Abstract
Objective
Parents frequently experience challenges implementing daily routines important for consistent hearing aid management. Education that supports parents in learning new information and gaining confidence is essential for intervention success. We conducted a pilot study to test an eHealth program to determine if we could implement the program with adherence and affect important behavioural outcomes compared to treatment as usual.
Design
Randomised controlled trial.
Study sample
Parents of children birth to 42 months who use hearing aids. Eighty-two parents were randomly assigned to the intervention or treatment-as-usual group. Four parents assigned to the intervention group did not continue after baseline testing.
Results
The intervention was delivered successfully with low drop out (10%), high session completion (97%), and high program adherence. The intervention conditions showed significantly greater gains over time for knowledge, confidence, perceptions, and monitoring related to hearing aid management. Significant differences between groups were not observed for hearing aid use time.
Conclusion
We found that we could successfully implement this eHealth program and that it benefitted the participants in terms of knowledge and confidence with skills important for hearing aid management. Future research is needed to determine how to roll programs like this out on a larger scale.
Childhood hearing loss affects approximately 34 million children globally (World Health Organization Citation2020). The diagnosis is often unanticipated by parents and for many, hearing loss is identified in infancy through newborn hearing screening and hearing aids provided shortly thereafter. Early and consistent access to sound through appropriately fitted hearing aids is critical for spoken language development (McCreery, Bentler, and Roush Citation2013; Ching and Dillon Citation2013). Parents, however, frequently experience challenges learning how to manage the hearing aids and implement daily routines important for consistent maintenance and use of the devices. Education that supports parents in learning new information and gaining confidence in their role is an essential component of intervention. An eHealth approach to supplement typical audiology services may provide benefits in the delivery of vital support for parents as they learn to engage in new habits to help their child.
Parents experience varying levels of difficulty, depending on their barriers, managing hearing aid use and monitoring device function. Parents have reported a range of challenges such as, frustration in keeping the hearing aids on their child and a lack of confidence knowing how to manage the hearing aids, and they have indicated that they want more learning support (Muñoz, Preston, and Hicken Citation2014; Muñoz et al. Citation2016, Citation2019). Hours of hearing aid use varies widely among young children, typically falling below recommendations (Muñoz et al. Citation2015; Walker et al. Citation2013; Jones and Launer Citation2010) with parent report often overestimating hours of use when compared to hearing aid datalogging (Walker et al. Citation2015). This is concerning because research has found that children have better language outcomes when they wear their hearing aids 10 or more hours per day (Tomblin et al. Citation2015).
Various factors likely contribute to parents’ difficulty in managing hearing aids within their daily routines. Education on hearing aid management is often provided when parents are experiencing difficult emotions (Kurtzer-White and Luterman Citation2003), raising considerations for later parent recall of the information (Watermeyer, Kanji, and Cohen Citation2012), and this may negatively influence their ability to relay information to other caregivers. It is also important to recognise that behaviour change can be difficult. Even when the changes are desired, individuals can experience barriers that derail their ability to act on intervention recommendations or persist when faced with challenging situations (Rollnick, Miller, and Butler Citation2008). Furthermore, professional practice guidelines do not directly address parent education beyond listing topics to discuss (American Speech-Language-Hearing Association Citation2020; American Academy of Audiology Citation2013), likely rendering vast differences in the extent of education and support parents receive during audiology appointments.
Supplemental remote support may improve parent engagement and success with home routines. Muñoz et al. (Citation2016) found that families struggling with hearing aid use were receptive to remote support and hearing aid use increased when barriers were addressed. eHealth, a broad term for remote services to address health-related needs, can offer flexible opportunities for parents to access hearing aid education and support. Supportive accountability theory is a model that includes human interaction within eHealth interventions to increase adherence with the program (Mohr, Cuijpers, and Lehman Citation2011). Social support, that is interaction with a person, is an important feature of this model, and can include phone, email and/or text interaction, because human factors (e.g. accountability, legitimacy, bond) can influence adherence to the educational program. eHealth can offer timely access to education and mitigate challenges parents may experience with attending in-person appointments (e.g. transportation problems, health issues) making travel to a clinic for services difficult (e.g. Coco, Champlin, and Eikelboom Citation2016). Furthermore, the recent global pandemic (COVID-19) has underscored the critical importance of having effective remote delivery options within audiology services. To address parent needs for education that supports development of hearing aid management routines, we conducted a pilot study of a supplemental eHealth program. The purpose of our study was to explore the adherence of program implementation, and to assess for differences between treatment as usual (TAU) and an eHealth education program in addition to TAU on hours of hearing aid use and parent outcomes for hearing aid management knowledge, perceptions, confidence, and monitoring.
