, with the highest rates of fetal distress and NICU admissions, and the lowest 1, 5, and 10-min Apgar scores. These findings suggest that overt UCP poses a greater threat to newborns than occult UCP. However, the 1-min Apgar score in the occult UCP group was still lower than the control group, and 26 patients in this group underwent cesarean delivery due to fetal distress. This highlights the potential for occult UCP to progress to overt UCP, for instance, with sudden membrane rupture [Citation5]. Therefore, early detection of both overt and occult UCP during labor remains critical for achieving positive perinatal outcomes. Consequently, obstetric staff should pay close attention to risk factors for UCP.
Importance of early identification risk factors of UCP
This study identified multiparity, breech presentation, polyhydramnios, and low birth weight as independent risk factors for overt UCP through multivariate logistic regression analysis. These findings differ to some extent from those of other related studies, which have primarily focused on intervention factors in obstetric management [Citation7,Citation8,Citation21]. For example, Tallhage et al. [Citation1] reported that labor induction and a previous cesarean section were risk factors for UCP during labor when artificial rupture of membranes was used. Similarly, Kawakita et al. [Citation22] found an association between artificial rupture of membranes and a higher UCP risk when cervical dilation was less than 6 cm. Additionally, a study investigating induction of labor (IOL) with a trans-cervical balloon catheter (TCBC) suggested an increased risk of cord prolapse with saline volumes exceeding 180 ml [Citation23]. In contrast to studies that highlight intervention-related risk factors, our approach prioritized minimizing such interventions. All obstetric procedures, including artificial rupture of membranes and intravenous oxytocin administration, were strictly guided by established protocols. Similarly, experienced doctors performed TCBC for IOL only when indicated. In these cases, a double balloon with a saline volume of 80 ml per balloon was used. By adhering to these protocols, we aimed to avoid obstetric interventions known to impede fetal presentation engagement with the lower uterine segment and/or pelvic brim, thus potentially reducing the risk of cord prolapse.
This study identified preterm labor and abnormal placental cord insertion as independent risk factors for occult UCP, aligning with findings from previous research [Citation3,Citation24]. This can be explained by two factors: 1) preterm labor often occurs before the fetal head engages in the pelvis, and 2) abnormal cord insertion places the cord closer to the cervix, just below the placenta. Both factors can contribute to the cord prolapsing through the gap between the cervix and the presenting part. Earlier detection of occult UCP, ideally before fetal distress develops, is crucial for improved neonatal outcomes. Therefore, clinicians should be vigilant for these risk factors and consider timely intrapartum ultrasound to diagnose occult UCP. Additionally, prompt cesarean delivery should be performed in women with fetal distress to minimize fetal hypoxia.
Significance of MDT first-aid simulation training for overt UCP
Early identification of patients with UCP risk factors represents a key component of the MDT first-aid simulation training program [Citation10]. This was followed by regular refresher training to maintain skills. The National Institute for Health and Clinical Excellence (NICE) Clinical Guideline recommends fetal delivery within 30 min during an emergency cesarean section [Citation25]. Instrumental delivery, when appropriate, can be an alternative to cesarean section during the second stage of labor [Citation26]. Weiner et al. also found that management protocols aimed at shortening the DDI in cases of emergency cesarean section for fetal heart rate abnormalities improved early neonatal outcomes [Citation27]. Our study results showed a significant increase in cesarean delivery rates after 2014, when all staff received standardized MDT first-aid simulation training for overt UCP every two months. This coincided with a significantly shorter DDI (20.32 ± 10.65 min), leading to improved 1, 5, and 10-min Apgar scores and lower NICU admission rates in the overt UCP group post-2014. These findings suggest that the MDT training program, as reported in other studies [Citation10,Citation11,Citation28], equipped staff to manage overt UCP patients more efficiently, reduce DDI, and facilitate faster implementation of cesarean sections or instrumental deliveries. MDT first-aid simulation training allows staff from various disciplines to practice and refine treatment procedures in high-risk scenarios, enhancing obstetric emergency management skills and teamwork [Citation29,Citation30]. Based on our findings, future training should emphasize identifying the previously analyzed high-risk factors, including multiparity, breech presentation, polyhydramnios, low birth weight, preterm labor, and abnormal placental cord insertion in all pregnant women. Additionally, the program should reinforce the importance of prenatal monitoring and care for these high-risk patients. Finally, the training should emphasize the use of prenatal ultrasound and the prompt termination of pregnancy in cases of fetal distress to optimize neonatal outcomes.
