Abstract
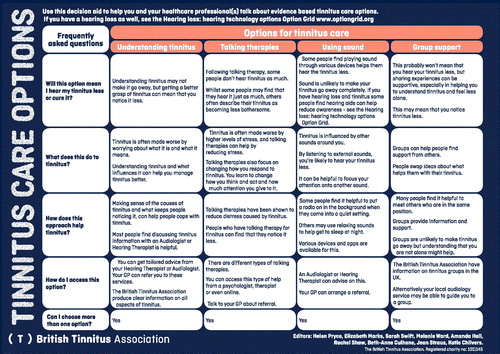
Objective: To develop a decision aid for tinnitus care that would meet international consensus for decision aid quality.
Design: A mixed methods design that included qualitative in-depth interviews, literature review, focus groups, user testing and readability checking.
Study sample: Patients and clinicians who have clinical experience of tinnitus.
Results: A decision aid for tinnitus care was developed. This incorporates key evidence of efficacy for the most frequently used tinnitus care options, together with information derived from patient priorities when deciding which choice to make.
Conclusion: The decision aid has potential to enable shared decision making between clinicians and patients in audiology. The decision aid meets consensus standards.
Background
Shared decision making has been enshrined in the United Kingdom National Health Service mandate as a principle of healthcare provision (NHS England Citation2014). It means that when there is more than one possible treatment or screening option available, clinicians can involve their patients in the process of deciding which course of care to pursue and patients can choose the treatment that reflects what is most important to them and fits with their lives (O’Connor et al. Citation2009). When patients have better knowledge and participation in decision making, there is evidence of increased decision quality, reduced decisional conflict and reduced decisional regret (O’Connor et al. Citation2009; Stacey et al. Citation2017). However, many clinicians still do not involve patients in these decisions (O’Connor et al. Citation2009; Pryce et al. Citation2018; Pryce and Hall Citation2014). Shared decision-making involves sharing clear information about the choice to be made and the pros and cons of that choice with the patient, and relevant others as applicable, to arrive at informed preferences (Pryce et al. Citation2016; Stacey et al. Citation2017).
Tinnitus is one of the most common chronic conditions affecting approximately 5–43% of the adult population with 3–31% finding it bothersome (McCormack et al. Citation2016). Currently, the quality of information for patients and clinicians on tinnitus treatments is highly variable (Fackrell et al. Citation2012). Clinical practices are non-standardised and rely heavily on individual clinical provider preferences (Hoare et al. Citation2012). This inhibits the potential for patients and clinicians to engage in shared decision making (Hoare et al. Citation2012). Moreover, while clinical guidelines emphasise the use of information as an important part of the therapy for people with tinnitus (Fackrell et al. Citation2012; Pryce and Hall Citation2014), the delivery of this information is framed within a “traditional” clinician-led prescription of care (Hoare et al. Citation2012; Hoare and Hall Citation2011).
It is a common misconception that variation in healthcare is a problem in itself (Mulley et al. Citation2012). Rather, the problem is that variation is not determined by patients’ informed preferences. In particular, there is a growing concern that patient preferences are commonly misdiagnosed (Mulley et al. Citation2012) with widespread inconsistency between clinicians’ perceived levels of shared decision making and that identified in actual performance (O’Connor et al. Citation1999). In particular, clinicians tend to confuse preferences in outcome with preferences in treatment (Mulley et al. Citation2012). In the case of tinnitus, there may be confusion between an outcome preference (e.g. to reduce awareness of tinnitus) with a treatment preference (cognitive or behavioural or acoustic self-management). This lack of clarity affects the interactions between patients and clinicians. A consistent approach to communicating the advantages and disadvantages of different treatment options is required to inform the patient and enable them to make a choice of treatment that is in line with their preferences.
