Abstract
Objective: Provide recommendations to audiologists for the management of children with unilateral hearing loss (UHL) and for needed research that can lend further insight into important unanswered questions.
Design: An international panel of experts on children with UHL was convened following a day and a half of presentations on the same. The evidence reviewed for this parameter was gathered through web-based literature searches specifically designed for academic and health care resources, recent systematic reviews of literature, and new research presented at the conference that underwent peer review for publication by the time of this writing.
Study sample: Expert opinions and electronic databases including Cumulative Index to Nursing and Allied Health Literature (CINAHL), Cochrane Library, Education Resources Information Centre (ERIC), Google Scholar, PsycINFO, PubMed, ScienceDirect, and Turning Research into Practice (TRIP) Database.
Results: The resulting practice parameter requires a personalised, family-centred process: (1) routine surveillance of speech-language, psychosocial, auditory, and academic or pre-academic development; (2) medical assessments for determination of aetiology of hearing loss; (3) assessment of hearing technologies; and (4) considerations for family-centred counselling.
Conclusions: This practice parameter provides guidance to clinical audiologists on individualising the management of children with UHL. In addition, the paper concludes with recommendations for research priorities.
Introduction
Unilateral hearing loss (UHL), once considered to be a nuisance and not taken seriously by hearing professionals, has been shown in recent decades to put children at risk for academic, speech and language, and social and/or behavioural deficits (e.g. Bess and Tharpe Citation1986; Lieu Citation2004; Lieu Citation2013). Despite increased understanding of these problems, there exists little evidence of effective interventions that ameliorate these deficits.
This practice parameter reviews the available empirical evidence, considers expert opinion, and provides specific recommendations for the management of children with UHL. The approach described requires a personalised, family-centred process: (1) routine developmental surveillance of speech-language, psychosocial, auditory skill, and academic or pre-academic development; and (2) assessments of hearing technologies specific to a variety of listening environments. In addition, although a number of important developments in the area of UHL have emerged over the past several decades, there remains a need for continued research. Recommendations are made for future research endeavours to enhance our understanding of and improve our management of children with UHL.
Much of the guidance for children with UHL applies to all children with hearing loss – those with unilateral or bilateral loss. Therefore, a brief summary of available published guidelines for assessment and management of children with hearing loss appears at the beginning of this document followed by more specific considerations for children with UHL and their families.
Definitions
Unilateral hearing loss (UHL) – any degree of permanent hearing loss in one ear (pure-tone average [0.5, 1.0. 2.0 kHz] > 15 dB for children), regardless of aetiology, with normal hearing1 in the opposite ear.
Paediatric population – for purposes of this guideline, refers to children birth through 18 years of age.
Contralateral routeing of signal (CROS) hearing aid – a type of hearing aid that is intended for use by those with normal or near-normal hearing in one ear and an opposite side un-aidable ear. Sound is transmitted from the side of the un-aidable ear to the ear with better hearing.
Bone-conduction devices2 – the class of bone-conduction devices that transmits vibration via transcutaneous or percutaneous means (surgical or non-surgical devices; transcranial).
Remote microphone system (RMS) – a wireless microphone system that converts audio signals into radio signals and transmits them to a receiver at the ear. Sounds can be transmitted via frequency modulation (FM) or digital modulation (DM).
Profound unilateral hearing loss3 – hearing loss in one ear with a pure tone average (PTA) of >90 dB HL.
Unaidable hearing loss – hearing loss that because of profound degree, very poor speech recognition, or intolerance for amplified sounds cannot be fitted with conventional hearing aids.
Description of the process
An international panel of experts on the screening, assessment, management, and monitoring of children with unilateral hearing loss and a parent advocate convened on October 24, 2017 following a day and a half of presentations on the same. Evidence reviewed for this parameter was gathered through literature searches using web search engines specifically designed for academic and health care resources and two recent systematic reviews of the literature were considered (Appachi et al. Citation2017; Anne, Lieu, and Cohen Citation2017). Eight electronic databases were searched using a series of keywords and expanded search terms related to children, unilateral hearing loss, cochlear implant, contralateral routeing of signal, bone conduction, BAHA, and single-sided deafness. Electronic databases included Cumulative Index to Nursing and Allied Health Literature (CINAHL), Cochrane Library, Education Resources Information Centre (ERIC), Google Scholar, PsycINFO, PubMed, ScienceDirect, and Turning Research into Practice (TRIP) Database.
Basic principles of identification, assessment, and management of children with all degrees of hearing loss
Audiologic monitoring
Numerous published guidelines by various national organisations have outlined recommendations for newborn hearing screening and assessment of hearing loss in children (e.g. Joint Committee on Infant Hearing [JCIH; AAP Citation2007]; American Academy of Audiology [AAA Citation2012]; American Speech-Language-Hearing Association [ASHA] Citation2004; American Academy of Paediatrics [AAP Citation2003]; Ministry of Children, Community and Social Services, 2018). This committee endorses the use of said guidelines in the provision of family-centered early intervention. Specifically, this committee supports the recommendation that hearing be screened by 1-month of age, hearing loss diagnosed by 3-months of age, and intervention be offered by 6-months of age. These recommendations hold true for all forms of permanent hearing loss, including those that are unilateral.
Developmental monitoring
In addition to routine audiologic measures, a variety of tools are available to paediatric audiologists and other professionals charged with monitoring auditory, speech, language, and developmental milestones for children with permanent hearing loss, before and after the provision of various technologies. These tools are especially important when children with minimal degrees of loss are receiving limited or no intervention services from specialised providers (see ). This committee endorses the use of these and other screening tools to assist families or teachers in identifying listening and/or speech or language concerns for children. Audiologists are encouraged to provide such tools to the families of children with UHL as deemed appropriate. Involving families and other professionals in the use of screening tools is expected to enhance communication among stakeholders, thus, leading to early suspicion, and perhaps intervention, of hearing-related problems.
Table 1. Auditory-related subjective outcome evaluation tools.
The AAP recommends developmental and behavioural screening with a standardised developmental screening tool when a child is 9, 18, and 24 or 30 months of age. Although some of this screening will be done in the child’s medical home (AAP Citation2007), audiologists and other professionals working with children with hearing loss should be aware of available resources for developmental screening, ensure such screenings are ongoing and, if not, consider the use of such measures themselves to determine if additional referrals are needed. One such tool, ‘Birth to Five: Watch Me Thrive! A Compendium of Developmental Screening Measures,’ is produced through a coordinated effort by several U.S. agencies.
Early intervention
The JCIH (AAP Citation2007) states that families of infants with any degree of bilateral or unilateral permanent hearing loss should be considered eligible for early intervention services and that services for infants with confirmed hearing loss should be provided by professionals who have expertise in hearing loss. Furthermore, the JCIH Supplement (AAP Citation2013) states that children identified with hearing loss of any degree, including those with unilateral or mild hearing loss, receive appropriate monitoring, and follow-up intervention services when appropriate.
Technology management
For children with hearing loss, guidelines provide recommendations for hearing aids and other hearing technologies, including remote microphone systems (RMS; AAA Citation2011a, Citation2011b, Citation2013; Ontario Infant Hearing Program Audiologic Assessment Protocol Citation2008).
