Abstract
Objective
To evaluate uptake of the internet-based hearing test, with respect to the 11% of UK adults that have hearing loss but do not use hearing aids.
Design
Feasibility study in a primary care practice in the North of England.
Study Sample
Adults aged 50–74 years were sent postal invitations to complete an internet hearing test (N = 600). Those who completed the test, those who failed (>35 dB HL in the better ear) and demographic correlates (age, gender, ethnicity and socioeconomic level) were recorded.
Results
11.2% of invited adults completed the hearing test and 7.7% failed it. Those who took the test tended to have a higher socioeconomic background than those who did not. There were no differences in age, ethnicity or gender between those who took the test and those who did not.
Conclusions
An estimated 70% (7.7%/11.0%) of adults with hearing loss but who do not use hearing aids took the test. Uptake was equitable across most demographic categories. Uptake was high among a study sample that was substantially more deprived than the general UK population. Internet-based hearing testing offers an efficient paradigm for identifying hearing loss.
Introduction
Hearing loss is the leading cause of years lived with disability in the United Kingdom (UK) (World Health Organization Citation2018). One in six people in the UK has an audiometric hearing loss, increasing to one in five by 2035 (Action on Hearing Loss, Citation2015). Hearing loss is more prevalent and rates of hearing aid use lower among people from more deprived socioeconomic backgrounds and those from ethnic minority groups in the UK (Dawes et al. Citation2014; Sawyer et al. Citation2019; Scholes et al. Citation2018). Hearing loss is associated with a range of negative outcomes including communication difficulties, depression, social isolation, cognitive decline, under- and un-employment (Chia et al. Citation2007; Maharani et al. Citation2018; Strawbridge et al. Citation2000).
Hearing aids are the primary method for management and are effective in reducing the impacts of hearing loss (Ferguson et al. Citation2017). Davis et al. (Citation2007) identified that 14% of UK adults aged 55–74 had an audiometric hearing loss >35 dB HL in the better ear (the level of hearing impairment at which people are likely to use and benefit from a hearing aid), but only 1 in 5 of those with that degree of hearing loss use a hearing aid. Those who do use a hearing aid typically lived with hearing impairment for around 15 years before seeking help (Davis et al. Citation2007), further increasing the years of healthy life lost.
Adult hearing screening has the potential to reduce the burden of hearing loss by increasing rates of hearing aid use and promoting use at an earlier age. Davis et al. (Citation2007) reported that systematic hearing screening (personal postal invitations) had higher uptake and coverage than opportunistic screening (notices in doctors’ waiting rooms. “Uptake” refers to the proportion of people who accept the offer of screening and take the opportunity to check their hearing. Over 90% of UK adults surveyed reported that hearing screening would be acceptable, particularly if screening was linked to their general medical practitioner (GP). Davis et al.’s modelling suggested that the degree of hearing loss predicted hearing aid use and benefit, and that at <35 dB HL, 95% of people accepted hearing aids following screening and used them long-term. Davis et al. recommended targeting those aged 55–74 years as this would identify those who are currently not likely to self-refer for hearing care, and where additional benefits from earlier identification and treatment of hearing loss could be realised (i.e. by around 10 years earlier than the current average age of first hearing aid fitting).
Hearing tests can now be automated and delivered over the internet, facilitating low cost, high volume, reliable hearing assessment (Potgieter et al. Citation2015; Smits, Kapteyn, and Houtgast Citation2004; Watson et al. Citation2012). Internet-based hearing testing offers a promising model for systematic screening because internet access and smartphone ownership are high. In 2019, 87% of UK adults reported that they access the internet and 79% own a smartphone (Office of Communications Citation2019). Internet-based hearing tests may avoid barriers to in-person hearing testing by eliminating the need to travel or take time off work to attend a clinic. Internet-based hearing assessment accords with the NHS long-term plan of using digital innovations, technology-supported self-management and remote care to better support people with long-term conditions and reduce health inequalities (Department of Health Citation2005; NHS England and NHS Improvement Citation2020).
