 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.The process of atherosclerosis is complex, involving multiple mechanisms. However, in recent decades, we have gained a better understanding of its natural course. Atherosclerotic plaque progresses through stages, and calcific plaque is considered the most stable form [Citation1]. Several pharmacological interventions have been evaluated for plaque quantification, including statins [Citation1], icosapent ethyl [Citation2], colchicine [Citation3] and direct oral anticoagulants (DOACS) [Citation4–6]. Multiple trials have shown transformation from non-calcified plaque to calcified plaque. Thus, calcification is thought to be the point at which the plaque is no longer at high risk. However, as highlighted in the classic work from Dr. Rumberger, calcium still represents approximately 20% of the total plaque burden, consisting of fibrous, low attenuation, and lipid laden plaque [Citation7]. Calcification can take on multiple morphologies in a vessel, including microcalcifications [Citation8], spotty calcification [Citation9], and large calcification (calcium deposit with an arc of >90° on optical coherence tomography (OCT)) [Citation10]. Each morphology has differing implications for prognosis and treatment, as shown in . Therefore, even though calcification represents a more stable form of plaque, it should not be underestimated or overlooked.
Figure 1. This figure is a schematic representation of the calcium morphologies, microcalcifications which is thought to be the beginning of the calcification cascade, spotty calcification, which is associated with high risk of events, large calcification which is thought to be more stable and dense calcification.
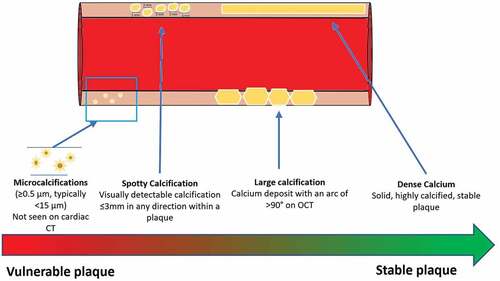
Several trials have evaluated different morphological distributions of calcium. Microcalcifications (≥0.5 μm, typically <15 μm) are thought to be beginning of the calcification cascade and cannot be seen in cardiac computed tomography (CCTA) [Citation11]. Spotty calcification is defined as a visually detectable calcification ≤3 mm in any direction within a plaque. In the ICONIC trial (Incident COroNary Syndromes Identified by Computed Tomography), the presence of spotty calcification resulted in a hazard ratio of 1.543 (1.169–2.037) for acute coronary syndromes [Citation12]. Spotty calcification was also demonstrated to be a high-risk finding when identified on IVUS and was associated with extensive and accelerated atherosclerotic progression [Citation13]. Another study using OCT showed an increased plaque vulnerability when spotty calcification was present [Citation14]. The presence of large calcification in one study tended to correlate inversely with plaque rupture, suggesting plaque stability [Citation10]. See . However, the reason why calcium provides greater risk in some morphologies and stability in others comes down to the plaque around the calcium and the local inflammation in the area where the calcium is seen. The creation of calcium deposits is an active metabolic process that involves complex mechanisms, such as TNF alpha, secretion of pro-inflammatory cytokines, and PKC, ERK1/2, JNK, signaling pathways [Citation15]. There has been much debate about the significance of calcium in coronary artery disease [Citation16,Citation17]. Perhaps, this is why it is so important to actually see it. For instance, calcium score testing (CAC), a test that only looks at calcium in the coronary arteries, has been proven to predict, stratify, and help to decide the treatment approach in patients [Citation18–20], regardless of its morphology. Due to its prognostic significance, the presence of calcium and plaque burden has been included in the new CAD-RADS 2.0, grading plaque burden from mild (P1) to extensive (P4), with one of the strategies to determine burden being CAC [Citation21]. The way calcium is measured is also important. One sub-study of the Global Assessment of Plaque reGression With a PCSK9 antibOdy as Measured by intraVascular Ultrasound (GLAGOV) measured plaque with IVUS and virtual histology but did not detect any differences in plaque composition with a signal of more calcified plaques in both groups, raising questions about the utility of this measurement approach [Citation22].
Table 1. This table describes the morphology of calcium and its significance.
