Abstract
Objective
Related to the hearing health journey, this study aimed to: (i) explore how empowerment manifests itself from individuals’ first awareness of hearing loss through to hearing aid fitting and then to becoming an active hearing aid user, (ii) identify points when the different dimensions of empowerment are most relevant, and (iii) conceptualise empowerment.
Design
A semi-structured interview study was conducted, followed by a template analysis of the data.
Study sample
Adult hearing aid users from Sweden (n = 8) and Australia (n = 10) who had worn hearing aids for between 6 and 36 months.
Results
The themes that emerged from the transcripts were knowledge, skills and strategies, participation, self-efficacy, and control.
Conclusions
This study conceptualises empowerment along the hearing health journey as the process through which individuals with hearing-related challenges acquire and use knowledge, skills, and strategies, and increase self-efficacy, participation, and the feeling of control of their hearing health care, hearing solutions, and everyday lives. There are not specific points along the hearing health journey where any dimension is uniquely relevant, instead, each dimension is a dynamic component at all stages.
Introduction
The past decades have produced a growing collection of research and interventions focussed on health-related patient empowerment, especially in populations affected by long-term conditions such as diabetes, cancer, and asthma (e.g. Anderson et al. Citation1995; Aujoulat, d’Hoore, and Deccache Citation2007; McAllister et al. Citation2012; Wallerstein Citation2006; Yeh et al. Citation2016). This body of work suggests that there is a significant relationship between patient empowerment and positive health outcomes for individuals diagnosed with these chronic illnesses. Specifically, in individuals with chronic conditions, empowerment may increase patients’ autonomy, self-management, and coping abilities (Cerezo, Juve-Udina, and Delgado-Hito Citation2016; Small et al. Citation2013).
Hearing loss is a condition that limits a person’s communication ability, social participation, and quality of life (World Health Organization Citation2004). The chronic nature of hearing loss indicates that the positive outcomes related to empowerment, seen in previous research in patients with other chronic illnesses (e.g. Anderson et al. Citation1995; Yeh et al. Citation2016), could also apply to individuals with hearing loss. Previous work investigating the clinician-hearing patient relationship concludes that patient empowerment is an important aspect of this dyad, in particular that clinicians can foster empowerment by giving knowledge, supporting the development of strategies and skills, and fostering participation through shared decision-making (Laplante-Lévesque et al. Citation2013; Poost-Foroosh et al. Citation2011). However, the intersection of hearing loss and empowerment from solely the perspective of the hearing aid user has received little research attention beyond a handful of articles published about empowerment in deaf children and adolescents (Ciciriello et al. Citation2016; Munoz-Baell and Ruiz Citation2000; Sexton Citation2017). Some studies briefly discuss certain dimensions of empowerment related to hearing aid users, for example reports that smartphone-connected listening devices are a tool to give hearing aid users control and a feeling of participation (Maidment, Ali, and Ferguson Citation2019). There are no published articles explicitly investigating the construct of empowerment in relation to adult hearing aid users. Due to the lack of research on hearing loss and empowerment, there is no agreed-upon operationalisation of patient empowerment specific to hearing health care.
Multiple researchers note that the concept of empowerment is generally rather ambiguous (Aujoulat, d’Hoore, and Deccache Citation2007; Barr et al. Citation2015; Bravo et al. Citation2015; Eskildsen et al. Citation2017; Fumagalli et al. Citation2015; Risling et al. Citation2017). A concept analysis review (Castro et al. Citation2016) found 21 different definitions of ‘patient empowerment’, and another review demonstrated that even the most cited definitions of empowerment are often cited in less than ten percent of empowerment studies (Bravo et al. Citation2015). However, according to Zimmerman’s (Citation1995) prominent psychological theory of empowerment that underpins much of prior research, it may be that a unified definition of empowerment is neither necessary nor possible. Zimmerman’s theoretical framework of empowerment posits that it takes different forms in different contexts, and therefore a population- or context-specific definition is necessary. Therefore, in the hearing loss context, the need for an empirically driven definition of empowerment tailored to the hearing aid patient journey is needed.
In the empowerment framework, Zimmerman (Citation1995) proposes that common to every setting, empowerment is the process of enabling patients to gain mastery over an issue of concern to them, from which the outcome is mastery and control of these processes (Johnsen et al. Citation2017; Zimmerman Citation1995). In the context of hearing health, this emphasises the role of the hearing aid user in their own care (Fumagalli et al. Citation2015). Empowerment is a multidimensional construct that includes intrapersonal, interactional, and behavioural components as necessary ingredients (Zimmerman Citation1995). In practice, this means that an individual must perceive that they can influence a given setting (intrapersonal component), possess the skills and knowledge to understand the given environment (interactional component), and then use behaviours that influence specific results (behavioural component).
In different settings, the intrapersonal, interactional, and behavioural components may comprise different specific dimensions. Of the dimensions suggested in the Zimmerman framework, we propose that five are particularly relevant to the hearing health journey: control, self-efficacy, knowledge, skills, and participation. These five have been highlighted in empirical literature investigating empowerment related to chronic illnesses (see Cerezo, Juve-Udina, and Delgado-Hito (Citation2016) for a review), in literature on empowerment in clinician-patient interactions in audiological visits (Bennett et al. Citation2020; Poost-Foroosh et al. Citation2011), and in research on three audiological constructs related to empowerment: self-management of hearing aids (Convery et al. Citation2016), help-seeking in hearing rehabilitation (Laplante-Lévesque et al. Citation2013), and patient-centred care (Mead and Bower Citation2002; Grenness et al. Citation2014).
