Abstract
Aims: We assessed care in cancer patients with cachexia across leading health systems (LHSs). Patients & methods: Qualitative interviews and quantitative surveys were conducted with LHSs executives and frontline health care personnel, representing 46 total respondents and 42 unique LHSs and including oncology service line leaders, supportive care services, dietitians and surgical oncologists. Results: Cachexia was not considered a top priority, and formal diagnoses were rare. Participants highlighted the importance of addressing barriers to increase clinical trial enrollment and support frontline health care personnel and patients in early detection of cachexia. Conclusion: Cachexia prioritization needs to be elevated across LHSs executives to obtain capital and strategic imperatives to advance related care.
Despite its widespread prevalence and its impact on the care of patients with cancer, cachexia is underdiagnosed and is often untreated or undertreated.
We report findings from an assessment of cachexia care in cancer patients with cachexia across leading health systems (LHSs) through an analysis of LHSs C-Suite executives, enterprise-wide service line leaders, and frontline healthcare personnel (HCP) perspectives. We also assessed perspectives from oncology service line leaders, supportive care services, dietitians and surgical oncologists.
We conducted qualitative interviews and administered a quantitative survey to LHSs executives and frontline HCP, representing 46 total respondents and 42 unique LHSs.
Cachexia was not considered a top priority, and formal diagnoses were rare. Participants highlighted the importance of addressing barriers to increase clinical trials enrollment, supporting frontline HCP and patients in early detection of cachexia.
The prioritization of cachexia needs to be elevated across C-Suite executives. To elevate cachexia as a priority among C-Suite executives, it is crucial that service line leaders demonstrate the value of investing in cachexia care and resources to LHSs.
1. Introduction
Cachexia is a multifactorial syndrome with an ongoing loss of skeletal muscle mass (with or without loss of fat mass) that cannot be fully reversed by conventional nutritional support [Citation1]. The international consensus panel defines cachexia as >5% weight loss in the preceding 6 months or >2% weight loss with one of the following: body mass index of <20 kg/m2 or loss of skeletal muscle mass (sarcopenia) based on imaging analysis. However, there is currently no uniform global consensus of the definition of cachexia [Citation2]. Therefore, for the purposes of this research, the term ‘unintentional weight loss’ was often used interchangeably with ‘cachexia’ depending on the preferred terminology or level of understanding of research participants.
Cachexia is observed in up to 80% of patients with advanced cancer and is often untreated or undertreated [Citation3]. In addition, the incidence of cachexia is projected to rise in years to come [Citation4]. As treatments improve, patients with cancer live longer, and as the population ages the incidence of cancer cachexia can be expected to rise. Despite the widespread prevalence and its impact on the care of patients with cancer, cachexia is largely underdiagnosed. This is due to a lack of awareness, other conditions taking precedence, and treatment focusing on the primary diagnosis of cancer with chemotherapy, which can also lead to the development of cachexia [Citation3,Citation5,Citation6]. Cancer patients with cachexia are likely to have reduced efficacy and tolerability following chemotherapy and surgery, as well as reduced quality of life, resulting in worse prognosis [Citation5,Citation7–10].
At present, evidence-based guidelines do not fully recommend any specific pharmacological agent for the treatment of cachexia. The US FDA recommends dietary counseling for patients and caregivers, and the EMA recommends nutritional therapeutic options, if required, and immediate symptomatic relief during the last weeks of life [Citation11,Citation12].
Clinical trials have shown that anamorelin, a ghrelin-receptor agonist, as a potential treatment for cachexia in patients with cancer resulted in an increase in body weight, lean body mass and fat mass, as well as insulin-like growth factor 1 and insulin-like growth factor-binding protein 3 [Citation13]. However, the FDA and EMA guidelines have not approved any pharmacological intervention for the treatment of cancer cachexia [Citation11,Citation12]. Clinical management should therefore involve a proactive approach of a multimodal, multidisciplinary team [Citation14].
Understanding the prioritization and care management of cachexia in patients with cancer in leading health systems (LHSs) is critical to optimizing patient outcomes and the success of the oncology service line and overall health system. For the purposes of this manuscript, LHSs are defined as the largest 150 LHSs in the USA, which can include over 50 hospitals, as well as physician group(s) and other facilities, such as skilled nursing facilities. These LHSs have over US$2 billion in annual total operating revenue (TOR) validated by the 2019 health system financial statements.
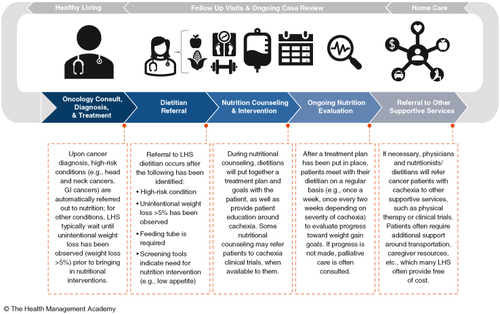
The current cachexia care pathway at most LHSs included in this study comprises an initial oncology consult, diagnosis, and treatment. Subsequently, patients attend follow-up visits and ongoing case review, including dietitian referrals, nutrition counseling and intervention, as well as ongoing nutrition evaluation. Thereafter, patients receive home care, including referral to other supportive services and ongoing reviews ().