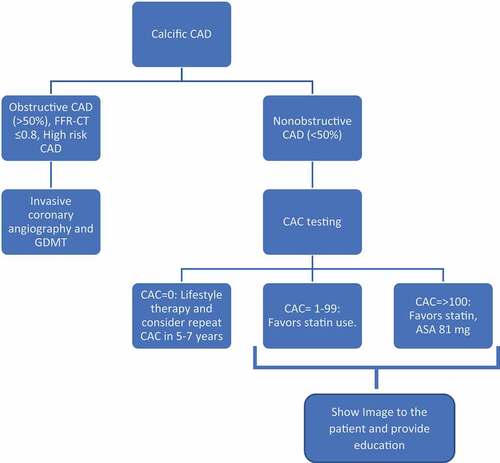
So how do we manage the presence of calcium in the coronary arteries? As of today, there is no proven therapy to transform calcified plaque into another type of plaque or to eliminate it. The Swedish Cardiopulmonary Bioimage study (SCAPIS) found that 40.2% of the population studied in their trial had CAC >0 [Citation23]. In patients with chest pain, intermediate risk, and anatomical significant obstruction (>50%) or physiological obstruction (fractional flow reserve with computed tomography (FFR-CT) <0.8), an invasive approach and guideline directed medical therapy would be indicated [Citation24] (). From an interventional point of view, approaches such as balloon angioplasty [Citation25], orbital and rotational atherectomy [Citation26,Citation27] and intravascular lithotripsy [Citation27] have been tested, with variable safety profiles and outcomes.
Figure 2. Suggested algorithm for calcific CAD. The presence of calcium in CAD can display different morphologies with different risk profiles, however, its only presence represents risk, thus, we suggest for nonobstructive CAD to go together with CAC score for better risk management.
One early IVUS trial demonstrated that patients with higher amounts of calcium were more resistant to plaque volume changes when traditional risk factors were intervened [Citation28]. A post-hoc analysis of eight studies that measured plaque using IVUS in patients on high dose, low dose, and no statins demonstrated that, independent of the plaque-regressive effect, statins promoted plaque transformation toward calcification [Citation29].
If the calcified plaque does not meet the definition of high-risk anatomy or physiological significance, noninvasive therapy has been shown to have better outcomes as shown in multiple trials [Citation30–33].
An observational study showed a significant reduction in cardiovascular events when CAC1 and statins were utilized [Citation34], demonstrating benefit when calcium is seen and treated. In an analysis of the Multi-ethnic study of atherosclerosis (MESA), aspirin was shown to have benefit when CAC
100 [Citation35]. One study showed that the presence of calcium plaque on CAC scans increased patient motivation, resulting in weight loss up to 33.3% and improved statin compliance [Citation36]. Another study with a similar methodology showed a three-fold increase in the likelihood of statin and aspirin usage [Citation37]. These interventions around the presence of calcium have been advocated in multiple international guidelines using CAC [Citation20].
In conclusion, the presence of calcium in the coronary arteries provides important clinical and prognostic information, with different calcium distributions carrying varying risk profiles. Treatment strategies around calcium have been shown to be effective in preventing cardiovascular outcomes, even increasing compliance and motivation for weight loss. Further research efforts should be carried out for each specific calcium morphology to develop tailored treatment strategies.
Abbreviations
CAD, Coronary Artery Disease; GDMT, Guideline Directed Medical Therapy.
Declaration of interest
MJ Budoff declares grant funding from General Electric, Amarin grant support, and speakers bureau. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Additional information
Funding
References
- Lee S-E, Chang H-J, Sung JM, et al. Effects of statins on coronary atherosclerotic plaques: the PARADIGM study. JACC Cardiovasc Imaging. 2018;11:1475–1484. InternetAvailable from https://www.sciencedirect.com/science/article/pii/S1936878X18303735
- Budoff MJ, Bhatt DL, Kinninger A, et al. Effect of icosapent ethyl on progression of coronary atherosclerosis in patients with elevated triglycerides on statin therapy: final results of the EVAPORATE trial. Eur Heart J. 2020;41:3925–3932. InternetAvailable from. DOI:10.1093/eurheartj/ehaa652.