The dimensions of control and self-efficacy are part of the intrapersonal component of the framework of patient empowerment (Zimmerman Citation1995). Control has come up in previous audiological work that indicates that hearing-related challenges can manifest as a loss of control over the aspect of an individual’s life related to hearing (Carson Citation2005). Other research suggests that a higher internal locus of control, the belief that events in one’s life result from one’s own actions, has been related to lower hearing handicap (Garstecki and Erler Citation1998), and to higher hearing aid use (Cox, Alexander, and Gray Citation2005). This suggests that when individuals feel that they have personal influence on their situation this may reduce hearing disability and increase help-seeking, two factors which are relevant to exploring empowerment in hearing aid users. Self-efficacy, the belief in the capability of oneself, can predict an individual’s level of coping with a challenging situation (Bandura, Freeman, and Lightsey Citation1999). Over the last decade, there has been an increased interest in the construct of self-efficacy in audiological research. Generally, the literature suggests that self-efficacy has a positive relationship with hearing aid uptake and better rehabilitation outcomes (Convery et al. Citation2016; Kricos Citation2006; Ferguson, Woolley, and Munro Citation2016; Hickson et al. Citation2014). Knowledge and skills are two dimensions of the interactional component of the empowerment framework (Zimmerman Citation1995). These dimensions have been researched in audiological studies on both self-management (Convery et al. Citation2016; Gomez and Ferguson Citation2020) and the patient-clinician interaction (Bennett et al. Citation2020). Improving an individuals’ knowledge about their hearing loss and rehabilitation options, and enhancing their skills related to managing their hearing challenges and hearing aids, may be connected to a feeling of empowerment and improved coping abilities (Barker, Leighton, and Ferguson Citation2017; Convery et al. Citation2016; Laplante-Lévesque et al. Citation2013; Maidment et al. Citation2020; Poost-Foroosh et al. Citation2011). Participation is a part of the behavioural component of the empowerment framework (Zimmerman Citation1995). The participatory aspects of the framework align with previous audiological research identifying that shared decision-making, where the patient is an active part of the decision-making process, is a central element of patient empowerment in the patient-clinician interaction (Poost-Foroosh et al. Citation2011; Pryce et al. Citation2016).
Different dimensions of empowerment may be relevant at different points along the hearing health journey. The journey, as defined here, comprises the period from first recognition of hearing challenges and help-seeking (the pre-fitting period) to acquisition (the fitting period) and through to active use (the post-fitting period). Although the experiences along this journey are important because they likely impact an individual’s decision to get hearing aids, and their ongoing satisfaction with their devices, there has been little research focussing on the hearing health journey as whole (Harvey Citation2020; Knudsen et al. Citation2010). Although the dimensions of empowerment seem to be relevant to the hearing aid user’s journey, and are beginning to feature in the hearing research literature (Maidment, Ali, and Ferguson Citation2019; Maidment et al. Citation2020), there is no research that has qualitatively scoped the experience from pre-fitting, through to fitting, and post-fitting, in relation to control, self-efficacy, knowledge, skills, and participation. Taken together, the strong relationship between empowerment and positive health outcomes, and the lack of previous research to conceptualise empowerment in a hearing health care context, indicate that this is an important area of interest.
The purpose of this research is to fully understand the construct of empowerment in relation to hearing health care, through three study aims:
To explore how empowerment manifests itself for individuals on the journey from first awareness of hearing loss through to hearing aid fitting and becoming an active hearing aid user.
To identify points along the hearing health journey when the different dimensions of empowerment are most relevant.
To conceptualise empowerment along the hearing health journey.
Materials and methods
Study design
Two research sites participated in a semi-structured interview study: ORCA Europe in Stockholm, Sweden, and National Acoustics Laboratories in Sydney, Australia. An interdisciplinary team from audiological and psychological backgrounds carried out the research. Analysing interviews from two different sites may help to iterate further insights and understanding than a single-site study, and therefore facilitate a broader understanding of the topic at hand (Jenkins et al. Citation2018; Knudsen et al. Citation2012). Service delivery models and rehabilitation practices vary slightly between the two countries, and therefore including participants from two countries may also illuminate regional differences in the patient’s hearing health journey. However, while intercultural differences are briefly discussed in the following sections, the evaluation of cultural differences is not the primary aim of the article. The study was approved by the Swedish Ethical Review Authority (dnr: 2019-05506) and the Australian Hearing Human Research Ethics Committee (Approval number AHHEC 2020-01).
Participant sampling and recruitment
Eighteen participants (eight in Sweden and ten in Australia) were recruited via participant pools using purposive sampling methods, whereby sampling is done using preselected criteria relevant to the research aims at hand. This method is particularly useful when the data are intended to contribute to an improved understanding of a theoretical framework (Bernard Citation2002). In this case, we wanted to learn about the experience of individuals who had been relatively recently fitted with their first hearing aids. Inclusion criteria were adults with hearing loss (>18 years of age), fluent in the local language of the research site, who experienced their first hearing aid fitting within the last 6–36 months. The participants were regular hearing aid wearers, identified by answering ‘about ½ the time’ to at least one of four pre-defined scenarios selected from the Glasgow Hearing Aid Benefit Profile (Gatehouse Citation1999). Eight individuals (two women) participated in interviews conducted in Sweden and ten (five women) in Australia. Data collection occurred between February and July 2020, with a pause in interviews from March to June 2020 due to the global coronavirus pandemic. After discussions within the research team, we determined that the pandemic experience would not adversely confound the participants’ ability to discuss the topics and themes at hand. When it was safe to do so, we resumed in-person interviews in July 2020. The mean age was 72.4 years (range = 56 − 85 years), mean hearing loss in the better ear across octave frequencies (PTA4) 0.5–4 kHz was 36.13 dB HL (SD = 16.21; range = 5.0–56.25 dB HL). There were no significant differences between the two sites in relation to age, pure tone average hearing losses, or length of hearing aid experience. The only substantive difference between the sites related to the use of apps, with 100% of the Australian participants and 25% of the Swedish participants using apps. See for further demographic information. All participants provided written informed consent and received a small monetary sum for their participation along with reimbursement of any travel costs.