We aimed to estimate (i) the rate of uptake and (ii) the proportion of those who take the screening that likely have hearing loss >35 dB HL in the better ear for an internet-based systematic hearing screening sent to UK adults aged 50–74 via a primary care practice.
Methods
Setting and participants
The study took place in a single large, diverse and socioeconomically deprived general medical (GP) practice in South Manchester, UK. Eligible persons were randomly selected using trial randomisation software from patient databases in the practice and invited to participate. Inclusion criteria were women and men aged between 50 and 75 years old who were not known to be deaf, existing hearing aid or cochlear implant users based on READ coded information in their GP medical records. READ is the UK diagnosis coding system developed by Dr. James Read in the early 1980s and used by the participating GP practice at the time of the study.
The study was powered to detect likely rates of uptake based on evaluations of similar recent GP-based health screening programs in the UK (Hazell et al. Citation2008; McRonald et al. Citation2014). Based on an uptake rate of 20%, a sample size of at least 246 would be required to estimate the proportion of adults who take up the offer of the internet-delivered hearing test to a degree of precision such that the 95% confidence interval has a width of ±5%. To facilitate investigation of demographics of uptake, 600 adults were invited to participate.
As a requirement of informed consent for research participation, participants were informed that “this is part of a research study looking at the use of an online hearing check”, the aim being “to find out how many people would try an online hearing check”. The study was granted ethical approval by the West Midlands-Solihull National Research Ethics Service Committee (IRAS ID 257098).
Internet-delivered hearing test
The internet-delivered hearing test can be accessed via smartphone, tablet or computer. The hearing test was based on the Digits in Noise test (DIN) and involved identifying digits spoken in background noise (Smits, Kapteyn, and Houtgast Citation2004). Versions of the DIN for telephone and internet-based adult hearing screening have been implemented in the Netherlands, United Kingdom, Australia, Poland, Switzerland, Germany, France and the USA (Watson et al. Citation2012). Performance on the DIN is strongly correlated with audiometric hearing thresholds for sensorineural hearing loss (Smits and Houtgast Citation2005). The version of the DIN test used in this study was that used in the UK Biobank biomedical research resource (https://www.ukbiobank.ac.uk/). The UK Biobank DIN was developed at the University of Southampton (Hall Citation2006). The DIN is described elsewhere (http://biobank.ctsu.ox.ac.uk/crystal/label.cgi?id=100049). Participants were asked to take the test using their own set of headphones and smartphone/tablet/computer device, and in a quiet room free of distractions. Fifteen sets of three monosyllabic digits (e.g. 1-5-8) were presented monaurally in a background of noise with each ear tested separately. Participants keyed in the digits they had heard using their computer keyboard, mouse or phone keypad. The level of the digits varied adaptively after each triplet to estimate the signal-to-noise ratio at which 50% of digits were correctly recognised. Testing took around 4 minutes. Performance was categorised as pass or fail based on a recognition threshold corresponding to a 35 dB HL hearing threshold over 0.5–4 kHz in the better ear. A 35 dB HL criterion was chosen because those with hearing loss >35 dB HL are likely to accept, use and benefit from a hearing aid in the long term (Davis et al. Citation2007). The DIN test had 90% sensitivity and 83% specificity for the 35 dB HL hearing level, based on data from 85 adults aged over 60 years from an unpublished study (). Participants were given feedback on whether they had passed or failed the test.
For those who passed, feedback was “Your score suggests hearing in the normal range. If you ever have any concerns about your hearing in future, please speak to your doctor. If you would like to find out more about hearing health, please visit https://www.nhs.uk/conditions/hearing-loss/”. For those who failed, feedback was “You may have a hearing problem. If you have any concerns about your hearing, please speak to your doctor. To make an appointment: (name, address and contact details of the participating GP). If you would like to find out more about hearing health, please visit https://www.nhs.uk/conditions/hearing-loss/”. The GP was able to refer the patient for a full audiometric evaluation and management.
