ABSTRACT
Background
Selling antibiotics without prescriptions is mostly illegal worldwide, including in Ghana, and promotes antimicrobial resistance. We evaluated the prevalence and practice of selling antibiotics without prescriptions among community pharmacies (CPs) and drug outlets, for the first time, in Ghana to quantify and characterize this issue to inform future interventions.
Research design and methods
Two scenarios utilizing the Simulated Client Methodology were enacted: an upper respiratory tract infection of viral origin (scenario one); and pediatric diarrhea (scenario two). CPs/Outlets were selected by stratified proportional random sampling from four metropolitan cities (~14% of the total Ghanaian population). Selling of antibiotics was assessed at three demand levels and its overall prevalence was estimated, then stratified by the study variables.
Results
Out of the 265 sampled CPs/outlets, the prevalence of selling antibiotic without prescription was 88.3% (n = 234/265), with variations not only across the four regions [92.5% (n = 123/133) in Kumasi, 87.5% (n = 14/16) in Cape Coast, 84.1% (n = 69/82) in Accra, and 82.4% (n = 28/34) in Tamale] but also across CPs [90% (n = 121/134)] and drug outlets [86% (n = 113/131)].
Conclusions
A very high prevalence/sub-optimal practice of selling antibiotics without prescriptions was found. This highlights the need to increase compliance with antibiotic dispensing legislation through evidence-based interventions including education of key stakeholders.
1. Introduction
Antimicrobial resistance (AMR) is a global public health issue that is estimated to have caused 1.27 million deaths globally and is associated with 4.95 million deaths in 2019 [Citation1]. Deaths due to AMR are projected to reach 10 million globally by 2050 if not addressed [Citation2]. The impact is greatest in Western Sub-Saharan Africa where AMR is currently estimated to cause 27.3 deaths per 100,000 [Citation1].
AMR is driven by the inappropriate utilization of antibiotics as well as poor sanitation and hygiene [Citation3]. In low and middle-income countries (LMICs), both the overuse and inappropriate use of antibiotics, particularly those classified under the World Health Organization (WHO) ‘Watch’ category (with greater potential for eliciting resistance), are of concern [Citation4]. In LMICs, antibiotics are predominantly utilized in ambulatory care and clinic settings, principally for respiratory tract infections, a large proportion of which may be self-limiting [Citation5,Citation6].
The purchase of antibiotics without a prescription is a common issue in many LMICs including in Ghana, despite being an illegal activity, with recent systematic reviews and meta-analysis reporting a pooled prevalence rate of 75.1% to 78% [Citation7,Citation8]. This practice of inappropriate antibiotic dispensing by pharmacies and unauthorized or unapproved outlets, compounded by lax enforcement of existing laws to curb this practice, has been identified as a major issue in Ghana [Citation9]. The reasons for this generally are complex and include factors such as lack of access to trained primary care practitioners (PCPs), inadequate education among dispensing facility staff regarding antibiotic use and AMR, as well as patient experience and expectations [Citation10]. Economic factors affecting patients [Citation11–13] are also important including lack of additional co-payment to consult a physician, and convenience without a potential loss of income when waiting to see a healthcare professional in busy clinics, especially in rural areas where pharmacies are often the principal healthcare provider [Citation10,Citation14]; however, Ghanaian specific reasons include shorter waiting times, belief in pharmacists’ expertise to manage minor ailments, employment status, and friendliness of personnel compared to hospital staff favored their use as first points of contact for health needs [Citation15]. However, perceptions that a community pharmacist’s main interest is in making profits rather than providing care exist among clients [Citation16].
Community pharmacies and over-the-counter medicine sellers (OTCMS) are major suppliers of antibiotics in Ghana with evidence suggesting pharmacies are more common in urban areas, while OTCMS dominate rural communities within Ghana [Citation16,Citation17]. There has been a demonstrated preference for OTCMS regarding medication needs over pharmacies in a rural Ghanaian setting [Citation17]. This is similar to findings from another study where over half of all respondents first visited an OTCMS for care of fever and were more likely to do so earlier than those who sought care from primary health centers, with a majority of them in the lowest socioeconomic quantiles [Citation18]. As such, they are a likely target for future strategies to enhance the appropriate dispensing of antibiotics. This is particularly pertinent in Ghana, where the high prevalence of AMR requires multimodal strategies to reduce current levels [Citation19,Citation20].
Pharmacy practice in Ghana is regulated by the Pharmacy Council of Ghana, which is responsible for the licensure of registered pharmacists as well as the licensing and oversight of any form of drug outlet including OTCMS [Citation21]. This includes regulation of various drug classes permitted to be sold from these different providers defined as prescription-only, pharmacy, and OTC medicines. Many antibiotics are prescription-only and require a medical practitioner’s prescription to be dispensed. Some antibiotics are classified as pharmacy medicines which can be dispensed based on the clinical judgment of a licensed pharmacist but some of these antibiotics are those indicated only for the treatment of sexually transmitted infections including ciprofloxacin, doxycycline, and erythromycin. The only antibacterials permitted as over-the-counter medications are ‘trimethoprim-sulfamethoxazole preparations’ with indications for its use currently not specified [Citation22]. Given current high rates of dispensing of antibiotics without a prescription in Ghana across locations and groups, with up to 56.2% of surveyed populations purchasing antibiotics without a prescription [Citation23–26], a number of interventions are needed to enhance appropriate dispensing behaviors among both community pharmacy staff and OTCMS in Ghana. There must be a balance with enforcing existing legislation which includes fines prohibiting illegal antibiotic dispensing against enhancing access and affordability to primary care facilities, including the prescribing of antibiotics where pertinent, especially among vulnerable personnel [Citation5,Citation6,Citation27]. This balance is especially crucial where there are considerable distances to primary care facilities versus drug outlets, especially in rural settings [Citation15,Citation28]. Consequently, the study aimed to quantify the current prevalence of dispensing antibiotics without a prescription from community pharmacies and OTCMS in Ghana. Subsequently, use the findings to start suggesting future policies, which can then be followed up in future research projects.
2. Methods
A prospective cross-sectional study was conducted using simulated client methodology (SCM) [Citation29,Citation30].