Table 1. Demographics for test participants.
Procedure
A semi-structured interview format was chosen to allow participants to describe their lived world (Kvale and Brinkmann Citation2009). All interviews were conducted face-to-face with participants in Stockholm and Sydney. The interviews lasted between 37 and 153 min, with an average length of 71 minutes (SD = 29.97). The conversation began with introductory questions asking for basic demographic and personal data, including age, current or former occupation, and use of assistive listening devices. Participants were then asked open-ended structured questions, followed up with individually adapted probing questions in order to allow them to elaborate and clarify their experiences. The interview guide (see Supplementary Materials) was designed to inquire about each of the selected empowerment dimensions (knowledge, participation, control, skills, and self-efficacy) at each of the timeline points of interest (pre-fitting, fitting, and post-fitting). The guide was created iteratively with input from researchers from both research sites, and then the final version translated into Swedish for the Stockholm interviews. Each conversation was recorded on two devices, and field notes were taken to supplement the recordings.
Data analysis
All interviews were professionally transcribed verbatim. A professional translation firm translated the Swedish interviews into English prior to data analysis. QSR International’s nVivo 13 software was used to conduct a template analysis (Brooks and King Citation2014; King Citation1998). Template analysis is a type of thematic analysis appropriate for experientially-oriented research designs. It allows for a comparison of observed data to an a priori template of theoretically-driven themes, by using an iterative coding template that summarises important themes and arranges them in a meaningful way (Brooks and King Citation2014; King Citation1998). In template analysis there is no specific distinction between the organisation of manifest and latent codes (Brooks and King Citation2014), which means that both types of codes are structured without specific attention to whether they are descriptive or interpretive.
The analysis began with a process of separate, within-site in-depth familiarisation with the data by listening to the recordings and reading through the transcripts (Braun and Clarke Citation2006). In order to align in our approach to coding and thematic categorisation, the research team co-coded two transcripts via internet-mediated meetings. We developed the first iteration of the coding template by organising all codes hierarchically, with broad overarching themes and more specific codes nested under broader ones in meaningful clusters. This version of the coding template was applied to the rest of the data analysis, which remained independent at each site for the remaining corpus of transcripts. The transcripts were each coded in their entirety, including references to the pre-defined empowerment dimensions and to text that did not directly relate to the theoretical framework. By coding in this way, the research team remained responsive to emergent codes and themes that were not included in the original empowerment framework. Some segments of text were coded in parallel, where the same passage is classified with more than one code at the same level.
The a priori empowerment themes (knowledge, skills and strategies, participation, self-efficacy, and control) were redefined as necessary, based on the data. As we approached the end of the coding process, the research sites exchanged two transcripts that had already been coded, independently analysed them, and then met to compare and discuss. This was to ensure that we were aligned in our coding and interpretation procedures. This was a pragmatic and collaborative approach to analysing relatively large amounts of data across two sites. It allowed for independent themes to emerge at each site while also ensuring an aligned approach to a shared understanding of common themes. Throughout the final process of refining the coding template, the research team met regularly to discuss, re-analyze, and reach consensus on the final coding template (see ).
Table 2. Coding template showing the key dimensions and sub-dimensions.
Several elements of the research and analytical process acted as techniques to enhance trustworthiness (Guba and Lincoln Citation1989). The thick description in the research design provides a detailed description of the theoretical perspectives, data collection, and analytical methods undertaken in the current study. Research and analytical methods most relevant to the research question at hand were selected, thereby increasing credibility. Triangulation, the search for data from multiple sources, was employed by including different researchers and collecting data from multiple research sites. Further, negative cases analysis was performed during the data analysis phase, whereby data that was inconsistent with the theoretically driven themes was discussed and analysed among the research team. These discussions also acted to ensure that we had enough supportive evidence for the final themes in the template. Finally, the research teams at the different sites acted as reviewers of each others’ data analyses by exchanging transcripts and independently analysing them, then meeting to review and discuss each other’s analyses and interpretations. Taken together, the use of these techniques increases trustworthiness that the findings are an authentic reflection of the experiences of the participants in the areas of interest.
Results
Reporting of the results are in line with the Standards for Reporting Qualitative Research (O’Brien et al. Citation2014). The thematic analysis at both sites centred on the five themes that correspond to the a priori empowerment dimensions: knowledge, skills and strategies, participation, self-efficacy, and control. The skills theme was expanded to include both skills and strategies. Skills are the acquired ability to do something well, and strategies are thoughts and behaviours that facilitate the management of hearing-related challenges and hearing solutions. Here, hearing solutions encompass a broad range of management options, for example hearing aids, assistive listening devices, and communication strategies. The skills and strategies constructs are so closely related that the research team chose to keep them together in one theme.
Interactional component
Knowledge
Knowledge refers to the acquisition and assimilation of information, leading to an understanding of an individual's hearing, hearing-related challenges and hearing solutions. In the subtheme knowing about myself, participants identified that knowledge about themselves was a central part of their patient journey. This includes knowing facts about their own hearing loss, being able to identify an array of situations in which it is particularly challenging to hear and knowing what was important to them when choosing hearing aids. Knowledge of themselves from outside their patient journey was also relevant here, as participants described knowing what type of person they are and how that influenced their experiences as first time hearing aid users:
At least I'm like that. I want to try the things out first if I'm happy with them. (P6)
Participants talked in depth about the hearing- and hearing aid-related information they had received and the knowledge that it had become. In acquiring information, participants shared that their main source of information was their audiologist, but some also sought out information from family, friends, and the internet. From their audiologist, participants recalled receiving a wide range of information, for example explanations of their audiograms and hearing loss, tips for hearing aid maintenance, and advice about when to return for adjustments. Overall, participants could not name one particularly important piece of information that their audiologist had given to them about their hearing aids nor hearing health.