Figure 1. Current state of cachexia care pathways across leading health systems: framework for lifestyle changes, case reviews and home care.
GI: Gastrointestinal; LHS: Leading health system.
Reprinted with permission from The LHSs Approach to Cachexia Care in Cancer Patients. ©The Health Management Academy March 2022, with permission from The Health Management Academy.
In this manuscript, we report the findings from an assessment of the current and future state of care in cancer patients with cachexia across LHSs, including approaches to risk identification and prevention, care delivery workflow and care pathway decision-making across the continuum of care. In addition, we highlight the challenges and priorities in cachexia care through an in-depth analysis of LHSs C-Suite executives (e.g., chief medical officers and chief nursing officers), enterprise-wide service line leaders, and frontline healthcare personnel (HCP) perspectives.
2. Patients & methods
The Health Management Academy (‘The Academy’) conducted qualitative interviews and administered a quantitative survey to LHSs executives and frontline HCP (dietitians, advanced practice providers, physicians) regarding their perspectives on the current and future landscape of unintentional weight loss in patients with cancer (e.g., cachexia). The Academy’s membership comprises >1600 executive and C-Suite leaders from the largest LHSs in the USA, and they were approached because of their expertise with the strategy and/or program for cancer cachexia care. Executives and frontline HCP were included to represent system and frontline perspectives of cancer cachexia. No compensation was provided to participants.
The respondents represented those who chose to participate or who were referred by an executive member. For example, the majority of the frontline HCP that participated in this study were referred by C-suite executives at their LHSs who were members of The Academy and were asked to participate in this study.
The 41 quantitative survey responses and 15 qualitative insight conversations represent 46 total respondents and 42 unique LHSs. From July to December 2021, The Academy conducted qualitative interviews and a quantitative survey (via email) with LHSs executives and frontline practitioners/HCP regarding the current and future landscape of unintentional weight loss in cancer patients with cachexia. This was a high-level assessment of LHSs C-Suite executives, service line leaders and frontline HCP perspectives across 46 health system leaders and frontline HCP; however, the individual n-counts for each of the survey questions are included in the text throughout. The assessment included patient and HCP-level perspectives, and the findings from this assessment included insights to inform considerations within the LHSs. All data were blinded to maintain confidentiality of participating LHSs. Note that the survey questions were intended to capture C-Suite executives’ perspectives on the state of cachexia care at their health systems. The data do not represent the exact numbers of clinicians familiar with clinical standards for cachexia but, rather, the extent to which C-Suite executives believed physicians at the health system were familiar with those standards, based on their experience with physicians and the standard of care delivered at the health system. The sample size remains consistent throughout the manuscript, in which quantitative survey responses (n = 41) and qualitative perspectives (n = 15) were aggregated to represent 42 unique health systems.
Surveys were distributed by email and included multiple choice questions (and used methodology) that have been previously described [Citation15]. Questions from each section were asked as relevant. The level of prioritization, maturity and proactivity of cachexia care across the LHSs surveyed was defined and assessed by The Academy based on responses to survey and interview questions in four categories: prioritization and strategic decision-making for cachexia care across LHSs; early identification and care management; resource allocation and wraparound services; and future outlook on closing the gap on cachexia care.
Quantitative survey data and percentages were calculated for each question, and the total number of responses to each question represented the denominator. If a respondent skipped a question, then the denominator for a question would be reduced by 1 [Citation15]. In April 2022 The Academy hosted a multistakeholder Advisory Council roundtable including oncology service line leaders, directors of supportive care services, dietitians and physician surgical oncologists. The aims of the roundtable meeting were to discuss the key themes in caring for cancer patients with cachexia and to further explore leader and frontline HCP perspectives on addressing barriers to increased clinical trials enrollment. The roundtable participants also explored leader and frontline HCP perspectives to encourage early detection/diagnosis, educating patients to support early detection and treatment compliance.
3. Results
3.1. Survey respondents
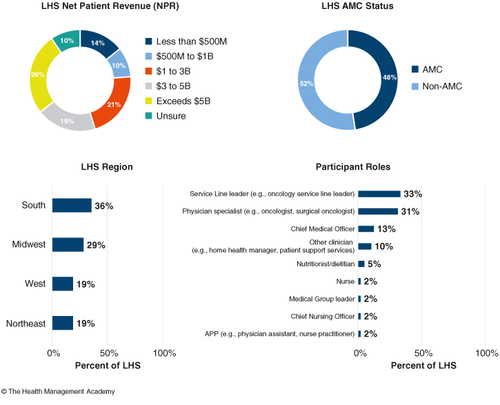
Overall, 41 quantitative survey responses and 15 qualitative insight conversations represented a total of 46 executive leaders and frontline HCP and 42 unique LHSs, which vary across a range of regions, sizes and academic medical center status. Respondent roles included chief medical officers, chief nursing officers, medical group chief executive officers/presidents, heads of oncology service lines/departments, heads of population health service lines/departments, heads of palliative care service lines/departments, physician specialists (e.g., oncologists, cardiologists, primary care physicians), advanced practice providers (e.g., nurse practitioners, physician assistants), dietitians/nutritionists and nurses.