2.1. Study site
Four metropolitan cities in Ghana (covering 14% of the total Ghana population) were selected representing the Southern: Cape Coast (population 69,894) and Accra (population 1,848,614); Northern: Tamale (population 371,351); and Central: Kumasi (population 2,035,064) areas of the country [Citation31].
2.2. Study population and sample size
There are approximately 2,809 registered licensed community pharmacies and OTCMS located in the four metropolitan cities. An estimated total sample size of 339 community pharmacies and OTCMS (increased to 385 to account for a non-response of about 10% for outlets that may not be found or are inaccessible) was estimated using a 95% confidence level (Z-score = 1.96), 0.5 prevalence, and confidence interval of ± 5. A prevalence of 0.5 was selected as per the stats recommendations and guidelines because it provides the largest sample size [Citation32–34]. Stratified proportional random sampling was used to select the pharmacies and OTCMS. The stratum was defined as per the four metropolitan areas included in the study (Accra, Tamale, Kumasi, Accra). The number of registered pharmacies and OTCMS required to be sampled from each area were subsequently calculated according to their proportional weight; for example, within Accra, there are 1,121 community pharmacies and OTCMS which constitutes 40% of the total community pharmacies and OTCMS numbers in the four areas (n = 2,809); hence, 40% (n = 154) of the total 385 required sample was randomly sampled from Accra (Table S1) Similarly, the ratio of CP and OTCMS within each areas was calculated based on their proportional weight within the area; for instance, in Accra, CP accounts for 59% (n = 662) of the total CP and OTCMS (n = 1,121); hence, 59% (n = 91) of the required/estimated sample from Accra (n = 154) would be for CP (Table S1). The random number function in Microsoft Excel 2016 was used to select the target sample.
2.3. Simulated client methodology (SCM) and data collection
Simulated client visits were made in July 2021 and January and March 2022. The SCM utilizes the enacting of scenarios by trained individuals to test specific behaviors allowing for a more reliable representation of practices or interactions between healthcare providers and their customers or patients [Citation29]. Eight research assistants aged 24 to 32 years, and residing in the cities under study with non-pharmacy-related Bachelor’s degrees, were recruited as simulated clients. The training (75 minutes) included enacting the scenarios, reporting methods, and ethical and legal considerations for the study. Piloting was conducted at 18 community pharmacies and 14 OTCMS (those were not part of the randomly selected sample) across all four regions before the study began; very minor changes were made to the scenarios which was related to adding new excuses for the clients say to avoid paying for the medications offered during the visit. The findings from the piloting were not included in the study analysis. The clients’ performance during the training and piloting was fairly consistent.
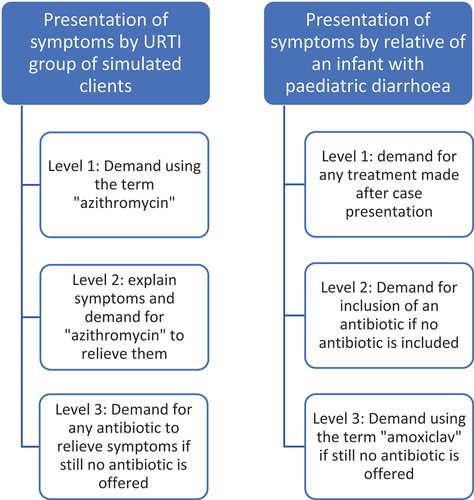
Two scenarios were developed to be delivered by the simulated clients to each of the selected pharmacies. Scenario 1 recounted symptoms of upper respiratory tract infections (URTI) of a sibling at home, with scenario 2 simulating pediatric diarrhea in an infant at home, both according to descriptions within the National Standard Treatment Guidelines (NSTGs) [Citation35]. Details of the choice for scenarios and the rationale are summarized in .
Table 1. Simulated scenarios and the rationale for the selection and client assignment.
The simulated clients were natives of one of the four target cities with fluency in the language(s) of the predominant ethnic groups in each of the four cities, e.g. Accra – Ga, Kumasi – Twi, Cape Coast – Fante and Tamale – Dagbani. Each of the Ghanaian investigators was fluent in at least one of the languages, and was a native of one of the respective towns. English is the official language of Ghana; consequently, this was the default language used when first approaching in the targeted outlets.
Three levels of demand for each presentation were utilized to observe at which level the attending staff member was willing to supply an antibiotic if at all based on previous studies [Citation37,Citation38] (). An adaptation of the SCM by Chang et al. (2017) [Citation39] was used in this study (). In line with a similar study in South Africa [Citation40], at the end of the encounter with the CP, the simulated client asked ‘are you a pharmacist’, because several cadres of staff are often present in a CP in Ghana (medicine counter assistants, pharmacy technicians, pharmacists), and pharmacists are the only cadre legally allowed to dispense certain classes of antibiotics based on their discretion. Therefore, this information could be used as a proxy measure of pharmacists’ knowledge/practice around appropriate antibiotic use because it is expected that pharmacists will be equipped with the required knowledge to identify any needs to offer antibiotics for these scenarios.
Data were recorded on a specifically designed data collection sheet by an accompanying investigator within five minutes of the visit via self-reporting by the investigator. Full details of the SCM methodology are provided in Supplementary File 1.
Antibiotics were categorized according to the WHO Access, Watch, and Reserve (AWaRe) classifications [Citation41]. This quality indicator tool is based on the ability of antibiotics to elicit resistance. ‘Access’ antibiotics are suggested initially due to their low resistance potential, while ‘Watch’ antibiotics are recommended for more severe conditions with a greater resistance potential. ‘Reserve’ antibiotics are generally reserved as last-line antibiotics for multidrug-resistant isolates, and should typically only be prescribed in hospital [Citation4,Citation42].
2.4. Data analysis
The primary study outcome was the prevalence of antibiotic dispensed from community pharmacies and OTCMS. Pharmacies and OTCMS that recommended an antibiotic were classified as exhibiting inappropriate practices for these two scenarios. Microsoft Excel 2016 was used for all descriptive analysis and R version 4.2.2 was used to perform Chi-square tests to compare the study outcomes across the metropolitan cities, type of premises, i.e. pharmacy or OTCMS, demand levels, and antibiotic supply according to simulated scenarios.