I mean, there were lots of things that we spoke about, but nothing that held my attention or was held in my memory anyway. (P12)
However, they generally reported that they were happy with the level of knowledge they had about their hearing aids and hearing. Reasons for actively searching out information included that participants preferred to look out for information themselves, they felt that they had been given unclear answers to their questions, or because they felt that they had not received information about certain topics.
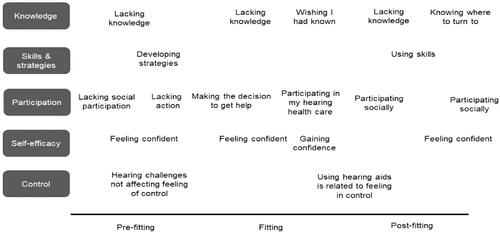
In a related subtheme, participants talked about knowing where to turn to. They revealed that for information on hearing and hearing loss they turn to the internet, local organisations, the library, or occasionally, directly to their audiologist. They also discussed where they turn for support, sharing that for assistance with both their hearing aids and hearing health they would turn to their hearing clinic. This was an especially common sentiment in the post-fitting period, suggesting that in this period participants had realised that the hearing clinic was a resource for assistance. An outline of the subthemes displaying temporal variations that are highlighted in this results section are summarised in .
Today I would probably go to a hearing clinic and ask […] [about] both hearing and hearing aids. And say that no, I don't understand my hearing aids, I get a strange sound. Today, I wouldn't go to read up on it, I would go and ask instead. (P4)
For those who had acquired information about hearing and hearing aids, participants displayed varied knowledge. Knowing about hearing and hearing aids comprises references to how to adjust, maintain, and use not only hearing aids, but also assistive devices, apps, and programs. Some participants also revealed a general understanding of developments in hearing aid technology, and a few had an awareness of new models that were being released.
This is how I've understood it, that hearing aids today start to become smarter, they start to understand context, and the older hearing aids were mostly about increasing the level. (P7)
Participants did not always have all the information or knowledge they needed or wanted. Lacking knowledge shows that in the pre-fitting period, some participants did not know where to get information and many were missing basic information about hearing aids. For those who lacked knowledge in the fitting and post-fitting periods, it tended to be about their hearing aid programs and hearing aid app functionalities. Wishing I had known reveals the after the fitting period, some participants realised that there was knowledge that they wished they had learned earlier in the process. Further, participants acquired knowledge along the journey that they now think would have helped them earlier on, for example to motivate them to try hearing aids earlier.
It was so good to be able to hear. It's easiest to say. To be able to use hearing aids and use assistive devices to hear. Actually, I wish that I learned this already earlier on. (P4)
Conversely, sharing knowledge illustrates that some participants passed on information to those around them, including family, friends and various community interest groups. Participants shared information as well as personal experiences on a range of topics like hearing, hearing aids, hearing protection, and the expense of hearing aids and other related costs. They also shared about various pathways to access hearing healthcare services and hearing solutions through private and public subsidies and government programs.
I know this one friend who said, "Oh they're too expensive." I said, "No they're not," I said”, "Go … you know, you can do it. (P13)
Other participants expressed a need to share knowledge about hearing and hearing protection to a wider audience through public awareness campaigns in the media.
So I think there's probably… [They] could do with a lot more ‘anti-smoking’ campaigns for ears. (P17)
Skills and strategies
Individuals use skills and strategies together to manage their hearing and improve communication with others. This theme displayed notable variation in how participants discussed skills and strategies in different time periods along the patient journey. In the pre-fitting stage, participants spoke in-depth about strategies that they acquired themselves to manage hearing challenges, suggesting that they do not always rely on their audiologists to teach them strategies. In this stage, developing strategies to manage their hearing challenges occurred both consciously and unconsciously. Some participants learned strategies from observing those around them who also had hearing challenges, and some were actively taught by family and friends. Others developed strategies instinctively without consciously noticing what they were doing.
I always look carefully at the one who's talking. I learned that by myself. Maybe it was subconscious, I don't know, but I've learned that. (P8)
Participants described that they had been using strategies to handle their hearing challenges and solutions both with and without awareness. Several participants talked about unconsciously using strategies that they were only made aware of once they recognised that they had a hearing loss, for example lipreading. Some participants framed their use of hearing aids as a strategy. Behavioural strategies were used for a variety of reasons, for instance to mask and manage hearing challenges. Less commonly, strategies were employed to feel in control of the situation. The strategies used to manage hearing challenges varied considerably, with the most common approaches being to ask people to repeat themselves or speak up, to sit closer to the speaker, and to be open with one’s communication partner about hearing challenges.
Then I ask them to repeat it, that's the thing, I'm pretty stubborn with that because I do want to hear. Oh, she can't hear, they say. Yes, that's right.’ (P5)
Strategies to manage hearing challenges can be adaptive, such as the those used above, or maladaptive, which lead to less desirable results. Using maladaptive strategies details the use of strategies that led to miscommunication or isolation. For example, participants disclosed that at times they would not want to reveal their hearing challenges and would instead guess what somebody had said or disconnect from the group by withdrawing when they could not hear.
Well, it was precisely when we were a group of people that I often sank into my own world because I couldn't hear everything. (P2)
In using skills, the references were mainly clustered in the post-fitting period. Participants described using a range of practical hearing aid handling and management skills and routines they developed for daily hearing use, hearing aid maintenance and repair.