Patients’ views and opinions about tinnitus healthcare services have typically been absent from the major reviews of service provision in the United Kingdom (Fackrell et al. Citation2012; Hoare et al. Citation2012). The chronicity of tinnitus means that therapeutic options rely on patient adherence to self-management and delivery (Tyler et al. Citation2008). Survey evidence suggests that in the US people with tinnitus are willing to pay for treatments to improve their symptoms (Tyler Citation2012). As such, patient preferences matter considerably in how tinnitus is managed over time.
Evidence suggests that if patients are given information about the range of therapeutic options available (including no treatment) patients who use a decision aid are more likely to choose one or a range of therapeutic options based on their preferences (Stacey et al. Citation2017). They are also more likely to adhere to and benefit from their chosen option. Current therapeutic options comprise largely acoustic strategies including hearing aids (where appropriate), and sound enrichment or psychological and stress reduction strategies (including relaxation, cognitive behavioural therapy (CBT) and mindfulness). Patient preferences for one or other management strategy are likely to be complex and individual. To facilitate conversations about these preferences, it is important to use evidence-based information and clearly outline the harms, benefits and potential side effects of all available options.
A way forward
We developed a targeted, evidence-based one-page decision aid in the form of a table to summarise treatment options considering the questions most frequently asked by patients. Evidence from previous studies suggests that a simple grid style decision aid is acceptable to clinicians (Health Foundation Citation2012). Furthermore, simpler paper-based decision aids are as effective as more expensive Digital Video Disks (DVD) decision tools (Shue et al. Citation2016). The decision aid can enable shared decision making by consistently presenting clear choices, for example, the preference for acoustic and auditory treatments compared to psychological or stress targeted treatments. Comparing treatments will thereby lead to clarity about treatment options and a formalised way of incorporating patient preferences into therapeutic decision-making. A recent Cochrane review of decision aids concluded that there is strong evidence that decision aids improve knowledge of options, help patients feel better informed and enable patients to identify what matters most to them (Stacey et al. Citation2017). Patients using decision aids had more realistic expectations. There is also moderate evidence that the presence of a decision aid leads to patient engagement with shared decision-making and may achieve decisions which are consistent with patient preferences (Stacey et al. Citation2017). In a chronic condition such as tinnitus with no single effective treatment, it is important that patient preferences are made explicit through the decision.
Objectives and methods
We were informed by Marrin’s guidance on decision aid development (Citation2013). The decision aid development process consisted of a sequence of steps, aligned with Marrin’s framework to develop option grid decision aids. This framework conforms to the standards required by the International Patient Decision Aid Standards (IPDAS) (Sepucha et al. Citation2018):
identify patient held preferences and frequently asked questions for tinnitus treatment.
identify the treatment options best supported by research evidence for inclusion in the decision aid.
form an editorial team to design drafts of the decision aid.
user test to iterate drafts of the decision aid with a series of focus groups involving professional groups, patient groups, and combinations of the two.
assess readability of the decision aid.
assess useability of the decision aid.
See supplement S5 for flow chart.
We number each section below to indicate the stage of this process that was being undertaken.
We were supported in this by members of the preferences laboratory at Dartmouth College in the United States of America. Specifically author (MD) had a role in supervision of the process and steering decision making.
Health Research Authority ethics approval was gained from West Midlands South Birmingham Research Committee [16/WM/0142].
Methods
A mixed methods approach (e.g. a range of qualitative methods including interview, focus group, observation, think aloud and user testing) was taken to fulfil the objectives.
Qualitative work – the development of the frequently asked questions (FAQs)
Four researchers (HP, BAC, SS, BC) conducted in depth interviews with 41 individuals who had sought help for tinnitus. These individuals differed in terms of demographic factors, nature of hearing help, hearing loss and tinnitus distress. Of the 41 participants in this phase, 32 (78%) lived on owner occupier housing and 9 (22%) lived in mixed housing districts. Seventeen (41%) were female and 24 (59%) were male. Twenty-four (58.5%) reported additional hearing loss and 19 (46%) had received care from Otolaryngologists. In addition, 10 (24%) had received care from Audio-Vestibular Physicians; 15(36%) from Audiologists and 22 (54%) from Hearing Therapists. All participants had consulted General Practitioners about tinnitus. The age range of our sample were predominantly over 50 years (80%). To ensure contrast, we sought and included participants in their 20 s and 30 s. Therefore the information gaps that led to the frequently asked questions on the decision aid were based on common information needs and not related to any particular help-seeking pathway.