The profiles of participating LHSs, executives and frontline HCP are shown in . All data and findings reflected the survey responses and qualitative insights from LHSs executives and frontline HCP. The sample size was consistent throughout the report, in which quantitative survey responses (n = 41) and qualitative perspectives (n = 15) were aggregated to represent 42 unique LHSs.
Figure 2. The profiles of participating health systems, executives, and frontline healthcare personnel from survey responses and qualitative insights from executives at leading health systems.
Most of the findings regarding the role of dietitians/nutritionists were obtained from the interview process. All data and findings are reflective of survey responses and qualitative insights from executives at LHSs. The sample size remained consistent throughout the assessment, in which quantitative survey responses (n = 41) and qualitative perspectives (n = 15) were aggregated to represent 42 unique health systems.
AMC: Academic medical center; APP: Advanced practice provider; HCP: Healthcare personnel; LHS: Leading health system; NPR: Net patient revenue.
Reprinted with permission from The LHSs Approach to Cachexia Care in Cancer Patients. ©The Health Management Academy March 2022, with permission from The Health Management Academy.
3.2. Survey responses: current state of cachexia care
In light of the current state of cachexia care at LHSs, it is critical to understand the factors that influence C-Suite executives and frontline HCP perspectives. These perspectives may influence the prioritization of cachexia care across LHSs in the next 5 years and approaches to standardization. The top three factors among LHSs C-Suite executives and frontline HCP in their evaluation of the current state of cachexia care delivery within the oncology service line are outlined below.
3.2.1. Prioritization & decision-making for cachexia care across LHSs
Owing to a lack of awareness and education among executives and frontline HCP, cachexia was not considered a top priority, and formal diagnoses were rare. LHSs executives and HCP surveyed indicated that cancer cachexia was most likely to be considered a top priority for oncology and palliative care service line leaders but not for C-Suite executives (). LHSs executives and HCP (n = 41) indicated that oncology service line leaders (56%) and palliative care leaders (41%) were most likely to consider cachexia as a top priority, whereas chief medical officers (12%) and chief nursing officers (5%) were identified as least likely to do so. Moreover, 12% of LHSs executives and HCP surveyed did not believe any of their health system leaders would consider cachexia a top priority.
Figure 3. Familiarization, prioritization, and decision-making for cachexia care across leading health systems, n = 41.
CMO: Chief medical officer; CNO: Chief nursing officer; LHS: Leading health system.
Reprinted with permission from The LHSs Approach to Cachexia Care in Cancer Patients. ©The Health Management Academy March 2022, with permission from The Health Management Academy.
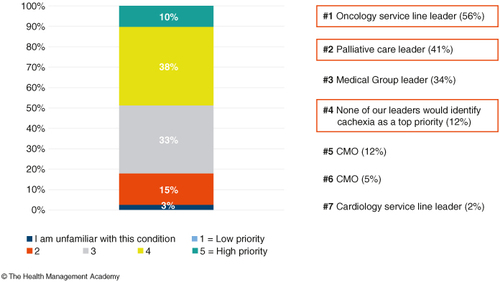
The low prioritization of cachexia by C-Suite executives may have been due to barriers to treatment, and 22% of respondents indicated this was due to cost and coverage. Physician awareness and education was considered a top barrier by 22% of respondents, and 20% of respondents indicated that patient awareness and education on cachexia was a top barrier to diagnosis and treatment of cachexia. Although cachexia was one of the top three common conditions among patients with cancer, it was often viewed as a side effect of cancer treatments and not a condition that requires tailored intervention.
Overall, 82% of LHSs executives and HCP reported that risk identification and care management of cachexia in patients with cancer was at least somewhat of a top priority for their oncology service line or health system. However, qualitative interviews with LHSs executives and HCP suggested that addressing cachexia in patients with cancer required investment in standardized, streamlined risk identification and collaborative care management across disciplines and departments.
3.2.2. Early identification & care management
HCP from LHSs with a proactive strategy for early identification and care management of cachexia reported that interventions were often triggered for patients prior to weight loss (e.g., in patients with high-risk conditions and treatment needs). The level of proactivity was defined and assessed by The Academy based on survey and interview questions. HCP from LHSs with a reactive approach to early identification and care management of cachexia indicated that interventions were often initiated after the referral to nutritional services was already triggered for the patient. Few LHSs reported having a proactive approach to the early identification and management of cachexia, often leading to late-stage intervention. At some proactive LHSs, patients identified as high risk for cachexia were targeted using a combination of screening protocols and clinical guidelines implemented across the health system. Within the surgical oncology subspecialty, it is often a priority to assess and treat unintentional weight loss in pre- and post-operative care plans for oncology patients. This optimizes patient health prior to surgery, facilitates healing and mitigates risks associated with surgical procedures.
