1. Introduction
Non-communicable diseases accounted for 74% of deaths globally in 2019, with cardiovascular disease (CVD) persisting as the leading cause of death [Citation1]. Atherosclerotic CVD or arterial thrombotic disease, which includes ischemic heart disease and cerebrovascular disease (mainly ischemic stroke) [Citation2], are the main clinical manifestations of CVD. Atherosclerotic CVD poses immense health and economic burdens globally. Major risk factors for atherosclerotic CVD include age, sex, family history, race, hypertension, high cholesterol levels, smoking, diabetes, overweight or obesity, physical inactivity, unhealthy diet, and stress [Citation3]. Given the significant challenges attributed to CVDs in the United States (US), the American Heart Association (AHA) developed a metric to tackle the burden of CVD among the US population, which is based on positively modifying four health behaviors (smoking, body mass index (BMI), physical activity, and diet) and three health factors (blood pressure (BP), fasting blood glucose and total cholesterol levels) [Citation4].
Venous thromboembolism (VTE) which includes both deep vein thrombosis (DVT) and pulmonary embolism (PE), is the third most common (CVD) [Citation5,Citation6]. Deep vein thrombosis is the most frequent presentation of VTE, with PE being the most serious clinical presentation of VTE. Though about 10 million cases of VTE occur annually across low-, middle- and high-income countries, fatal events related to VTE are largely undocumented [Citation7,Citation8]. It has been reported that estimating the number of confirmed deaths attributable to VTE is challenging partly due to the multifactorial nature of deaths and the low rates of autopsy in most countries [Citation8]. Apart from being a leading and preventable cause of deaths, VTE is associated with substantial disability and health-care costs like atherosclerotic CVD [Citation9,Citation10]. Major risk factors implicated in VTE development include immobilization, trauma, surgery, cancer, hormonal therapy, obesity, and hypercoagulation disorders [Citation11]. Unlike atherosclerotic CVD, lifestyle factors are reported to make minimal contributions to the risk of VTE. However, recent epidemiological data based on population attributable risks (PARs) in the US estimate that obesity may contribute to 30% of VTEs, Western dietary patterns to 11%, physical inactivity to 4%, and current smoking to 3% [Citation12].
Though distinct diseases, atherosclerotic CVD and VTE are closely related disease conditions; they share (i) common risk factors such as age, obesity, and cigarette smoking [Citation13–15], (ii) common pathophysiological mechanisms such as coagulation, platelet activation, and dyslipidaemia [Citation16], and (iii) common preventive and/or therapeutic strategies which include aspirin, heparin, and warfarin [Citation17]. Despite substantial progress made in understanding the epidemiology of both conditions and the development of several effective preventive strategies, they remain a global public health burden.
It appears that CVDs (including VTE), at least in part, may be due to inappropriate or poor dietary and other lifestyle habits, of which a major element is physical activity [Citation18]. Physical activity is defined as any bodily movement produced by skeletal muscles that requires energy expenditure and includes exercise as well as usual occupational and/or domestic activity [Citation19]. The role of physical activity in promoting health and preventing atherosclerotic CVD, mortality, and other chronic diseases is well established [Citation20,Citation21]. Physical inactivity, typically defined as not meeting specified physical activity guideline recommendations [Citation19,Citation22], is not the exact inverse of physical activity. Sedentary behavior, commonly and erroneously referred to as physical inactivity, is defined as any waking behavior characterized by low levels of metabolic energy expenditure (≤1.5 metabolic equivalents, METs) while in a sitting, reclining,or lying posture [Citation23,Citation24]. Sitting time is a sub-component of sedentary behavior and one of the main indicators used to quantify the time devoted to sedentary behaviors [Citation25]. Though physical inactivity and sedentary behavior are different constructs, they are among the leading modifiable risk factors for several chronic disease conditions, atherosclerotic CVD and mortality [Citation26–28]. Emerging evidence also shows regular physical activity to be associated with a reduced risk of VTE [Citation29]; though physical inactivity and prolonged sedentary behavior are not the inverse constructs of physical activity, they are part of the same energy spectrum [Citation30] and may increase the risk of VTE. Indeed, several observational studies have reported associations of physical inactivity and sedentary behaviors such as long-distance travel with an increased risk of VTE [Citation31,Citation32].