Consensus-based principles of identification and audiologic assessment and monitoring of children with UHL
Identification
The identification of UHL among children might be improved by monitoring children who present with risk factors for progressive or late-onset hearing loss, as recommended by JCIH (AAP Citation2007). The culmination of several reports demonstrate that the majority (>50%) of cases of UHL are due to cochlear malformations such as enlarged vestibular aquaduct syndrome (EVA) and Mondini dysplasia (Dodson et al. Citation2012; Friedman et al. Citation2013; Haffey, Fowler, and Anne Citation2013; Masuda, Usui, and Matsunaga Citation2013; Paul Citation2016; Fitzpatrick et al. Citation2017; van Beeck Calkoen et al. Citation2017). Environmental causes, such as cytomegalovirus (Paul Citation2016) and genetic causes are also implicated as common aetiologies of UHL (Dodson et al. Citation2012; Paul Citation2016; Fitzpatrick et al. Citation2017) although no specific genes for UHL have been identified to date. Additional risk factors for UHL include a stay in a neonatal intensive care unit (NICU), in utero infections, craniofacial anomalies, postnatal infections, and syndromes (Friedman et al. Citation2013; Fitzpatrick et al. Citation2017). Given the association between UHL and specific medical conditions, this committee supports etiologic assessment following confirmation of UHL. Specifically, audiologists should ensure that recommendations are made for complete otologic evaluation, including imaging, whether testing is completed within one’s own institution or requires referrals to outside care providers.
Audiologic assessment and monitoring
Recent estimates (2013–2014) show the prevalence of UHL among newborns to be approximately .6 to .7 per 1000 births in the U.S. (Centers for Disease Control Early Hearing Detection and Intervention [CDC] Database). Further evidence shows that UHL progresses to bilateral hearing loss in 7.5 to 11% of cases (Paul et al. 2017; Haffey, Fowler, and Anne Citation2013) and the number of children with UHL increases considerably after the newborn period. In fact, investigators have reported that approximately 2.5–3% of school-age children are reported to have UHL (Bess, Dodd-Murphy, and Parker Citation1998; Shargorodsky et al. Citation2010). This increase in prevalence underscores the need for ongoing vigilance throughout childhood.
The immediate consequence of UHL is loss of binaural function, which has a negative impact on localisation (Humes, Allen, and Bess Citation1980; Johnstone, Nabelek, and Roberston Citation2010) and speech perception in noise (Bess, Tharpe, and Gibler Citation1986; Ruscetta, Arjmand, and Pratt Citation2005). There is also evidence that suggests UHL negatively impacts balance (Wolter et al. Citation2016), early auditory behaviour and preverbal vocalisation (Kishon-Rabin et al. Citation2015), speech and language development (Ead et al. Citation2013; Lieu Citation2013), academic attainment (Bess and Tharpe Citation1986; Lieu Citation2004; Lieu Citation2013), and even cognition (Ead et al. Citation2013; Lieu Citation2013). Therefore, children with UHL will benefit from referral for comprehensive speech and language diagnostics, and academic monitoring. Measures that focus on speech-in-noise ability are recommended to assess the need for hearing assistive technologies (HAT) that enhance the signal-to-noise ratio (SNR).
A formal assessment of localisation is also needed to determine degree of difficulty. The ability to localise sounds on the horizontal plane is ideally measured in an anechoic chamber using a large number of speakers arranged in an array (Besing and Koehnke Citation1995; Johnstone, Nabelek, and Robertson Citation2010). This set up is not feasible for clinical use, though some clinics might choose to set up a speaker array with a smaller number of speakers. A more clinically feasible approach is to measure localisation using functional surveys or questionnaires. Localisation is a target skill of the Auditory Behaviour in Everyday Life (ABEL; Purdy et al. Citation2002) and a major domain of the Speech Spatial and Qualities of Hearing Questionnaire (SSQ parent and child versions; Galvin and Noble Citation2013). See for these and other functional assessment tools.
Consensus-based principles of medical management of children with UHL
Medical considerations, although not the direct responsibility of paediatric audiologists, can impact the audiologic management of a child with UHL. Recommendations for the medical evaluation of children with hearing loss vary widely. However, we can draw upon international and interdisciplinary statements of recommendations that are relevant to children with UHL (e.g. International Paediatric Otorhinolaryngology Group [IPOG; Liming et al. Citation2016]; AAp Citation2007). These reports include several recommendations that are relevant to children with UHL, including temporal bone imaging (specifically with magnetic resonance imaging [MRI]); genetic testing (in patients with known or suspected syndromic hearing loss or in children with unilateral or bilateral Auditory Neuropathy Spectrum Disorder [ANSD] when imaging for cochlear dysplasia is negative); ophthalmology (because of the increased risk of ocular abnormalities in nonsyndromic sensorineural hearing loss [SNHL]); and testing for cytomegalovirus (CMV), which causes 20–25% of all congenital sensory hearing loss and is a frequent cause of progressive hearing loss (Fowler Citation2013). A specific link between CMV and UHL has not been determined at the time of this writing. However, with the nascent introduction of CMV screenings that are being initiated in some newborn nurseries, these data might soon be available.
Consensus-based principles of technology management for children with UHL
Conventional hearing aids
For permanent hearing loss on the affected side, conventional air-conduction hearing aid fitting is recommended as a first-line treatment if the affected side is moderate to severe in degree, regardless of child’s age. If the affected side is minimal to mild in degree, it is recommended that audiologists refer to the Clinical Decision Support Guideline (Bagatto and Tharpe Citation2014) for guidance. If the affected side is profound in degree, the ear might be unaidable and an RMS is recommended as first-line treatment for certain listening situations. Currently, there are no adjustments for prescriptive targets for paediatric unilateral hearing aid fittings. When appropriate, speech perception abilities, speech-in-noise testing, and spatial hearing assessments can be conducted to determine benefit with a device. Also, note that for some children, detection of sound – not just speech perception – might be a desirable outcome of an aided ear for safety purposes.
Bone-conduction devices
For infants and young children with unilateral microtia or atresia and for whom conventional air-conduction hearing aids cannot be fitted, a bone-conduction device should be considered. Children under the age of 5 years are not eligible for surgical bone-conduction devices in most countries and, therefore, can be offered devices on a soft headband. Surgical repair of the affected side often does not occur until age 7 or 8 years of age, so a non-surgical bone conduction device can be considered to support access to sounds to the affected side.
Remote microphone systems (RMS)
RMS provides a means of overcoming the deleterious effects of noise, distance, and reverberation by placing a microphone/transmitter close to the mouth of a talker or connecting the transmitter to audio sources such as televisions or computers (e.g. Wolfe, Lewis, and Eiten Citation2016). Remote receiver options include
small receivers coupled to the listener’s ear(s) in a variety of ways (personal ear level RMS);
one or more loudspeakers placed at strategic locations in a room (classroom audio distribution systems, aka sound field RMS);
a small loudspeaker placed on a tabletop close to the listener (personal desktop RMS).