Formal diagnosis of cachexia is rare across the majority of LHSs surveyed, leading to lack of or delayed intervention until substantial weight loss has already occurred (). Only 17% of LHSs executives and HCP reported diagnosis and treatment of cachexia prior to weight loss. The survey also showed 11% of LHSs executives and HCP did not typically diagnose patients with cachexia, and many stated this was due to low awareness of the condition among patients and physicians, as well as minimal reimbursement. Cost and coverage (22%), physician awareness and education (22%), patient awareness and education (20%), access to nutrition counseling and support (15%), access to effective diagnosis and therapies (12%), and low efficacy of current treatments (12%) were the key barriers to patients seeking diagnosis and treatment as reported by LHSs executives and HCP.
Figure 4. Barriers to diagnosis of cachexia and triggers for intervention across leading health systems, n = 18.
LHS: Leading health system.
Reprinted with permission from The LHSs Approach to Cachexia Care in Cancer Patients. ©The Health Management Academy March 2022, with permission from The Health Management Academy.
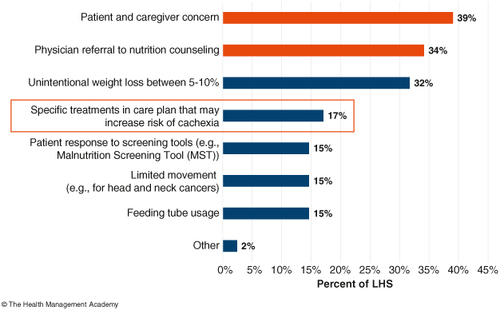
Initiatives to support early risk identification and care management for cachexia were limited to nutritional counseling and education for patients among the LHSs surveyed (). With intervention typically occurring after referral for nutritional counseling, dietitians were often responsible for providing cachexia care, which is often too little and too late. Of the LHSs executives and HCP surveyed (n = 18), 28% stated nutritionists and dietitians, as opposed to physicians, were the primary practitioners on the care team responsible for making treatment recommendations for cancer patients with cachexia. In qualitative interviews, dietitians indicated they were likely to prioritize cachexia and called for increased prioritization from frontline HCP and executives within their systems.
Figure 5. Initiatives across leading health systems to support risk identification and care management. n = 41.
EMR: Electronic medical record; LHS: Leading health system.
Reprinted with permission from The LHSs Approach to Cachexia Care in Cancer Patients. ©The Health Management Academy March 2022, with permission from The Health Management Academy.
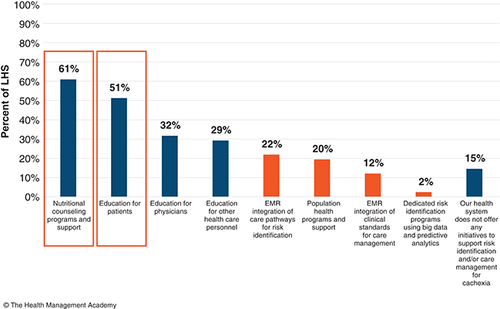
Across LHSs, the most common initiatives used to support risk identification and care management for cancer patients with cachexia were limited to nutritional counseling programs and support (61%) and education for patients (51%). Moreover, less than one-third of LHSs executives and HCP indicated their LHSs pursued cachexia initiatives that required substantial investment and strategic prioritization, including electronic medical record (EMR) integration of care pathways for risk identification (22%), EMR integration of clinical standards for care management (12%), and dedicated risk identification programs using big data and predictive analytics (2%). In addition, 15% of LHSs executives and HCP indicated their health system did not offer any initiatives to support risk identification and/or care management for cachexia (). Furthermore, only 33% of LHSs executives and physicians indicated their health system had invested in standardizing at least one of these initiatives.
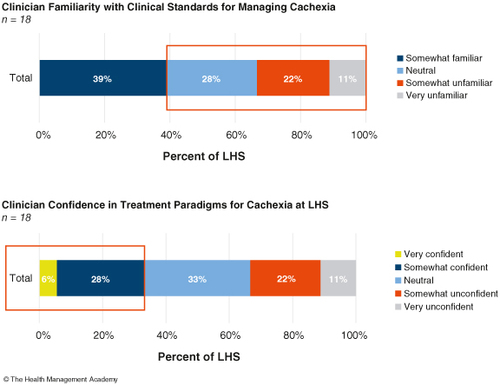
Challenges with timely intervention may be due, in part, to low physician familiarity with cachexia, low physician recognition of the warning signs that cachexia is present, or lack of confidence in clinical standards or treatment paradigms. These factors indicated physicians need clear guidance on clinical standards for delivering care to cancer patients with cachexia (). Indeed, low physician familiarity and confidence with clinical standards for cachexia was evident in the variation of evaluation metrics used across LHSs. Of the 18 LHSs surveyed, none indicated their clinicians were very familiar with the clinical standards for managing cachexia in patients with cancer. This was based on 18 LHSs clinicians surveyed. Overall, 61% stated they were either neutral or unfamiliar with the clinical standards for managing cachexia in patients with cancer. According to participant perspectives, most health systems did not seem to have access to registered dietitians who are appropriately trained and qualified to treat cachexia [Citation16]. This is a critical factor that limits the ability in the management of cachexia, which may, in turn, lead to the lower priority given to cachexia.