No more than the habitual things like taking them out every night, giving them a bit of a clean and putting them in a charger and back out in the morning and in the ear. (P18)
Several participants also reported using routines and problem-solving skills, for example getting ears checked routinely for earwax, recording the date and time when batteries were replaced, or carrying spare batteries, to proactively manage and care for their hearing aids.
I'll take the plastic case, so that if all else fails, I can take them out and put them into the plastic case to look after them. (P12)
Behavioural component
Participation
Participation is the active involvement in both hearing rehabilitation and all aspects of social life, including family and informal social relationships. It encompasses the decisions, processes, and actions on the hearing health journey, and the emotional aspects of everyday and social life. Within this theme, participants revealed feelings both of lacking participation and actively participating. In lacking participation and involvement, some participants talked about lacking participation in my hearing health care. These experiences were centred around a lack of decision-making power in the clinical visit when the professional led the session during, for example, adjustments and choice of hearing aids. The references were framed both negatively and neutrally. At times, participants perceived that their audiologist was in charge during their clinical visits due to their expertise and knowledge, and therefore that it was reasonable for them to drive the interaction.
No, [I did not feel involved], I presumed the results from the test made it possible to adjust them correctly. (P1)
Lacking social participation encompasses a different type of participation. This subtheme describes feelings of losing enjoyment, avoiding situations, feeling left out, and not being able to participate in the group due to hearing challenges. The references are generally clustered in the pre-fitting period. Generally, participants voiced a sense of frustration, distance, and unease with their inability to participate as they previously had.
No, not conflicts, but this feeling of being an outsider. Family get togethers were no fun, I felt isolated. (P8)
Participating in my hearing health care reveals different aspects of feeling involved in hearing aid adjustments and visits to the audiologist. At times, participants expressed a more passive sense of participation, describing that their involvement was guided by what their audiologist told them in the course of undergoing clinical encounters. Some participants said that they felt actively involved through asking questions, choosing between different models and price points, and expressing to their audiologist how they wanted their hearing aids adjusted.
Involved? Well, we had discussions, it wasn't a monologue from his side. We talked about advantages and disadvantages with certain things, and it was me who decided what things to get […] I listened to what he said, of course, his advice and such like, but I felt that it was my choice. (P2)
In participating socially, most references were clustered in the fitting and post-fitting phases. Participants conveyed that after being fitted with hearing aids, they were able to feel part of the group again, their feelings of isolation were diminished, and they were able to try new activities that they hitherto would have avoided. Further, they re-gained the desire to participate in their social life.
I don't feel I'm left outside. And I dare to ask, if I don't hear I can say “what, what was that you said?” I can ask when I don't hear, and I'm no longer ashamed of that, now I want to participate. (P8)
Within this theme, participants also shared about both lacking action and taking action to get help for their hearing challenges. Lacking action is about delaying action or not acting at all. The references are almost entirely clustered into the pre-fitting period. Various reasons were provided for postponing going to a hearing clinic even after acknowledgment of hearing challenges. Some participants reported that the decline in their hearing was so gradual or that they felt that their hearing loss was not severe enough or frustrating enough to act, while others felt that hearing aids were an additional burden or thing to wear, worry about and remember to take with them.
I'm one of the oldest of all of my friends. They're all a lot younger. So that makes it feel like, "Now I've got this." I wear orthotics in my shoes and I'm thinking, "Now it's another thing.” (P10)
A few participants expressed that they felt ‘too young’ for hearing aids or that they thought there was a societal stigma attached to having hearing aids, while others had concerns about the general appearance of the hearing aids. Many participants explained that their decision to delay was based on others’ negative experiences using hearing aids or dealing with service providers.
There was an inhibition and horror stories that I had heard about cost and commercial operators who were selling the equipment, giving tests and advice. (P8)
In making the decision to get help, clustered in the pre-fitting period, participants reported that taking the initiative to seek assistance was borne from a variety of reasons, both intrinsic and extrinsic. For example, their rationales for going to get a hearing test included wanting to hear better or being encouraged by a family member, to being enticed by a free test or seeing an ad in the newspaper. Their explanations for taking the step to get hearing aids were similarly driven both internally and externally. Some participants themselves actively wanted to find a solution for their hearing challenges, and others were urged by others or encouraged by a clinician. Other participants reported being aware of the effect their hearing loss had on communication partners.
Because my kids used to just, I used to drive them mad because they'd go, "Oh, for goodness' sake, Mother, go get something." I said I've got glasses whatever, I'm not having a hearing aid. But you really have to, in the end, you really have to do it. (P18)
Intrapersonal component
Self-efficacy
Self-efficacy refers to the belief in ones' ability to successfully manage hearing-related challenges and hearing solutions. This results in a feeling of confidence and capability. When talking about feeling confident, participants showed variation in their levels of self-confidence before the fitting period. Some expressed that they had a strong sense of security in themselves from their professional and/or personal lives and carried this through into the fitting process and use of their hearing aids. These participants expressed that their sense of confidence did not change through their hearing patient process. After fitting, many participants expressed that they felt confident in managing their hearing challenges, using their hearing aids, and communicating with others.
I feel confident when I sit and talk and I hear what people say, most of them. (P6)
Some participants shared more deeply about gaining confidence through the process from pre-fitting to post-fitting. Many participants had more confidence in communicating after being fitted and beginning to use hearing aids. They shared how they felt more secure particularly in group settings, and more secure in their ability to manage their hearing challenges.
Yeah. I feel good with them, when I got them […] I just felt a bit more confident […] That I could hear things. I can hear sirens coming now, in the car. Just things like that. (P10)
At times, participants were also lacking confidence. This pertained to acclimatising to wearing hearing aids and managing hearing aid maintenance, and also in navigating social and professional interactions, particularly in challenging conditions that require careful listening and concentration.