- Vaidya K, Arnott C, Martínez GJ, et al. Colchicine therapy and plaque stabilization in patients with acute coronary syndrome: a CT coronary angiography study. JACC Cardiovasc Imaging. 2018;11:305–316. InternetAvailable from https://www.sciencedirect.com/science/article/pii/S1936878X1730791X
- Lee J, Nakanishi R, Li D, et al. Randomized trial of rivaroxaban versus warfarin in the evaluation of progression of coronary atherosclerosis. Am Heart J. 2018;206:127–130. InternetAvailable from https://www.sciencedirect.com/science/article/pii/S0002870318302497
- Win TT, Nakanishi R, Osawa K, et al. Apixaban versus warfarin in evaluation of progression of atherosclerotic and calcified plaques (prospective randomized trial). Am Heart J. 2019;212:129–133. InternetAvailable from https://www.sciencedirect.com/science/article/pii/S0002870319300493
- Aldana-Bitar J, Moore J, Manubolu VS, et al. Plaque progression differences between apixaban and rivaroxaban in patients with atrial fibrillation measured with cardiac computed tomography and plaque quantification. Am J Ther [Internet]. 9900; Available from: https://journals.lww.com/americantherapeutics/Fulltext/9900/Plaque_Progression_Differences_Between_Apixaban.88.aspx.
- Post WS, Budoff M, Kingsley L, et al. Associations between HIV infection and subclinical coronary atherosclerosis. Ann Intern Med. 2014;160:458–467.
- Vengrenyuk Y, Cardoso L, Weinbaum S. Micro-CT based analysis of a new paradigm for vulnerable plaque rupture: cellular microcalcifications in fibrous caps. Mol Cell Biomech. 2008;5:37–47.
- Ehara S, Kobayashi Y, Yoshiyama M, et al. Spotty calcification typifies the culprit plaque in patients with acute myocardial infarction: an intravascular ultrasound study. Circulation. 2004;110:3424–3429.
- Mizukoshi M, Kubo T, Takarada S, et al. Coronary superficial and spotty calcium deposits in culprit coronary lesions of acute coronary syndrome as determined by optical coherence tomography. Am J Cardiol. 2013;112:34–40. InternetAvailable from. DOI:10.1016/j.amjcard.2013.02.048.
- Otsuka F, Sakakura K, Yahagi K, et al. Has our understanding of calcification in human coronary atherosclerosis progressed? Arterioscler Thromb Vasc Biol. 2014;34:724–736. InternetAvailable from. DOI:10.1161/ATVBAHA.113.302642.
- Hyuk-Jae C, Lf Y, Sang-Eun L, et al. Coronary atherosclerotic precursors of acute coronary syndromes. J Am Coll Cardiol. 2018;71:2511–2522. InternetAvailable from. DOI:10.1016/j.jacc.2018.02.079.
- Kataoka Y, Wolski K, Uno K, et al. Spotty calcification as a marker of accelerated progression of coronary atherosclerosis: insights from serial intravascular ultrasound. J Am Coll Cardiol. 2012;59:1592–1597. InternetAvailable from https://www.sciencedirect.com/science/article/pii/S073510971200959X
- Kataoka Y, Puri R, Hammadah M, et al. Spotty calcification and plaque vulnerability in vivo: frequency-domain optical coherence tomography analysis. Cardiovasc Diagn Ther. 2014;4:460–469.
- Nadra I, Mason JC, Philippidis P, et al. Proinflammatory activation of macrophages by basic calcium phosphate crystals via protein kinase C and MAP kinase pathways. Circ Res. 2005;96:1248–1256. InternetAvailable from. DOI:10.1161/01.RES.0000171451.88616.c2.
- Shi X, Gao J, Lv Q, et al. Calcification in atherosclerotic plaque vulnerability: friend or foe? Front Physiol. 2020;11:56.
- Wang Y, Osborne MT, Tung B, et al. Imaging cardiovascular calcification. J Am Heart Assoc. 2018;7:e008564. InternetAvailable from. DOI:10.1161/JAHA.118.008564.
- Detrano R, Guerci AD, Carr JJ, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358:1336–1345.
- Budoff MJ, Young R, Burke G, et al. Ten-year association of coronary artery calcium with atherosclerotic cardiovascular disease (ASCVD) events: the multi-ethnic study of atherosclerosis (MESA). Eur Heart J. 2018;39:2401–2408. InternetAvailable from. DOI:10.1093/eurheartj/ehy217.