2.5. Ethics statement
Ethical approval and a consent waiver were obtained from the Cape Coast Teaching Hospital Research Ethical Review Committee (CCTHERC/EC/2021/009). Consent was waived with prior written approval from the Pharmacy Council of Ghana (PC-20/4/21) since the SCM phase is an observational and minimal-risk study to attain a true assessment of antibiotic supply in the everyday setting as used in other studies globally [Citation37,Citation38,Citation43]. Additionally, non-disclosure agreements were signed by all research assistants, and all data from visited premises were treated with strict confidence and anonymized.
3. Results
3.1. Total prevalence of antibiotic supply
A total of 265 out of 385 outlets (68.8%) were found and visited (133 from Kumasi, 82 from Accra, 34 from Tamale, and 16 from Cape Coast) which comprised 134 pharmacies and 131 OTCMS (). The prevalence of inappropriate supply of antibiotics without a prescription was 88% (234/265) overall, with 91% (122/134) in pharmacies and 86% (113/131) in OTCMS.
Table 2. Prevalence of antibiotics supplied without a prescription among drug outlets by type and case scenarios.
3.2. Prevalence of antibiotic supply for viral upper respiratory tract infection (scenario one)
Overall, antibiotics were offered in 83.9% (115/137) of URTI simulation visits. Azithromycin was the most commonly offered antibiotic (80%, 93/115) followed by amoxicillin-clavulanic acid (13%, 15/115) and amoxicillin (6.1%, 7/115) (). In all except two instances, non-azithromycin antibiotics were supplied on demand level three. A cough syrup was offered on 13 occasions of all simulated visits (13/137) and in 11 of these, this was together with an antibiotic. On the remaining two occasions, a cough syrup was dispensed alone as the condition was deemed not to require antibiotics. In 65.2% of instances where antibiotics were offered, the staff in both pharmacies and OTCMS did not ask the clients any questions (75/115). In cases resulting in antibiotic supply where at least one question was asked (40/115), the most commonly asked question across both outlet types pertained to whom the medication was meant for (55%, 22/40). On one occasion, the staff attending to the client asked questions but did not offer any antibiotics.
Table 4. Different types of antibiotics offered by pharmacies for both simulated conditions.
3.3. Otcms
In one instance, amoxicillin was offered at demand level one as azithromycin was unavailable. For other medications offered with antibiotics on nine occasions (17.3%, 9/52), a cough syrup was included on six occasions (6/52) with vitamin C being included on three occasions (3/52). Specific to this outlet type, questions were asked by outlet personnel on 16 visits, which all resulted in antibiotics being offered.
3.4. Pharmacy
Amoxicillin-clavulanic acid was co-offered with azithromycin at demand level one on one occasion. A cough syrup was offered seven times out of the total number of pharmacy visits (10%, 7/70). For five encounters where an antibiotic was offered, a cough syrup was offered alongside the antibiotic (5/63). However, out of the remaining seven occasions where no antibiotic was offered, a cough mixture was given as a standalone medication in two instances. The reason being that the condition did not require antibiotics. Simulated clients were asked questions on 25 occasions during pharmacy visits, with 24 of these instances resulting in antibiotics being offered.
3.5. Prevalence of antibiotic supply for paediatric diarrhoea (scenario two)
Antibiotic therapy was offered in 93% (119/128) of outlets visited with multiple antibiotics being offered on 20 occasions. The most common antibiotic for this scenario was metronidazole alone or plus furazolidone (85.7%, 102/119) (). Amoxicillin (6.7%, 8/119) and amoxicillin-clavulanic acid (5.0%, 6/119) were the next most frequently offered antibiotics. Ciprofloxacin was the antibiotic of choice by one OTCMS, and a pharmacy offered ciprofloxacin on two occasions, both on demand level one (1.7%, 2/119). Dispensing of multiple antibiotics occurred on 20 occasions (16.8%, 20/119), usually amoxicillin with metronidazole with or without furazolidone (35%, 7/20). Oral rehydration salt (ORS) was the most frequent non-antibiotic choice by staff in both pharmacies and OTCMS (28.9%, 37/128). In 119 visits where antibiotics were offered, ORS was co-offered in 35 of these while being offered alone in only two out of nine visits where no antibiotic was given. For this scenario, the most common questions were regarding additional symptoms of the fictitious child needing treatment (10.9%, 14/128). Only one outlet in this instance asked for a prescription and refused to include antibiotics as part of the offered medications when no prescription was offered.
3.6. OTCMS
Aside from metronidazole with or without furazolidone (73.4%, 47/64), amoxicillin was the second most prevalent antibiotic offered (23.4%, 15/64) for all visits (). For medications offered together with antibiotics, oral rehydration salt (ORS) formed the majority (19.7%, 12/61). On the three occasions where no antibiotic was offered (4.7%, 3/64), ORS, paracetamol, and ‘mist kaolin’ were the alternative medications offered to the simulated clients. The reason for the non-offer among these three OTCMS was the non-availability of antibiotics in the outlet. Questions were asked on five occasions (7.8%, 5/64), out of which four ended up in an antibiotic being dispensed. The most common question asked by the staff was for the simulated client to verify the age of the fictitious child suffering from diarrhea (60%, 3/5).
Table 5. Different types of antibiotics offered by OTC medicine sellers for both simulated conditions.
3.7. Pharmacy
The most offered antibiotic was similar to OTCMS with metronidazole with or without furazolidone offered on 87.5% of occasions (56/64) followed by amoxicillin-clavulanic acid (7.8%, 5/64) (). ORS (40.7%, 24/59) was commonly offered with zinc tablets (16.9%, 10/59) when antibiotics were given. Out of five occasions with no antibiotic given, ORS was offered once (20%, 1/5). Questions were asked by staff on 21 visits, and 13 of these centered around any additional symptoms the child was exhibiting such as a fever, blood in the stool, vomiting, stomach pain, and if the child was active (61.9%, 13/21). Only one attending staff asked for a prescription and later refused to offer any antibiotic when no prescription was provided.
