ABSTRACT
Background: This is the first detailed Indian electronic medical record (EMR)-based real-world observational study to understand the clinical characteristics, associated comorbidities/risk factors and treatment(s) of CAD patients across India.Methods: EMR data of adult Indians (aged ≥ 18 years) diagnosed with CAD was retrospectively analyzed.Results: The majority of the participants had stable IHD (93%), were men (68.5% in ACS, 59.8% in stable IHD), most common age group was 40–64 years in ACS (56.6%) and stable IHD (51.4%). Both are common in metros (ACS 52%, 62% stable IHD). There is a high frequency of hypertension (38.2% in ACS, 59% in stable IHD) and diabetes mellitus (32.3% in ACS, 57.6% in stable IHD). Most common treatments are antiplatelet drugs and lipid-lowering drugs (96%).Conclusions: In India, stable IHD is the most prevalent form in vast majority of patients. The patients with CAD are mostly males, are mainly located in metros and majority fall between the age group of 40–64. The major comorbidities are hypertension and diabetes mellitus. Sociodemographic and clinical characteristics for CAD in India may not be similar to what is reported from the west. There is a significant difference in drug usage and adherence to guidelines in India for CAD.
1. Introduction
In spite of the recent advances in the prevention and management of athero-thrombosis, coronary artery disease (CAD) [Citation1] still remains the primary cause of mortality worldwide. Further, CAD is still a major public health burden [Citation2]. In India, cardiovascular diseases (CVD) are one of the leading causes of mortality and morbidity [Citation1]. According to The Global Burden of Diseases (GBD) Study, Ischemic Heart disease (IHD) in India increased to become the number one cause of death from year 1990 to 2013.
Stable IHD (SIHD) in India has shown steady increase in numbers, geographic variations, early onset, lack of quality management, and high mortality [Citation1]. According to the INTERHEART study 9 standard risk factors - dyslipidemia (high apolipoprotein B/apolipoprotein A1 ratio), smoking, hypertension, diabetes, high waist-hip ratio, unhealthy diet, low physical activity, irregular alcohol consumption and psychosocial stress - can be attributed for more than 90% of the first acute myocardial infarction cases. Early onset of the same biological risk factors was shown to explain the incidence of premature IHD in the South Asian region in the INTERHEART study [Citation1]. Increase in life expectancy and increases in the prevalence of risk factors such as diabetes mellitus (DM) and obesity along with the improved survival of patients presenting with acute coronary syndrome, is likely to cause a rise in the number of patients with CAD.
Clinical characteristics, CV risk factors, management, and the treatment outcomes of patients with CAD have changed remarkably over the years [Citation2]. Occurrence and outcomes in both ACS and IHD are dependent on the prevalence of risk factors in the population, availability and easy access to good quality and evidence-based healthcare services, and awareness and inclination toward healthy behavior. These characteristics in turn are all a function of social, economic, geographical factors and cultural habits. Therefore, in a country as diverse as India these characteristics in turn influence the occurrence, treatment and outcomes of ACS and IHD and are bound to be varied across different regions of the country. Most of the large registries on CAD are from western countries with very few Indian studies.
One of the largest ACS registries in India: CREATE (20,937 patients; 2001–2005) registry is more than decade old [Citation3] and more recent registries: Kerala ACS registry [Citation4], HP ACS registry and DEMAT [Citation5] registries focused more on ACS patients and the CADY registry focused on premature IHD. This will be one of the first Indian electronic medical records-based study to assess the clinical characteristics, risk factors, and treatment patterns of coronary artery disease patients across India across the entire spectrum of coronary artery disease (stable IHD and acute coronary syndrome), across age groups and genders.
2. Methods
2.1. Data sources
This retrospective study used anonymous data extracted from EMR. This EMR database captured clinical information directly from the clinical encounter, including patient demographics, diagnosis, agents prescribed, comorbidities, risk factors, tests, test results, procedures, functional status, and other data elements for patients receiving ambulatory care treatment at physicians’ offices across India. EMR of all the patients satisfying the inclusion criteria of the study was collected. The criteria for the objective diagnosis of CAD were based on the discretion of the physician in medical records. Further, patient’s admissibility into this retrospective study was based on the review of medical records, as per the inclusion and exclusion criteria. Patients included were of age group ≥ 18-years in EMR database meeting the inclusion criteria.