Guidelines for eligibility, implementation, and validation of RMS are available (AAA Citation2011a, Citation2011b). According to these guidelines, children are considered potential candidates for RMS when they demonstrate documented evidence of hearing, listening, and/or learning problems. Children with UHL exhibit poorer speech perception in noise and reverberation than peers with normal hearing (Bess, Tharpe, and Gibler Citation1986; Bovo et al. Citation1988; Hartvig Jensen, Johansen, and Borre Citation1989; Ruscetta, Arjmand, and Pratt Citation2005), thus, are candidates for RMS. However, there is limited research examining the efficacy of ear level RMS specifically for children with UHL and no research that has examined the benefits of desktop or classroom audio distribution systems for these children. In two studies conducted in the 1990s (Kenworthy, Klee, and Tharpe Citation1990; Updike Citation1994), children with UHL demonstrated better speech recognition with personal RMS than with either CROS or conventional hearing aids. However, the current applicability of those studies is limited by the small number of subjects as well as more recent advances in all classes of amplification technologies. At present, determining the efficacy of RMS for children with UHL relies on evidence of benefit from cohorts that include children with bilateral hearing loss and children with normal hearing who have special listening needs (Moeller et al. Citation1996; Pittman et al. Citation1999; Tharpe, Ricketts, and Sladen Citation2004; Anderson and Goldstein Citation2004; Iglehart Citation2004; Johnston et al Citation2009; Wolfe et al. Citation2013; Mulla and McCracken Citation2014).
Decisions regarding RMS use for a child with UHL should be made on an individual basis. Considerations include the child’s age, the degree and configuration of hearing loss in the poorer hearing ear, whether the child uses personal amplification, and where the RMS will be used (National Workshop on Mild and Unilateral Hearing Loss: Workshop Proceedings 2005; AAA Citation2013; McKay, Gravel, and Tharpe Citation2008). When deciding whether to fit a receiver to the poorer hearing ear, it is important to consider aided speech discrimination ability; if significantly poorer than in the normally hearing ear, it is possible that RMS input to the personal amplification device might not improve outcomes.
Contralateral routing of signal (CROS)
Currently, CROS systems are typically used when no benefit is expected from fitting amplification to the ear with hearing loss. There is limited information about either the efficacy of CROS systems for children or the relative merits of the various options available. Results in children with simulated UHL suggest CROS systems can improve sentence recognition and story comprehension performance in noisy classroom situations, relative to unaided and a remote microphone condition. Benefits of the CROS system over RMS were most apparent for signals originating from the side of a child when the remote microphone stays with a talker located in front of the child (Picou, Lewis, Angley, and Tharpe, Citationin press).
Contralateral routing of signal can be achieved using
a satellite microphone on the ear with hearing loss, coupled to an air-conduction hearing aid worn on the normal hearing ear (‘conventional’ CROS) or
bone conduction to transmit stimuli detected on the side with the UHL to the cochlea of the normally hearing ear. Transcranial CROS fittings use a high-powered air-conduction hearing aid fitted to the ear with hearing loss, such that the amplified signal is transmitted via bone conduction to stimulate the normally hearing cochlea.
Bone-conduction devices can also be used to transmit sounds from the ear with the UHL to the ear with normal hearing. They can be worn on a headband or coupled to a surgically implanted component, but limited data are available on the use of implantable technology in children (Christensen, Richter and Dornhoffer Citation2010).
Considerations when considering CROS fittings include the following.
Inability to localise sound
CROS fittings are unlikely to improve localisation because they do not facilitate the use of binaural hearing.
Inability to hear speech on the side with the UHL
CROS fittings improve detection of speech on the side of the UHL under quiet listening situations, but also enable the presentation of interfering noise to the normal hearing ear when the noise would previously have been attenuated due to head shadow effects in the unaided condition. Therefore, the CROS aid might have an adverse effect in complex listening situations if children are unable to control their device or listening environment, and, for this reason, CROS aids have not previously been recommended for young children (McKay, Gravel, and Tharpe Citation2008).
Unaidable hearing due to poor speech discrimination
If a CROS system is being considered because of poor speech perception in the ear with UHL, a conventional CROS aid is recommended to avoid adverse effects of stimulating that ear via bone conduction. When fitting a conventional CROS system, occlusion of the normal hearing ear by an earmold should be avoided to prevent reduced benefit from natural hearing.
Cochlear implantation
Some children with severe-to-profound UHL and their families might seek hearing restoration of the affected side via cochlear implantation (CI) with the ultimate goal of achieving some level of binaural hearing. Though limited in number, preliminary studies of CI use in children with UHL are encouraging. Investigators have reported that older children with post-lingual onset of UHL wear their devices consistently, and demonstrate that a normal hearing contralateral ear does not prevent device use (Távora-Vieira and Rajan Citation2015; Polonenko, Papsin, and Gordon Citation2017). However, it is worth noting that there are also examples of children with congenital hearing loss and longer periods of auditory deprivation who choose to discontinue device use after implantation (Távora-Vieira and Rajan Citation2015; Sladen et al. Citation2017a; Thomas et al. Citation2017).
Studies of adults and children with post-lingual onset of UHL show that patients demonstrate improved word and sentence recognition on the affected side (Friedman et al. Citation2016; Sladen et al. Citation2017a, Citation2017b; Finke et al. Citation2017), improved localisation on the horizontal plane (Firszt et al. Citation2012; Arndt et al. Citation2015; Dorman et al. Citation2015; Rahne and Plontke Citation2016), and modest improvements in overall speech recognition in noise (Mertens et al. Citation2015; Friedman et al. Citation2016; Rahne and Plontke Citation2016; Sladen et al. Citation2017b; Finke et al. Citation2017). Studies have also used disease-specific measures to demonstrate improvements in HRQoL (Härkonen et al. Citation2015; Sladen et al. Citation2017b; Thomas et al. Citation2017).
See for a listing of hearing technologies available for children with UHL.
Table 2. Hearing technologies for children with unilateral hearing loss.
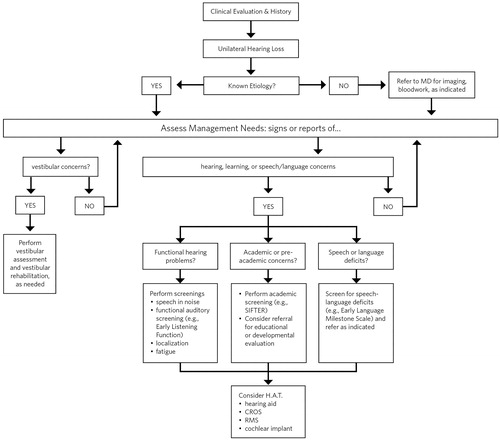
The Committee endorses consideration of these technologies in the context of the child’s and family’s needs and desires. provides a recommended clinical care plan for aiding in management decisions by the audiologist.
Consensus-based principles of information counselling for families
Despite technological progress and enhanced professional understanding of UHL in children and its implications, there remain numerous challenges to effective communication between audiologists and families of these children. This is in large part the result of a lack of management standards for UHL, and in part reflective of the difficulty audiologists face in talking with families about the variety of impacts UHL might have on their children. Services need to be family focussed, allowing for modifications based on unique family-identified concerns, priorities, goals, and desires (Moeller et al. Citation2013). Reactions of families to a hearing loss diagnosis are not necessarily related to the degree of the loss. Parents of children who have UHL can be just as concerned for their child’s future as are parents of a child with a severe or profound bilateral hearing loss. Moreover, families of these children are faced with a variety of intervention options that range from watchful waiting to classroom systems, and surgical as well as non-surgical technology options.
The following are consensus-based considerations on the essential components of effective communication to be included in counselling families of children with UHL:
What are the possible consequences of their child’s hearing loss? Are all children affected the same way?
What are the potential benefits, limitations, and risks of the technology for helping their child’s hearing and communication? What do we know and what do we not know?
Are there other health concerns impacting the child with UHL that will influence success with technology?