3.8. Prevalence of antibiotic supply by metropolis and outlets
The prevalence of antibiotics being supplied without a prescription was still high when analyzing practices between the outlet types by case scenarios and outlet types by metropolis. The highest prevalence of supply of antibiotics without a prescription among OTCMS was seen in Kumasi (90.5%, 67/74) with Cape Coast having all pharmacies supplying antibiotics without a prescription (100%, 6/6). However, a statistically significant difference in antibiotic supply practices was seen among pharmacies in the various metropolitan cities (P = 0.03) ().
Significant differences were also observed among the demand levels utilized in the study for URTI case scenario one (P= <0.001). A majority of the community pharmacies (78.6%; n = 55/70) supplied azithromycin at demand level one compared to only 43.3% (n = 29/67) among OTCMS (). In this scenario, azithromycin was demanded at the first level, before any other antibiotic was demanded at the second level, and finally asking for any other medication for the third level. No significant differences (P = 0.40) were, however, observed for scenario two (). Demand level one had the highest dispensing prevalence for both scenarios in pharmacies and OTCMS ().
Table 3. Antibiotic supply at various demand levels for both case scenarios among OTCMS and pharmacies.
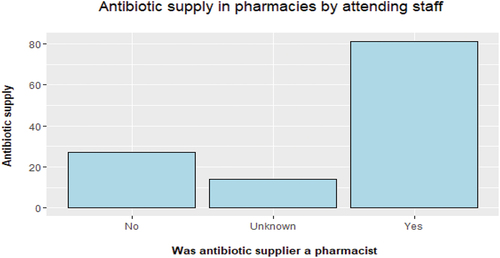
A total of 92 (92/134, 68.7%) visits involved pharmacists as a supplier out of all 134 pharmacies. Out of this, 122 visits resulted in antibiotic supply with 81 (81/92, 88%) pharmacists offering antibiotics to clients. This left only 12% (11/92) of all pharmacists refusing to recommend antibiotics to the client after all three levels of demand were exhausted. Additionally, all pharmacy staff who were unwilling to reveal whether they were pharmacists in the ‘unknown’ category (n = 14) offered antibiotics and 27 staff who admitted to not being pharmacists also offered antibiotics ().
Eight unique antibiotic types comprising 256 antibiotics were offered across all visited outlets with two antibiotics being offered on 21 occasions (9%, 21/234). Of note, OTCMS offered a wider variety of different antibiotics (7/8) than pharmacies (5/8) with flucloxacillin, amoxicillin, and trimethoprim-sulfamethoxazole being unique to OTCMS and tinidazole being unique to pharmacies. ‘Access’ antibiotics were most prevalent among the types of antibiotics offered in both OTCMS (5/7) and pharmacies (3/6), with tinidazole being unclassified ().
The reasons for antibiotic refusal mainly differed when considering outlet types rather than case scenarios. Among pharmacies, five outlets (41.7%, 5/12) stated that a prescription was needed before an antibiotic could be offered, with four (33.3%, 4/12) stating that the simulated condition for URTI did not require antibiotics. Encouragingly 91.7% (11/12) of the attendants refusing antibiotics for both case scenarios in community pharmacies were pharmacists. With regard to the OTCMS, the non-offer of antibiotics among all 16 outlets was either due to antibiotics not being stocked or the attendant reporting to have run out of antibiotics, rather than being a decision not to supply the antibiotics. Advice on how to take the offered medication was given on only 9.8% (23/234) occasions by the attendants in both pharmacies and OTCMS. On all of these occasions, an antibiotic was included among the offered medicines. In circumstances where no advice on the duration, timing, or how the antibiotic should be taken was given, clients did not ask the attendants for this. This approach would be interesting going forward to determine pharmacy and OTCMS personnel knowledge as this is a key problem area.
4. Discussion
A higher prevalence of dispensing antibiotic without a prescription was observed among both community pharmacies and OTCMS for two common, self-limiting clinical scenarios, where there is clear consensus and guidance on the need for non-antibiotic management, which is a real concern. In line with the findings of our study, a systematic review on self-medication in Africa found community pharmacies to be the most common source of antibiotics where the major reasons for request also coincided with the clinical scenarios used in this study, i.e. upper respiratory and gastrointestinal symptoms [Citation44]. Then highlight that substantially higher rates than seen in other studies in Ghana [Citation23–26]. This may be due to the methodology involving simulated patients as opposed to questionnaires and other approaches [Citation45]. In addition, we are aware that this study took place during the recent COVID-19 pandemic where published studies have shown greater use of antibiotics to treat patients with suspected or proven COVID-19 despite limited evidence of bacterial infections or co-infections in LMICs [Citation46–48]. However, we cannot say anything with certainty at this stage, and will be following up the reasons for the high rates seen in future studies.
However, compared to pooled overall estimates from other Sub-Saharan countries, the prevalence of antibiotic supply was higher (88%) than found by Belachew et al. of 69% (CI: 58–80) [Citation49]. However, for studies utilizing simulated clients, our findings were similar compared to Eritrea (88%), Ethiopia (86–87%), and Kenya (87%), whereas it was substantially higher compared to one study conducted in a rural and suburban community (36.1% dispensing) in Ghana which utilized exit interviews [Citation26,Citation30].
For pediatric diarrhea, the ‘Access’ antibiotic metronidazole was the most recommended, and it was offered in many visits at the first level of demand without client pressure. The prevalence of supply for this scenario was high in our study (95.3%) compared to other countries which ranged from 9% to 89% [Citation49].