Inclusion criteria
•Must have CAD as a diagnosis (Clinical diagnosis by physician) and includes patients with both Stable Ischemic heart disease and Acute coronary syndrome (STEMI, NSTEMI, Unstable angina)
•Must be ≥18 years old
•Patient follow up data available up to 3 visits from baseline visit
Exclusion criteria
Key exclusion criteria
•Patients in EMR system with diagnosis (clinical diagnosis by physician) of CAD prior to study data period
•Patients <18-year-old
•Patients who had no coronary artery disease mentioned at the entry
•Patients with no follow up data available
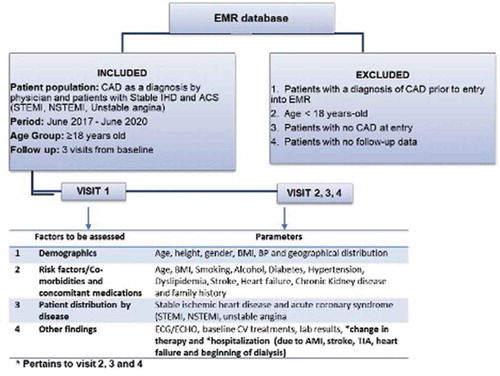
For further details refer to . Please note that data for family history, electrocardiographic and echocardiographic characteristics were not captured in the EMR database and hence have not been reported in the study.
Figure 1. Overall study design with inclusion, exclusion criteria and various parameters at baseline and follow-up visit to be assessed
Data were collected from an Indian electronic software owned and administered by HealthPlix Technologies PRV. This software has been in operation since 2016 and fulfills day-to-day operational needs of 12 medical specialties across 150+ cities in 20 states.
2.2. Study design and endpoints
For full details of study design including inclusion and exclusion criteria kindly refer to .
The primary endpoint was to assess demographics, risk factors, co-morbidities and type of CAD at baseline. The secondary endpoints were aimed at evaluating the treatment patterns by type of coronary artery disease.
2.3. Statistical analysis
The study was conducted as per the applicable national regulatory laws and guidelines. The study protocol was approved on 06/11/2020 by the Surakhsha- Ethics Committee, Asian Institute of Medical Sciences, Plot 72, Milap Nagar, MIDC, Dombivli, 421,203. Patient confidentiality was ensured at all times since the study was performed using anonymized information only.
Pertinent retrospective data, relevant to the defined study objectives were sourced from the EMR database and collated according to the study parameters using a pre-defined templated data collection form. The collated and organized data were investigated to ensure use of an accurate, reliable, consistent, and reproducible data set for subsequent statistical analyses. Any deviations in the data set, such as non-identifiable data, gaps, and missing and non-applicable data points were indicated and appropriately documented in the data collection form. The study sponsor had no direct access to the source EMR data.
Classical statistics was employed for data modeling and statistical analysis. An appropriate statistical null hypothesis was developed based on defined study objectives and subsequently tested using the appropriate parametric or non-parametric statistical tests. Pearson’s first coefficient of skewness was measured for continuous data. Central tendency & dispersion for continuous distributed data were evaluated and reported in terms of mean and standard deviation. Means were compared using Students t test and proportions were compared using the Z test. Nominal data were reported in terms of numbers or/and percentages. Unless otherwise specified, p-value < 0.05 was determined to be the metric for statistical significance.
3. Results
3.1. Primary endpoints
EMR data from 58,701 patients who met the inclusion criteria was analyzed to assess demographics, risk factors, co-morbidities, distribution of ACS and SIHD in CAD patients at baseline. Stable IHD comprised 93% (n = 54,830) and with ACS were 7% (n = 3,871). Patient data at baseline are presented in .
Table 1. Patient clinical profile at baseline visit
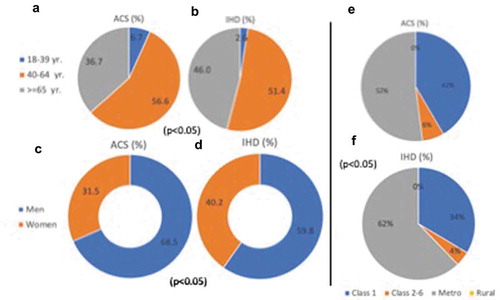
As presented in C-D, males comprised of 68.5% of study population in ACS and 59.8% of study population in SIHD (p < 0.05). Females represented 31.5% of the study population in ACS and 40% in SIHD (p < 0.05%). The vast majority of patients were in the 40–64 years old age group A-B (56.6% ACS and 51.4% SIHD, p < 0.05) with predominant geographical distribution being in metros E-F (52% ACS and 62.1% SIHD, p < 0.05).
