Despite Several Studies Demonstrating The Safety And Efficacy Of Transradial (TR) Versus Transfemoral (TF) Approaches For Percutaneous Coronary Intervention (PCI), This Transition For Cardiovascular Intervention Has Been Gradual [Citation1]. This Can Partly Be Explained By Rare, Yet One Of The Most Feared And Devastating Neurovascular Complications (Stroke) In Patients Undergoing TR-PCI. Previous Studies Comparing The Merits Of TR-PCI With Transfemoral (TF) PCI Had Conflicting Findings. A Study By Jolly Et Al. Demonstrated A Marginally Comparable Risk Of Stroke, While A Larger Scale Meta-Analysis Showed A Favorable Trend Of Stroke In Patients Undergoing TR-PCI [Citation2,Citation3]. In Light Of The Recent Large Scale Randomized Control Trials (Rcts), The Applicability Of Previous Meta-Analyses Is Uncertain [Citation4]. Our Study Sought To Aid In Clinical Decision Making By Collating All Studies On The Neurovascular Safety Of TR Vs. TF-PCI.
Pubmed, Embase, And Cochrane Databases Were Searched And Relevant Rcts Comparing The Safety Of TR Vs. TF PCI Were Included. The Pooled Relative Risk Ratio (RR) For Hard Clinical Endpoints Was Calculated Using The Dersimonian And Laird Method On A Random Effect Model. Quality Assessment Of The Included Studies Was Performed Using The Cochrane Collaboration Tool (Rob-2 Tool). Higgin’s Equation Was Used To Calculate Heterogeneity Among The Outcome Of Studies. All Analysis Was Performed Using Review Manager (Revman) Version-5.3 (Copenhagen: The Nordic Cochrane Center, The Cochrane Collaboration, 2008).
A Total Of 14 Rcts Comprising 19,824 Patients Were Included. There Was No Significant Difference In The Baseline Characteristics Of The Two Groups.() On Pooled Analysis There Was No Significant Difference In The Risk Of Net Cerebrovascular Events (RR 1.06, 95% CI 0.70–1.62, P = 0.9), Overall Stroke Incidence (RR 1.04, 95% CI 0.71–1.53, P = 0.75), Transient Ischemic Attacks (TIA)(RR 0.38, 95% CI 0.14–1.01, P = 0.93), Periprocedural Stroke Rate (RR 0.33, 95% CI 0.05–2.12, P = 1), 48 Hour Post-Procedure Stroke Risk (RR 1.15, 95% CI 0.42–3.17, P = 0.93) And 30-Day Post-PCI Stroke Incidence (RR 1.39, 95% CI 0.76–2.55, P = 0.97) Between Patients Undergoing TR And TF-PCI.() The Overall Quality Of The Included Studies Based On The Assessment Of Five Different Types Of Methodological Biases (Selection, Attrition, Reporting, Detection And Performance Bias) Was High. There Was Minimal To Moderate Heterogeneity In The Outcomes Of The Included Studies (I2 = 0%-50%, P > 0.05).
Figure 1. Forest Plot Showing Relative Risk Of Stroke And TIA Between Transradial And Transfemoral Percutaneous Coronary Intervention At Different Time Intervals
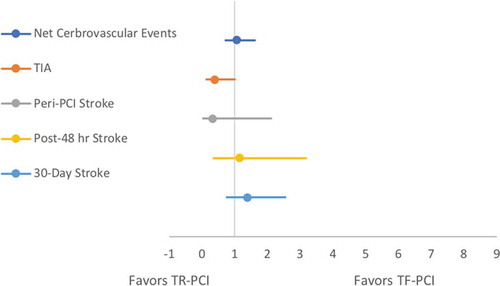
Table 1. Baseline Characteristics Of Patients In The TR And TF Groups
The Decision To Choose Between TR And TF Approach For PCI During A Time-Sensitive Door To Balloon Time In The STEMI Population Has Long Been Debated. Operators Have Conventionally Been Using Large Bore Access Through The TF Route, However TR-PCI Have Recently Gained Traction Due To A Potentially Shortened In-Hospital Stay, Lower Risk Of Bleeding And Early Recovery [Citation18]. A Recent Meta-Analysis Also Showed That TR Approach Is Associated With A Lower Rate Of Acute Kidney Injury [Citation18]. However, Some Researchers Believe That TR-PCI Carries A Higher Risk Of Post-Procedure Stroke Limiting Its Widespread Adaptation In The Cardiovascular Community.