Conclusion
MDT simulation training for overt UCP effectively improves the comprehensive first-aid skills of obstetric staff, ultimately leading to better neonatal outcomes. However, the cornerstone of effective medical simulation training lies in the early identification of risk factors for both overt and occult UCP. Analyzing these factors provides a crucial foundation for subsequent training modules.
Ethics statement
This research project was approved by the Ethics Committee of the Third Affiliated Hospital of Sun Yat-Sen University.
Author contributions
Zijing Zhang and Linjia Zhong collected the data. Xiaojing Zheng, Minli Huang, Shuzhen Wu performed the data analysis and interpretation. Changping Fang, Xiaojing Zheng and Minli Huang drafted the article, Lingling Wu critically revised it, and Minli Huang and Lingling Wu gave final approval of the version to be published.
Acknowledgments
The authors would like to acknowledge and thank the clinicians and midwives who made this study possible by sharing their experiences and valuable recommendations.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data will be made available on request.
Additional information
Funding
References
- Tallhage S, Årestedt K, Schildmeijer K, et al. Incidence and risk factors for umbilical cord prolapse in labor when amniotomy is used and with spontaneous rupture of membranes: a swedish nationwide register study. Acta Obstet Gynecol Scand. 2024;103(2):1–9. doi: 10.1111/aogs.14717.
- Wong L, Kwan AHW, Lau SL, et al. Umbilical cord prolapse: revisiting its definition and management. Am J Obstet Gynecol. 2021;225(4):357–366. doi: 10.1016/j.ajog.2021.06.077.
- Holbrook BD, Phelan ST. Umbilical cord prolapse. Obstet Gynecol Clin North Am. 2013;40(1):1–14. doi: 10.1016/j.ogc.2012.11.002.
- Boushra M, Stone A, Rathbun K. Umbilical cord prolapse. Treasure Island (FL): StatPearls Publishing; 2023. https://www.ncbi.nlm.nih.gov/books/NBK542241/
- Kalu C, Umeora O. Risk factors and perinatal outcome of umbilical cord prolapse in Ebonyi state university teaching hospital. Niger J Clin Pract. 2011;14(4):413–417. doi: 10.4103/1119-3077.91746.
- Adegbola O, Ayanbode O. The incidence, risk factors and determinants of perinatal outcome of umbilical cord prolapses in Lagos, Nigeria. Niger Med J. 2017;58(2):53–57. doi: 10.4103/0300-1652.219344.
- Gabbay-Benziv R, Maman M, Wiznitzer A, et al. Umbilical cord prolapse during delivery - risk factors and pregnancy outcome: a single center experience. J Matern Fetal Neonatal Med. 2014;27(1):14–17. doi: 10.3109/14767058.2013.799651.
- Sayed Ahmed WA, Hamdy MA. Optimal management of umbilical cord prolapse. Int J Womens Health. 2018;10:459–465. doi: 10.2147/IJWH.S130879.
- Siassakos D, Hasafa Z, Sibanda T, et al. Retrospective cohort study of diagnosis-delivery interval with umbilical cord prolapse: the effect of team training. BJOG. 2009;116(8):1089–1096. doi: 10.1111/j.1471-0528.2009.02179.x.
- Copson S, Calvert K, Raman P, et al. The effect of a multidisciplinary obstetric emergency team training program, the in time course, on diagnosis to delivery interval following umbilical cord prolapse - A retrospective cohort study. Aust N Z J Obstet Gynaecol. 2017;57(3):327–333. doi: 10.1111/ajo.12530.
- Meschiari M, Kaleci S, Orlando G, et al. Risk factors for nosocomial rectal colonization with carbapenem-resistant Acinetobacter baumannii in hospital: a matched case-control study. Antimicrob Resist Infect Control. 2021;10(1):69. doi: 10.1186/s13756-021-00919-6.
- Royal College of Obstetricians and Gynaecologists. Umbilical cord prolapse (green-top guideline no. 50). London: RCOG Press; 2014.
- Xing X, Beihua K, Tao D. Obstetrics and gynecology. 9th edn. Beijing: People’s Medical Publishing House; 2018. p. 135,138,139,159,170.