What are the consequences of proceeding or not proceeding with a particular technological intervention?
If others will also have to engage with the technology (e.g. an RMS), what support is available to help with this?
If the UHL is known to be progressive, consider how the various technology options are applicable if the hearing changes.
Is it possible for parents to change their minds in the future (e.g. proceed with a surgical versus a non-surgical intervention)?
When and how might the family begin to see a benefit (or a disadvantage) from technology use? Because it can be difficult to observe the impact of a UHL in young children, it is important to help families to have realistic expectations of progress.
Families who choose a ‘watchful waiting’ approach should be equipped with information about key developmental milestones including knowing when and how to act if they are concerned. The use of functional assessment tools such as those listed in can assist in engaging families in the monitoring of their child’s progress.
If device fitting is declined or terminated by a family, ensure that the family is comfortable that they have received enough information to help with their decision and whether other support or information might be needed. For example,
Is the device itself the concern, or the feelings associated with its use?
Are there other factors impacting successful device use (e.g. influential others, bullying)?
What is the cost a concern? Are they considering what to buy and when (e.g. waiting on newer technology) and are there hidden costs such as repairs, spare parts, and compatibility with other technology?
Is the parent able to use the complicated features associated with the technology?
Which HAT features benefit children in which environments and at what age? Ensure that families consider their child’s future needs as well as current concerns, so their decisions will provide the best value for their investment (both time and money).
When is it time to invest in new technology or wait until a future feature or version comes out?
What are the most advantageous and useful features that a particular child in his or her unique setting might need (DesGeorges Citation2015)?
Families receive information from a variety of sources including professionals, other families who have children who are deaf or hard of hearing, adults who are deaf or hard-of-hearing, and written and online information and resources. Audiologists can provide families with information to help them identify reputable online resources and to be aware that because the management of UHL is not clearly defined, they might encounter a variety of opinions about the best options for this type of hearing loss.
Consensus-based priorities for research
Recent systematic reviews have identified that studies characterising the consequences of UHL and evaluating the effectiveness of different management options have included different UHL characteristics (i.e. varying degrees and types of UHL), used different definitions of UHL, and used different outcome measures (Anne, Lieu, and Cohen Citation2017; Appachi et al. Citation2017). This heterogeneity in study design limits our ability to compare and contrast study findings. The following are consensus-based recommendations for further research in children with UHL designed to address treatment uncertainties and promote consistency in research design. These recommendations identify key issues in terms of PICOS (i.e. Participants, Interventions, Comparators, Outcomes, and Study designs/settings).
Participants
Compare yield and accuracy of diagnostic tests
Universal newborn hearing screening (UNHS) has lowered the average age of diagnosis for UHL by several years (Fitzpatrick, Whittingham, and Durieux-Smith Citation2014; Ghogomu, Umansky, and Lieu Citation2014). However, uncertainty remains over how to optimise audiological monitoring or medical evaluations based on known risk factors to detect late-onset or progressive cases of UHL.
Separate reporting of children with UHL
Synthesising evidence across studies is impeded by inconsistent definitions of the participant group such as the combined reporting of outcomes for children with UHL and mild bilateral losses (e.g. Appachi et al. Citation2017). Characteristics and outcomes of children with UHL should be reported separately from children with bilateral losses. Where effects of UHL or management options can be assumed to vary by degree of severity (e.g. Lieu et al. Citation2010), baseline characteristics and outcomes should be stratified into clearly defined categories of severity.
Describe samples/cohorts in detail
Standardised reporting frameworks consistently emphasise the need to report detailed information on sample characteristics (Schulz, Altman, and Moher Citation2010; Von Elm et al. Citation2014). A non-exhaustive list of key information that should be reported includes gender, ear with UHL, age at diagnosis, age at assessment, aetiology, degree of hearing loss in the poorer ear, age at intervention (e.g. HAT fitting), type of intervention, and any changes in intervention. Consideration should be given to self-selection bias in the design of the research and, where possible, an assessment of self-selection bias should be undertaken as part of the research design (Lieu and Dewan Citation2010).
Interventions/comparators
Compare effectiveness of existing and emerging HATs
There remains a lack of high-level evidence for the relative effectiveness of both established and emerging technologies and a paucity of evidence for the effectiveness of contemporary non-surgical interventions. Additional research should determine the effectiveness of these management options, report how the device was fitted, and consider assessing the influence of early versus late fitting.
Determine what degrees of UHL are aidable with conventional hearing aids
At the extremes of UHL are cases where the hearing loss is sufficiently minimal to raise questions about the benefits of aiding (McKay, Gravel, and Tharpe Citation2008) or so severe as to prompt the question as to whether aiding is likely to be appropriate and effective (Arndt et al. Citation2015). Future research should evaluate the effectiveness of HATs at or close to these extremes at a variety of ages (i.e. infants, school-aged children) to establish the points at which using a conventional hearing aid is unnecessary or ineffective.
Outcomes
Ensure consistent selection, measurement, and reporting of outcomes
Outcome measurement and reporting in studies of UHL are highly variable (Anne, Lieu, and Cohen Citation2017; Appachi et al. Citation2017). Research methodologies have been developed to identify what is most important to measure (Williamson et al. Citation2012) and for determining how those important outcomes can be measured (Mokkink et al. Citation2010). Further research should use consensus-based methods that involve clinicians, children with UHL, and the parents of children with UHL to identify the most important domains of the outcome when studying children with UHL and seek international consensus on the choice of measurement tools and instruments.
Determine what a ‘successful’ intervention is and what predicts success
As the impact of UHL can be highly variable across individual children (Reeder, Cadieux, and Firszt Citation2015), so too will be their needs, the choice of optimal intervention, and the desired effects of any intervention. A necessary step in designing studies to evaluate the effectiveness of an intervention is to define clearly what a ‘successful’ outcome is. This definition also needs to account for the smallest change that would be considered clinically meaningful, referred to as the minimal clinically important difference (MCID; Copay et al. Citation2007).
Exploit data logging features of contemporary hearing technologies
Contemporary HATs now include the capability to gather continuous and real-time information on device usage and the characteristics of the acoustic environments to which a child is exposed. Future research should exploit data logging as a tool to characterise the needs of children with UHL based on the environments in which they listen and use HAT.
Study the relationship between behavioural and neuro-imaging outcomes
Recent work has suggested that children with UHL form different connections and activate different neural networks than children with normal hearing (Jung et al. Citation2017). Future research should seek to combine detailed behavioural assessments of the impact of UHL and HATs with measures of central changes that might underpin longer-term effects of cognitive and emotional functioning, or provide predictive markers for the longer-term effects of early intervention.
Study design/setting
Adopt multi-site designs
Single-site studies are more likely to report larger effects than multi-site studies, an effect that can arise because single-site studies tend to have smaller sample sizes, be at greater risk of bias, and recruit more homogeneous samples (Bafeta et al. Citation2012). Multi-site designs should be adopted whenever possible and research teams should consider publishing study protocols either in scientific journals or online databases (e.g. clinicaltrials.gov).
Consider conducting replication studies
Replicating the methodology of key studies should be considered where the research question being answered is important and a limited number of existing studies have been conducted. To assist with replication, all teams conducting interventional research on UHL should ensure that their studies are registered prospectively and comply with established reporting standards (Schulz, Altman, and Moher Citation2010).