Methods
Participants
Participants, one parent per family, were recruited via flyers posted on Facebook, Google advertisements, in clinics, word of mouth, and through state Early Hearing Detection and Intervention programs from September 2019 to August 2020. Thus, about half of this study occurred during the COVID-19 outbreak in the USA. Parents were included if they had a child with a behind-the-ear hearing aid, aged 42 months or younger, had access to the internet, and if they were proficient in English. Parents were excluded from the study if their child did not have hearing aids, used another type of amplification device exclusively (i.e. cochlear implants, bone conduction hearing aid), or did not have access to the internet. Participants were given an incentive ($50 Amazon eGift card) for their time to complete study surveys that took place at four timepoints (i.e. baseline, 4 weeks, 8 weeks, 12 weeks); the study was funded through a Utah State University Research Catalyst grant. A total of 82 parents were included in the study with 41 parents being randomised to the intervention group and 41 randomised to the TAU group (see Supplementary Figure 1; CONSORT checklist Supplementary Table 1). The study planned to recruit 100 participants; however, due to COVID inquiries to participate slowed down significantly and the decision was made to end recruitment. Of the 41 participants allocated to the intervention, 37 received the intervention, completed post-treatment, and follow-up assessments (n = 4 lost to follow-up). One participant discontinued the intervention prior to post-treatment but provided data at post-treatment and follow-up (i.e. that individual received a ‘lower dose’ of the intervention). All 41 participants in the TAU group completed post-treatment and follow-up assessments.
Figure 1. Change over time for both the intervention and TAU groups, with the error bars showing ± 1 standard error of the mean.
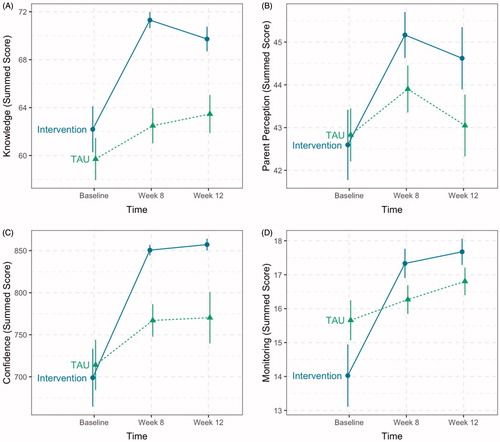
Table 1. eHealth intervention schedule.
Procedure
Study procedures were approved by the Utah State University institutional review board. After participants were deemed eligible, they were sent the link to the consent form via email or text to sign electronically. Participants then completed a child and family demographic form and baseline measures online via REDCap, an online survey platform. Once completed, participants were randomly assigned to the intervention or TAU. Throughout the duration of the study, the allocations and randomizations were conducted by the same psychology graduate students who was blinded to the allocation up until interventions were assigned. A separate psychology graduate student prepared the simple randomisation that was completed using an online random number generator to create a list of participant identifiers randomly assigned to one of two equally sized conditions (i.e. intervention vs. TAU). After randomisation, participants were sent an email containing their incentive for completing the baseline assessments and were informed of their group allocation. If the participant was randomised into the intervention condition, they were assigned a coach from the research team. The coaches included a faculty member who is a licenced paediatric audiologist and five audiology graduate students. Coaches received guidance from a member of the research team, Dr. Twohig, a licenced psychologist, on effective methods for guiding parents in identifying and addressing challenges they are experiencing related to hearing aid management. Participants in both groups completed the measures at four time points (i.e. baseline, 4 weeks, 8 weeks, 12 weeks); the 8-week timepoint was post-intervention, and 12-week timepoint was 1 month follow-up. Incentives were sent after each assessment timepoint. At the conclusion of the study, participants randomised into the TAU condition were given the option to participate in the intervention. Six participants from the TAU condition decided to opt-in for the intervention at the conclusion of the study. No data were collected on these six participants.