- Paladugu V, Sreedhar S, Chitra R, et al. Association of CTG diagnosis of intrapartum fetal distress and immediate postpartum acidemia in foetal umbilical artery. J Obstet Gynaecol India. 2023;73(1):28–35. doi: 10.1007/s13224-022-01702-2.
- Lee L, Dy J, Azzam H. Management of spontaneous labour at term in healthy women. J Obstet Gynaecol Can. 2016;38(9):843–865. doi: 10.1016/j.jogc.2016.04.093.
- Neal JL, Lowe NK, Ahijevych KL, et al. Active labor" duration and dilation rates among low-risk, nulliparous women with spontaneous labor onset: a systematic review. J Midwifery Womens Health. 2010;55(4):308–318. doi: 10.1016/j.jmwh.2009.08.004.
- WHO recommendations for care of the preterm or low-birth-weight infant. Geneva: world Health Organization; 2022.
- Pagan M, Eads L, Sward L, et al. Umbilical cord prolapse: a review of the literature. Obstet Gynecol Surv. 2020;75(8):510–518. doi: 10.1097/OGX.0000000000000818.
- Kuhr K, Axelsson PB, Andersen BR, et al. Postoperative infections after non-elective cesarean section - a retrospective cohort study of prevalence and risk factors at a single center in Denmark administering prophylactic antibiotics after cord clamping. BMC Pregnancy Childbirth. 2022;22(1):945. doi: 10.1186/s12884-022-05300-y.
- Kahana B, Sheiner E, Levy A, et al. Umbilical cord prolapse and perinatal outcomes. Int J Gynaecol Obstet. 2004;84(2):127–132. doi: 10.1016/S0020-7292(03)00333-3.
- Kaymak O, Iskender C, Ibanoglu M, et al. Retrospective evaluation of risk factors and perinatal outcome of umbilical cord prolapse during labor. Eur Rev Med Pharmaco. 2015;19:2336–2339.
- Kawakita T, Huang CC, Landy HJ. Risk factors for umbilical cord prolapse at the time of artificial rupture of membranes. AJP Rep. 2018;8(2):e89–e94. doi: 10.1055/s-0038-1649486.
- Yamada T, Kataoka S, Takeda M, et al. Umbilical cord presentation after use of a trans-cervical balloon catheter. J Obstet Gynaecol Res. 2013;39(3):658–662. doi: 10.1111/j.1447-0756.2012.02008.x.
- Hasegawa J, Ikeda T, Sekizawa A, et al. Obstetric risk factors for umbilical cord prolapse: a nationwide population-based study in Japan. Arch Gynecol Obstet. 2016;294(3):467–472. doi: 10.1007/s00404-015-3996-3.
- Soltanifar S, Russell R. The national institute for health and clinical excellence (NICE) guidelines for caesarean section, 2011 update: implications for the anaesthetist. Int J Obstet Anesth. 2012;21(3):264–272. doi: 10.1016/j.ijoa.2012.03.004.
- Polkowski M, Kuehnle E, Schippert C, et al. Neonatal and maternal Short-Term outcome parameters in Instrument-Assisted vaginal delivery compared to second stage cesarean section in labour: a retrospective 11-Year analysis. Gynecol Obstet Invest. 2018;83(1):90–98. doi: 10.1159/000458524.
- Weiner E, Bar J, Fainstein N, et al. The effect of a program to shorten the decision-to-delivery interval for emergent cesarean section on maternal and neonatal outcome. Am J Obstet Gynecol. 2014;210(3):224.e1–224.e6. e221–226. doi: 10.1016/j.ajog.2014.01.007.
- Gallagher G, Griffin A, Clipperton S, et al. Impact of simulation training on decision to delivery interval in cord prolapse. BMJ Simul Technol Enhanc Learn. 2021;7(6):543–547. doi: 10.1136/bmjstel-2021-000860.
- Lutgendorf MA, Spalding C, Drake E, et al. Multidisciplinary in situ simulation-Based training as a postpartum hemorrhage quality improvement project. Mil Med. 2017;182(3):e1762–e1766. doi: 10.7205/MILMED-D-16-00030.
- Bogne Kamdem V, Daelemans C, Englert Y, et al. Using simulation team training with human’s factors components in obstetrics to improve patient outcome: a review of the literature. Eur J Obstet Gynecol Reprod Biol. 2021;260:159–165. doi: 10.1016/j.ejogrb.2021.03.015.