Figure 2. Overall patient demographics by age (A, B), gender (C, D), and location (E, F). Class 1: City tier 1, population according to 2001 census >100,000, Class 2-6: City tier 1, population according to 2001 census = 10,000–100,000, Metro: city with population according to 2001 census >1000,000, Rural: area with population according to 2001 census <10,000
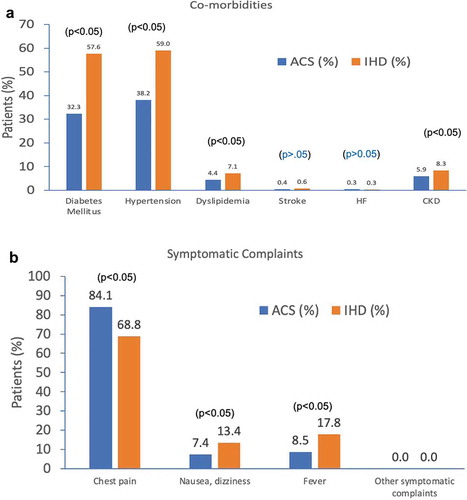
As highlighted in A-B, based on the inclusion criteria, further data were collected and analyzed to evaluate any existing baseline co-morbidities/underlying conditions and risk factors along with the type of CAD. These data are presented in A-B below based on the inclusion criteria described in . Majority of the patients with both stable IHD and ACS had underlying comorbidity/medical conditions including hypertension (59% in SIHD and 38% in ACS population, p < 0.05), followed by diabetes mellitus (57.6% in ACS and 32.3% in SIHD, p < 0.05), CKD (5.9% in ACS and 8.3% in SIHD, p < 0.05), and dyslipidemia (4.4% in ACS and 7.1% in SIHD) as evident from A. Further, data collected showed symptomatic complaints including chest pain, fever, and nausea/dizziness B. Most common complaint was chest pain (84.1% in ACS and 68.8% in SIHD p < 0.05), followed by fever (8.5% in ACS and 17.8% in SIHD p < 0.05), followed by nausea/dizziness (7.4% in ACS and 13.4% in SIHD p < 0.05).
Figure 3. Major co-morbidities, risk factors and symptomatic complaints observed in the data collected for patients with ACS and stable IHD
Additionally, laboratory findings suggested an elevated mean levels of serum creatinine (1.48 mg/dL in ACS and 1.5 mg/dL in SIHD), LDL (94.7 mg/dL in ACS and 93.06 mg/dL in SIHD), total cholesterol (155.7 mg/dL in ACS and 167.3 mg/dL in SIHD p < 0.05), HDL (44.5 mg/dL in ACS and 42.8 mg/dL in SIHD), triglycerides (145.8 mg/dL in ACS and 160.3 mg/dL in SIHD p < 0.05), HbA1C (8.06 mmol/L in ACS and 8.5 mmol/L in SIHD p < 0.05) and eGFR (63.5 mL/min in ACS and 62.6 mL/min in SIHD) in both the patient pools including SIHD and ACS . In the current study, tobacco consumption was seen in only 1.1% ACS and 2.1% SIHD patients. This is much lower than that observed in European and Indian studies (5,1).
3.2. Secondary endpoints
The overall objective was to analyze and compare the treatment patterns determined from the EMR data analysis and data modeling with respect to type of CAD, at baseline.
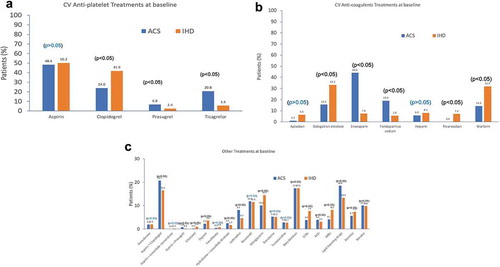
To capture and understand the treatment patterns, data were analyzed at baseline for both patients with stable IHD and ACS. Details of drug/drug class administered are shown in A-C.