Intervention
The eHealth Program (intervention) was 6 weeks in duration and included weekly phone check-ins and watching a series of eight videos, two videos per week during weeks two through five (available on www.heartolearn.org). The video series was developed by the research team using health literacy principles to support understanding of the information (e.g. narrating and captioning the content), short segments to facilitate re-watching information, and insights from professional and parent focus groups (Whicker, Smith, and Muñoz Citation2020) to provide parents with information and instruction to support their engagement in hearing aid management. See for the video sequence and participant time commitment. During session 1, the coach introduced themselves to the participant, described the program, inquired as to the participant’s motivation to be involved in the study, and collaborated on goal development based on the participant’s immediate priorities. For sessions two through five, coaches asked three open-ended questions (i.e. ‘what did you like about these tutorials, what did you learn from these tutorials that you did not know before, and what questions do you have after watching these tutorials’) regarding the participants’ experience with the video tutorials assigned for the respective session, explored progress on their goals, and supported participant’s in their problem-solving process, if applicable. Flexibility was built into the manual, but the predetermined questions served as the base of the call. The final session was devoted to reviewing participant’s views on their goals and developing a plan of action for their continued management of hearing care for their child. Participants received a text reminder the day before their scheduled call, unless the call was on a Monday then the participant would receive the reminder on the previous Friday.
Measures
Four measures were used to assess the parent outcomes important to the intervention. Items are available in the tables in Supplemental Information online.
Hearing Management Knowledge is a 15-item self-reported questionnaire, developed by the research team, that used a rating scale to determine the level of understanding (1 = very poor; 2 = poor; 3 = fair; 4 = good; 5 = very good). Items were modified from a previous study (Muñoz et al. Citation2016) to assess the level of understanding parents have as to why each item is important (e.g. ‘clean earwax out of my child’s earmolds’).
Parent Perceptions is a 17-item self-reported measure that used a rating scale to determine extent of agreement (1 = strongly disagree; 2 = disagree; 3 = somewhat disagree; 4 = somewhat agree; 5 = agree; 6 = strongly agree) that was developed by the research team. Items were modified from a previous study (Muñoz et al. Citation2015) to investigate parent perceptions in reference to hearing aid benefit, hearing aid use and confidence. Herein, this is referred to as parent perceptions (e.g. ‘I accept that my child has a hearing loss’) for the items ranked from 1 to 6 while the items on a scale of 0–100 is referred to as confidence (e.g. ‘putting the hearing aid on my child’).
Hearing Aid Monitoring is a 6-item is a self-reported measure developed by the research team. Responses indicated frequency of task performance (i.e. not yet; when needed; weekly, daily; other). Items were modified from a previous study (Muñoz et al. Citation2019) to assess how often and the method parent uses to examine their child’s hearing aid (e.g. ‘check sound quality is the listening tube’).
Treatment Received is a 12-item questionnaire, developed by the research team, designed to describe elements of treatment as usual (e.g. number of audiology appointments) and to obtain hearing aid use data.