Preference themes were analysed from in-depth interviews with patient participants who contrasted in tinnitus services received, nature of tinnitus and levels of distress associated with it. In-depth interviews were conducted in the participants’ homes or clinic locations, were audio recorded and transcribed. They were analysed using grounded theory methods. This involves constant comparison of accounts to develop themes that are modelled into an overarching theory about how a phenomenon (in this case how preference for coping with tinnitus occur and are mediated) (Straus and Corbin Citation1998, 78). These interviews were focussed on eliciting patient preferences for tinnitus care and the key information that patients required to make decisions about clinical care.
Literature review – the development of the options for treatment
In accordance with the procedure described by Marrin et al. (Citation2013) evidence from systematic review and clinical guidance was reviewed. Five databases (PubMed, Ovid, Web of Science, Cochrane Library and Google Scholar) were searched with “tinnitus” in the title and “management” or “intervention” or “treat*” in the abstract. No limit to the search by time period or publication date were applied. Twenty-five articles were selected according to methodological quality in the form of meta-analysis or systematic review where possible. Where that was not possible researchers sought experimental studies with a low risk of bias (controlled, blinded as far as possible, no obvious conflicts of interest, adequate sample size). Researchers also consulted professional guidelines (e.g. Tunkel et al. Citation2014) and evidence from cohort and qualitative studies to determine clinically relevant interventions that are frequently recommended in practice. The options were included on the basis of research evidence and editorial team consensus on clinical practice as suggested by Marrin et al. (Citation2013). The evidence drawn upon to address points in the decision aid was included in a evidence summary published alongside the decision aid (). The editorial team agreed to refer to options as “approaches” without specifying the precise intervention, for example “talking therapies” was used to encompass a range of possible interventions including cognitive behavioural and mindfulness interventions. This is to enable the choices presented to be responsive to local health commissioning and provision arrangements and to allow for the evidence supporting individual interventions to emerge while still maintaining the relevance of the decision aid. “Consensus” refers to complete agreement by all editorial team. The hearing loss option grid decision aid (www.optiongrid.org) was referred to under the “using sound” section to direct patients to further information on how to manage hearing loss. See for evidence summary.
The editorial team
Following the procedure in Marrin et al. (Citation2013), we recruited a multidisciplinary stakeholder team (overseen by Marie-Anne Durand). The editorial team included the research team plus other volunteers with appropriate expertise: one Head of Hearing Therapy and Audiology service, two Clinical Scientists in Audiology, one Health Psychologist, one Clinical Psychologist, four researchers (also trained Hearing Therapists) and a patient research ambassador (a lay member with particular knowledge and interest of research). The editorial team worded the decision aid initially. All members disclosed any interest with the evidence reported on the decision aid. No conflicts of interest were reported.
Once the decision aid had been drafted, a wider reference group of professionals were asked to consider whether the content reflected current views of tinnitus treatments. The wider references group were volunteer members of the British Tinnitus Association’s Professional Advisory Committee and included medical experts including Audio-Vestibular Physicians and Otolaryngologists.
Iterative development – focus groups
Once a drafted version of the decision aid was agreed between the editorial team, it was circulated to members of six focus groups. illustrates the make-up of the focus group participants in each location.
Table 1. Focus group participants.
The focus group questions () were derived to capture both participant views of decision aids, the potential uses of the tinnitus decision aid, and the notion of choice of treatments in hearing healthcare. The questions below were used in each location and group. The decision aid was also distributed to British Tinnitus Association Professional Advisory Committee members for feedback and any clarifications required were made to the text.