Azithromycin was frequently offered for the upper respiratory tract simulation despite this being a WHO ‘Watch’ category antibiotic [Citation41]. This may be because azithromycin was promulgated along with hydroxychloroquine for possible treatment of patients with COVID-19 in the early stages of the pandemic in view of its in-vitro impact and effectiveness in other viral infections [Citation50,Citation51] and it may be that pharmacists or their assistants might have thought the ARI could be COVID-19 related. However, the use of azithromycin did not translate into improved outcomes in practice [Citation50,Citation52]; consequently not typically recommended. Whilst amoxicillin was found to be the antibiotic of choice in other studies, this difference in our study can be explained by the use of demand levels where azithromycin was expressly requested by the simulated client at the first level as well as possible concerns with the presence of COVID-19. In one study, antibiotics purchased from OTCMS for a drug bag study found macrolides unavailable in these outlets unlike in pharmacies where 50% stocked them. It is important to note that this was conducted in a rural constituency outside of our sampled metropoles from 24 February to 19 March 2020 which was prior to any COVID-19 restrictions in Ghana and may explain the disparity observed [Citation17]. This finding was buttressed by Ahiabu et al., with macrolides dispensed more frequently in pharmacies using direct observation [Citation53]. The mere availability of this antibiotic in OTCMS and its supply across sampled outlets is particularly concerning and needs to be addressed going forward. The prevalence of 77.6% in this study was within the pooled range found in other studies (84% [CI: 74–94]) [Citation49]. Conversely, in a study conducted in South Africa using SCM, no antibiotics were presented for URTIs even after explicit demand at the last level of request by clients. This could facilitate a reasonable comparison with the methodology used in this study [Citation40]. This also reflects generally greater recognition and enforcements of the regulations in South Africa; however, this is not always the case [Citation40].
There is currently no clear consensus across different levels of stakeholders on the necessary measures needed to be taken to effectively curb the inappropriate dispensing of antibiotics without a prescription, especially among OTCMS in Ghana. Fines and other punitive measures exist to discourage the illegal sale of antibiotics but enforcement is weak and stricter enforcement may help to curb this practice with regular monitoring. However, care is needed as the potential for limited fines among community pharmacists in Vietnam had little impact on the dispensing of antibiotics without a prescription [Citation54]. Senior officials of the OTCMS association of Ghana harbored the view that adequate training would enable them to be able to dispense antibiotics adequately to promote increased access as they have a strong presence in rural areas [Citation55]. This view was opposed at the regional level among the Ghana Health Service, Pharmacy Council, and National AMR Platform members. Among the reasons cited, the issue of profit-seeking practices which may overshadow any training was a key issue, with this concern also shared by OTCMS leadership at the regional level [Citation55]. Having said this, we have seen in other African countries, and other LMICs, that the presence of trained pharmacists, along with guidelines and increasing recognition of current regulations, negates or reduces the dispensing of antibiotics without a prescription for essentially viral infections such as URTIs [Citation56–60]
Multiple stakeholder groups need to be targeted using various interventions which include improved curricula on AMR given current concerns [Citation23], continued education post-qualification using evidence-based guidelines, and limiting the selection of antibiotics available in community drug outlets based on the ‘Access’ list with ‘Watch’ and ‘Reserve’ antibiotics only available at defined levels of the healthcare system in Ghana. The use of technology to monitor dispensing [Citation61] as well as utilizing point-of-care testing and other approaches as their costs and feasibility become manageable [Citation62–64] should further help to enhance appropriate dispensing of antibiotics. Patient education is also important generally surrounding antibiotics and AMR to reduce requests for antibiotics especially with community pharmacists a trusted healthcare provider across LMICs [Citation60,Citation65].
Few studies on non-prescription supply of antibiotics reported who the dispenser on duty was. From our findings, we observed that even among pharmacies where pharmacists were suppliers there was still a high level of dispensing of antibiotics without a prescription, which may indicate that even among this cadre of trained professionals, other factors may influence their practice including client pressure [Citation14,Citation66,Citation67]. A qualitative study among PCPs developed a conceptual model of several identities adopted in their dealing with patients when dispensing antibiotics specifically for acute respiratory tract infections (ARTIs). In one of these identities termed ‘the benevolent self,’ pharmacists admitted dispensing antibiotics to patients based on their desire to help them [Citation66]. This attempted benevolence, with the additional burden of patient pressure, could be an important factor in the over-the-counter antibiotic sales in LMICs including Ghana. Tackling this will require behavior change strategies targeting addressing key influences in the dispensing process from both the patient and dispenser perspectives.
4.1. Strengths and limitations
We believe this is the first study in Ghana in recent years following the start of the COVID-19 pandemic to determine the extent/nature of the dispensing of antibiotics without a prescription across four metropolitan cities in the southern and northern parts of Ghana (covering 14% of the total Ghana population) not only among community pharmacies but also among OTCMS. Furthermore, we utilized two scenarios, an URTI and a pediatric diarrhea, both of which are mostly of virus origin, accounting for the majority of community consultations and hence dispensing antibiotics without prescriptions [Citation5,Citation44]. Moreover, for the first time in Ghana, we included three demand levels to assess the likelihood/willingness of CP/OTCMS to dispense antibiotics instantly/first choice in response to the client’s presenting symptoms or to dispense antibiotics in response to client’s pressure/demand, which provides useful insights on the dispensing practice of antibiotics without prescriptions. We believed this was important as we have seen inappropriate increasing use of antibiotics to treat patients with COVID-19 across sectors in Ghana despite limited evidence of bacterial infections or co-infections in response to patients’ demand/pressure. Such activities will drive up AMR in Ghana, which is already a concern, unless addressed.
However, there are some limitations that need to be acknowledged. Firstly, we only undertook the study in some parts of Ghana; hence, generalizability of our findings to other parts of Ghana should be with caution. In addition, it is possible that we have underestimated the prevalence of advice given on how to take the medication because medication advice may have been provided to a patient (the simulated clients in our study) after payment for the medicines which our simulated clients did not do. Each outlet was visited only once by each simulated client. Thus, dispensing practices may be limited to the individual staff on duty on that day rather than the general practice of staff within that outlet, which may bias the findings; however, this is standard way of conducting SCM [Citation29,Citation30]; hence, the limitation is something inherited to this methodology. Since the scenarios were enacted by eight individuals (clients), it could be argued that there might have been variations in how they presented the scenarios; however, all the eight clients undertook comprehensive training and their performance was fairly consistent during the piloting; therefore, we do not believe this has impacted our study findings substantially. Despite these limitations, we believe our findings are robust and suggest real concerns for key stakeholder groups in Ghana as the authorities try and reduce AMR as part of the Ghana’s NAP.