- Gi S, To G, Stephanie K, et al. Major global coronary artery calcium guidelines. JACC Cardiovasc Imaging. 2022;0. InternetAvailable from. doi:10.1016/j.jcmg.2022.06.018
- Cury RC, Blankstein R, Leipsic J, et al. CAD-RADS™ 2.0 – 2022 coronary artery disease – reporting and data system an expert consensus document of the society of cardiovascular computed tomography (SCCT), the American college of cardiology (ACC), the American College of Radiology (ACR) and the North America society of cardiovascular imaging (NASCI). J Cardiovasc Comput Tomogr. 2022;4: United States; 2022.
- Ns J, Rishi P, Todd A, et al. Effect of evolocumab on coronary plaque composition. J Am Coll Cardiol. 2018;72:2012–2021. InternetAvailable from. DOI:10.1016/j.jacc.2018.06.078.
- Bergström G, Persson M, Adiels M, et al. Prevalence of subclinical coronary artery atherosclerosis in the general population. Circulation. 2021;144:916–929. InternetAvailable from. DOI:10.1161/CIRCULATIONAHA.121.055340.
- Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American college of cardiology/American heart association joint committee on clinical practice guidelines. Circulation. 2021;144:e368–454. InternetAvailable from. DOI:10.1161/CIR.0000000000001029.
- Fitzgerald PJ, Ports TA, Yock PG. Contribution of localized calcium deposits to dissection after angioplasty. An observational study using intravascular ultrasound. Circulation. 1992;86:64–70.
- Yamamoto MH, Maehara A, Karimi Galougahi K, et al. Mechanisms of orbital versus rotational atherectomy plaque modification in severely calcified lesions assessed by optical coherence tomography. JACC: Cardiovasc Interv. 2017;10:2584–2586. InternetAvailable from https://www.sciencedirect.com/science/article/pii/S1936879817320137
- Abdel-Wahab M, Richardt G, Joachim Büttner H, et al. High-speed rotational atherectomy before paclitaxel-eluting stent implantation in complex calcified coronary lesions: the randomized ROTAXUS (rotational atherectomy prior to taxus stent treatment for complex native coronary artery disease) trial. JACC Cardiovasc Interv. 2013;6(1):10–19. DOI:10.1016/j.jcin.2012.07.017
- Nicholls SJ, Tuzcu EM, Wolski K, et al. Coronary artery calcification and changes in atheroma burden in response to established medical therapies. J Am Coll Cardiol. 2007;49:263–270. InternetAvailable from https://www.sciencedirect.com/science/article/pii/S0735109706026556
- Puri R, Nicholls SJ, Shao M, et al. Impact of statins on serial coronary calcification during atheroma progression and regression. J Am Coll Cardiol. 2015;65:1273–1282. InternetAvailable from https://www.sciencedirect.com/science/article/pii/S0735109715003010
- Boden WE, O’rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007;356:1503–1516. InternetAvailable from. DOI:10.1056/NEJMoa070829.
- De Bruyne B, Pijls NHJ, Kalesan B, et al. Fractional flow reserve–guided PCI versus medical therapy in stable coronary disease. N Engl J Med. 2012;367(11):991–1001. InternetAvailable from. https://doi.org/10.1056/NEJMoa1205361
- A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med. 2009; 360: 2503–2515. doi: 10.1056/NEJMoa0805796 InternetAvailable from.
- Maron DJ, Hochman JS, Reynolds HR, et al. Initial invasive or conservative strategy for stable coronary disease. N Engl J Med. 2020;382:1395–1407. InternetAvailable from. DOI:10.1056/NEJMoa1915922.
- Mitchell JD, Fergestrom N, Gage BF, et al. Impact of statins on cardiovascular outcomes following coronary artery calcium scoring. J Am Coll Cardiol. 2018;72:3233–3242.
- Cainzos-Achirica M, Miedema MD, McEvoy JW, et al. Coronary artery calcium for personalized allocation of aspirin in primary prevention of cardiovascular disease in 2019. Circulation. 2020;141:1541–1553. InternetAvailable from. DOI:10.1161/CIRCULATIONAHA.119.045010.
- Kalia NK, Cespedes L, Youssef G, et al. Motivational effects of coronary artery calcium scores on statin adherence and weight loss. Coron Artery Dis. 2015;26:225–230.
- Taylor AJ, Bindeman J, Feuerstein I, et al. Community-based provision of statin and aspirin after the detection of coronary artery calcium within a community-based screening cohort. J Am Coll Cardiol. 2008;51:1337–1341. InternetAvailable from https://www.sciencedirect.com/science/article/pii/S0735109708003240