Table 2. Focus group questions.
Readability testing
Readable.io software was used to determine the average reading age of the decision aid (https://readable.io/).
User testing
The participants at focus groups “user tested” the decision aid by reading it, checking it was understandable and that the intended meaning was clear. Clinical colleagues from the teams involved in the decision aid development tried out the decision aid in clinical practice. The clinicians subsequently fed their experience back to the editorial group regarding the feasibility (e.g. time to administer, resources to incorporate, skills to incorporate into routine care) and acceptability (e.g. quality of decision aid and toleration of decision aid) in routine practice and any clarifications that were required.
Results
Development of the frequently asked questions
Explicit and inferred preferences were included in the initial analysis by coding all utterances that related to treatment and outcome preferences for their tinnitus. Indirect references, including throwaway comments, non-verbal communication (tone, physical signs and cues) were included as meaning units. Meaning units were identified across the whole sample of interview data and were given a summary code (derived from language used by the participant e.g. “cure”).
The coded themes were examined for uncertainties or questions that were voiced and these formed the basis for the frequently asked question items. The wording of these items was then amended by focus group members to express the question more precisely. Five frequently asked questions were included which summarised the main concerns expressed by participants. Four therapeutic approaches were worded in broad terms to allow for variations in evidence of efficacy. For example, “using sound” referred to using a variety of sources of sound. Likewise, “talking therapies” encompasses a range of therapeutic techniques. Please see Supplementary Table S1 (http://tandfonline.com/doi/suppl.) for an illustration of how interview data informed frequently asked questions. Patient preferences were captured for both treatments and for outcomes. In describing preferences patients were asked to comment on the quality and value of information that was required to make decisions about their care. This was collated into themes and translated from comment into question. Please see Supplementary Table S1 to illustrate this process. The frequently asked questions to include in the decision aid were derived from these qualitative interviews and were the questions that participants reported needing information on in order to decide what to do about tinnitus.
Refinement as a result of the focus group
The focus groups were helpful in refining the wording and arrangement of the decision aid. For example, participants asked for re-wording of the frequently asked questions to capture their most pressing question first in the decision aid. The participants also proposed re-ordering the options to present understanding tinnitus as the first option. All participants reflected on the best way and time to introduce the decision aid and the consensus was that it would be best used before the initial dedicated tinnitus appointment with the audiological clinician. All participants reported finding this helpful as a tool to navigate therapeutic options. Please see Supplementary Tables S2 and S3 for detail on changes made through the process (http://tandfonline.com/doi/suppl).
Readability
Following the final focus group changes, the decision aid was further refined through the process of establishing readability. Readable.io software was used to identify current reading age of the text and areas where it could be simplified to lower the reading age. As a result, longer clauses were simplified and shortened and some technical language was removed for example “cognitive behaviour therapy” and “mindfulness based cognitive behavioural therapy” were removed in favour of the more generic “talking therapy”. This resulted in a lowered reading age from 8.7 to 7.8 (Flesch-Kincaid grade) and a readability rating of “A”. The text that prevented the reading age being lowered further was the use of technical terms “tinnitus” and “audiologist” but the editorial consensus was that these terms should remain.
Useability
The decision aid was formatted by the British Tinnitus Association and branding was incorporated into the decision aid. The aid was then distributed to clinicians to try in practice. Two clinicians provided feedback on the use of the aid. Feedback from clinicians was that the aid was clear and easy to use, but that the process of introducing choices into the standard clinical scripts was challenging as it required a change to usual practice. Feedback was that this tool was a helpful addition in communicating information and that they would be willing to adopt the decision aid into routine practice. A future service evaluation of this change in practice is required to assess the impact of the decision aid on patient satisfaction with decisions. Such evaluations should be reported according to consensus standards (Sepucha et al. Citation2018).