Demographic data
Pseudo-anonymised data were extracted from GP patient databases on key demographic parameters including age, gender, ethnicity, number of GP visits in the previous year and partial (to preserve anonymity) postcode. Postcode data were limited to postal sector (e.g. a postcode of M16 0RA is represented as M16 0). The partial postcodes were used to derive a proxy indicator of socioeconomic status, using the Townsend Index (Norman Citation2010). Lower Townsend scores represent more affluent areas. Ethnicity was coded according to UK census categories.
Patient and public involvement
Seven adults who were members of patient advisory panels were consulted for feedback on the wording and content of the cover letter from the GP inviting participants to take the hearing screening and the participant information sheets.
Procedure
Potential participants meeting inclusion criteria were randomly selected from patient registers by the participating GP surgery using trial randomisation software and sent a written postal invitation to participate along with a participant information sheet. The invitation contained a link to the internet-delivered hearing test and a unique participant identification number that participants entered when they took the hearing test. The unique identifier ensured each person only completed the test once and allowed test-takers to be matched to de-identified demographic data extracted from patient records. Participants who had not completed the internet-delivered test within 2 weeks of sending the initial invitation letter were sent a reminder letter.
Statistical analysis
The percentage of people completing the internet-delivered hearing test, and how many were identified as having a hearing loss were calculated along with 95% confidence intervals. Information on differences in uptake according to age, gender, socioeconomic status and ethnicity according to responders and non-responders were tested using t-tests or chi-square tests as appropriate.
Results
In the study sample of n = 600, 11.2% (67 people; 95% confidence interval 8.8–14.0%) completed the on-line hearing test (). Of those who took the test, 68.6% (46 people, or 7.7% of the study sample; 95% confidence interval 56.2–79.4%) failed the test. The 7.7% of people who took and failed the hearing test compares favourably to the estimated 11% of UK adults aged 50–74 years who have a hearing loss but do not use hearing aids (; based on data from Davis et al. Citation2007). Hence we estimate that the hearing test reached 70% (i.e. 7.7/11) of the target population of adults with hearing loss who do not currently use hearing aids.
Figure 2. Percentage of UK adults aged 50–74 years as a function of (i) hearing loss at 0.5, 1, 2 and 4 kHz in the better ear using a criterion of 35 dB HL or greater (reported by Davis et al. Citation2007); (ii) took the internet hearing test; (iii) failed the internet hearing test (indicating hearing loss of 35 dB HL or greater).
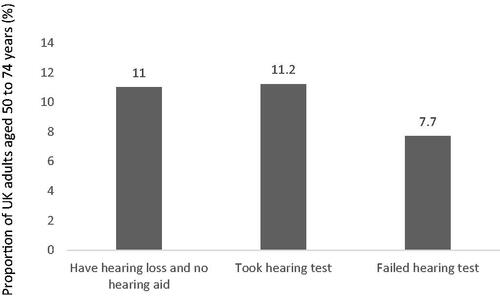
Table 1. Sample demographics for the uptake study, including those who took the hearing test and those who did not take the hearing test.
There was no evidence of a difference in age (t(598) = 1.24, p = 0.21), number of GP consultations in the past year (Mann–Whitney U p = 0.548), proportion of women and men (Χ2(1) = 0.55, p = 0.46) or ethnic background (Χ2(1) = 0.12, p = 0.72) between those who took the test and those who did not. Those who took the test were from more affluent backgrounds than those do did not take the test (t(598) = 3.39, p = 0.002).
Discussion
The internet-delivered hearing test offered via postal invitation from a general medical practitioner was an efficient and acceptable paradigm for systematic adult hearing screening. In this study, 11.2% of adults aged 50–75 took the hearing test, with 7.7% failing it at the 35 dB HL criterion. Davis et al. (Davis et al. Citation2007) identified that 11% of UK adults aged 55–74 have a hearing loss >35 dB HL and do not use a hearing aid. Assuming similar levels of hearing loss in the current study to those reported by Davis et al. the internet hearing screening paradigm may therefore have reached about 70% of the target population.
The majority (7.7/11.2; 69%) of people who took the test failed it, suggesting that there was selective uptake of the test by people with a hearing impairment. If uptake of the test was random, one would expect around 11% of people who took the hearing test to have failed it (following Davis et al.’s estimates).