Prolonged television (TV) viewing (usually defined as watching TV at least 4 hours/day [Citation33–36]) is one of the most predominant sedentary, passive behaviors in industrialized countries [Citation37]. It is important to note that though TV viewing time and total sitting time are common self-report measures of sedentary behavior, they are not interchangeable measures of sedentary behavior [Citation38]. Prolonged TV viewing has consistently been shown to be associated with an increased risk of atherosclerotic CVD, other chronic diseases and mortality [Citation35,Citation36,Citation39–41]. Prolonged TV viewing is henceforth referred to as binge TV viewing, given that the term ‘binge watching’ refers to long periods of focused, deliberate viewing of TV content, which may be planned, purposeful activity, or unintentional [Citation42]. The impact of binge TV viewing on these adverse health outcomes can be mainly attributed to the sedentary behavior associated with TV viewing. The adverse impact of sedentary behaviors is of immense clinical and public interest and the past decade has witnessed increasing research activity in the area. It is a very important topic given the substantial public health burden attributed to CVDs, high prevalence of sedentary behaviors and the fact that most adults in industrialized nations spend majority of their awake times being sedentary [Citation43,Citation44]. Even more worrying is the fact that detrimental effects associated with TV viewing have been observed in adults who met public health guidelines for physical activity [Citation45]. Though there is a large body of evidence on the associations of binge TV viewing with the risk of atherosclerotic CVD, other chronic diseases and mortality, there are only few studies that have evaluated the association between TV viewing and VTE risk. This commentary paper summarizes the available evidence on the relationships between binge TV viewing and CVDs (including VTE), given CVDs and VTEs are the leading causes of mortality; the postulated biologic mechanisms underlying the relationships; outlines areas of outstanding uncertainty; and the possible implications. The adverse effects of sedentary behavior associated with non-TV screens such as computers and handheld devices will not be the focus of this commentary; there is abundant literature available in this area and needs to be the focus of a separate commentary.
2. Binge TV viewing and CVD
Given the strong correlations between binge TV viewing and adverse levels of biomarkers of cardiometabolic risk, Dunstan and colleagues published the first report in 2010 on the associations of prolonged TV viewing time with all-cause, CVD, cancer, and non-CVD/noncancer mortality in Australian adults [Citation41]. In analysis adjusted for age, sex, waist circumference, and exercise, 1-hr increment in TV viewing time per day was associated with an increased risk of CV mortality hazard ratio (HR), 1.18 (95% confidence interval (CI), 1.03 to 1.35). However, further adjustment for other covariates attenuated the association to null. Comparing TV viewing time of ≥2 to <4 hrs/day with <2 hrs/day, there was no significant evidence of an association [Citation41]. In the same year 2010, Warren and colleagues reported their evaluation of the relationship between two sedentary behaviors (riding in car and/or TV viewing) and CVD mortality in men using the Aerobics Center Longitudinal Study [Citation46]. Multivariable-adjusted analysis showed no significant association between TV watching time and CVD mortality risk [Citation46]. Since the publication of these initial studies, several other observational cohort studies have reported on the association between binge TV viewing and the risk of CVD [Citation47,Citation48]. Given some inconsistency in the evidence, there have been efforts to pool the published data, resulting in a number of meta-analyses. Grøntved and colleagues conducted a meta-analysis of prospective cohort studies to evaluate the association between TV viewing and risk of type 2 diabetes, fatal or nonfatal CVD, and all-cause mortality [Citation39]. In pooled analysis of 4 studies, longer duration of TV viewing time (per 2 hrs/day increase) was associated with an increased risk of fatal or nonfatal CVD and the association was consistent with a linear dose-response relationship [Citation39]. Subsequent meta-analyses have been published on the relationship between TV viewing and CVD risk and they have all reported significant evidence of an association [Citation49,Citation50]. In the meta-analysis by Patterson and colleagues [Citation50], a nonlinear association was demonstrated between TV viewing time and CVD mortality, with a threshold of 3–4 hrs/day of TV viewing time, above which the risk of CVD mortality increased. In a recent analysis of the UK Biobank study to evaluate potential nonlinear relationships between TV viewing time and adverse health outcomes, Foster and colleagues demonstrated that the relationship between TV time and CVD mortality was curvilinear, with lowest risk observed for <2 hrs/day [Citation51]. Estimation of potential impact fractions showed that limiting TV time to 2 hrs/day might have prevented, or at least delayed, 8.0% of CVD deaths [Citation51]. In a harmonized meta-analysis of prospective cohort studies to examine if the associations between sedentary behaviors and mortality from CVD and cancer differ by different levels of physical activity, Ekelund and colleagues demonstrated a dose–response association between TV time and CVD mortality in the inactive group, with no increased risk for CVD mortality in the physically active group [Citation52]. Their conclusion was that physical activity modifies the association between TV viewing time and CVD mortality [Citation52]. Taking the overall evidence together, it can be suggested that binge TV viewing is associated with an increased risk of CVD.