Analysis
Three core analyses were used to assess the effect of the intervention on the various measures. First, groups were compared at baseline using Chi-square (and when necessary based on assumptions, the Fisher’s Exact test) and Wilcoxon Rank Sum tests. Standardised effect sizes (Cramer’s V for the Chi-square tests and r for the Wilcoxon Rank Sum tests) are reported for each test. This was done for each item for the demographics, and each measure (knowledge, perceptions, confidence, monitoring, and treatment received). Next, linear mixed effects models were used to test for differential changes over time between the intervention and TAU groups. These analyses used the summed scores of each measure predicted by the group, time point, and the interaction of group and timepoint. Ultimately, the interaction was the estimate of interest as it provides information on whether the change over time depends on the group (i.e. differential change over time by group). The interactions are shown visually to highlight the trajectories of both groups. Lastly, to assess final differences measured in the study (at week 12), Chi-square (and again when necessary based on assumptions, the Fisher’s Exact test) and Wilcoxon Rank Sum tests were used to compare differences between the groups at week 12 (the final time point). Standardised effect sizes (Cramer’s V for the Chi-square tests and r for the Wilcoxon Rank Sum tests) are reported for each test for week 12.
Notably, of the 82 participants that were randomised into groups, four did not complete any time points beyond baseline and one discontinued the intervention. The four without baseline were dropped from the analyses. The individuals that discontinued the intervention provided data just for the baseline for the linear mixed effects models. As a check, the four without baseline data were compared to the rest of the sample to assess if any characteristic predicted drop out. The four were similar in all variables to the general distribution of each demographic characteristic and were similar to all other measures.
All analyses were completed R version 4.0.2 (R Core Team Citation2020) using the tidyverse, gtsummary, and effectsize packages (Ben-Shachar and Lüdecke Citation2020; Sjoberg et al. Citation2020; Wickham et al. Citation2019). All data, code, and output for this project can be found at osf.io/xxxx.
Results
Parents from 36 states and 2 countries (Ireland and Canada) participated in the study (see for demographic information). Parents responded to 11 items related to the audiology services they received prior to entering the study (see Supplementary Table 2). Just over half (54%) in each group were given information on parent support organisations, and local parent-to-parent groups for hearing loss were provided for some (intervention 32%; TAU 41%); however, some parents indicated they received no information on support services (intervention 43%; TAU 27%). Parents reported the hearing aid management tools that were provided by their audiologist, including a listening tube (intervention 78%; TAU 76%), battery tester (intervention 70%; TAU 39%), air blower to remove moisture from earmold tubing (intervention 73%; TAU 68%), and a cleaning tool to remove earwax (intervention 89%, TAU 93%).
Table 2. Parent demographic information.
Program adherence
Ninety percent (37/41) of the participants in the intervention group completed the study, and of those 36 (97%) completed all six phone calls, suggesting acceptability of the eHealth educational intervention. One participant in the intervention group completed two out of the six phone calls. Although participants in the intervention group were asked if they had watched the assigned videos during the phone check-ins, there was no official record of which participants completed this task.
To explore the fidelity (i.e. adherence to program protocols) of the intervention, 20% of audio sessions were randomly chosen and reviewed by raters familiar with the intervention objectives using a scoring sheet. Specifically, of the 216 voice recorded sessions, 7 audio files from each call (e.g. call 1, call 2, call 3) were selected at random from different participants. This was done with an online random number generator used to create one list of random numbers between 1 and 37 (i.e. used to label participants who have attended at least one session) without replacement. Two members of the research team that did not provide the coaching completed the scoring. The scoring was based on the use of counselling skills (i.e. asking open-ended questions, validating and responding to emotions) throughout the call and completion of the three intervention objectives (i.e. asked what was helpful about the program, goals moving forward and anticipated challenges going forward). Each item was scored ‘1′ if the coach enacted the behaviour and ‘0′ if the behaviour never happened. Both raters had 100% agreement that each randomly selected call was conducted with the use of counselling skills and completed all intervention objectives (total score = 4).
Baseline comparisons
The groups were compared at baseline to determine similarities/differences. There were no statistically significant differences between the intervention and the TAU groups at baseline, except for on two items. One knowledge item, getting loaner hearing aids if my child’s hearing aids are sent for repair, was different (p = 0.008); more parents in the TAU group rated their understanding as good or very good (61%) compared to the intervention group (54%), and one hearing aid maintenance tools item, battery tester (p = 0.011); more parents in the intervention group had a battery tester (70%) compared to the TAU group (39%).