Conduct randomised control trials to compare effects of interventions
Using randomisation to determine the choice of intervention for an individual child within a study reduces the influence of selection bias, and allows one to assume that differences in outcomes between groups are likely to be due to the differences in the intervention they received (Akobeng Citation2005). A systematic review of surgical and non-surgical interventions for UHL in children identified no studies that used randomisation (Appachi et al. Citation2017).
Exploit longitudinal study designs to characterise long-term effects of untreated UHL and effects of interventions
Few studies have followed cohorts of children with UHL over long periods of time (Anne, Lieu, and Cohen Citation2017). Future research should consider the use of longitudinal designs to characterise the specific deficits that UHL imposes on a child’s developmental profile.
Leverage a ‘big data’ approach to identify risk factors for UHL
Identifying key risk factors requires access to a wide range of information including the results of audiometric evaluations and medical imaging (Friedman et al. Citation2013), and genetic testing (Dodson et al. Citation2012). The uncertainty around potential risk factors and the numerous potential aetiologies means that a large sample of cases and controls will be necessary to identify key risk factors with a high degree of certainty. Future research should address the identification of these risk factors, and in doing so consider whether existing large-scale population databases (‘biobanks’) could be leveraged and/or extended to address questions related to UHL.
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
Acknowledgements
The Consensus Committee thanks those who contributed to this endeavour by their participation and engagement in the UHL Conference on October 24 and 25, 2017. The Committee also acknowledges with gratitude the support of Angela Pelosi, Evert Dijkstra, Stacey Rich, and Phonak AG as a whole for their logistical and financial support of this conference and document development.
Disclosure statement
M. Bagatto, J. DesGeorges, D. Lewis, P. Roush, and A. M. Tharpe serve on the Pediatric Research Advisory Board for Phonak AG.
Additional information
Funding
Notes
1 For purposes of this document, normal hearing refers to an ear that is audiologically normal to near normal, not requiring audiologic intervention.
2 Although commonly referred to as bone-anchored hearing aids (BAHA), Cochlear Corporation now holds a trademark on that term for their specific devices. For purposes of this document, the term for this class of device is bone-conduction devices.
3 Profound unilateral hearing loss has been referred to as single-sided deafness, which is a non-audiologic term that emerged in recent years (Cire Citation2017). For purposes of this guideline, the term profound unilateral hearing loss is used.
References
- Akobeng, A. K. 2005. “Understanding Randomized Controlled Trials.” Archives of Disease in Childhood 90 (8): 840–844. doi:10.1136/adc.2004.058222.
- AAA (American Academy of Audiology). 2013. Clinical Practice Guidelines: Pediatric Amplification. Accessed 1 August 2018. http://www.audiology.org/sites/default/files/publications/PediatricAmplificationGuidelines.pdf
- AAA (American Academy of Audiology). 2011a. Clinical Practice Guidelines: Remote Microphone Hearing Assistance Technologies for Children and Youth from Birth to 21 Years and Supplement A: Fitting and Verification Procedures for Ear-Level FM. Accessed 1 August 2018. http://audiology-web.s3.amazonaws.com/migrated/HAT_Guidelines_Supplement_A.pdf_53996ef7758497.54419000.pdf
- AAA (American Academy of Audiology). 2011b. Clinical Practice Guidelines: Remote Microphone Hearing Assistance Technologies for Children and Youth from Birth to 21 Years. Supplement B: Classroom Audio Distribution Systems-Selection and Verification. Accessed 1 August 2018. http://audiology-web.s3.amazonaws.com/migrated/20110926_HAT_GuidelinesSupp_B.pdf_53996ef98259f2.45364934.pdf
- AAA (American Academy of Audiology). 2012. Audiologic Guidelines for the Assessment of Hearing in Infants and Young Children. Accessed 1 August 2018. https://audiology-web.s3.amazonaws.com/migrated/201208_AudGuideAssessHear_youth.pdf_5399751b249593.36017703.pdf
- AAP (American Academy of Pediatrics). 2003. “Hearing Assessment in Infants and Children: Recommendation beyond Neonatal Screening.” Pediatrics 3 (2): 436–440.
- AAP (American Academy of Pediatrics). 2007. “Joint Committee on Infant Hearing Year 2007 Position Statement: Principles and Guidelines for Early Hearing Detection and Intervention Programs.” Pediatrics 120 (4): 898–921.
- AAP (American Academy of Pediatrics). 2013. Supplement to the JCIH 2007 Position Statement: Principles and guidelines for early intervention following confirmation that a child is deaf or hard of hearing. doi:10.1044/policy.et2013-00339.
- American Speech-Language-Hearing Association 2004. Guidelines for the audiologic assessment of children from birth to 5 years of age [Guidelines]. Accessed 30 August 2019. www.asha.org/members/deskref-journals/deskref/default
- Anderson, K. L. 1989. SIFTER: Screening Identification For Targeting Educational Risk In Children Identified by Hearing Screening or Who Have Known Hearing Loss User’s Manual, The Educational Audiology Association. Accessed 29 July 2018. https://msu.edu/course/asc/823e/casby/screening/sifter.pdf
- Anderson, K. L. 2002. Early Listening Function (ELF). Accessed 29 July 2018. http://home.earthlink.net/∼karenlanderson/ELF.html
- Anderson, K., and H. Goldstein. 2004. “Speech Perception Benefits of FM and Infrared Devices to Children with Hearing Aids in a Typical Classroom.” Language, Speech, and Hearing Services in Schools 35: 169–184. doi:10.1044/0161-1461(2004/017).
- Anderson, K., and N. Matkin. 1996. Screening Instrument for Targeting Educational Risk in Preschool Children (S.I.F.T.E.R.). Accessed 29 July 2018. https://successforkidswithhearingloss.com/wp-content/uploads/2014/09/1.k.-Preschool_SIFTER_fillable.pdf
- Anderson, K., and J. J. Smaldino. 2011. Children’s Home Inventory for Listening Difficulties (C.H.I.L.D.). Accessed 29 July 2018. http://www.http://home.earthlink.net/∼karenlanderson/child.html
- Anderson, K., J. J. Smaldino, and C. Spangler. 2011. Listening Inventory for Education – Revised (L.I.F.E. – R) Accessed 29 July 2018. https://successforkidswithhearingloss.com/wp-content/uploads/2011/08/LIFE-R.pdf
- Anne, S., J. E. Lieu, and M. S. Cohen. 2017. “Speech and Language Consequences of Unilateral Hearing Loss: A Systematic Review.” Otolaryngology–Head and Neck Surgery 157 (4): 572–579. doi:10.1177/0194599817726326.
- Arndt, S., S. Prosse, R. Laszig, T. Wesarg, A. Aschendorff, and F. Hassepass. 2015. “Cochlear Implantation in Children with Single-Sided Deafness: Does Aetiology and Duration of Deafness Matter?” Audiology and Neurotology 20 (1): 21–30. doi:10.1159/000380744.
- Appachi, S., J. L. Specht, N. Raol, J. E. Lieu, M. S. Cohen, K. Dedhia, and S. Anne. 2017. “Auditory Outcomes with Hearing Rehabilitation in Children with Unilateral Hearing Loss: A Systematic Review.” Otolaryngology–Head and Neck Surgery 157 (4): 565–571. doi:10.1177/0194599817726757.
- Bafeta, A., A. Dechartres, L. Trinquart, A. Yavchitz, I. Boutron, and P. Ravaud. 2012. “Impact of Single Centre Status on Estimates of Intervention Effects in Trials with Continuous Outcomes: Meta-Epidemiological Study.” Bmj 344 (1): e813. doi:10.1136/bmj.e813.