Overall, 52.6% ACS patients and 16% of SIHD patients received antiplatelet drugs A (aspirin, clopidogrel (24% in ACS and 41.9% in SIHD p < 0.05), prasugrel (6.8% in ACS and 2.4% in SIHD, p < 0.05) or ticagrelor (20.8% in ACS and 5.5% in SIHD, p < 0.05). Further, 2.2% of ACS and 0.8% of SIHD patients received anticoagulants (apixaban, enoxaparin (44% ACS and SIHD 14% p < 0.05), fondaparinux sodium, (19% ACS and 5.6% p < 0.05), heparin, rivaroxaban (none in ACS and 7.2% SIHD p < 0.05), warfarin (14.3% in ACS and 31.9% in SIHD p < 0.05), and dabigatran etexilate (15.5% in ACS and 7.4% in SIHD p < 0.05)), B. Lipid lowering drugs including rosuvastatin and atorvastatin were prescribed to 45% patients with ACS and 21% patients with SIHD. Beta blockers were prescribed to 42% ACS and 30% SIHD patients (p < 0.05). ACE inhibitors and ARBs were 9.5% and 9.9% (p < 0.05) respectively in ACS. In SIHD ACE inhibitors were prescribed to 4.6% and ARBs to 12% (p < 0.05) of the patients. Calcium channel blockers were prescribed in 9% ACS and 11.7% SIHD patients, nitrates in 24% ACS and 15% SIHD (p < 0.05) and diuretics 5.7% in ACS and 7.3% in SIHD (p < 0.05).
4. Discussion and conclusions
Overall, the collected data suggested that majority of the patients with CAD had SIHD (93%). Studies in US, have shown that there are 30 patients of SIHD for every patient with ACS [Citation6]. An Indian study has shown higher prevalence of ACS than IHD, though the authors of the study contend that estimation of IHD is an underestimate. The true prevalence in India would be similar to statistics shown by studies in the US [Citation1]. Both patients in the ACS and IHD cohorts exhibit a trend of obesity/overweight, similar to previous studies [Citation1]. .
Most of the patients in ACS as well as SIHD cohorts were males, located in metros and had an age group of 40–64 years. Western as well as some Indian registries have shown a similar gender distribution skewed toward CAD being more common amongst males [Citation1,Citation5,Citation7]. Data from the current study is consistent with earlier studies showing that CAD appears to be more common in age group 40–64 years in the Indian setting [Citation1,Citation3] versus >65 years in the west [Citation5,Citation7].
Additionally, study data suggest that amongst ACS and SIHD, there is a higher proportion of ACS in males as compared to SIHD. Further, the proportion of ACS is also higher in the 40–64-year age group. While a higher proportion of SIHD is seen in metro cities (see ).
Majority of patients with both stable IHD and ACS had underlying comorbidity/medical conditions including hypertension (59% in SIHD and 38.2% in ACS population) followed by diabetes mellitus (57.6% in SIHD and 32.3% in ACS population), CKD (5.9% in ACS and 8.3% in SIHD, p < 0.05), and dyslipidemia (4.4% in ACS and 7.1% in SIHD) as shown in . This pattern of comorbidities is similar to what has been reported previously in India [Citation1] but is not consistent with what is observed in western registries, where dyslipidemia [Citation5,Citation7] appears to be most prevalent comorbidity/risk factor associated with CAD. Further, current study data suggests that the prevalence of comorbidities like hypertension, diabetes, dyslipidemia, and CKD is significantly higher in SIHD compared to ACS (p < 0.05).
The symptomatic complaints in IHD and ACS patients included chest pain (84.1% in ACS and 68.8% in SIHD p < 0.05), followed by fever (8.5% in ACS and 17.8% in SIHD p < 0.05), followed by nausea/dizziness (7.4% in ACS and 13.4% in SIHD p < 0.05). While chest pain is a more commonly reported symptom in ACS (p < 0.05), fever, nausea/dizziness are more commonly reported in SIHD (p < 0.05) B. This trend of symptomatic complaints in SIHD is similar to that reported in some previous studies on SIHD in India [Citation8].
Additionally, laboratory findings suggested an overall elevated mean level of HbA1C in both ACS and SIHD (8.06% in ACS and 8.5% in SIHD p < 0.05) similar to trends observed previously in Indian setting [Citation9] . While we also observed that mean total cholesterol (155.7 mg/dL in ACS and 167.3 mg/dL in SIHD p < 0.05), triglycerides (145.8 mg/dL in ACS and 160.3 mg/dL in SIHD p < 0.05), and HbA1C (8.06% in ACS and 8.5% in SIHD p < 0.05) are all higher in SIHD patients than ACS.