That's sort of like when I was with my group of friends. I mean, they're really close friends, but I wasn't confident to tell them that I can't actually hear anything you're saying. (P10)
Control
Control refers to a sense of power to influence and manage hearing-related challenges and hearing solutions in everyday life. This can be achieved by utilising acquired knowledge, skills and strategies to use hearing solutions and supportive services. The findings in this theme had considerable variation between participants. Some participants expressed that using hearing aids is related to feeling in control. They stated that the sense of control they gained after being fitted with hearing aids came both in their everyday lives and in specific communication situations.
I've got the hearing aids in, so I am in control. (P13)
In hearing challenges not affecting feeling of control, many participants revealed that their sense of control in their everyday lives and communication situations had not been altered due to their hearing challenges. They explained that they had not regained a sense of control after being fitted, because they never felt out of control. Some participants used compensatory behaviours and strategies to feel in control, such as avoiding problematic situations and taking control of the conversation. A handful of participants expressed that they found the questions about control strange or difficult to answer, saying that they had a sense of control in all other aspects of their life and that the feeling carried over into the hearing domain.
I still think that I've had control in my everyday life, what I wanted to do and what I can do. And it's rare that I don't feel that I […] have that sense of control. (P4)
In lacking control, some participants answered that their sense of control was affected by their hearing challenges, the inability to influence or manage external factors that impact on communication and safety, such as challenging listening conditions in social situations.
I've got caught in a situation like that where you can't politely escape for a while, so … and again, that's, "Oh no, I'll have to do a lot of nodding and smiling here." So I'm not in control in those situations, which is why I try and avoid them, yeah. (P13)
Acceptance
Acceptance was an additional theme extracted during the analysis. This dimension was not directly covered in the interview guide, but many participants spontaneously brought up the topic at a descriptive and/or interpretive level. After discussion between all members of the research team and a close look at the data, acceptance was not deemed to be an additional dimension of the empowerment framework on the hearing health journey. Participants’ references to acceptance were often combined with their thoughts about the general aging process and their acceptance or lack thereof of getting older, and clustered early in their hearing health journey. Therefore, we propose that acceptance is a topic related to the empowerment process rather than an integral part of it.
Discussion
This study aimed to explore how empowerment manifests itself for individuals along the hearing health journey, from their first awareness of hearing-related challenges through to hearing aid fitting and becoming an active hearing aid user. Knowledge, skills and strategies, participation, self-efficacy, and control were each important dimensions along the hearing health journey, regardless of time period. The current findings support the need for a context-specific definition of empowerment. Driven by the findings in the current study, we conceptualise the empowerment process along the hearing health journey as follows:
Empowerment along the hearing health journey is the process through which individuals with hearing-related challenges acquire and use knowledge, skills, and strategies, and increase self-efficacy, participation, and the feeling of control of their hearing health care, hearing solutions, and everyday lives.
The themes extracted from the interviews aligned with, and expanded, on previous work in the areas of interest. Knowledge featured prominently in the descriptions of the participants. Individuals generally start by lacking information, and then they acquire and assimilate information that becomes relevant knowledge as the empowerment process progresses. This mirrors prior work demonstrating that knowing about hearing loss, solutions, and rehabilitation possibilities was related to a feeling of empowerment and enhanced coping abilities (Barker, Leighton, and Ferguson Citation2017; Laplante-Lévesque et al. Citation2013; Maidment et al. Citation2020; Poost-Foroosh et al. Citation2011), and that the receipt of information and knowledge is a central part of the process (Aujoulat, d’Hoore, and Deccache Citation2007). Further, the findings also showed that acquiring self-knowledge is an important aspect of this process, which has thus far been less explored in the literature. Participants emphasised that understanding the nuances of situations that challenge them and knowing specific facts about their own hearing loss and related challenges, was part of their journey, including the wish that some important information had been acquired earlier. In this way, participants demonstrated that they considered knowledge to be gained from both information and from learned experience.
Participants discussed the acquisition and use of skills and strategies at length. For some participants, communication strategies were most prominently featured in the pre-fitting stage, suggesting that they learn from observing others, or that they unconsciously develop coping strategies to compensate for their hearing-related challenges, as reported in previous work (Wänström et al. Citation2014). Other participants emphasised their use of hearing aid handling and self-management skills and strategies to proactively care for and use their hearing aids in the post-fitting phase, indicating that their audiologist may have had a role in teaching them these tools, as well as learning by ‘trial and error’. Some of the strategies that participants leaned on were maladaptive, such as withdrawing from the group or pretending to understand a conversation (Heffernan et al. Citation2016). This aligns with prior research related to using maladaptive strategies in both unconscious and conscious ways (Wänström et al. Citation2014), and the use of maladaptive strategies which were not perceived to be problematic, even if they did not help communication (Gomez and Madey Citation2001).
The findings in the participation dimension support previous work on action processes along the hearing health journey. How participants framed their decisions to seek help, and to get hearing aids, matches earlier work that presents decision-making as an aspect of participation (Knudsen et al. Citation2013; Cerezo, Juve-Udina, and Delgado-Hito Citation2016). The representations of participation in hearing health care also align with previous research that proposed that shared decision making is a central facet of patient empowerment in patient-clinician interactions (Mead and Bower Citation2002; Poost-Foroosh et al. Citation2011; Pryce et al. Citation2016). In addition to shared decision-making, our findings also elucidate how individuals experience participation through being involved in the adjustments and conversations that make up their visits to the audiologist. Beyond hearing health, there were two additional facets of participation that were highlighted in our findings: involvement in social life, which has been explored in prior work on social participation and isolation (Heffernan et al. Citation2016), and the delay or lack of participation in hearing health journey, which has been less researched so far.