Cerebral Embolization Secondary To Catheter Manipulation Of The Atherosclerotic Plaque, Disruption Of Unstable Thrombus At The Access Site, De-Novo Thrombus Formation At The Catheter Site And Air Embolism Are All Suggested Mechanisms For Post-PCI Stroke [Citation19]. Since Patients With The Acute Coronary Syndrome (ACS) Are At A Higher Risk Due To Significant Atherosclerotic Debris In Their Arteries, Any Invasive Manipulation Can Potentially Dislodge This Debris Leading To Embolism. This Tropism Of Neurological Complications Associated With The TR Approach Can Be Explained By Two Simple Facts Of The Proximity Of The TR Approach To Cerebral Vessels And Increased Duration Of Intravascular Manipulation Of The Guidewire/Catheter. Theoretically, These Mentioned Possible Factors Can Lead To Various Neurological Manifestations.
Our Meta-Analysis In This Context Studied Both The Immediate And Long-Term Post-PCI Incidence Of Cerebrovascular Events, Demonstrating An Identical Rate Stroke And TIA In Both TR And TF Approaches At All Timelines. It Should, However, Be Noted That The Overall Incidence Of TIA Or Ischemic Strokes Were Rare In Both Procedures. This Might Be Because Clinically We See Only One-Tenth Of Cerebral Embolism And The Majority Of Events Are Minute Which Can Only Be Seen By Diffusion Weighted Magnetic Resonance Imaging (MRI) [Citation20]. Additionally, Our Study Is Not Designed To Assess The Efficacy Or Other Safety Endpoints (Bleeding, Mortality) Of The Two Approaches.
In Nutshell, Our Study Provides Stronger Evidence That The Risk Of TIA And Stroke Is Rare And Identical In Patients Undergoing TR Or TF-PCI.
Declaration of interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose
Author contributions
Conception and Writing: Hafeez Ul Hassan Virk
Data collection: Mohammed Ahmed, Christian F Witzke
Manuscript writing and Analysis: Waqas Ullah
Critical Review: Saurav Chattarjee
Supervision and Validation: Sahil Banka
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Additional information
Funding
References
- Aggarwal A, Dai D, Rumsfeld JS, et al. Incidence and predictors of stroke associatedwithpercutaneouscoronaryintervention. AmJCardiol. 2009;104:349–353.
- Jolly SS, Amlani S, Hamon M, et al. Radial versus femoral access for coronary angiography or intervention and the impact on major bleeding and ischemic events: a systematic review and meta-analysis of randomized trials. Am Heart J. 2009;157:132–140.
- Patel V, Brayton KM, Dharam J, et al. Meta-analysis of stroke after transradial versus transfemoral artery catheterization. Int J Cardiol. 2013;168:5234–5238.
- Valgimigli M, Gagnor A, Paolo C. Radial versus femoral access in patients with acute coronary syndromes undergoing invasive management: a randomized multicenter trial. Lancet. 2015;385:2465–2476.
- Bernat I, Horak D, Stasek J, et al. ST-segment elevation myocardial infarction treated by radial or femoral approach in a multicenter randomized clinical trial: the STEMI-RADIAL trial. J Am Coll Cardiol. 2014 Mar 18;63(10):964–72.