In terms of therapies prescribed, the current study data show that overall, the choice of therapies is very similar for both ACS and SIHD in Indian settings. However, amongst the antiplatelets clopidogrel (24% in ACS and 41.9% in SIHD p < 0.05) appears to be more frequently used in SIHD, while prasugrel (6.8% in ACS and 2.4% in SIHD, p < 0.05) and ticagrelor (20.8% in ACS and 5.5% in SIHD, p < 0.05) are more frequently used in ACS (). Further the data also indicates that the use of antiplatelet agents (52.6% ACS patients and 16% of SIHD) is much lower than that observed in European studies [Citation2,Citation10], or even in some previous Indian studies (3). The level of use is also not consistent with the clinical guidelines, which recommend antiplatelet therapy in all patients with CAD unless contraindicated [Citation11,Citation12]. The nationwide CREATE registry (n = 20,468) has also reported that the use of evidence-based medical drugs (thrombolytics, beta-blockers, antiplatelets, and statins) is low in India. Similar results were reported in Kerala ACS registry (n = 25,748) and multicenter DEMAT and SPREAD registries.
Further, the use of anticoagulants, 2.2% of ACS and 0.8% of SIHD patients received anticoagulants (apixaban, enoxaparin (44% ACS and SIHD 14% p < 0.05), fondaparinux sodium, (19% ACS and 5.6% p < 0.05) as well lipid lowering drugs including rosuvastatin and atorvastatin were prescribed to 45% patients with ACS and 21% patients with SIHD is also lower in Indian CAD population. The use of ivabradine (8.1% in ACS and 4.7% in SIHD p < 0.05), beta blockers were prescribed to 42% ACS and 30% SIHD patients (p < 0.05), ACE inhibitors and ARBs (9.5% and 9.9% (p < 0.05) respectively in ACS and 4.6% and ARBs to 12% (p < 0.05) in SIHD) of the patients, calcium channel blockers (9% ACS and 11.7% SIHD patients), nitrates (24% ACS and 15% SIHD (p < 0.05)) and diuretics (5.7% in ACS and 7.3% in SIHD (p < 0.05)) is all consistently lower than that seen in western registries [Citation11,Citation13]. Further, the CLARIFY registry describes a much higher use of Beta blockers (>70%), ACEI/ARBs (>50% in SIHD) and diuretics (>20%) which is not in line with the current study [Citation2]. This points toward a need for more evidence-based treatment practices in the Indian setting.
However, data from this study suggests that amongst the anticoagulant’s enoxaparin and fondaparinux are both more frequently prescribed in ACS. Ivabradine, beta blockers, ACE’s and nitrates are also more frequently used for ACS. While ARBs, CCBs, and diuretics seem to be more commonly used for SIHD ().
4.1. Limitations and strengths
Some limitations of the current study should be considered when studying the results. Such as the set-up of the EMR collection systems. The penetration would be more in bigger tier cities and metros due to socio geographic factors in India. Thus, this method of data collection in India raises the issue of whether the sample is representative of the population under study. The study being retrospective is another limitation. Different methods used to detect CAD at various centers is another limitation. However, several factors contribute to the importance of this study, such as the large number of patients enrolled in the study and, in particular, the similarity of its results with those of other studies in the Indian patient population. This large patient number makes the results more generalizable. Despite these limitations, the current study has several novel findings to offer such as detailed information on sociodemographic, clinical characteristics and daily clinical practice in across the entire spectrum of ACS and SIHD in CAD patients, which has not been previously provided by any other study in India.
4.2. Conclusions
We evaluated the overall prevalence of ACS and SIHD in India along with the treatment patterns for CAD across India.
In India, similar to the west SIHD seems to be the most prevalent form in vast majority of patients. Patients with ACS and SIHD patients were mainly located in metros and majority fell between the age group of 40–64. Males composed of majority of the patients. The major underlying comorbidity/medical conditions including hypertension, diabetes mellitus, CKD, and dyslipidemia. Data from the current study indicates that sociodemographic and clinical characteristics for ACS and SIHD in Indian settings may not be similar to data that has been reported from the west.