Uptake of the test was equitable across gender, age and ethnic background groups. The study samples had a similar proportion of people with White British background (80.5% of the UK population is White British (Office for National Statistics Citation2011), compared with 76.4% White British in this study), but much more deprived than average (Townsend index of 1.95 versus 0 for the whole of the UK, i.e. the 3% most deprived in the UK). Given the association between deprivation and uptake, one might expect that uptake of the test would be higher in a sample that was more representative of the UK population in terms of deprivation.
The observation that uptake was higher among more affluent people in the present study is consistent with observations from health screening programs in the UK and overseas (Jepson et al. Citation2000). Low uptake of screening is of concern because selective uptake may exacerbate health inequalities. Lack of internet access may be one reason for lower uptake among more deprived people; 30% of households in the lowest social grade (Semi-skilled & unskilled manual occupations, unemployed) do not have any internet connection at home, versus 3% of those in the highest social grade (Office of Communications Citation2019). One might also have expected differences in uptake of internet hearing screening by age. In the 54–74 year old age range, 22% of people do not have a home internet connection (Office of Communications Citation2019). However, within the age range in the present study, there were no differences in uptake. Encouragingly for internet-based hearing testing, internet access is increasing. In 2012, 21% of adults never used the internet. By 2018, 12% of adults reported never using the internet (Office of Communications Citation2018). Further, internet use is ubiquitous among younger age groups. Even without considering any other factors that may increase access, internet use in older age groups will become universal as younger cohorts age.
One limitation of the present study was that we had hoped to send an email, text message or postal letter according to individual patient preference for how they wish to be contacted by their GP. However, using alternative modes of contact was not feasible within the resource constraints of the study. We used a short web address to facilitate typing the address from the paper invitation letter into an internet browser. However, using email or text message invitations may increase uptake, as the hearing test could then be easily accessed via hyperlinks in the invitation.
The response rate of 11% was lower than the estimated uptake of 20% on which the sample size was based on. However, the study sample size of 600 well exceeded the minimum 246 that was originally determined to be required to estimate uptake with the 95% confidence interval at ±5%. The effect of the lower than expected uptake rate was to increase the power of the study; the sample size of 600 provides a precision of 2.5%.
The present study was focussed on testing the uptake of an internet-based hearing screen. We were not able to access information on the numbers of people who acted on a failed hearing test result and sought help for their hearing. Previous research reported that only 36% of adults acted on a failed telephone hearing screen by seeking audiological help, with only 5% then accepting and using a hearing aid (Meyer et al. Citation2011). Meyer et al. suggested that automated low cost hearing screening may still be cost effective despite low rates of hearing aid uptake.
Currently, someone failing a hearing screening test would still be required to come to an audiology clinic to verify hearing impairment and obtain a hearing aid. Having to come to a hearing aid clinic in person may present a barrier to acting on the results of a failed hearing screening (Meyer et al. Citation2011) and expose someone to the risk of communicable disease. We are presently validating a version of the DIN test that can be used for those who fail a hearing screening test to provide audiometric information required to establish hearing aid settings at different frequencies. This version of the DIN test will allow provision of individualised, remotely delivered hearing support following a failed hearing screening. This version of the DIN will also allow access to hearing interventions to be directly linked to the hearing screening test, making it easy for people to act on the results of hearing screening. To further address the issue of seeking help following hearing screening, we are (i) co-developing hearing intervention options with members of the public that include non-device-based interventions (e.g. problem-solving and self-management skills to reduce communication difficulties (Hickson, Worrall, and Scarinci Citation2007)); (ii) including evidence-based decision aids to inform patient choice of hearing intervention and facilitate decision-making (Stacey et al. Citation2017); and (iii) targeting audiometric hearing levels at which people are likely to accept and benefit from hearing interventions (Davis et al. Citation2007).