Hearing aid use
Parents reported hearing aid use four times (i.e. baseline, 4 weeks, 8 weeks, 12 weeks) based on their perception, and when average daily hours per use from data logging was provided to them by their audiologist. Few parents reported that they have received data logging from their audiologist (Intervention n = 7; TAU n = 9). On average, for the data logged time, the intervention group went from 8 h a day to nearly 11 h while the TAU group went from 6.5 h to almost 8.5 h a day. Similarly, for parent reported time, the intervention group went from just over 9 h to almost 9.5 h while the TAU group went from 7.6 h to 8.4 h. Given both groups experienced a slight increase over the 12 weeks in both the parent reported and data logged hours of hearing aid use, no differences emerged between the groups (ps > .250).
Parent outcomes
Two research questions guided the assessment of the four parent outcome measures. First, is there a differential change over time (i.e. baseline, 8-weeks [post-intervention], 12 weeks [1 month after intervention]) based on group? That is, does the intervention group improve over time in ways that the TAU group does not? Second, were there significant differences between the groups at the end of the study (week 12). This second question is more of a snapshot of how the groups ended the study.
Differential change over time
First, to assess change over time, and how that change over time may differ by group, four linear mixed effects models were used to assess the change over time for each of the parent outcome measures. For knowledge, there was a significant interaction effect (p = 0.008), showing the intervention group increasing from baseline at week 8 and week 12 compared to the TAU group (see panel A). For parent perceptions, it appeared to have what could be an interaction effect (p = 0.065). Again, a similar pattern emerges where the intervention group, although similar at baseline, is higher at week 8 and week 12 compared to the TAU group (see panel B). For the confidence measure, there was a clear significant interaction (p = 0.004). As with the knowledge and parent perception measures, the confidence measure showed a similar pattern of similar values at baseline for the groups but higher week 8 and week 12 for the intervention group (see panel C). Lastly, the monitoring measure, again showed a similar pattern with an interaction (p = 0.004; see panel D).
Differences at week 12
A major aspect of the study is to assess differences at the end of the intervention. Herein, Chi-square (and when necessary Fisher’s Exact test), as well as Wilcoxon Rank Sum tests were used based on the type of measure being assessed. Knowledge measures at week 12 is shown in Supplementary Table 3 with associated hypothesis tests. Five of the individual items showed significant differences (p < 0.05) between the groups. For the summed score of knowledge, there was a significant difference (p = 0.001) with a large effect size (Cohen’s d = 0.73). Parent perception measures are shown in Supplementary Table 4 with associated hypothesis tests. No individual items were significant (ps > 0.110). The summed score was possibly significant (p = 0.059) with small effect size (Cohen’s d = 0.35). As for the confidence measures, five of the items were significant at alpha of .05 (see Supplementary Table 5). The summed score for confidence was significant (p = 0.042) with a moderate effect size (Cohen’s d = 0.60). Finally, of the monitoring measures, as shown in Supplementary Table 6, one item was significantly different between the groups (p = .006). The summed score was not significantly different between the groups (p = 0.100) with a small effect size (Cohen’s d = 0.35) although this effect should be considered in light of the intervention group having started somewhat lower than the TAU group at baseline. Tables 3–6 are available online as supplemental information.
Discussion
The current study investigated parent acceptance of and outcomes from a 6-week supplemental eHealth education and support program for hearing aid management compared to parents who received TAU only. The eHealth program was conducted with a high level of fidelity among coaches, and parents in the intervention group were responsive to the eHealth program. They watched the videos and engaged in the coaching phone calls. All parents completed questionnaires at four time points (i.e. baseline, 4 weeks, 8 weeks, 12 weeks). Results showed that from baseline to 12 weeks, parents in the intervention group had more gains in knowledge, perceptions, confidence, and monitoring related to hearing aid management than parents in the TAU group. Hearing aid use increased over the time points for both groups and group differences were not significant. These findings from the pilot study suggest that this supplemental eHealth education and support program is beneficial for parents and can improve parents’ daily hearing aid management routines.