5. Conclusions
A high level of inappropriate antibiotic dispensing without a prescription for two well-defined self-limiting conditions not requiring antibiotic therapy is a real concern needing urgent action. This included the offer of ‘Watch’ antibiotics for URTIs at the level one where no additional pressure for an antibiotic was enacted in both pharmacies and OTCMS. It is evident in the literature that evidenced-based strategies with a focus on behavior change is the best approach/strategy to curb this practice in line with the current legislation while maintaining access to antibiotics in populations who need them. Our research is ongoing in Ghana to explore key reasons underpinning this issue (using qualitative interviews), and the combined findings will be used to guide all key stakeholder groups in Ghana going forward as the authorities strive to reduce AMR as part of the NAP. Furthermore, there is a need to improve the consultation practice of all dispensers (for example through education and training) to ask key relevant questions when dispensing antibiotics including any information regarding allergies as well as to instruct patients on dosing schedules and the importance of completing the course.
Declaration of interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Author contribution statement
Study conception and design: all authors; data collection and management: JA (Joseph Acolatse), GA (George Akafity), RI (Robert Incoom), AR (Audu Rauf); data analysis and interpretation: AK (Amanj Kurdi), JA, AS (Andrew Seaton), JS (Jacqueline Sneddon), EC (Elaine Cameron), MW (Margaret Watson), MWat (Marta Wanat), BG (Brian Godman); manuscript writing and drafting: JA, EN (Eric Kofi Ngyedu); manuscript reviewing and revising as well as providing constructive criticism and final approval: all authors. All authors have substantially contributed to the conception and design of the article and interpreting the relevant literature, and have been involved in writing the article or revised it for intellectual content.
Supplemental Material
Download Zip (58.7 KB)Acknowledgments
The authors wish to thank the simulated clients, Pharm Theresa Acolatse, and Pharm Joseph Gyewu for their roles in the study. We also wish to thank the management of the Cape Coast Teaching Hospital for their support in implementing this project and the Pharmacy Council of Ghana for providing the necessary support to conduct this study. This work has not been previously presented as an abstract at a conference or similar forum.
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/14787210.2023.2283037
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Murray CJ, Ikuta KS, Sharara F, et al. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. 2022;399(10325):629–655. doi: 10.1016/S0140-6736(21)02724-0
- O’Neill J Review on antimicrobial resistance: tackling drug-resistant infections globally: final report and recommendations. Review on antimicrobial resistance: tackling drug-resistant infections globally: final report and recommendations. 2016.
- Pulingam T, Parumasivam T, Gazzali AM, et al. Antimicrobial resistance: Prevalence, economic burden, mechanisms of resistance and strategies to overcome. Eur J Pharm Sci. 2022;170:106103. doi: 10.1016/j.ejps.2021.106103
- Sulis G, Sayood S, Katukoori S, et al. Exposure to World Health Organization’s AWaRe antibiotics and isolation of multidrug resistant bacteria: a systematic review and meta-analysis. Clin Microbiol Infect. 2022;28(9):1193–1202. doi: 10.1016/j.cmi.2022.03.014
- Godman B, Haque M, McKimm J, et al. Ongoing strategies to improve the management of upper respiratory tract infections and reduce inappropriate antibiotic use particularly among lower and middle-income countries: findings and implications for the future. Curr Med Res Opin. 2020;36(2):301–327. doi: 10.1080/03007995.2019.1700947
- Godman B, Egwuenu A, Haque M, et al. Strategies to improve antimicrobial utilization with a special focus on developing countries. Life. 2021;11(6):528. doi: 10.3390/life11060528
- Li J, Zhou P, Wang J, et al. Worldwide dispensing of non-prescription antibiotics in community pharmacies and associated factors: a mixed-methods systematic review. Lancet Infect Dis. 2023;23(9):e361–e370. doi: 10.1016/S1473-3099(23)00130-5
- Torres NF, Chibi B, Kuupiel D, et al. The use of non-prescribed antibiotics; prevalence estimates in low-and-middle-income countries. A systematic review and meta-analysis. Arch Public Health. 2021;79(1):1–15. doi: 10.1186/s13690-020-00517-9
- World Health Organization. Ghana country level report: Resource mobilisation for antimicrobial resistance(AMR). 2018.
- Torres N, Chibi B, Middleton L, et al. Evidence of factors influencing self-medication with antibiotics in low and middle-income countries: a systematic scoping review. Public Health. 2019;168:92–101. doi: 10.1016/j.puhe.2018.11.018
- Afari-Asiedu S, Kinsman J, Boamah-Kaali E, et al. To sell or not to sell; the differences between regulatory and community demands regarding access to antibiotics in rural Ghana. J of Pharm Policy and Pract. 2018;11(1):1–10. doi: 10.1186/s40545-018-0158-6
- Janssen J, Afari-Asiedu S, Monnier A, et al. Exploring the economic impact of inappropriate antibiotic use: the case of upper respiratory tract infections in Ghana. Antimicrob Resist Infect Control. 2022;11(1):53. doi: 10.1186/s13756-022-01096-w
- Abbey M, Chinbuah MA, Gyapong M, et al. Community perceptions and practices of treatment seeking for childhood pneumonia: a mixed methods study in a rural district, Ghana. BMC Public Health. 2016;16(1):1–10. doi: 10.1186/s12889-016-3513-z
- Belachew SA, Hall L, Erku DA, et al. No prescription? No problem: drivers of non-prescribed sale of antibiotics among community drug retail outlets in low and middle income countries: a systematic review of qualitative studies. BMC Public Health. 2021;21(1):1056. doi: 10.1186/s12889-021-11163-3
- Okai GA, Abekah-Nkrumah G, Asuming PO. Determinants of community pharmacy utilization in Ghana. J Pharm Health Serv Res. 2020;11(2):159–165. doi: 10.1111/jphs.12338
- Okai GA, Abekah-Nkrumah G, Asuming PO. Perceptions and trends in the use of community pharmacies in Ghana. J of Pharm Policy and Pract. 2019;12(1):1–9. doi: 10.1186/s40545-019-0186-x
- Bonnah J, Chandler CI. Availability and use of antibiotics in the dormaa municipal district of the bono region in Ghana. Report For Fleming Fund Fellowship Programme. 2020. doi: 10.17037/PUBS.04658918
- Ansah EK, Gyapong M, Narh-Bana S, et al. Factors influencing choice of care-seeking for acute fever comparing private chemical shops with health centres and hospitals in Ghana: a study using case–control methodology. Malar J. 2016;15(1):1–9. doi: 10.1186/s12936-016-1351-1
- Godman B, Egwuenu A, Wesangula E, et al. Tackling antimicrobial resistance across sub-Saharan Africa: Current challenges and implications for the future. Expert Opin Drug Saf. 2022;21(8):1089–1111. doi: 10.1080/14740338.2022.2106368
- Ghana Ministry of Health, Ministry of food agriculture MoES, technology innovation, ministry of fisheries aquaculture development. Ghana National Action Plan for Antimicrobial Use and Resistance. 2017–2021.