- Bagatto, M., P, and A. M. Tharpe. 2014. Decision Support Guide for Hearing Aid Use in Infants and Children with Minimal/Mild Bilateral Hearing Loss. Proceedings of the Sixth International Conference: A Sound Foundation through Early Amplification, Stäfa, Switzerland, Phonak AG.
- Besing, J., and J. Koehnke. 1995. “A Test of Virtual Auditory Localization.” Ear and Hearing 16 (2): 220–229.
- Bess, F. H., J. Dodd-Murphy, and R. A. Parker. 1998. “Children with Minimal Sensorineural Hearing Loss: Prevalence, Educational Performance, and Functional Status.” Ear and Hearing 19 (5): 339–354. doi:10.1097/00003446-199810000-00001.
- Bess, F., and A. M. Tharpe. 1986. “Case History Data on Unilaterally Hearing-Impaired Children.” Ear and Hearing 7 (1): 14–19.
- Bess, F. H., A. M. Tharpe, and A. M. Gibler. 1986. “Auditory Performance of Children with Unilateral Sensorineural Hearing Loss.” Ear and Hearing 7 (1): 20–26. doi:10.1097/00003446-198602000-00005.
- Bovo, R., A. Martini, M. Agnoletto, A. Beghi, D. Carmignoto, M. Milani, and A. M. Zangaglia. 1988. “Auditory and Academic Performance of Children with Unilateral Hearing Loss.” Scandinavian Audiology Supplement 30: 71–74.
- Ching, T., and M. Hill. 2005. Parents’ Evaluation of Aural/Oral Performance of Children (P.E.A.C.H.). Accessed 13 February 2018. https://outcomes.nal.gov.au/Assesments_Resources/PEACH%20ratings%20with%20coverpage%20260509.pdf
- Christensen, L., G. T. Richter, and J. L. Dornhoffer. 2010. “Update on Bpone-Anchored Hearing Aids in Pediatric Patients with Profound Unilateral Sensoirneural Hearing Loss.” Archives of Otolaryngology Head and Neck Surgery 136 (2): 175–177. doi:10.1001/archoto.2009.203.
- Cire, G. 2017. “Understanding Single Sided Deafness: Evaluation and Treatment for Professionals. Course Presented on.” AudiologyOnline.
- Copay, A. G., B. R. Subach, S. D. Glassman, D. W. Polly, and T. C. Schuler. 2007. “Understanding the Minimum Clinically Important Difference: A Review of Concepts and Methods.” The Spine Journal 7 (5): 541–546. doi:10.1016/j.spinee.2007.01.008.
- DesGeorges, J. 2015. Impact of Multiple Technologies, Proceedings of the Seventh International Conference: A Sound Foundation through Early Amplification, Stäfa, Switzerland, Phonak AG.
- Dodson, K. M., A. Georgolios, N. Barr, B. Nguyen, A. Sismanis, K. S. Arnos, V. W. Norris, D. Chapman, W. E. Nance, and A. Pandya. 2012. “Etiology of Unilateral Hearing Loss in a National Hereditary Deafness Repository.” American Journal of Otolaryngology 33 (5): 590–594. doi:10.1016/j.amjoto.2012.03.005.
- Dorman, M. F., D. Zeitler, S. J. Cook, L. Loiselle, W. A. Yost, G. B. Wanna, and R. H. Gifford. 2015. “Interaural Level Difference Cues Determine Sound Source Localization by Single-Sided Deaf Patients Fit with a Cochlear Implant.” Audiology and Neurotology 20 (3): 183–188. doi:10.1159/000375394.
- Ead, B., S. Hale, D. DeAlwis, and J. E. C. Lieu. 2013. “Pilot Study of Cognition in Children with Unilateral Hearing Loss.” International Journal of Pediatric Otorhinolaryngology 77 (11): 1856–1860. doi:10.1016/j.ijporl.2013.08.028.
- Finke, M., A. Strauß-Schier, E. Kludt, A. Büchner, and A. Illg. 2017. “Speech Intelligibility and Subjective Benefit in Single-Sided Deaf Adults after Cochlear Implantation.” Hearing Research 348: 112–119. doi:10.1016/j.heares.2017.03.002.
- Firszt, J. B., L. K. Holden, R. M. Reeder, S. B. Waltzman, and S. Arndt. 2012. “Auditory Abilities after Cochlear Implantation in Adults with Unilateral Deafness.”Otology & Neurotology 33 (8): 1339–1346. doi:10.1097/MAO.0b013e318268d52d.
- Fitzpatrick, E. M., R. S. Al-Essa, J. Whittingham, and J. Fitzpatrick. 2017. “Characteristics of Children with Unilateral Hearing Loss.” International Journal of Audiology 56 (11): 819–828. doi:10.1080/14992027.2017.1337938.
- Fitzpatrick, E. M., J. Whittingham, and A. Durieux-Smith. 2014. “Mild Bilateral and Unilateral Hearing Loss in Childhood: A 20-Year View of Hearing Characteristics, and Audiologic Practices before and after Newborn Hearing Screening.” Ear and Hearing 35 (1): 10–18. doi:10.1097/AUD.0b013e31829e1ed9.
- Fowler, K. B. 2013. “Congenital Cytomegalovirus Infection: Audiologic Outcome.” Clinical Infectious Diseases 57 (suppl_4): S182–S184. https://doi-org.libproxy.lib.unc.edu/10.1093/cid/cit609.
- Friedman, D. R., O. H. Ahmed, S. O. McMenomey, W. H. Shapiro, S. B. Waltzman, and J. T. Roland. 2016. “Single-Sided Deafness Cochlear Implantation.” Otology & Neurotology 37 (2): 154–160. doi:10.1097/MAO.0000000000000951.
- Friedman, A. B., R. Guillory, R. H. Ramakrishnaiah, R. Frank, M. B. Gluth, G. T. Richter, and J. L. Dornhoffer. 2013. “Risk Analysis of Unilateral Severe-to-Profound Sensorineural Hearing Loss in Children.” International Journal of Pediatric Otorhinolaryngology 77 (7): 1128–1131. doi:10.1016/j.ijporl.2013.04.016.
- Galvin, K. L., and W. Noble. 2013. “The Speech, Spatial and Qualities of Hearing Scale for Use with Children, Parents, and Teachers.” Cochlear Implants International 14 (3): 135–141. doi:10.1179/1754762812Y.0000000014.
- Ghogomu, N., A. Umansky, and J. E. Lieu. 2014. “Epidemiology of Unilateral Sensorineural Hearing Loss with Universal Newborn Hearing Screening.” The Laryngoscope 124 (1): 295–300. doi:10.1002/lary.24059.
- Grimshaw, S. 1996. The Extraction of Listening Situations which are Relevant to Young Children, and the Perception of Normal-hearing Subjects of the Degree of Difficulty Experienced by the Hearing Impaired in Different Types of Listening Situations. Nottingham: MRC Institute of Hearing Research.
- Haffey, T., N. Fowler, and S. Anne. 2013. “Evaluation of Unilateral Sensorineural Hearing Loss in the Pediatric Patient.” International Journal of Pediatric Otorhinolaryngology 77 (6): 955–958. doi:10.1016/j.ijporl.2013.03.015.