3. Binge TV viewing and VTE
In our recent review of 14 prospective cohort studies, we showed that the risk of VTE was reduced by 13% comparing the most physically active with the least physically active groups [Citation29]. Several observational studies have also reported associations between sedentary behaviors and increased risk of VTE [Citation31,Citation32]. Data on the association between TV viewing and VTE risk is, however, limited and inconsistent. Only three primary studies have evaluated the association between TV viewing and VTE risk to date. The first-ever study to investigate the association between TV viewing and VTE risk was published in 2016 by Shirakawa and colleagues [Citation53]. Using the Japanese Collaborative Cohort Study (JACC) comprising 86,024 participants, the authors demonstrated that watching TV for ≥5 hrs/day or each additional 2-hr increment of TV viewing was associated with an increased risk of mortality from PE. In the Atherosclerosis Risk in Communities (ARIC) study comprising 15,158 individuals free of baseline VTE, Kubota and colleagues [Citation54] demonstrated a positive dose–response relationship between frequency of TV viewing and VTE incidence, in which ‘very often’ TV viewers had a 71% increased risk of VTE compared with ‘never or seldom’ TV viewers. In recently published findings of the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study comprising over 30,000 Black and White adults, heavy TV viewing (≥4 hrs/day) was not significantly associated with VTE risk [Citation55]. Given the plausibility that prolonged TV viewing may be associated with an increased VTE risk and the sparseness and inconsistency of the published data, our group aggregated the best available evidence using a meta-analysis approach. The pooled multivariable-adjusted relative risk (95% CI) of VTE comparing prolonged (≥4 hrs/day) versus never/seldom TV viewing (<2.5 hrs/day) groups was 1.35 (1.07 to 1.70) [Citation34]. Though adjustment for covariates was not consistent across all three studies, they all adjusted for age, sex, BMI, smoking, and physical activity [Citation34], suggesting that the increased risk of VTE due to TV viewing was independent of physical activity. It seems that higher levels of physical activity might not be able to neutralize the VTE risk due to prolonged TV viewing. One of the studies reported that achieving recommended physical activity levels did not eliminate the increased VTE risk associated with frequent TV viewing [Citation54] and another reported that physical activity did not modify the association between TV viewing and VTE risk [Citation55].
4. Postulated mechanisms
The underlying atherosclerotic process with thrombosis is the major cause of CVD events. Major risk factors for atherosclerosis include hypercholesterolemia, hypertension and cigarette smoking, which act in synergy with oxidative stress, endothelial dysfunction and enhanced inflammation in the arterial wall, the main processes that drive the pathogenesis of atherosclerosis [Citation56]. Mechanistic pathways implicated to be involved in the pathogenesis of VTE include alterations in blood flow and the coagulation cascade, abnormalities in fibrin clot properties, endothelial dysfunction, dyslipidemia and hypercoagulable states [Citation57–59]. An inflammatory hypothesis has also been commonly proposed, but the role of inflammation in VTE pathogenesis has been still under discussion [Citation60,Citation61]. Evidence for the importance of the inflammatory hypothesis is partly based on the protective effect of statins on VTE risk [Citation62–65], which has been attributed to the anti-inflammatory properties of statins [Citation66]. It has been reported that atherosclerotic CVD and VTE share common pathophysiological mechanisms such as coagulation, platelet activation and dyslipidemia [Citation16]. Whereas, some studies have reported that atherosclerotic CVD is an underlying condition and precedes the development of VTE [Citation67], some others report that VTE might rather precede atherosclerotic CVD [Citation68].