- Ghana Parliament Council. Health Professions Regulatory Bodies Act. 2013. Act 857 2017
- Food and DruRgs Board. Reviewed drug classification list. 2017.
- Owusu-Ofori AK, Darko E, Danquah CA, et al. Self-medication and antimicrobial resistance: a survey of students studying healthcare programmes at a tertiary institution in Ghana. Front Public Health. 2021;9:706290. doi: 10.3389/fpubh.2021.706290
- Kretchy J-P, Adase SK, Gyansa-Lutterodt M. The prevalence and risks of antibiotic self-medication in residents of a rural community in Accra, Ghana. Scientific African. 2021;14:e01006. doi: 10.1016/j.sciaf.2021.e01006
- Mensah BN, Agyemang IB, Afriyie DK, et al. Self-medication practice in Akuse, a rural setting in Ghana. Niger Postgrad Med J. 2019;26(3):189–194. doi: 10.4103/npmj.npmj_87_19
- Do NT, Vu HT, Nguyen CT, et al. Community-based antibiotic access and use in six low-income and middle-income countries: a mixed-method approach. Lancet Glob Health. 2021;9(5):e610–e619. doi: 10.1016/S2214-109X(21)00024-3
- Jacobs TG, Robertson J, van den Ham HA, et al. Assessing the impact of law enforcement to reduce over-the-counter (OTC) sales of antibiotics in low-and middle-income countries; a systematic literature review. BMC Health Serv Res. 2019;19(1):1–15. doi: 10.1186/s12913-019-4359-8
- Afari-Asiedu S, Oppong FB, Tostmann A, et al. Determinants of inappropriate antibiotics use in rural central Ghana using a mixed methods approach. Front Public Health. 2020;8:90. doi: 10.3389/fpubh.2020.00090
- Watson MC, Norris P, Granas A. A systematic review of the use of simulated patients and pharmacy practice research. Int J Pharm Pract. 2006;14(2):83–93. doi: 10.1211/ijpp.14.2.0002
- Ahmad T, Khan SA, Mallhi TH, et al. Assessing antibiotic dispensing without prescription through simulated client methodology in developing countries: a comprehensive literature review from 2009 to 2021. J Public Health. 2023;1–23. doi: 10.1007/s10389-023-02032-x
- Ghana Statistical Service. 2010 population and housing census: summary report of final results. Ghana Statistical Service Accra. 2012.
- Daniel WW, Cross CL. Biostatistics: a foundation for analysis in the health sciences. New York: Wiley; 2018.
- Lwanga SK, Lemeshow S, Organization WH. Sample size determination in health studies: a practical manual. World Health Org. 1991.
- Raosoft. Sample size calculator. Available from: http://www.raosoft.com/samplesize.html
- Ministry of Health Ghana. Standard treatment guidelines: seventh ghana national drugs programme. 2017.
- Ministry of Health Ghana. Standard treatment guidelines for novel coronavirus infection COVID-19 guidelines for Ghana. 2020.
- Saleem Z, Hassali MA, Godman B, et al. Sale of WHO AWaRe groups antibiotics without a prescription in Pakistan: a simulated client study. J Of Pharm Policy And Pract. 2020;13(1):1–8. doi: 10.1186/s40545-020-00233-3
- Alrasheedy AA, Alsalloum MA, Almuqbil FA, et al. The impact of law enforcement on dispensing antibiotics without prescription: a multi-methods study from Saudi Arabia. Exp Rev Anti-Infective Ther. 2020;18(1):87–97. doi: 10.1080/14787210.2020.1705156
- Chang J, Ye D, Lv B, et al. Sale of antibiotics without a prescription at community pharmacies in urban China: a multicentre cross-sectional survey. J Antimicrob Chemother. 2017;72(4):1235–1242. doi: 10.1093/jac/dkw519
- Mokwele RN, Schellack N, Bronkhorst E, et al. Using mystery shoppers to determine practices pertaining to antibiotic dispensing without a prescription among community pharmacies in South Africa—A pilot survey. JAC Antimicrob Resist. 2022;4(1):dlab196. doi: 10.1093/jacamr/dlab196
- World Health Organization. WHO Access, Watch, Reserve (AWaRe) classification of antibiotics for evaluation and monitoring of use, 2021. WHO access, watch, reserve (AWaRe) classification of antibiotics for evaluation and monitoring of use, 2021. 2021.