Figure 6. Barriers to timely intervention in the management of cachexia across leading health systems.
LHS: Leading health system.
Reprinted with permission from The LHSs Approach to Cachexia Care in Cancer Patients. ©The Health Management Academy March 2022, with permission from The Health Management Academy.
3.2.3. Resource allocation & wraparound services
Low prioritization of cachexia by C-Suite executives was shown to drive caregivers to rely upon wraparound services, such as psychiatry, social work, oncology, nutrition, home health and family therapy, provided within the oncology service line. For LHSs with wraparound services provided within the service line, these services are vital to comprehensive care for cancer patients with cachexia.
3.3. Survey responses: future outlook – closing the gap on cachexia care
The assessment found that some LHSs were more proactive than others in their approach to cachexia care. Reactive LHSs tended to wait until significant unintentional weight loss had been observed, while proactive LHSs triggered interventions prior to weight loss (e.g., for patients with high-risk conditions and treatments). A proactive health system typically implemented the correct screening protocols and processes for early intervention in the patient care journey, whereas reactive LHSs did not, with less advanced protocols. For example, HCP within some organizations may wait until substantial weight loss occurs in the patient prior to intervention. However, others took a proactive approach, adhering closely to cachexia risk identification and management guidelines.
LHSs executives and frontline HCP (n = 41) identified approaches that would elevate the priority given to cachexia (). Based on the research participants’ perspectives, 63% believed that the integration of care pathways into the EMR for cancer patients with cachexia would help elevate cachexia as a top long-term priority across the health system. Moreover, 61% of the research participants indicated that education for clinicians and senior leadership on the value of risk identification and care management would raise the priority of cachexia. Participants believed that EMR integration and providing education would increase clinician awareness and the likelihood to formally diagnose cachexia. Furthermore, 51% of executives and 10% of clinicians believed that investment in risk identification programs using ‘big data’ and predictive analytics would further elevate cachexia as a top long-term health system priority. For the purposes of this manuscript, the term ‘big data’ was defined for research participants as patient data collected from multiple sources, such as EMR, claims data, patient-generated information and social determinants of health.
Figure 7. Factors influencing the relative importance of cachexia in patients with cancer from the leading health system perspective. n = 41.
EMR: Electronic medical record; LHS: Leading health system.
Reprinted with permission from The LHSs Approach to Cachexia Care in Cancer Patients. ©The Health Management Academy March 2022, with permission from The Health Management Academy.
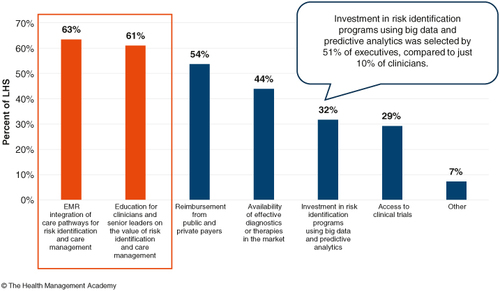
Executives and frontline HCP believed investment in risk identification programs using ‘big data’ and predictive analytics would also elevate cachexia to a top priority. None of the LHSs executives and HCP surveyed reported they actively used predictive analytics and ‘big data’ to identify patients at risk for cachexia. However, one large cancer center was evaluating optimal use of predictive analytics as it relates to use of proactive feeding tubes. The majority (77%) of respondents indicated they did not currently use these tools, although 33% stated they may do so in the future. LHSs executives and HCP surveyed indicated that a basics-first approach (beginning with EMR integration and education for frontline HCP and patients) would likely be the most effective approach to increase the uptake of more advanced solutions, such as predictive analytics, in the long term.
Overall, 32% of respondents indicated that investment in risk identification programs using big data and predictive analytics would help elevate cachexia to a top priority. Service line leaders must demonstrate the value in cachexia resources to elevate the priority of cachexia with C-Suite executives. This represents a twofold challenge because investment is needed to elevate cachexia as a priority; however, this requires resource and capital allocation.
3.4. Roundtable meeting faculty discussions
3.4.1. Addressing barriers to increase clinical trials enrollment
Roundtable participants indicated patient and health system barriers contributed to low clinical trial recruitment of cancer patients with cachexia. Challenges from the patient perspective were limited education or awareness of the benefits of clinical trial participation and access to transportation. Research personnel were critical to support clinical trial recruitment; however, LHSs were challenged to support these needs during an ongoing workforce crisis, workload and challenges with the identification of eligible participants. A collaboration between LHSs external partners may facilitate the development of novel solutions to address clinical trial recruitment, including EMR integration and external partnerships to support workforce needs. Roundtable participants also expressed a need for alerts, workflows and processes to streamline patient identification and clinical trial recruitment. However, providers indicated decision support aids would be useful to address potential ‘alert fatigue’.
3.4.2. Supporting frontline HCP to encourage early detection of cachexia
Physicians were aware of the critical role that dietitians play in the management of cancer patients with cachexia. However, many dietitians were unfamiliar with the published treatment guidelines. The health system has implemented the correct screening protocols and processes for early intervention in a patient’s care journey with LHSs that are reactive, which typically have less advanced protocols.