Parents are key partners in the intervention process, and their engagement is critical as they are with their child each day. Parents can be poised to be more effective when they have an understanding of why it is important for them to attend to various tasks to help their child hear. For children to have audibility they need well-functioning hearing aids (McCreery, Bentler, and Roush Citation2013) and troubleshooting problems (e.g. wax blockage) is part of hearing aid management. Of the parents in the intervention group, 95% reported good or very good understanding of why troubleshooting hearing aid problems is important compared to 70% in the TAU group at the end of the study. Confidence with skills is also important for tackling daily hearing aid routines, such as completing a listening check to determine if the hearing aid is functioning properly. At the end of the study 38% of parents in the intervention group reported doing a daily check, compared to 10% of parents in the TAU group. While the intervention helped, most parents are not doing daily listening cheques. This may be influenced by various factors; however, one concern is approximately one-quarter of the parents in each group did not have a listening tube. Investing time in supporting parents and making sure they have the tools they need, can help parents to integrate hearing aid management habits into their daily lives, and this can offer developmental benefits for children. Research with adults who use hearing aids found improved knowledge and self-efficacy with multimedia education and m-health programs (Ferguson et al. Citation2016, Citation2020; Gomez and Ferguson Citation2020), providing further support of the importance of offering programs that address hearing aid management.
Improvement in parent knowledge and confidence is important for hearing aid management; however, this alone may not result in increased hours of hearing aid use. Hearing aid use differences were not observed as both groups reported increased use over the time of the study. It should be noted that there was broad variability in hours of use within both groups, and most parents reported their perception of use as they did not have data logging results from their audiologist and as such, the hours reported may be an over-estimation of use. Walker and colleagues (2013) found that on average, parents over-estimate use on average by 2 h. In the intervention group, 75% of parents indicated they had a good or very good understanding of why it is important to know their child’s hearing aid data logging results, compared to 39% of parents in the TAU group. Incorporating data logging into parent education would address an important gap by helping parents identify problems with use and determine solutions they can implement.
eHealth offers opportunities to support parents in hearing aid management. Our study shows feasibility of delivery and acceptability for parents, as well as provides some data on benefits of providing supplemental education and support for parents, beyond treatment as usual. This is particularly salient in the current environment with the COVID-19 pandemic. Treatment needs for children with hearing loss have not changed, and development cannot wait for in-person visits. This study has clinical implications as audiologists may be interested in including supplemental eHealth support in their practice. Our study used instructional videos, developed by our research team, that are freely available (www.heartolearn.org) to support parent learning and retention.
Supportive accountability was a factor in this study and provided valuable human factors to encourage engagement and improve adherence. Supportive accountability (Mohr, Cuijpers, and Lehman Citation2011) incorporates human interaction into eHealth delivery, and in the current study participants were accountable to the homework (i.e. videos) as they were discussed in the weekly phone calls. Key factors in communication during coaching phone calls included having unconditional positive regard for the parents, asking open-ended questions to understand their concerns and challenges, responding to their emotions, guiding parents as they identify meaningful goals and determine steps that they feel ready and capable of taking in addressing their hearing aid management struggles. The weekly calls also served to provide accountability in the process. The majority of the coaching calls were conducted by graduate students, were on average 10 minutes in duration, and were provided for six consecutive weeks—representing minimal additional commitment for audiologists while yielding important benefits for parents.
Limitations and future directions
Although we sought to recruit a diverse sample of parents of children who use hearing aids, our sample was not representative of the population. The majority of the parents were White, college educated, and had a fairly high-income level. The study was limited to English-speaking parents of children who use behind-the-ear hearing aids. Future research is needed that includes a more diverse demographic, as well as parents with children who use other types of hearing devices. This study illustrated benefits of a structured educational program and frequent (weekly) coaching to help parents address barriers; however, it did not sufficiently address problems with hearing aid use. The length of the eHealth program and the scope of support offered may have been insufficient to address problems and increase hours of hearing aid use. Parents had to wait for the weekly scheduled call to talk, and there may be benefit in providing support that is more dynamic and addresses a broader range of treatment adherence barriers.
Future research is needed to further explore frequency and type of support to best target parent needs.