- Sharland M, Zanichelli V, Ombajo LA, et al. The WHO essential medicines list AWaRe book: from a list to a quality improvement system. Clin Microbiol Infect. 2022;28(12):1533–1535. doi: 10.1016/j.cmi.2022.08.009
- Chang J, Xu S, Zhu S, et al. Assessment of non-prescription antibiotic dispensing at community pharmacies in China with simulated clients: a mixed cross-sectional and longitudinal study. Lancet Infect Dis. 2019;19(12):1345–1354. doi: 10.1016/S1473-3099(19)30324-X
- Yeika EV, Ingelbeen B, Kemah BL, et al. Comparative assessment of the prevalence, practices and factors associated with self‐medication with antibiotics in Africa. Trop Med Int Health. 2021;26(8):862–881. doi: 10.1111/tmi.13600
- Batista A, Rodrigues DA, Figueiras A, et al. Antibiotic dispensation without a prescription worldwide: a systematic review. Antibiotics. 2020;9(11):786. doi: 10.3390/antibiotics9110786
- Bednarčuk N, Golić Jelić A, Stoisavljević Šatara S, et al. Antibiotic Utilization during COVID-19: Are We Over-Prescribing? Antibiotics. 2023;12(2):308. doi: 10.3390/antibiotics12020308
- Alshaikh FS, Godman B, Sindi ON, et al. Prevalence of bacterial coinfection and patterns of antibiotics prescribing in patients with COVID-19: a systematic review and meta-analysis. PLoS One. 2022;17(8):e0272375. doi: 10.1371/journal.pone.0272375
- Sefah IA, Essah DO, Haque M, et al. Covid-19, healthcare and self-medication issues in resource limited-settings: findings and implications based on experiences in Ghana. Adv Hum Biol. 2021;11(3):224–233. doi: 10.4103/aihb.aihb_82_21
- Belachew SA, Hall L, Selvey LA. Non-prescription dispensing of antibiotic agents among community drug retail outlets in Sub-Saharan African countries: a systematic review and meta-analysis. Antimicrob Resist Infect Control. 2021;10(1):1–15. doi: 10.1186/s13756-020-00880-w
- Echeverría-Esnal D, Martin-Ontiyuelo C, Navarrete-Rouco ME, et al. Azithromycin in the treatment of COVID-19: a review. Exp Rev Anti-Infective Ther. 2021;19(2):147–163. doi: 10.1080/14787210.2020.1813024
- Khezri MR, Zolbanin NM, Ghasemnejad-Berenji M, et al. Azithromycin: immunomodulatory and antiviral properties for SARS-CoV-2 infection. Eur J Pharmacol. 2021;905:174191. doi: 10.1016/j.ejphar.2021.174191
- Group CH, Popp M, Stegemann M, et al. Antibiotics for the treatment of COVID‐19. Cochrane Database Syst Rev. 1996;2022(7):CD015025.
- Ahiabu M-A, Magnussen P, Bygbjerg IC, et al. Treatment practices of households and antibiotic dispensing in medicine outlets in developing countries: the case of Ghana. Res Social Administrative Pharm. 2018;14(12):1180–1188. doi: 10.1016/j.sapharm.2018.01.013
- Nguyen TTP, Do TX, Nguyen HA, et al. A national survey of dispensing practice and customer knowledge on antibiotic use in Vietnam and the implications. Antibiotics. 2022;11(8):1091. doi: 10.3390/antibiotics11081091
- Afari-Asiedu S, Hulscher M, Abdulai MA, et al. Stakeholders’ perspectives on training over the counter medicine sellers and community-based Health planning and services facilities to dispense antibiotics in Ghana. J of Pharm Policy and Pract. 2021;14(1):1–14. doi: 10.1186/s40545-021-00349-0
- Mukokinya MMA, Opanga S, Oluka M, et al. Dispensing of antimicrobials in Kenya: a cross-sectional pilot study and its implications. J Res Pharm Pract. 2018;7(2):77. doi: 10.4103/jrpp.JRPP_17_88
- Opanga SA, Rizvi N, Wamaitha A, et al. Availability of medicines in community pharmacy to manage patients with COVID-19 in Kenya; pilot study and implications. Sch Acad J Pharm. 2021;10(3):36–43. doi: 10.36347/sajp.2021.v10i03.001
- Kamati M, Godman B, Kibuule D. Prevalence of self-medication for acute respiratory infections in young children in Namibia: findings and implications. J Res Pharm Pract. 2019;8(4):220. doi: 10.4103/jrpp.JRPP_19_121
- Kibuule D, Nambahu L, Sefah I, et al. Activities in Namibia to limit the prevalence and mortality from COVID-19 including community pharmacy activities and the implications. Sch Acad J Pharm. 2021;10(5):82–92. doi: 10.36347/sajp.2021.v10i05.001
- Marković-Peković V, Grubiša N, Burger J, et al. Initiatives to reduce nonprescription sales and dispensing of antibiotics: findings and implications. J Res Pharm Pract. 2017;6(2):120. doi: 10.4103/jrpp.JRPP_17_12
- Kalungia A, Godman B. Implications of non-prescription antibiotic sales in China. The Lancet infectious diseases. Lancet Infect Dis. 2019;19(12):1272–1273. doi: 10.1016/S1473-3099(19)30408-6
- Vicentini C, Vola L, Previti C, et al. Antimicrobial stewardship strategies including point-of-care testing (POCT) for pediatric patients with upper-respiratory-tract infections in primary care: a systematic review of economic evaluations. Antibiotics. 2022;11(8):1139. doi: 10.3390/antibiotics11081139
- van Hecke O, Butler C, Mendelson M, et al. Introducing new point-of-care tests for common infections in publicly funded clinics in South Africa: a qualitative study with primary care clinicians. BMJ Open. 2019;9(11):e029260. doi: 10.1136/bmjopen-2019-029260
- Do NT, Ta NT, Tran NT, et al. Point-of-care C-reactive protein testing to reduce inappropriate use of antibiotics for non-severe acute respiratory infections in Vietnamese primary health care: a randomised controlled trial. Lancet Glob Health. 2016;4(9):e633–e641. doi: 10.1016/S2214-109X(16)30142-5
- Chowdhury M, Stewart Williams J, Wertheim H, et al. Rural community perceptions of antibiotic access and understanding of antimicrobial resistance: qualitative evidence from the Health and demographic surveillance system site in matlab. Bangladesh Global Health Action. 2019;12(sup1):1824383. doi: 10.1080/16549716.2020.1824383
- Germeni E, Frost J, Garside R, et al. Antibiotic prescribing for acute respiratory tract infections in primary care: an updated and expanded meta-ethnography. Br J Gen Pract. 2018;68(674):e633–e645. doi: 10.3399/bjgp18X697889
- Dixon J, MacPherson EE, Nayiga S, et al. Antibiotic stories: a mixed-methods, multi-country analysis of household antibiotic use in Malawi, Uganda and Zimbabwe. BMJ Global Health. 2021;6(11):e006920. doi: 10.1136/bmjgh-2021-006920