Roundtable participants emphasized the importance of educating multidisciplinary teams on the management and treatment of cancer patients with cachexia. Education on the importance of cachexia needs to be tailored to enhance the recognition of its symptoms, which underpins improved awareness, early identification and management.
Along with expanding provider education, almost all participants agreed that integrating dietitians within oncology teams and service lines would support care delivery in cancer patients with cachexia. Additionally, LHSs executives were interested in new drug therapies to support the management of cancer patients with cachexia.
3.4.3. Educating patients to support early detection & treatment compliance
Participants recognized the importance of supporting patient education and awareness of cancer cachexia. It was reported that many cancer patients with cachexia are unaware of the signs and symptoms of unintentional weight loss. Indeed, early prevention through patient education may improve health outcomes. Therefore, it is important that LHSs executives and external partners build patient education curriculums to support early detection efforts.
4. Discussion
Cachexia occurs in approximately 80% of patients with advanced cancer; however, it is often underdiagnosed, untreated, or undertreated [Citation3]. A meta-analysis of data from studies involving patients with advanced cancer showed that poor prognosis was linked to weight loss and anorexia [Citation17]. Cachexia also has a significant psychological impact for patients, families and caregivers, which often leads to poor quality of life [Citation18]. Left untreated, cachexia in elderly patients with cancer means they are at increased risk of disability, lengthy hospitalizations and greater costs while receiving chemotherapy compared with patients without cachexia, highlighting the need for early intervention [Citation19].
In light of the current state of cachexia care at LHSs, it is critical to understand the driving forces shaping C-Suite executive and frontline HCP perspectives. These perspectives may, and should, influence the prioritization of cachexia care in the next 5 years. In this assessment, cachexia was not considered a top priority by C-Suite executives across LHSs, and formal diagnoses were rare because of a lack of awareness and education. C-Suite executive support is often necessary to influence change in the prioritization of cachexia.
Low prioritization of cachexia leads to a lack of dedicated resources for care, leading patients to rely upon support services, which are often inconsistent and underfunded. Elevating cachexia as a top priority within oncology care could encourage changes in cost and coverage policy and highlight the importance of formally charted diagnoses.
The top perceived barriers to diagnosis and treatment of cachexia were cost, coverage and a lack of physician and patient awareness and education. As with other conditions, cost and coverage were perceived barriers to timely care for cancer patients with cachexia. This was largely related to coverage for feeding tubes, home health visits and nutrition counseling. Though nutrition counseling is critical to successful cachexia outcomes, many LHSs executives noted insurance does not often cover this, leading to late-stage diagnoses and referrals.
As intervention typically occurred after referral for nutritional counseling, dietitians were often leading cachexia care delivery, and only half of LHSs indicated physicians were responsible for making treatment recommendations for cancer patients with cachexia. Moreover, almost 30% of LHSs executives indicated nutritionists or dietitians were responsible for making treatment recommendations. However, it is critical that frontline physicians take a more active role in the identification, prevention and management of cachexia. Similarly, it is critical for C-Suite executives to implement and operationalize robust protocols for cachexia risk identification and care management across the health system, at scale.
Discussions at the roundtable meeting provided further perspectives on some key topics, including recommendations for early identification of patients at risk of cachexia and strategies to overcome barriers to detection, diagnosis and care. Educating patients to support early detection and treatment compliance, the role of education and LHSs and the importance of multidisciplinary patient care and the roles of nutrition and supportive care also were key elements in the approach to the management of cancer patients with cachexia.
None of the LHSs executives indicated they were very familiar with clinical standards for managing cachexia in patients with cancer. This low familiarity contributed to low rates of diagnosis and late intervention. This is of particular concern in light of the importance of early identification and intervention in cachexia outcomes. Low familiarity with cachexia contributed to low rates of diagnosis and late intervention. This was a critical issue because cachexia outcomes are positively impacted by early identification and intervention [Citation3]. Our findings are consistent with the results from a quantitative survey of physicians, nurses, dietitians and other oncology HCP, which found that 24% of participants lacked confidence in their ability to provide care for cachexia in patients with cancer [Citation20].
Patient engagement is key to the management of cancer patients with cachexia, together with a multidisciplinary team throughout the cancer journey, with weight loss as a continuous clinical indicator. A recent workshop that focused on addressing the needs of cancer patients with cachexia and their caregivers found that lack of awareness and understanding of cachexia among patients and their frontline HCP continues to be a challenge and underpinned the need for a multimodal, multidisciplinary approach to care [Citation21].
At present, the FDA and the EMA have not approved any pharmacological intervention for the treatment of cancer cachexia [Citation11,Citation12]. Treatment alternatives and support for clinical trial enrollment are important factors, and further research is needed to understand the challenges of recruiting patients for clinical trials. Patients that were not involved in clinical trials of cachexia expressed an interest in data from studies, as many patients indicated a lack of evidence around cachexia to inform evidence-based pathways.
LHSs or centers often provided cancer patients with cachexia with comprehensive wraparound services and support. These included proactive measures taken to avoid cachexia, active nutrition and dietitian involvement in care planning, and clinical trial offerings. Furthermore, clinical trial involvement and findings could benefit patients with cachexia and supplement the limited evidence-based care practices that exist today.