Furthermore, as a pilot study, there was not an active control group and the sample was designed to detect a moderate-to-large effect size at each time point, which may have produced under-powered analysis in some cases where the true effect size was smaller. This was also the reason an adjustment for the multiple comparisons was not used (i.e. an adjustment would further lower power). As such, significance was not the focus of the paper but rather general patterns of effect and the size of those effects.
Overall, outcomes were better for the intervention group compared to the treatment-as-usual group. The findings suggest the eHealth program provided benefit to parents for hearing aid management. Future research is needed to better understand variables that influence parent behaviour and mechanisms to help parents achieve effective routines.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- American Academy of Audiology. 2013. “American Academy of Audiology Clinical Practice Guidelines: Pediatric Amplification.” Accessed 14 June 2020. http://galster.net/wp-content/uploads/2013/07/AAA-2013-Pediatric-Amp-Guidelines.pdf
- American Speech-Language-Hearing Association. 2020. “Practice Portal: Permanent Childhood Hearing Loss.” Accessed 14 June 2020. https://www.asha.org/PRPSpecificTopic.aspx?folderid=8589934680§ion=Overview
- Ben-Shachar , Makowski Lüdecke. 2020. Compute and interpret indices of effect ize. CRAN. Available from https://github.com/easystats/effectsize
- Ching, T. Y. C., and H. Dillon. 2013. “Major Findings of the LOCHI Study on Children at 3 Years of Age and Implications for Audiological Management.” International Journal of Audiology 2 (52): S65–S68.
- Coco, L., C. A. Champlin, and R. H. Eikelboom. 2016. “Community-Based Intervention Determines Tele-Audiology Site Candidacy.” American Journal of Audiology 25 (3S): 264–267. doi:10.1044/2016_AJA-16-0002.
- Ferguson, M., M. Brandreth, W. Brassington, P. Leighton, and H. Wharrad. 2016. “A Randomized Controlled Trial to Evaluate the Benefits of a Multimedia Educational Program for First-Time Hearing Aid Users.” Ear and Hearing 37 (2): 123–136. doi:10.1097/AUD.0000000000000237.
- Ferguson, M. A., D. W. Maidment, R. Gomes, N. Couslon, and H. Wharrad. 2020. “The Feasibility of an m-Health Educational Programme (m2Hear) to Improve Outcomes in First-Time Hearing Aid Users.” International Journal of Audiology. doi:10.1080/14992027.2020.1825839.
- Gomez, R., and M. Ferguson. 2020. “Improving Self-Efficacy for Hearing Aid Self-Management: The Early Delivery of a Multimedia-Based Education Programme in First-Time Hearing Aid Users.” International Journal of Audiology 59 (4): 272–281. doi:10.1080/14992027.2019.1677953.
- Jones, C., and S. Launer. 2010. “Pediatric Fittings in 2010: The Sound Foundations Cuper Project.” In A Sound Foundation through Early Amplification: Proceedings of the 2010 International Conference, edited by R. C. Seewald and J. M. Bamford, 187–192. Chicago, IL: Phonak AG.
- Kurtzer-White, E., and D. Luterman. 2003. “Families and Children with Hearing Loss: Grief and Coping.” Mental Retardation and Developmental Disabilities Research Reviews 9 (4): 232–235. doi:10.1002/mrdd.10085.
- McCreery, R. W., R. A. Bentler, and P. A. Roush. 2013. “Characteristics of Hearing Aid Fittings in Infants and Young Children.” Ear and Hearing 34 (6): 701–710. doi:10.1097/AUD.0b013e31828f1033.
- Mohr, D. C., P. Cuijpers, and K. Lehman. 2011. “Supportive Accountability: A Model for Providing Human Support to Enhance Adherence to eHealth Interventions.” Journal of Medical Internet Research 13 (1): e30. doi:10.2196/jmir.1602.
- Muñoz, K., M. Larsen, L. Nelson, S. Leopold, and M. Twohig. 2019. “Pediatric Amplification Management: Parent Experiences Monitoring Children’s Aided Hearing.” Journal of Early Hearing Detection and Intervention 4 (1): 2–11.