Conclusions
Internet-based hearing screening offers potential for acceptable and equitable large scale early identification of hearing problems in adults to promote quality of life and reduce the social and economic impacts of hearing loss. Particularly post-COVID19, accessible, efficient and effective online assessment could reduce the risk of communicable diseases and promote uptake of hearing aids without the need to visit a hospital or clinic.
Disclosure statement
David Moore is a paid scientific advisor to HearX and Otonomy Inc. and a shareholder of HearX. No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Action on Hearing Loss. 2015. “Hearing matters.” Retrieved from London: https://www.actiononhearingloss.org.uk/-/media/ahl/documents/research-and-policy/reports/hearing-matters-report.pdf
- Chia, E. M., J. J. Wang, E. Rochtchina, R. R. Cumming, P. Newall, and P. Mitchell. 2007. “Hearing Impairment and Health-Related Quality of Life: The Blue Mountains Hearing Study.” Ear and Hearing 28 (2): 187–195. doi:https://doi.org/10.1097/AUD.0b013e31803126b6
- Davis, A., P. Smith, M. Ferguson, D. Stephens, and I. Gianopoulos. 2007. “Acceptability, Benefit and Costs of Early Screening for Hearing Disability: A Study of Potential Screening Tests and Models: National Coordinating Centre for Health Technology Assessment, University of Southampton.” Health Technology Assessment 11 (42): 1–294. doi:https://doi.org/10.3310/hta11420.
- Dawes, P., H. Fortnum, D. R. Moore, R. Emsley, P. Norman, K. Cruickshanks, A. Davis, M. Edmondson-Jones, A. McCormack, M. Lutman, and K. Munro. 2014. “Hearing in Middle Age: A Population Snapshot of 40–69 Year Olds in the UK. Ear and Hearing 35 (3): p.e44.
- Department of Health. 2005. “Supporting people with long term conditions. An NHS and social care model to support local innovation and integration”. Retrieved from London: https://webarchive.nationalarchives.gov.uk/20130105013243/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4122574.pdf.
- Ferguson, M. A., P. T. Kitterick, L. Y. Chong, M. Edmondson-Jones, F. Barker, and D. J. Hoare. 2017. “Hearing Aids for Mild to Moderate Hearing Loss in Adults.”. Cochrane Database of Systematic Reviews (9).
- Hall, J. S. 2006. “The Development of a New English Sentence in Noise Test and an English Number Recognition Test.” MSc. University of Southampton, Southampton.
- Hazell, M., J. Morris, M. Linehan, P. Frank, and T. Frank. 2008. “Factors Influencing the Response to Postal Questionnaire Surveys about Respiratory Symptoms.” Primary Care Respiratory Journal 18 (3): 165–170. doi:https://doi.org/10.3132/pcrj.2009.00001.
- Hickson, L., L. Worrall, and N. Scarinci. 2007. “A Randomized Controlled Trial Evaluating the Active Communication Education Program for Older People with Hearing Impairment.” Ear and Hearing 28 (2): 212–230. doi:https://doi.org/10.1097/AUD.0b013e31803126c8.
- Jepson, R., A. Clegg, C. Forbes, R. Lewis, A. Sowden, and J. Kleijnen. 2000. “Systematic Review of the Determinants of Screening Uptake and Interventions for Increasing Uptake.” Health Technology Assessment 4 (14): 1–133.
- Maharani, A., P. Dawes, J. Nazroo, G. Tampubolon, and N. Pendleton, Sense-Cog WP1 group, & ageing. 2018. “Visual and Hearing Impairments Are Associated with Cognitive Decline in Older People.” Age and Ageing 47 (4): 575–581. doi:https://doi.org/10.1093/ageing/afy061.
- McRonald, F. E., G. Yadegarfar, D. R. Baldwin, A. Devaraj, K. E. Brain, T. Eisen and R. C.Rintoul. 2014. “The UK Lung Screen (UKLS): Demographic Profile of First 88,897 Approaches Provides Recommendations for Population Screening.” Cancer Prevention Research 7 (3): 362–371. doi:https://doi.org/10.1158/1940-6207.CAPR-13-0206.