A limitation of this analysis was the small sample size and, thus, uncertainty as to how these findings can be generalized. However, the aim of this assessment was to capture information from the largest and most innovative LHSs in the USA. Indeed, the survey and qualitative interviews reflected perspectives of C-Suite executives, service line leaders, and frontline practitioners from the entire health system/enterprise. A secondary limitation to the sample may be that the assessment only focused on the largest LHSs in the USA (~150 with over US$2 billion in total operating revenue). The smaller LHSs perspectives were not included in this assessment, as this analysis was conducted to demonstrate the best practices and standards set by LHSs, which comprise a substantial share of total patients in the USA.
There is some evidence to suggest that early screening for the risk of cancer cachexia and nutritional intervention may contribute to the management of cachexia; however, there is currently no consensus on the use of nutritional supplementation. Further research is needed to identify the efficacy and tolerability of nutritional supplementation in patients with cancer cachexia, to inform evidence-based recommendations [Citation22].
Our research did not provide evidence that intervention in cancer cachexia will impact affected patients and the necessary redirection of healthcare resources, or the consequences of the poor prioritization of cachexia. Further research is needed to address these points. The roundtable participants made several recommendations on the current and future approach to cachexia. Participants expressed a need for alerts, workflows, and processes to streamline patient identification and recruitment to clinical trials. Roundtable participants also expressed an interest in integrating algorithms within existing workflows to identify eligible patients for clinical trials of cachexia. Additionally, dedicated providers to assess radiology and nutrition markers could assist in the identification of high-risk patients eligible for clinical trials. Participants also agreed that research centers and dedicated personnel are essential to cachexia clinical recruitment and retention. Indeed, integrating research coordinators within clinical visits may reduce patient barriers and streamline enrollment into clinical trials. Furthermore, extending clinical partnerships through digital care pathways or external partners providing LHSs with trained research personnel may support the expansion of frontline HCP capabilities to enroll patients in cachexia clinical trials.
Roundtable participants highlighted a need for continuing education on cancer cachexia clinical guidelines and treatments. Participants also agreed that integrating dietitians within oncology service lines is essential to the prevention and treatment of cachexia. Extending clinical partnerships through digital care pathways or remote monitoring may expand access to dietitians and support LHSs to manage cancer cachexia.
Additionally, roundtable participants expressed an interest in pharmacological advancements to support cancer cachexia prevention and management to optimize the management of the disease and improve health outcomes. Participants reported a need to educate patients on the signs and symptoms of cancer cachexia. Participants also agreed that dedicated personnel are essential to patient education, and that integrating dietitians and nurse educators within clinical visits would improve patient knowledge and awareness of cancer cachexia. Extending clinical partnerships through digital care pathways or external partners providing LHSs with trained personnel could support expansion of patient education services.
5. Conclusion
This assessment demonstrated that cachexia is not appropriately prioritized in cancer care among LHSs, and formal diagnoses are rare. Few LHSs executives and HCP reported that their health system took a proactive approach to cachexia, often leading to later-stage intervention for patients. Low C-Suite executive prioritization of cachexia leads to a lack of dedicated resources for risk identification and care management, driving patients to rely upon other support services provided by the health system or the community. Education on signs and symptoms is key to increasing prioritization and establishing formal diagnoses, backed by data from cancer care websites, including advocacy groups, major medical reference repositories and National Cancer Institute information sites. As awareness and education improve, the processes and structures in place to support patients will, in turn, be optimized.
The strategic and clinical prioritization of cachexia needs to be elevated across health system C-Suite executives. A proactive approach is needed for risk identification and management, as well as close adherence to current screening and treatment guidelines. There is great interest in predictive analytics for cachexia, although its current uptake is low. To elevate cachexia as a priority among C-Suite executives, service line leaders must demonstrate the value of investing in cachexia care and resources to LHSs.
Author contributions
All authors have contributed to the preparation and writing of the manuscript and approved the final manuscript.
Financial disclosure
This study was funded by Pfizer. I Jacobs and L Tarasenko are employees of Pfizer and hold stock and/or stock options. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Writing disclosure
Medical writing support was provided by N Misra of Engage Scientific Solutions and was funded by Pfizer.
Ethical conduct of research
This research was considered exempt from institutional research board review according to the US Department of Health and Human Services, Office for Human Research Protections, §46.101, (b)(2) (Basic HHS Policy for Protection of Human Research Subjects. US Department of Health and Human Services, Office for Human Research Protections. URL: www.hhs.gov/ohrp/regulations-and-policy/regulations/regulatory-text/index) because it involved survey procedures, and the information obtained could not be linked to the participants and did not place them at risk.
Data availablity statement
Upon request, and subject to review, Pfizer will provide the data that support the findings of this study. Subject to certain criteria, conditions, and exceptions, Pfizer may also provide access to the related individual de-identified participant data. See www.pfizer.com/science/clinical-trials/trial-data-and-results for more information.