- Muñoz, K., W. A. Olson, M. P. Twohig, E. Preston, K. Blaiser, and K. R. White. 2015. “Pediatric Hearing Aid Use: Parent-Reported Challenges.” Ear and Hearing 36 (2): 279–287. doi:10.1097/AUD.0000000000000111.
- Muñoz, K., E. Preston, and S. Hicken. 2014. “Pediatric Hearing Aid Use: How Can Audiologists Support Parents to Increase Consistency?” Journal of the American Academy of Audiology 25 (4): 380–387. doi:10.3766/jaaa.25.4.9.
- Muñoz, K., S. E. P. Rusk, L. Nelson, E. Preston, K. R. White, T. S. Barrett, and M. P. Twohig. 2016. “Pediatric Hearing Aid Management: Parent-Reported Needs for Learning Support.” Ear & Hearing 37 (6): 703–709. doi:10.1097/AUD.0000000000000338.
- Pennarola, B. W., A. M. Rodday, D. K. Mayer, S. J. Ratichek, S. M. Davies, K. L. Syrjala, S. Patel, et al. 2012. “Factors Associated with Parental Activation in Pediatric Hematopoietic Stem Cell Transplant.” Medical Care Research and Review : MCRR 69 (2): 194–214. doi:10.1177/1077558711431460.
- R Core Team 2020. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing. https://www.R-project.org/.
- Rollnick, S., W. R. Miller, and C. Butler. 2008. Motivational Interviewing in Health Care. New York: Guilfor Press.
- Sjoberg, Daniel D., Curry Michael, Hannum Margie, Whiting Karissa, and Emily C. Zabor. 2020. gtsummary: Presentation-Ready Data Summary and Analytic Result Tables. R package version 1.3.5. https://CRAN.R-project.org/package=gtsummary
- Tomblin, J. B., M. Harrison, S. E. Ambrose, E. A. Walker, J. J. Oleson, and M. P. Moeller. 2015. “Language Outcomes in Young Children with Mild to Severe Hearing Loss.” Ear & Hearing 36 (Supplement 1): 76s–91s. doi:10.1097/AUD.0000000000000219.
- Walker, E. A., R. W. McCreery, M. Spratford, J. J. Oleson, J. Van Buren, R. Bentler, P. Roush, and M. P. Moeller. 2015. “Trends and Predictors of Longitudinal Hearing Aid Use for Children Who Are Hard of Hearing.” Ear & Hearing 36 (Supplement 1): 38S–47S. doi:10.1097/AUD.0000000000000208.
- Walker, E. A., M. Spratford, M. P. Moeller, J. Oleson, H. Ou, P. Roush, and S. Jacobs. 2013. “Predictors of Haring Aid Use Time in Children with Mild-Severe Hearing Loss.” Language, Speech, and Hearing Services in Schools 44 (1): 73–88. doi:10.1044/0161-1461(2012/12-0005).
- Watermeyer, J., A. Kanji, and A. Cohen. 2012. “Caregiver Recall and Understanding of Paediatric Diagnostic Information and Assessment Feedback.” International Journal of Audiology 51 (12): 864–869. doi:10.3109/14992027.2012.721014.
- Whicker, J. J., B. K. Smith, and K. Muñoz. 2020. “Parent and Professional Perceptions and Feedback on the Content of an eHealth Hearing Aid Learning Series for Parents of Children Who Are Deaf or Hard of Hearing.” ASHA Perspectives 5 (6): 1514–1523. doi:10.1044/2020_PERSP-20-00093.
- Wickham, Hadley, Mara Averick, Jennifer Bryan, Winston Chang, Lucy McGowan, Romain François, Garrett Grolemund, et al. 2019. “Welcome to the Tidyverse.” Journal of Open Source Software 4 (43): 1686. doi:10.21105/joss.01686.
- World Health Organization 2020. “Deafness and Hearing Loss.” Accessed 14 June 14 2020. https://www.who.int/news-room/fact-sheets/detail/deafness-and-hearing-loss