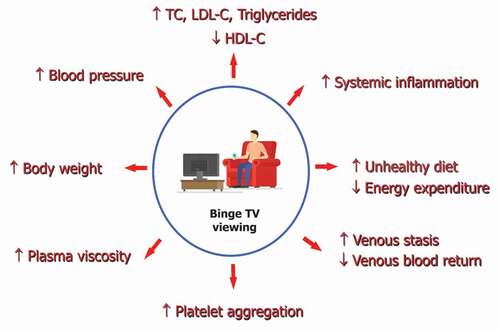
Binge TV viewing is a predominant sedentary behavior which involves high levels of immobilization or inactivity, which can drive the pathogenesis of venous and arterial thromboembolic disease via the following pathways (): (i) increase in levels of adverse levels of risk factors such as lipids, body weight, and blood pressure; (ii) increase in systemic inflammation; (iii) increase in plasma viscosity and platelet aggregation; and (iv) promotion of venous stasis through inhibiting venous blood return from the lower extremities during prolonged sitting [Citation69]. The time spent binge TV viewing possibly displaces exercise time, thus contributing to reductions in overall daily energy expenditure [Citation41], which has adverse effects on cardiometabolic risk markers. Furthermore, binge TV viewing is associated with unhealthy dietary intakes (e.g. sugar-sweetened beverages and fried foods) [Citation70,Citation71], which also increase the risk of thrombotic disease [Citation72].
Figure 1. Proposed mechanistic pathways underlying the association between binge TV viewing venous and arterial thromboembolic disease.
5. Conclusions
The overall body of evidence on the topic suggests that prolonged or binge TV viewing plays a potential role in increasing the risk of CVD in addition to other chronic diseases and mortality. The relationship between TV viewing and CVD risk has been described as curvilinear, with the lowest risk observed for TV viewing time <2 hrs/day and an increased risk beyond a threshold of 3–4 hrs/day of TV viewing time. Though it is biologically plausible that prolonged TV viewing may increase the risk of VTE, the current evidence is still limited, albeit based on pooled analysis of three studies [Citation34]. We encourage investigators of large population-based cohorts with access to data on TV viewing and VTE outcomes, to publish their data, whether the findings are null or significant. This will help shed more light on the relationship between binge TV viewing and VTE risk.
The overall evidence seems to suggest that high or recommended physical activity levels may attenuate but not eliminate the increased risk of venous and arterial thrombotic disease associated with binge TV viewing. Nevertheless, regular physical activity could still play a major role in preventing these adverse conditions. It is well documented that physical activity modifies the associations between sedentary behaviors and chronic disease outcomes such as CVD and cancer and all-cause mortality [Citation35,Citation52]. To echo Ekelund and colleagues [Citation52], these observations suggest that higher volumes of moderate and vigorous physical activity could reduce, or even eliminate the risk of passive lifestyle, especially for those who do a lot of sitting in their daily lives. Components of physical activity include the frequency, duration, and intensity (combined as the volume) and these play an important role in its beneficial effects. To derive the maximal benefits of physical activity, an appropriate intensity, frequency, and duration, is required. The total volume of physical activity is a more important determinant of health benefits than the intensity, duration, or frequency alone [Citation73]. Vigorous or high-intensity physical activity is associated with reduced risk of CVD and other chronic diseases, compared with lower or moderate intensity physical activity [Citation74–77]. Current physical activity guideline recommendations state that adults should engage in at least 150–300 minutes of moderate-intensity aerobic physical activity or 75–150 minutes of vigorous-intensity aerobic physical activity per week [Citation22]. On the other hand, current guidelines on sedentary behavior lack specific recommendations and only suggest that people should limit the amount of time spent being sedentary and replace sedentary time with physical activity of any intensity [Citation19]. The UK Chief Medical Officers’ Physical Activity Guidelines recommend breaking up long periods of sitting time with activity for just 1–2 minutes [Citation78]. There are no recommendations on the amount of time one should spend sitting viewing TV every day. However, countries such as Australia do recommend that children should limit TV and video games screen time to 1–2 hours a day [Citation79]. Findings from the large UK Biobank study seems to suggest that majority of health risks associated with binge TV viewing could be reduced if people limited their viewing time to two hours a day, or less [Citation51].