Conclusion
Assessing the quality of the tinnitus decision aid
The IPDAS consensus has led to a quantile checklist (IPDASi) (Elwyn et al. Citation2009). Here, we apply the checklist to our decision aid (Supplementary Table S4). The process outlined in Marrin et al. (Citation2013) has been followed in the development of this decision aid.
Decision aids are deceptively simple looking but require a complex range of skills from their developers. This decision aid required interpretation and synthesis of qualitative data, secondary literature review, focus group management, coordination of experts, professional groups and teams. Given this complexity, a structured procedure was helpful.
Similarly, the process of incorporating shared decision-making into practice is complex and requires skill on the part of clinicians to recognise and respond to patient’s values and preferences. This tool is a contribution to informing the patient of the opportunities for care and engaging them in clinical decision making. Please see Supplementary Table S4 to illustrate how the decision aid fits IPDASi domains (http://tandfonline.com/doi/suppl).
The decision aid is available at www.tinnitus.org.uk/decision-aid.
Further guidance on how to apply shared decision making and an illustration of the process of using the decision aid is available on video at: https://www.youtube.com/watch?v=6726cCoRDrE and at www.tinnitus.org.uk/decision-aid.
Supplemental Material
Download MS Word (40.7 KB)Supplemental Material
Download MS Word (12.4 KB)Supplemental Material
Download MS Word (12.1 KB)Supplemental Material
Download MS Word (12.5 KB)Supplemental Material
Download MS Word (12.2 KB)Supplemental Material
Download MS Word (44.8 KB)Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Elwyn, G., A. M. O’Connor, C. Bennett, R. G. Newcombe, M. Politi, M. A. Durand, E. Drake, et al. 2009. “Assessing the Quality of Decision Support Technologies Using the International Patient Decision Aid Standards instrument (IPDASi).” PLoS One 4 (3): e4705. doi:10.1371/journal.pone.0004705.
- Fackrell, K., D. J. Hoare, S. Smith, A. McCormack, and D. A. Hall. 2012. “An Evaluation of the Content and Quality of Tinnitus Information on Websites Preferred by General Practitioners.” BMC Medical Informatics and Decision Making 12 (1): 70. doi:10.1186/1472-6947-12-70.
- Health Foundation. 2012. MAGIC: Shared decision making. Accessed 22 January 2018. http://www.health.org.uk/areas-of-work/programmes/shared-decision-making/
- Hoare, D. J., P. E. Gander, L. Collins, S. Smith, and D. A. Hall. 2012. “Management of Tinnitus in English NHS Audiology Departments: an Evaluation of Current Practice.” Journal of Evaluation in Clinical Practice 18 (2): 326–334. doi:10.1111/j.1365-2753.2010.01566.x.
- Hoare, D. J., and D. A. Hall. 2011. “Clinical Guidelines and Practice: A Commentary on the Complexity of Tinnitus Management.” Evaluation & The Health Professions 34 (4): 413–420. doi:10.1177/0163278710390355.
- Marrin, K., K. Brain, M. A. Durand, A. Edwards, A. Lloyd, V. Thomas, and G. Elwyn. 2013. “Fast and Frugal Tools for Shared Decision-making: How to Develop Option Grids.” European Journal for Person Centered Healthcare 1 (1): 240–245. doi:10.5750/ejpch.v1i1.657.
- McCormack, A., M. Edmondson-Jones, S. Somerset, and D. Hall. 2016. “A Systematic Review of the Reporting of Tinnitus Prevalence and Severity.” Hearing Research 337: 70–79. doi:10.1016/j.heares.2016.05.009.
- Mulley, A. G., C. Trimble, and G. Elwyn. 2012. Patients’ Preferences Matter: Stop the Silent Misdiagnosis. London: King’s Fund.
- NHS England. 2014. “Shared Decision Making.” Accessed 26 July 2017. https://www.england.nhs.uk/ourwork/pe/sdm/
- O’Connor, A. M., C. L. Bennett, D. Stacey, M. Barry, N. F. Col, K. B. Eden, V. A. Entwistle, et al. 2009. “Decision Aids for People Facing Health Treatment or Screening Decisions.” The Cochrane Database of Systematic Reviews (3): CD001431. doi:10.1002/14651858.CD001431.pub2.