In terms of drug usage there is a significant difference in drug usage and adherence to recommended treatment guidelines in India both for SIHD and ACS.
Abbreviations
EMR - Electronic Medical Records, CAD- Coronary Artery Disease, IHD- Ischemic Heart Disease, ACS-Acute Coronary Syndrome, BMI-Body Mass Index, BP-Blood Pressure, TIA-Transient Ischemic Attack.
Ethics approval
The study protocol was approved on 06/11/2020 by the Surakhsha- Ethics Committee, Asian Institute of Medical Sciences, Plot 72, Milap Nagar, MIDC, Dombivli, 421,203.
Author contributions
MY Khan, SA Pandit, K Gauray and A Mane developed the concept and performed the study. SS performed data analysis. YK and SP drafted the manuscript. A
ll authors reviewed the manuscript and gave final approval.
Declaration of interest
S Guha, U Jadhav and MS Rao are board members for Dr Reddy’s Laboratories Ltd. MY Khan, S Pandit, K Gaurav and A Mane are members of the Medical Affairs Department in Dr Reddy’s Laboratories Ltd. S Shah is an employee of Healthplix. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Acknowledgments
The authors thank PharmaSolutions360 LLC for their support to the preparation of the manuscript.
Availability of data and material
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Additional information
Funding
References
- Iyengar SS, Gupta R, Ravi S, et al. Premature coronary artery disease in India: coronary artery disease in the young (CADY) registry. Indian Heart J. 2017;69(2):211–216.
- Sorbets E, Greenlaw N, Ferrari R, et al. Rationale, design, and baseline characteristics of the CLARIFY registry of outpatients with stable coronary artery disease. Clin Cardiol. 2017;40(10):797–806.
- Xavier D, Pais P, Devereaux PJ, et al., investigators, C. r. Treatment and outcomes of acute coronary syndromes in India (CREATE): a prospective analysis of registry data. Lancet. 2008;371(9622):1435–1442.
- Mohanan PP, Mathew R, Harikrishnan S, et al. Presentation, management, and outcomes of 25 748 acute coronary syndrome admissions in Kerala, India: results from the Kerala ACS Registry. Eur Heart J. 2013;34(2):121–129.
- Pagidipati NJ, Huffman MD, Jeemon P, et al. Association between gender, process of care measures, and outcomes in ACS in India: results from the detection and management of coronary heart disease (DEMAT) registry. PLoS One. 2013;8(4):e62061.
- Zamorano JL, Garcia-Moll X, Ferrari R, et al. Demographic and clinical characteristics of patients with stable coronary artery disease: results from the CLARIFY registry in Spain. Rev Esp Cardiol (Engl Ed). 2014;67(7):538–544.
- Esmatjes E, Blanco AJ. [The REACH registry: baseline and 1-year results]. Med Clin (Barc). 2009;132Suppl 2:5–9. . (Registro REACH: datos basales y a 1 ano.)
- N, H. K. H. A retrospective study on the profile of ischemic heart disease (IHD) cases admitted in KMC Attavar Mangalore. J Clin Exp Cardiolog. 2014;5:3.
- Hiremath S, Vala DR, Roy T, et al. Changing patterns in the prevalence and management of cardiovascular risk factors in India and their comparison with the rest of the world along with clinical outcomes at 5-year: an analysis of stable coronary artery disease patients from The prospective observational longitudinal registry of patients with stable coronary artery disease (CLARIFY) registry. Indian Heart J. 2018;70(Suppl 3):S36–S42.
- Cordero A, Bertomeu-Martinez V, Mazon P, et al. Differences in medical treatment of chronic coronary heart disease patients according to medical specialities. Cardiovasc Ther. 2009;27(3):173–180.
- Perk J, De Backer G, Gohlke H, et al., European Association for Cardiovascular, P., & Rehabilitation. European guidelines on cardiovascular disease prevention in clinical practice (version 2012) : the fifth joint task force of the European society of cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts). Int J Behav Med. 2012;19(4):403–488. .
- Mishra S, Ray S, Dalal JJ, et al. Management standards for stable coronary artery disease in India. Indian Heart J. 2016;68(Suppl 3):S31–S49.
- Civeira F, International Panel on Management of Familial, H. Guidelines for the diagnosis and management of heterozygous familial hypercholesterolemia. Atherosclerosis. 2004;173(1):55–68. .