Both the current findings and previous work demonstrate that self-efficacy is an important aspect of the hearing health journey. In prior literature, positive relationship between self-efficacy, hearing aid uptake, and better rehabilitation outcomes been shown (Ferguson et al. Citation2017; Hickson et al. Citation2014; Knudsen et al. Citation2010). The findings here suggest that self-efficacy extends beyond an internal process of confidence and self-belief. It also applies to an individual’s belief in their ability to handle more practical tasks, such as maintain hearing aids or navigate their hearing aid programs. In this way, self-efficacy was also evident in the strategies dimension, when participants talked about the confidence that they gained from having both coping and practical strategies in their toolbox to access in challenging communication situations.
The ways that participants interpreted and answered questions about control varied considerably. When asked about how hearing-related challenges affect the feeling of control in their life, many participants expressed that they had not lost their sense of control due to their hearing challenges. Those who had experienced a loss of control described this to be the case in specific situations, rather than generally in everyday life. This contrasts with research demonstrating that hearing-related challenges can bring a loss of both communicative control and self-presentational control (Carson Citation2005). Some said that being fitted with hearing aids mitigated the feeling. Aligning with previous work, our participants also spoke about being able to gain a sense of control over their hearing by using devices such as apps on smartphones (Maidment, Ali, and Ferguson Citation2019), or environmental factors that may influence communication (Carson Citation2005). In comparison to other empowerment literature that puts control at the centre of the process (e.g. Johnsen et al. Citation2017; Zimmerman Citation1995), our findings suggest that, while control is part of the empowerment process on the hearing health journey, for this patient group it may not be as central as for other chronic illnesses. One reason for this may be that the sense of control related to hearing is less tangible than in other chronic conditions. In hearing loss, an individual can control their surroundings and hearing aids but not necessarily modify the associated ‘condition’.
Taken together, none of the dimensions of empowerment exist in a vacuum. Instead, they influence and overlap one another. Knowledge and skills and strategies are two such dimensions. General knowledge, for instance knowing where to access help, is important for the hearing health journey. But the functional knowledge that underpins the acquisition and use of skills and strategies may be equally vital. This lines up with research saying that knowledge of communication strategies leads to an empowered outcome for hearing aid clients (Laplante-Lévesque et al. Citation2013; Maidment et al. Citation2020). These two dimensions are also linked bidirectionally to the participation dimension. An individual uses their understanding of what is going on with their hearing, and the tools to change and modify behaviours, in order to participate in their hearing journey. In the other direction, for a client to receive professional information, they need to participate in the decision-making process (Poost-Foroosh et al. Citation2011; Pryce et al. Citation2016). The participation dimension also overlaps with self-efficacy, because before one can take the action to participate in their hearing health care, they must believe that they possess the ability to do so. For some research participants, there was also a relationship between self-efficacy and control, in that their sense of control came from having the confidence to manage their situation. Furthermore, strategies adopted to manage hearing-related difficulties depends on both an individual’s level of self-efficacy and sense of control (Carson Citation2005).
Cross-referencing the entire collection of theme-related codes to their time period did not reveal specific points along the hearing health journey when any dimension varied in relevance. Instead, we saw nuanced differences related to the time periods in lower-level codes. For example, in knowledge, there were more representations of participants’ rich self-knowledge and lack of general knowledge about hearing and hearing aids in the pre-fitting period. The descriptions were thick and varied in this stage, and then became less so in the fitting and post-fitting period. The opposite trend was observed in the codes referencing knowledge about hearing, hearing solutions, and where to turn for help and information. Taken from a higher-level perspective, we see that each dimension is an important part of the empowerment process throughout all time periods, and that certain codes related to lacking or having are relevant at different stages of the journey. This finding was similar across all dimensions. Therefore, contrary to our second research aim, we cannot claim that any dimension is particularly relevant at different stages of the journey.
There is some disagreement in the literature about the temporal nature of empowerment, specifically whether the thematic dimensions are a part of the process or outcomes thereof. For instance, some authors argue that control (Bulsara et al. Citation2006; Gibson Citation1991; McAllister et al. Citation2012; Small et al. Citation2013) and participation (Anderson et al. Citation1995) are actually outcomes of empowerment. Self-efficacy is also the subject of such debate, with some researchers positioning it as a precursor and others as an outcome or indicator of empowerment (for a detailed review, see Aujoulat, d’Hoore, and Deccache Citation2007). Based on our findings, we propose that the dimensions are components of the empowerment process itself. However, this does not rule out that the dimensions can be outcomes as well. This view also aligns with Zimmerman’s (Citation1995) assertion that empowerment is not a static trait, but instead, individuals who feel empowered at one time may feel disempowered at another time. In this manner, aspects of knowledge, skills and strategies, participation, self-efficacy and control may be experienced in varying intensities and relevance depending on the characteristics of both the individual and situation.
Certain concepts and constructs outside the empowerment process are related to it in a meaningful way. In this research, we introduced acceptance as a theme associated with, but not integrated into, the hearing patient process of empowerment. The initial, internal process of acceptance seems to be a precursor to the empowerment process, with milestones like recognising that hearing challenges are a normal part of aging and comparing hearing aids to other health equipment, such as glasses. This mirrors previous work showing that for a client to be ready to become an active hearing aid user, they have to both accept the need for help and have a positive attitude towards hearing aids (Ferguson, Woolley, and Munro Citation2016; Poost-Foroosh et al. Citation2011; Wänström et al. Citation2014). Exploring the role of acceptance in future work will help to clarify whether the experience of acceptance varies in different patient groups, for example younger individuals or those with sudden deafness.