- Meyer, C., L. Hickson, A. Khan, D. Hartley, H. Dillon, and J. Seymour. 2011. “Investigation of the Actions Taken by Adults Who Failed a Telephone-Based Hearing Screen.” Ear and Hearing 32 (6): 720–731. doi:https://doi.org/10.1097/AUD.0b013e318220d973.
- NHS England and NHS Improvement. 2020. “Science in healthcare: Delivering the NHS long-term plan.” The Chief Scientific Offcier’s strategy. Retrieved from https://www.england.nhs.uk/wp-content/uploads/2020/03/science-in-healthcare-delivering-the-nhs-long-term-plan.pdf
- Norman, P. 2010. “Identifying Change over Time in Small Area Socio-Economic Deprivation.” Applied Spatial Analysis and Policy 3 (2–3): 107–138. doi:https://doi.org/10.1007/s12061-009-9036-6.
- Office for National Statistics. 2011. “2011 Census.” https://www.ons.gov.uk/census/2011census.
- Office of Communications. 2018. “UK communications market report.” https://www.ofcom.org.uk/__data/assets/pdf_file/0022/117256/CMR-2018-narrative-report.pdf.
- Office of Communications. 2019. “Communications market report 2019.” https://www.ofcom.org.uk/__data/assets/pdf_file/0028/155278/communications-market-report-2019.pdf.
- Potgieter, J.-M., D. W. Swanepoel, H. C. Myburgh, T. C. Hopper, and C. Smits. 2015. “Development and Validation of a Smartphone-Based Digits-in-Noise Hearing Test in South African English.” International Journal of Audiology 55 (7): 405–411. doi:https://doi.org/10.3109/14992027.2016.1172269.
- Sawyer, C. S., C. J. Armitage, K. Munro, G. Singh, and P. Dawes. 2019. “Correlates of Hearing Aid Use in UK Adults: Self-Reported Hearing Difficulties, Social Participation, Living Situation, Health, and Demographics.” Ear and Hearing 40 (5): 1061–1068. doi:https://doi.org/10.1097/AUD.0000000000000695.
- Scholes, S.,. J. Biddulph, A. Davis, and J. S. Mindell. 2018. “Socioeconomic Differences in Hearing among Middle-Aged and Older Adults: cross-Sectional Analyses Using the Health Survey for England.” BMJ Open 8 (2): e019615 doi:https://doi.org/10.1136/bmjopen-2017-019615.
- Smits, C., and T. Houtgast. 2005. “Results from the Dutch Speech-In-Noise Screening Test by Telephone.” Ear Hear 26 (1): 89–95. doi:https://doi.org/10.1097/00003446-200502000-00008.
- Smits, C., T. S. Kapteyn, and T. Houtgast. 2004. “Development and Validation of an Automatic Speech-in-Noise Screening Test by Telephone.” International Journal of Audiology 43 (1): 15–28. doi:https://doi.org/10.1080/14992020400050004.
- Stacey, D., F. Légaré, K. Lewis, M. J. Barry, C. L. Bennett, K. B. Eden, M. Holmes‐Rovner, H. Llewellyn‐Thomas, A. Lyddiatt, R. Thomson, and L. Trevena. 2017. “Decision Aids for People Facing Health Treatment or Screening Decisions.” Cochrane Database of Systematic Reviews (4).
- Strawbridge, W. J., M. I. Wallhagen, S. J. Shema, and G. A. Kaplan. 2000. “Negative Consequences of Hearing Impairment in Old age: a longitudinal analysis.” The Gerontologist 40 (3): 320–326. doi:https://doi.org/10.1093/geront/40.3.320.
- Watson, C. S., G. Kidd, J. D. Miller, C. Smits, and L. E. Humes. 2012. “Telephone Screening Tests for Functionally Impaired Hearing: Current Use in Seven Countries and Development of a US Version.” Journal of the American Academy of Audiology 23 (10): 757–767. doi:https://doi.org/10.3766/jaaa.23.10.2.
- World Health Organization. 2018. “Global health estimates 2016: Disease burden by cause, age, sex, by country and by region, 2000–2016.” Retrieved from Geneva: https://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html.