- O’Connor, A. M., A. Rostom, V. Fiset, J. Tetroe, V. Entwistle, H. Llewellyn-Thomas, M. Holmes-Rovner, M. Barry, and J. Jones. 1999. “Decision Aids for Patients Facing Health Treatment or Screening Decisions: Systematic Review.” British Medical Journal 319 (7212): 731–734. doi:10.1136/bmj.319.7212.731.
- O’Connor, A. M., J. E. Wennberg, F. Legare, H. A. Llewellyn-Thomas, B. W. Moulton, K. R. Sepucha, A. G. Sodano, and J. S. King. 2007. “Toward the ‘Tipping Point’: Decision Aids and Informed Patient Choice.” Health Affairs 26 (3): 716–725. doi:10.1377/hlthaff.26.3.716.
- Pryce, H., and A. Hall. 2014. “The Role of Shared Decision-making in Audiologic Rehabilitation.” Perspectives on Aural Rehabilitation and Its Instrumentation 21 (1): 15–23. doi:10.1044/arri21.1.15.
- Pryce, H., A. Hall, A. Laplante-Lévesque, and E. Clark. 2016. “A Qualitative Investigation of Decision Making During Help-seeking for Adult Hearing Loss.” International Journal of Audiology 55 (11): 658–665. doi:10.1080/14992027.2016.1202455.
- Pryce, H., A. Hall, E. Marks, B. A. Culhane, S. Swift, J. Straus, R. L. Shaw. 2018. “Shared Decision Making in Tinnitus Care – An Exploration of Clinical Encounters.” British Journal of Health Psychology online doi:10.1111/bjhp.12308.
- Readable software from https://readable.io/
- Sepucha K. R., P. Abhyankar, A. S. Hoffman, H. Bekker, A. LeBlanc, C. Levin, M. Ropka, et al. 2018. “Standards for UNiversal Reporting of Patient Decision Aid Evaluation Studies: The Development of SUNDAE Checklist” BMJ Quality & Safety Published Online First: 21 December 2017. doi:10.1136/bmjqs-2017-006986.
- Shue, J., R. Karia, D. Cardone, J. Samuels, M. Shah, and J. Slover. 2016. “A Randomized Controlled Trial of Two Distinct Shared Decision Making Aids for Hip and Knee Osteoarthritis in an Ethnically Diverse Patient Population.” Value in Health 419: 487–493. doi:10.1016/j.jval.2016.01.006.
- Stacey, D., F. Légaré, K. Lewis, M. J. Barry, C. L. Bennett, K. B. Eden, M. Holmes-Rovner, et al. 2017. “Decision Aids for People Facing Health Treatment or Screening Decisions.” Cochrane Database of Systematic Reviews, (4): CD001431. doi:10.1002/14651858.CD001431.pub5.
- Straus, A., and J. Corbin. 1998. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. Thousand Oaks, CA: Sage Publications.
- Tunkel, D. E., C. A. Bauer, G. H. Sun, R. M. Rosenfeld, S. S. Chandrasekhar, E. R. Cunningham Jr, S. M. Archer, et al. 2014. “Clinical Practice Guideline: Tinnitus.” Otolaryngology–Head and Neck Surgery 151 (2_suppl): S1–S40. doi:10.1177/0194599814545325.
- Tyler, R. S. 2012. “Patient preferences and willingness to pay for tinnitus treatments.” Journal of the American Academy of Audiology 223: 115–125. doi:10.3766/jaaa.23.2.6.
- Tyler, R. S., S. A. Chang, A. K. Gehringer, and S. A. Gogel. 2008. “Tinnitus: How You Can Help Yourself!” Audiological Medicine 16: 85–91. doi:10.1080/16513860801912281.