- Härkonen, K., I. Kivekäs, M. Rautiainen, V. Kotti, V. Sivonen, and J. Vasama. 2015. “Single-Sided Deafness: The Effect of Cochlear Implantation on Quality of Life, Quality of Hearing, and Working Performance.” Orl 77 (6): 339–345. doi:10.1159/000439176.
- Hartvig Jensen, J., P. Johansen, and S. Borre. 1989. “Unilateral Sensorineural Hearing Loss in Children and Auditory Performance with respect to Right/Left Ear Differences.” British Journal of Audiology 23 (3): 207–213. doi:10.3109/03005368909076501.
- Hayes, D. E., and J. M. Chen. 1998. “Bone-Conduction Amplification with Completely-in-the-Canal Hearing Aids.” Journal of American Academy of Audiology 9: 59–66.
- Hol, M. K. S., S. J. W. Kunst, A. F. M. Snik, and C. W. R. J. Cremers. 2010. “Pilot Study on the Effectiveness of the Conventional CROS, the Transcranial CROS and the BAHA Transcranial CROS in Adults with Unilateral Inner Ear Deafness.” European Archives of Oto-Rhino-Laryngology 267 (6): 889. doi:10.1007/s00405-009-1147-9.
- Humes, L. E., S. K. Allen, and F. H. Bess. 1980. “Horizontal Sound Localization Skills of Unilaterally Hearing-Impaired Children.” International Journal of Audiology 19 (6): 508518. doi:10.3109/00206098009070082.
- Iglehart, F. 2004. “Speech Perception by Students with Cochlear Implants Using Sound-Field Systems in Classrooms.” American Journal of Audiology 13 (1): 62–72. doi:10.1044/1059-0889(2004/009).
- Johnston, Kristin N., Andrew B. John, Nicole V. Kreisman, James W. Hall, Carl C. Crandell, Kristin N. Johnston, Andrew B. John, Nicole V. Kreisman, James W. Hall, and Carl C. Crandell. 2009. “Multiple Benefits of Personal FM System Use by Children with Auditory Processing Disorder (APD).” International Journal of Audiology 48 (6): 371–383. doi:10.1080/14992020802687516.
- Johnstone, P. M., A. K. Nabelek, and V. S. Robertson. 2010. “Sound Localization Acuity in Children with Unilateral Hearing Loss Who Wear a Hearing Aid in the Impaired Ear.” Journal of the American Academy of Audiology 218: 522–534. doi:10.3766/jaaa.21.8.4.
- Jung, M. E., M. Colletta, R. Coalson, B. L. Schlaggar, and J. E. Lieu. 2017. “Differences in Interregional Brain Connectivity in Children with Unilateral Hearing Loss.” The Laryngoscope 127 (11): 2636–2645. doi:10.1002/lary.26587.
- Kenworthy, O. T., T. Klee, and A. M. Tharpe. 1990. “Speech Recognition Ability of Children with Unilateral Sensorineural Hearing Loss as a Function of Amplification, Speech Stimuli and Listening Condition.” Ear and Hearing 11 (4): 264–274. doi:10.1097/00003446-199008000-00003.
- Kishon-Rabin, Liat, Jacob Kuint, Minka Hildesheimer, and Daphne Ari-Even Roth. 2015. “Delay in Auditory Behaviour and Preverbal Vocalization in Infants with Unilateral Hearing Loss.” Developmental Medicine & Child Neurology 57 (12): 1129–1136.
- Kuhn-Inacker, H., V. Weichbold, L. Tsiakpini, F. Corinx, and P. D’Haese. 2003. LittEARS auditory questionnaire. Innsbrook, Austria: .Med-El.
- Lieu, J. E. 2004. “Speech-Language and Educational Consequences of Unilateral Hearing Loss in Children.” Archives of Otolaryngology–Head & Neck Surgery 130 (5): 524–530. doi:10.1001/archotol.130.5.524.
- Lieu, J. E. 2013. “Unilateral Hearing Loss in Children: Speech-Language and School Performance.” B-Ent Suppl. (21): 107–115.
- Lieu, J. E., and K. Dewan. 2010. “Assessment of Self-Selection Bias in a Pediatric Unilateral Hearing Loss Study.” Otolaryngology–Head and Neck Surgery 142 (3): 427–433. doi:10.1016/j.otohns.2009.11.035.
- Lieu, J. E., N. Tye-Murray, R. K. Karzon, and J. F. Piccirillo. 2010. “Unilateral Hearing Loss Is Associated with Worse Speech-Language Scores in Children.” Pediatrics 125 (6): e1348–e1355. doi:10.1542/peds.2009-2448.
- Liming, Bryan J., John Carter, Alan Cheng, Daniel Choo, John Curotta, Daniela Carvalho, John A. Germiller, et al. 2016. “International Pediatric Otolaryngology Group (IPOG) Consensus Recommendations: Hearing Loss in the Pediatric Patient.” International Journal of Pediatric Otorhinolaryngology 90: 251. doi:10.1016/j.ijporl.2016.09.016.
- Masuda, S., S. Usui, and T. Matsunaga. 2013. “High Prevalence of Inner-Ear and/or Internal Auditory Canal Malformations in Children with Unilateral Sensorineural Hearing Loss.” International Journal of Pediatric Otorhinolaryngology 77 (2): 228–232. doi:10.1016/j.ijporl.2012.11.001.
- McKay, S., J. S. Gravel, and A. M. Tharpe. 2008. “Amplification Considerations for Children with Minimal or Mild Bilateral Hearing Loss and Unilateral Hearing Loss.” Trends in Amplification 12 (1): 43–54. doi:10.1177/1084713807313570.
- Mertens, G., A. K. Punte, M. D. Bodt, and P. V. Heyning. 2015. “Binaural Auditory Outcomes in Patients with Postlingual Profound Unilateral Hearing Loss: 3 Years after Cochlear Implantation.” Audiology and Neurotology 20 (1): 67–72. doi:10.1159/000380751.
- Ministry of Children, Community and Social Services. 2018. Protocol for auditory brainstem response-based audiological assessment (ABRA), 2018.01, Ontario Infant Hearing Program.
- Mokkink, L. B., C. B. Terwee, D. L. Patrick, J. Alonso, P. W. Stratford, D. L. Knol, L. M. Bouter, and H. C. De Vet. 2010. “The COSMIN Checklist for Assessing the Methodological Quality of Studies on Measurement Properties of Health Status Measurement Instruments: An International Delphi Study.” Quality of Life Research 19 (4): 539–549. doi:10.1007/s11136-010-9606-8.
- Moeller, M. P., G. Carr, L. Seaver, A. Stredler-Brown, and D. Holzinger. 2013. “Best Practices in Family-Centered Early Intervention for Children Who Are Deaf or Hard of Hearing: An International Consensus Statement.”Journal of Deaf Studies and Deaf Education 18 (4): 429. doi:10.1093/deafed/ent034.
- Moeller, M. P., K. Donaghy, K. Beauchaine, D. Lewis, and P. Stelmachowicz. 1996. “Longitudinal Study of FM System Use in Non-Academic Settings: Effects on Language Development.” Ear and Hearing 17 (1): 28–41. doi:10.1097/00003446-199602000-00004.
- Mulla, I., and W. McCracken. 2014. “The Use of FM Technology for Pre-School Children with Hearing Loss.” In J. Northern (Ed.), A sound foundation through early amplification 2013: Proceedings of the sixth international conference, 71–76. Stäfa, Switzerland: Phonak AG.