The importance of physical activity as a strategy for the prevention of venous and arterial thrombotic disease may just be one piece of the puzzle. Single risk factor modification is not enough to reduce the risk of disease; there should be more emphasis on modification of multiple risk factors such as physical inactivity, obesity, current smoking, and unhealthy diets [Citation12]. If atherosclerotic CVD and VTE share some common risk factors, then adoption of these healthy lifestyles might be an effective approach for preventing both conditions. Because atherosclerotic CVD and VTE share some common risk factors, it appears the most effective ways of preventing venous and arterial thrombotic disease are to engage in regular physical activity, consume a healthy diet, achieve healthy weights, and avoid smoking. Furthermore, avoid binge TV viewing if you can; but if you do binge watch TV, take frequent breaks in-between; binge TV viewing involves a lot of sitting time, hence sitting-reducing strategies such as standing, moving or stepping could minimize its adverse effects. Finally, do not snack on unhealthy diets and engage in higher volumes of moderate and vigorous physical activity if safe to do so.
Declaration of interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Additional information
Funding
References
- WHO. World Health Organization. Fact sheets. The top 10 causes of death. 2021. [cited 2020 Sep 10]. Available from: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death
- Barquera S, Pedroza-Tobias A, Medina C, et al. Global overview of the epidemiology of atherosclerotic cardiovascular disease. Arch Med Res. 2015 Jul;46(5):328–338.
- Hajar R. Risk factors for coronary artery disease: historical perspectives. Heart Views. 2017 Jul-Sep;18(3):109–114.
- Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American heart association’s strategic impact goal through 2020 and beyond. Circulation. 2010 Feb 2 121(4):586–613.
- Heit JA. The epidemiology of venous thromboembolism in the community. Arterioscler Thromb Vasc Biol. 2008 Mar;28(3):370–372.
- Cohen AT, Agnelli G, Anderson FA, et al. Venous thromboembolism (VTE) in Europe. The number of VTE events and associated morbidity and mortality. Thromb Haemost. 2007 Oct;98(4):756–764.
- Wt DI. Thrombosis: a major contributor to the global disease burden. J Thromb Haemost. 2014 Oct;12(10):1580–1590.
- Wendelboe AM, Raskob GE. Global burden of thrombosis: epidemiologic aspects. Circ Res. 2016 Apr 29; 118(9):1340–1347.
- Douketis JD, Gu CS, Schulman S, et al. The risk for fatal pulmonary embolism after discontinuing anticoagulant therapy for venous thromboembolism. Ann Intern Med. 2007 Dec 4 147(11):766–774.
- Heit JA. Epidemiology of venous thromboembolism. Nat Rev Cardiol. 2015 Aug;12(8):464–474.
- Cushman M. Epidemiology and risk factors for venous thrombosis. Semin Hematol. 2007 Apr;44(2):62–69.
- Folsom AR, Cushman M. Exploring opportunities for primary prevention of unprovoked venous thromboembolism: ready for prime time? J Am Heart Assoc. 2020 Dec;9(23):e019395.
- Ageno W, Becattini C, Brighton T, et al. Cardiovascular risk factors and venous thromboembolism: a meta-analysis. Circulation. 2008 Jan 1 117(1):93–102.
- Mahmoodi BK, Cushman M, Anne Naess I, et al. Association of traditional cardiovascular risk factors with venous thromboembolism: an individual participant data meta-analysis of prospective studies. Circulation. 2017 Jan 3 135(1):7–16.
- Gregson J, Kaptoge S, Bolton T, et al. Cardiovascular risk factors associated with venous thromboembolism. JAMA Cardiol. 2019 Feb 1 4(2):163–173.
- Ray JG. Dyslipidemia, statins, and venous thromboembolism: a potential risk factor and a potential treatment. Curr Opin Pulm Med. 2003 Sep;9(5):378–384.
- Ray JG. Why might statins prevent venous thromboembolism: what needs to be done to know more? Expert Opin Investig Drugs. 2002 Nov;11(11):1659–1668.