Competing interests disclosure
The authors have no competing interests or relevant affiliations with any organization or entity with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Additional information
Funding
References
- Fearon K, Strasser F, Anker SD, et al. Definition and classification of cancer cachexia: an international consensus. Lancet Oncol. 2011;12(5):489–495. doi:10.1016/S1470-2045(10)70218-7
- Dunne RF, Roussel B, Culakova E, et al. Characterizing cancer cachexia in the geriatric oncology population. J Geriatr Oncol. 2019;10(3):415–419. doi:10.1016/j.jgo.2018.08.008
- von Haehling S, Anker SD. Cachexia as major underestimated unmet medical need: facts and numbers. Int J Cardiol. 2012;161(3):121–123. doi:10.1016/j.ijcard.2012.09.213
- Lim S, Brown JL, Washington TA, et al. Development and progression of cancer cachexia: perspectives from bench to bedside. Sports Med Health Sci. 2020;2(4):177–185. doi:10.1016/j.smhs.2020.10.003
- Aoyagi T, Terracina KP, Raza A, et al. Cancer cachexia, mechanism and treatment. World J Gastrointest Oncol. 2015;7(4):17–29. doi:10.4251/wjgo.v7.i4.17
- Pin F, Barreto R, Couch ME, et al. Cachexia induced by cancer and chemotherapy yield distinct perturbations to energy metabolism. J Cachexia Sarcopenia Muscle. 2019;10(1):140–154. doi:10.1002/jcsm.12360
- Bruggeman AR, Kamal AH, LeBlanc TW, et al. Cancer cachexia: beyond weight loss. J Oncol Pract. 2016;12(11):1163–1171. doi:10.1200/JOP.2016.016832
- Bossi P, Delrio P, Mascheroni A, et al. The spectrum of malnutrition/cachexia/sarcopenia in oncology according to different cancer types and settings: a narrative review. Nutrients. 2021;13(6):1980. doi:10.3390/nu13061980
- Esper DH, Harb WA. The cancer cachexia syndrome: a review of metabolic and clinical manifestations. Nutr Clin Pract. 2005;20(4):369–376. doi:10.1177/0115426505020004369
- Watanabe H, Oshima T. The latest treatments for cancer cachexia: an overview. Anticancer Res. 2023;43(2):511–521. doi:10.21873/anticanres.16188
- Roeland EJ, Bohlke K, Baracos VE, et al. Management of cancer cachexia: ASCO guideline. J Clin Oncol. 2020;38(21):2438–2453. doi:10.1200/JCO.20.00611
- Arends J, Strasser F, Gonella S, et al. Cancer cachexia in adult patients: ESMO clinical practice guidelines. ESMO Open. 2021;6(3):100092. doi:10.1016/j.esmoop.2021.100092
- Rezaei S, de Oliveira LC, Ghanavati M, et al. The effect of anamorelin (ONO-7643) on cachexia in cancer patients: systematic review and meta-analysis of randomized controlled trials. J Oncol Pharm Pract. 2023;29(7):1725–1735. doi:10.1177/10781552231189864
- Vaughan VC, Harrison M, Dowd A, et al. Evaluation of a multidisciplinary cachexia and nutrition support service—the patient and carers perspective. J Patient Exp. 2021;8:2374373520981476. doi:10.1177/2374373520981476
- Stahl M, Cheung J, Post K, et al. Accelerating virtual health implementation following the COVID-19 pandemic: questionnaire study. JMIR Form Res. 2022;6(5):e32819. doi:10.2196/32819
- Lee J, Briggs Early K, Kovesdy CP, et al. The impact of RDNs on non-communicable diseases: proceedings from the State of Food and Nutrition Series Forum. J Acad Nutr Diet. 2022;122(1):166–174. doi:10.1016/j.jand.2021.02.021
- Donohoe CL, Ryan AM, Reynolds JV. Cancer cachexia: mechanisms and clinical implications. Gastroenterol Res Pract. 2011;2011:601434. doi:10.1155/2011/601434
- Vaughan VC, Martin P, Lewandowski PA. Cancer cachexia: impact, mechanisms and emerging treatments. J Cachexia Sarcopenia Muscle. 2013;4(2):95–109. doi:10.1007/s13539-012-0087-1
- Biolcati-Rinaldi A, Sgarbi E. Cholangiocholecystography with phlebocysis of large doses of contrast medium in glucose solution. Arch Ital Mal Appar Dig. 1968;35(2):161–181.
- Baracos VE, Coats AJ, Anker SD, et al. Identification and management of cancer cachexia in patients: assessment of healthcare providers’ knowledge and practice gaps. J Cachexia Sarcopenia Muscle. 2022;13(6):2683–2696. doi:10.1002/jcsm.13105
- Garcia JM, Dunne RF, Santiago K, et al. Addressing unmet needs for people with cancer cachexia: recommendations from a multistakeholder workshop. J Cachexia Sarcopenia Muscle. 2022;13(2):1418–1425. doi:10.1002/jcsm.12910
- Braha A, Albai A, Timar B, et al. Nutritional interventions to improve cachexia outcomes in cancer—a systematic review. Medicina (Kaunas). 2022;58(7):966. doi:10.3390/medicina58070966