- Ministry of Children, Community and Social Services. 2018. Protocol for auditory brainstem response-based audiological assessment (ABRA), 2018.01, Ontario Infant Hearing Program.
- National Workshop on National Mild and Unilateral Hearing Loss: Workshop Proceedings. Breckinridge, CO: Centers for Disease Control and Prevention, 2005.
- Paul, A. 2017. “Unilateral Sensorineural Hearing Loss: Medical Context and Etiology.” Audiology and Neurotology 22: 83–88. doi:10.1159/000474928.
- Pittman, A., D. Lewi, B. Hoover, and P. Stelmachowicz. 1999. “Recognition Performance for Four Combinations of FM System and Hearing Aid Microphone Signals in Adverse Listening Conditions.” Ear and Hearing 20 (4): 279–289. doi:10.1097/00003446-199908000-00001.
- Picou, E. M., Lewis, D., Angley, G., Tharpe, A. M. (in press). Re-routing Hearing Aid Systems for Overcoming Simulated Limited Useable Unilateral Hearing in Dynamic Listening Situations. Ear and Hearing.
- Polonenko, M. J., B. C. Papsin, and K. A. Gordon. 2017. “Children with Single-Sided Deafness Use Their Cochlear Implant.” Ear and Hearing 38 (6): 681–689. doi:10.1097/AUD.0000000000000452.
- Purdy, Suzanne C., Denise R. Farrington, Carolyn A. Moran, Linda L. Chard, and Shirley-Anne Hodgson. 2002. “A Parental Questionnaire to Evaluate Childrens Auditory Behavior in Everyday Life (ABEL).” American Journal of Audiology 11 (2): 72. doi:10.1044/1059-0889(2002/010).
- Rahne, T., and S. K. Plontke. 2016. “Functional Result after Cochlear Implantation in Children and Adults with Single-Sided Deafness.” Otology & Neurotology 37 (9): 332–340. doi:10.1097/MAO.0000000000000971.
- Reeder, R. M., J. Cadieux, and J. B. Firszt. 2015. “Quantification of Speech-in-Noise and Sound Localization Abilities in Children with Unilateral Hearing Loss and Comparison to Normal Hearing Peers.” Audiology and Neurotology 20 (1): 31–37. doi:10.1159/000380745.
- Ruscetta, Melissa N., Ellis M. Arjmand, and Sheila R. Pratt. 2005. “Speech Recognition Abilities in Noise for Children with Severe-to-Profound Unilateral Hearing Impairment.” International Journal of Pediatric Otorhinolaryngology 69 (6): 771–779. doi:10.1016/j.ijporl.2005.01.010.
- Schulz, K. F., D. G. Altman, and D. Moher. 2010. “CONSORT 2010 Statement: Updated Guidelines for Reporting Parallel Group Randomised Trials.” BMC Medicine 8 (1): 18. doi:10.1186/1741-7015-8-18.
- Shargorodsky, J., S. G. Cerhan, G. C. Curhan, and R. Eavey. 2010. “Change in Prevalence of Hearing Loss in US Adolescents.” Jama 304 (7): 772–778. doi:10.1001/jama.2010.1124.
- Sladen, Douglas P., Matthew L. Carlson, Brittany P. Dowling, Amy P. Olund, Kathryn Teece, Melissa D. DeJong, Alyce Breneman, et al. 2017a. “Early Outcomes after Cochlear Implantation for Adults and Children with Unilateral Hearing Loss.” The Laryngoscope 127 (7): 1683–1688. doi:10.1002/lary.26337.
- Sladen, D. P., C. D. Frisch, M. L. Carlson, C. L. Driscoll, J. H. Torres, and D. M. Zeitler. 2017b. “Cochlear Implantation for Single-Sided Deafness: A Multicenter Study.” The Laryngoscope 127 (1): 223–228. doi:10.1002/lary.26102.
- Távora-Vieira, D., and G. P. Rajan. 2015. “Cochlear Implantation in Children with Congenital and Noncongenital Unilateral Deafness: A Case Series.” Otology & Neurotology 36 (8): 1457–1458. doi:10.1097/MAO.0000000000000806.
- Tharpe, A. M. 2008. “Unilateral and Mild Bilateral Hearing Loss in Children: Past and Current Perspectives.” Trends in Amplification 12 (1): 7–15. doi:10.1177/1084713807304668.
- Tharpe, A. M., T. Ricketts, and D. P. Sladen. 2004. FM systems for children with minimal to mild hearing loss, In: D. Fabry & C.D. Johnson (Eds.), Access Conference Proceedings.
- Thomas, J. P., K. Neumann, S. Dazert, and C. Voelter. 2017. “Cochlear Implantation in Children with Congenital Single-Sided Deafness.” Otology & Neurotology 38 (4): 496–503. doi:10.1097/MAO.0000000000001343.
- Updike, C. D. 1994. “Comparison of FM Auditory Trainers, CROS Aids and Personal Amplification in Unilaterally Hearing Impaired Children.” The Journal of American Academy of Audiology 5 (3): 204–209.
- Valente, M., L. G. Potts, M. Valente, and J. Goebel. 1995. “Wireless CROS versus Transcranial CROS for Unilateral Hearing Loss.” American Journal of Audiology 4 (1): 52–59. doi:10.1044/1059-0889.0401.52.
- Van Beeck Calkoen, E. A., E. Sanchez Aliaga, P. Merkus, C. F. Smit, J. M. van de Kamp, M. F. Mulder, S. T. Goverts, and E. F. Hensen. 2017. “High Prevalence of Abnormalities on CT and MR Imaging in Children with Unilateral Sensorineural Hearing Loss Irrespective of Age or Degree of Hearing Loss.” International Journal of Pediatric Otorhinolaryngology 97 (97): 185–191. doi:10.1016/j.ijporl.2017.04.002.
- Von Elm, E., D. G. Altman, M. Egger, S. J. Pocock, P. C. Gøtzsche, and J. P. Vandenbroucke. 2014. “The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies.” International Journal of Surgery 12 (12): 1495–1499. doi:10.1016/j.ijsu.2014.07.013.
- Williamson, P. R., D. G. Altman, J. M. Blazeby, M. Clarke, D. Devane, E. Gargon, and P. Tugwell. 2012. “Developing Core Outcome Sets for Clinical Trials: Issues to Consider.” Trials 13 (1): 132. doi:10.1186/1745-6215-13-132.
- Wolfe, J., D. Lewis, and L. Eiten. 2016. “Remote Microphone Systems and Communication Access for Children.” In Comprehensive Handbook of Pediatric Audiology, edited by A. M. Tharpe & R. Seewald, 2nd ed., 677–711. San Diego: Plural Publishing.
- Wolfe, J., M. Morais, S. Neumann, E. Schafer, H. E. Mülder, N. Wells, and M. Hudson. 2013. “Evaluation of Speech Recognition with Personal FM and Classroom Audio Distribution Systems.” Journal of Educational Audiology 19: 65–79.
- Wolter, Nikolaus E., Sharon L. Cushing, Luis D. Vilchez-Madrigal, Adrian L. James, Jennifer Campos, Blake C. Papsin, and Karen A. Gordon. 2016. “Unilateral Hearing Loss Is Associated with Impaired Balance in Children: A Pilot Study.”Otology and Neurotology 37 (10): 15891.