- Sanchis-Gomar F, Lavie CJ, and Marin J, et al. Exercise effects on cardiovascular disease: from basic aspects to clinical evidence. Cardiovasc Res. 2022 Jul;188(10):2253–2266.
- Bull FC, Al-Ansari SS, Biddle S, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020 Dec;54(24):1451–1462.
- Lear SA, Hu W, Rangarajan S, et al. The effect of physical activity on mortality and cardiovascular disease in 130 000 people from 17 high-income, middle-income, and low-income countries: the PURE study. Lancet. 2017 Dec 16 390(10113):2643–2654.
- Kyu HH, Bachman VF, Alexander LT, et al. Physical activity and risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events: systematic review and dose-response meta-analysis for the global burden of disease study 2013. BMJ. 2016 Aug 9;354:i3857.
- Piercy KL, Troiano RP, Ballard RM, et al. The physical activity guidelines for Americans. JAMA. 2018 Nov 20 320(19):2020–2028.
- Sedentary behaviour research N. Letter to the editor: standardized use of the terms “sedentary” and “sedentary behaviours.” Appl Physiol Nutr Metab. 2012 Jun;37(3):540–542.
- Tremblay MS, Aubert S, Barnes JD, et al. Sedentary Behavior Research Network (SBRN) - terminology consensus project process and outcome. Int J Behav Nutr Phys Act. 2017 Jun 10 14(1):75.
- Healy GN, Clark BK, Winkler EA, et al. Measurement of adults’ sedentary time in population-based studies. Am J Prev Med. 2011 Aug;41(2):216–227.
- Biswas A, Oh PI, Faulkner GE, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med. 2015 Jan 20 162(2):123–132.
- Lippi G, Henry BM, Sanchis-Gomar F. Physical inactivity and cardiovascular disease at the time of coronavirus disease 2019 (COVID-19). Eur J Prev Cardiol. 2020 Jun;27(9):906–908.
- Lavie CJ, Ozemek C, Carbone S, et al. Sedentary behavior, exercise, and cardiovascular health. Circ Res. 2019 Mar;124(5):799–815.
- Kunutsor SK, Makikallio TH, Seidu S, et al. Physical activity and risk of venous thromboembolism: systematic review and meta-analysis of prospective cohort studies. Eur J Epidemiol. 2020 May;35(5):431–442.
- van der Ploeg Hp, Hillsdon M, van der Ploeg HP. Is sedentary behaviour just physical inactivity by another name? Int J Behav Nutr Phys Act. 2017 Oct 23; 14(1):142.
- Kabrhel C, Varraso R, Goldhaber SZ, et al. Physical inactivity and idiopathic pulmonary embolism in women: prospective study. BMJ. 2011 Jul 4 343(jul04 1):d3867.
- Chandra D, Parisini E, Mozaffarian D. Meta-analysis: travel and risk for venous thromboembolism. Ann Intern Med. 2009 Aug 4; 151(3):180–190.
- Kunutsor SK, Laukkanen JA. TV viewing and venous thromboembolism: risk or red herring? J Thromb Haemost. 2021 Oct;19(10):2635–2637.
- Kunutsor SK, Dey RS, Laukkanen JA. Television viewing and venous thrombo-embolism: a systematic review and meta-analysis. Eur J Prev Cardiol. 2022 Jan 20 10.1093/eurjpc/zwab220
- Ekelund U, Steene-Johannessen J, Brown WJ, et al. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet. 2016 Sep 24 388(10051):1302–1310.
- Hamer M, Yates T, Demakakos P. Television viewing and risk of mortality: exploring the biological plausibility. Atherosclerosis. 2017 Aug;263:151–155.
- Clark BK, Sugiyama T, Healy GN, et al. Validity and reliability of measures of television viewing time and other non-occupational sedentary behaviour of adults: a review. Obes Rev. 2009 Jan;10(1):7–16.
- Minton HA M, Thevenet-Morrison K, Fernandez ID. Using television-viewing hours and total hours sitting as interchangeable measures of sedentary behavior. Am J Lifestyle Med. 2019 Jan-Feb;13(1):98–105.
- Grontved A, Hu FB. Television viewing and risk of type 2 diabetes, cardiovascular disease, and all-cause mortality: a meta-analysis. JAMA. 2011 Jun 15; 305(23):2448–2455.