- Romagnoli E, Biondi-Zoccai G, Sciahbasi A, et al. Radial versus femoral randomized investigation in ST-segment elevation acute coronary syndrome: the RIFLE-STEACS (Radial Versus Femoral Randomized Investigation in ST-Elevation Acute Coronary Syndrome) study. J Am Coll Cardiol. 2012 Dec 18;60(24):2481–2489.
- Chodór P, Kurek T, Kowalczuk A, et al. Radial vs femoral approach with StarClose clip placement for primary percutaneous coronary intervention in patients with ST-elevation myocardial infarction. RADIAMI II: a prospective, randomised, single centre trial. Kardiol Pol. 2011;69(8):763–771.
- Jolly SS, Yusuf S, Cairns J, et al. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomised, parallel group, multicentre trial. Lancet. 2011 Apr 23;377(9775):1409–20. doi:DOI: 10.1016/S0140-6736(11)60404-2.
- Koltowski L, Filipiak KJ, Kochman J, et al. Access for percutaneous coronary intervention in ST segment elevation myocardial infarction: radial vs. femoral ‐ a prospective, randomised clinical trial (OCEAN RACE). Kardiologia Polska. 2014;72(7):604‐611.
- Brueck M, Bandorski D, Kramer W, et al. A randomized comparison of transradial versus transfemoral approach for coronary angiography and angioplasty. JACC Cardiovasc Interv. 2009 Nov;2(11):1047–1054. doi:DOI: 10.1016/j.jcin.2009.07.016.
- Chodór P, Krupa H, Kurek T, et al. RADIal versus femoral approach for percutaneous coronary interventions in patients with Acute Myocardial Infarction (RADIAMI): A prospective, randomized, single-center clinical trial. Cardiol J. 2009;16(4):332–40.
- Achenbach S, Ropers D, Kallert L, et al. Transradial versus transfemoral approach for coronary angiography and intervention in patients above 75 years of age. Catheter Cardiovasc Interv. 2008 Nov 1;72(5):629–35. doi:10.1002/ccd.21696.
- Cantor WJ, Puley G, Natarajan MK, et al. Radial versus femoral access for emergent percutaneous coronary intervention with adjunct glycoprotein IIb/IIIa inhibition in acute myocardial infarction--the RADIAL-AMI pilot randomized trial. Am Heart J. 2005 Sep;150(3):543–9.doi:10.1016/j.ahj.2004.10.043.
- Louvard Y, Benamer H, Garot P, et al. Comparison of transradial and transfemoral approaches for coronary angiography and angioplasty in octogenarians (the OCTOPLUS study). Am J Cardiol. 2004 Nov 1;94(9):1177–80.
- Louvard Y, Lefèvre T, Allain A, et al. Coronary angiography through the radial or the femoral approach: The CARAFE study. Catheter Cardiovasc Interv. 2001 Feb;52(2):181–7.
- Cooper CJ, El-Shiekh RA, Cohen DJ, et al. Effect of transradial access on quality of life and cost of cardiac catheterization: A randomized comparison. Am Heart J. 1999 Sep;138(3 Pt 1):430–6.
- Benit E, Missault L, Eeman T, et al.Brachial, radial, or femoral approach for elective Palmaz‐Schatz stent implantation: a randomized comparison. Catheterization and Cardiovascular Diagnosis 1997;41:124‐30.
- Andò G, Gragnano F, Calabrò P, et al. Radial vs femoral access for the prevention of acute kidney injury (AKI) after coronary angiography or intervention: A systematic review and meta‐analysis. Cathet Cardiovasc Interv. 2018 Dec 1;92(7):E518–26.
- Segal AZ, Abernethy WB, Palacios IF, et al. Stroke as a complication of cardiac catheterization: risk factors and clinical features. Neurology. 2001;56:975–977.
- Busing KA, Schulte-Sasse C, Fluchter S, et al. Cerebral infarction: incidence and riskfactors after diagnostic and interventional cardiac catheterization–prospective evaluation at diffusion- weighted MR imaging. Radiology. 2005;235:177–183.