- Keadle SK, Moore SC, Sampson JN, et al. Causes of death associated with prolonged TV viewing: NIH-AARP diet and health study. Am J Prev Med. 2015 Dec;49(6):811–821.
- Dunstan DW, Barr EL, Healy GN, et al. Television viewing time and mortality: the Australian diabetes, obesity and lifestyle study (AusDiab). Circulation. 2010 Jan 26 121(3):384–391.
- Rubenking B, and Baracken CC. Binge watching: implications and motivations of our changing viewing behaviors. New York, Bern, Berlin, Bruxelles, Oxford, Wien: Peter Lang Inc., International Academic Publishers; 2020.
- Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the United States, 2003-2004. Am J Epidemiol. 2008 Apr 1 167(7):875–881.
- Hansen BH, Kolle E, Dyrstad SM, et al. Accelerometer-determined physical activity in adults and older people. Med Sci Sports Exerc. 2012 Feb;44(2):266–272.
- Healy GN, Dunstan DW, Salmon J, et al. Television time and continuous metabolic risk in physically active adults. Med Sci Sports Exerc. 2008 Apr;40(4):639–645.
- Warren TY, Barry V, Hooker SP, et al. Sedentary behaviors increase risk of cardiovascular disease mortality in men. Med Sci Sports Exerc. 2010 May;42(5):879–885.
- Stamatakis E, Hamer M, Dunstan DW. Screen-based entertainment time, all-cause mortality, and cardiovascular events: population-based study with ongoing mortality and hospital events follow-up. J Am Coll Cardiol. 2011 Jan 18; 57(3):292–299.
- Wijndaele K, Brage S, Besson H, et al. Television viewing time independently predicts all-cause and cardiovascular mortality: the EPIC Norfolk study. Int J Epidemiol. 2011 Feb;40(1):150–159.
- Takagi H, Hari Y, Nakashima K, et al. Meta-analysis of the relation of television-viewing time and cardiovascular disease. Am J Cardiol. 2019 Dec 1;124(11):1674–1683.
- Patterson R, McNamara E, Tainio M, et al. Sedentary behaviour and risk of all-cause, cardiovascular and cancer mortality, and incident type 2 diabetes: a systematic review and dose response meta-analysis. Eur J Epidemiol. 2018 Sep;33(9):811–829.
- Foster HME, Ho FK, Sattar N, et al. Understanding how much TV is too much: a nonlinear analysis of the association between television viewing time and adverse health outcomes. Mayo Clin Proc. 2020 Nov;95(11):2429–2441.
- Ekelund U, Brown WJ, Steene-Johannessen J, et al. Do the associations of sedentary behaviour with cardiovascular disease mortality and cancer mortality differ by physical activity level? A systematic review and harmonised meta-analysis of data from 850 060 participants. Br J Sports Med. 2019 Jul;53(14):886–894.
- Shirakawa T, Iso H, Yamagishi K, et al. Watching television and risk of mortality from pulmonary embolism among Japanese men and women: the JACC study (Japan Collaborative Cohort). Circulation. 2016 Jul 26 134(4):355–357.
- Kubota Y, Cushman M, Zakai N, et al. TV viewing and incident venous thromboembolism: the atherosclerotic risk in communities study. J Thromb Thrombolysis. 2018 Apr;45(3):353–359.
- Munger JA, Koh I, Howard G, et al. Television viewing, physical activity and venous thromboembolism risk: the reasons for geographic and racial differences in stroke (REGARDS) study. J Thromb Haemost. 2021 Sep;19(9):2199–2205.
- Scott J. Pathophysiology and biochemistry of cardiovascular disease. Curr Opin Genet Dev. 2004 Jun;14(3):271–279.
- Kyrle PA, Eichinger S.Deep vein thrombosis.Lancet.2005Mar26;365:1163–1174. Apr 19465
- Ray JG, Rosendaal FR. The role of dyslipidemia and statins in venous thromboembolism. Curr Control Trials Cardiovasc Med. 2001;2(4):165–170.
- Undas A. Fibrin clot properties and their modulation in thrombotic disorders. Thromb Haemost. 2014 Jul 03; 112(1):32–42.
- Fox EA, Kahn SR. The relationship between inflammation and venous thrombosis. A systematic review of clinical studies. Thromb Haemost. 2005 Aug;94(2):362–365.
- Lippi G, Favaloro EJ, Montagnana M, et al. C-reactive protein and venous thromboembolism: causal or casual association? Clin Chem Lab Med. 2010 Dec;48(12):1693–1701.
- Kunutsor SK, Seidu S, Khunti K. Statins and primary prevention of venous thromboembolism: a systematic review and meta-analysis. Lancet Haematol. 2017 Jan 12; 4(2):e83–e93.
- Kunutsor SK, Seidu S, Khunti K. Statins and secondary prevention of venous thromboembolism: pooled analysis of published observational cohort studies. Eur Heart J. 2017 Mar 22; 38(20):1608–1612.
- Kunutsor SK, Whitehouse MR, Blom AW, et al. Statins and venous thromboembolism: do they represent a viable therapeutic agent? Expert Rev Cardiovasc Ther. 2017 Aug;15(8):629–637.
- Zaccardi F, Kunutsor SK, Seidu S, et al. Is the lower risk of venous thromboembolism with statins related to low-density-lipoprotein reduction? A network meta-analysis and meta-regression of randomised controlled trials. Atherosclerosis. 2018 Apr;271:223–231.
- Poredos P, Jezovnik MK. The role of inflammation in venous thromboembolism and the link between arterial and venous thrombosis. Int Angiol. 2007 Dec;26(4):306–311.
- Prandoni P, Bilora F, Marchiori A, et al. An association between atherosclerosis and venous thrombosis. N Engl J Med. 2003 Apr 10 348(15):1435–1441.
- Prandoni P, Ghirarduzzi A, Prins MH, et al. Venous thromboembolism and the risk of subsequent symptomatic atherosclerosis. J Thromb Haemost. 2006 Sep;4(9):1891–1896.
- Hamer M, Smith L, Stamatakis E. Prospective association of TV viewing with acute phase reactants and coagulation markers: english longitudinal study of ageing. Atherosclerosis. 2015 Apr;239(2):322–327.
- Wiecha JL, Peterson KE, Ludwig DS, et al. When children eat what they watch: impact of television viewing on dietary intake in youth. Arch Pediatr Adolesc Med. 2006 Apr;160(4):436–442.
- Vereecken CA, Todd J, Roberts C, et al. Television viewing behaviour and associations with food habits in different countries. Public Health Nutr. 2006 Apr;9(2):244–250.
- Kunutsor SK. Can a healthy dietary pattern alone prevent venous thromboembolism in the general population? Nutr Metab Cardiovasc Dis. 2021 Sep 22; 31(10):2839–2841.
- 2018 Physical Activity Guidelines Advisory Committee. 2018 Physical activity guidelines advisory committee scientific report. Washington, DC: U.S. Department of Health and Human Services, 2018.
- Lee IM, Paffenbarger RS Jr. Associations of light, moderate, and vigorous intensity physical activity with longevity. The Harvard Alumni Health Study. Am J Epidemiol. 2000 Feb 01;151(3):293–299.
- Chomistek AK, Cook NR, Flint AJ, et al. Vigorous-intensity leisure-time physical activity and risk of major chronic disease in men. Med Sci Sports Exerc. 2012 Oct;44(10):1898–1905.
- Williams PT. Reductions in incident coronary heart disease risk above guideline physical activity levels in men. Atherosclerosis. 2010 Apr;209(2):524–527.
- Williams PT. Reduced total and cause-specific mortality from walking and running in diabetes. Med Sci Sports Exerc. 2014;46(5):933–939.
- Physical activity guidelines: UK chief medical officers’ report 2020. Accessed on 2022 Jun 28 https://www.gov.uk/government/publications/physical-activity-guidelines-uk-chief-medical-officers-report
- Active Healthy Kids Australia (2014). Is sport enough? The 2014 active healthy kids Australia report card on physical activity for children and young people. Adelaide South Australia: Active Healthy Kids Australia. [cited 2022 Jun 28]. Available form: file:///C:/Users/sk14345/Downloads/Australia_Report_Card_2014-Long.pdf