The dimensions of the empowerment process also tap into constructs such as self-management, achieved when patients can actively manage their hearing challenges on their own (Convery et al. Citation2016; Gomez and Ferguson Citation2020). Literature in this field suggests that possessing knowledge, skills and self-efficacy are central components of being able to self-manage hearing-related challenges (Convery et al. Citation2016). Patient educational interventions such as interactive multimedia videos (e.g. C2HearOnline.com, Ferguson et al. Citation2020) have shown improvements in knowledge, practical handling skills and self-efficacy for hearing aids (Ferguson et al. 2019; Gomez and Ferguson Citation2020; Maidment et al. Citation2020), and therefore such interventions can be used clinically to enhance certain empowerment dimensions and, therefore, self-management. Some authors actually argue that the ultimate goal of the empowerment process is self-management (e.g. McAllister et al. Citation2012; Shearer, Cisar, and Greenberg Citation2007), leading to the question of whether empowerment is a necessary precursor to self-management. While our findings cannot directly address this question, they do suggest that the empowerment process may bring the acquisition of knowledge, skills and self-efficacy, whereas self-management is framed as a more discrete personal contextual factor (Convery et al. Citation2019; Convery et al. Citation2016). Together, this suggests a temporal ordering whereby an individual gains components of empowerment through experience, and puts them into action in the self-management of their hearing-related challenges.
Methodological limitations
While this study added valuable knowledge to the understanding of empowerment along the hearing health journey, some limitations must be noted. Recruitment via internal databases at both research sites skews the group of participants to those who are willing to take part in research studies and, particular to this study, willing to share their experiences and reflections. Furthermore, using purposive sampling methods, and recruiting only first-time hearing aid users, means that certain types of hearing loss are not represented within the sample, namely those with severe or profound hearing losses. Related to trustworthiness, one aspect not encompassed by the current research design was member checking, where participants take part in verifying that the researchers’ emerging inferences match their lived experiences (Guba and Lincoln Citation1989). This study was the first step in a series of studies on the topic of empowerment on the hearing health journey, and participants were invited to contribute and give feedback on the next stage of this research, which evolved directly from the findings discussed here. However, in the future it would be valuable to include member checks as the final stage in all qualitative work of this nature, in order to enhance trustworthiness as much as possible.
Although the goal of qualitative work is not representativeness, it is nonetheless important to note the characteristics of the sample when interpreting the findings. By drafting the interview guide around a priori, theory-driven themes, we introduced the possibility of not examining parts of the experience of the hearing health journey that are not within the empowerment framework. However, this constraint exists for all thematic analysis methods, due to the researchers’ pre-existing awareness of literature and theory central to their subject of interest (Braun and Clarke Citation2006). This limitation was somewhat mitigated by using template analysis methods, which allowed us to remain responsive to extracting themes that were not part of the original framework.
Conclusion and future directions
This study explored the dimensions of the empowerment process along the hearing health journey. We conceptualised the process of empowerment in hearing health care and verified the need for a hearing health-specific contextualisation. The current study also contributes to knowledge about the hearing health journey by elucidating how individuals think about the dimensions of empowerment through pre-fitting, first fitting, and post-fitting. The findings support previous empowerment and audiological research by demonstrating that knowledge, skills and strategies, participation, self-efficacy, and control are all important dimensions on the hearing health journey, and revealed that self-knowledge, maladaptive strategies, and participation in social life are nuances of the empowerment process that could be further investigated in later studies. Future work on how this process intersects with the roles of the audiologist, for example in relation to information delivery and shared decision making, would be relevant and interesting, along with research on empowerment in cases where hearing aids are purchased without consulting a hearing health professional (direct-to-consumer hearing aids). Complementary research on the role of family and main communication partners in the empowerment process in hearing rehabilitation would also be valuable and illuminating. Lastly, the development of a tool to measure the dimensions of empowerment would allow for research on interventions with goal to increase empowerment on the hearing health journey.
Acknowledgments
The authors would like to thank Anja Kofoed Pedersen for her helpful contributions to the planning and analysis of this study.
Disclosure statement
The authors associated with National Acoustic Laboratories received financial support from WS Audiology. We have no other known conflicts of interest to disclose.
References
- Anderson, R. M., M. M. Funnell, P. M. Butler, M. S. Arnold, J. T. Fitzgerald, and C. C. Feste. 1995. “Patient Empowerment: Results of a Randomized Controlled Trial.” Diabetes Care 18 (7): 943–949. doi:https://doi.org/10.2337/diacare.18.7.943.
- Aujoulat, Isabelle, William d’Hoore, and Alain Deccache. 2007. “Patient Empowerment in Theory and Practice: Polysemy or Cacophony?” Patient Education and Counseling 66 (1): 13–20. doi:https://doi.org/10.1016/j.pec.2006.09.008.
- Bandura, A., W. Freeman, and R. Lightsey. 1999. Self-Efficacy: The Exercise of Control. New York: Springer.
- Barker, A. B., P. Leighton, and M. A. Ferguson. 2017. “Coping Together with Hearing Loss: A Qualitative Meta-Synthesis of the Psychosocial Experiences of People with Hearing Loss and Their Communication Partners.” International Journal of Audiology 56 (5): 297–305. doi:https://doi.org/10.1080/14992027.2017.1286695.
- Barr, P. J., I. Scholl, P. Bravo, M. J. Faber, G. Elwyn, and M. McAllister. 2015. “Assessment of Patient Empowerment-A Systematic Review of Measures.” PLoS One 10 (5): e0126553. doi:https://doi.org/10.1371/journal.pone.0126553.
- Bennett, R. J., C. Barr, J. Montano, R. H. Eikelboom, G. H. Saunders, M. Pronk, J. E. Preminger, et al. 2020. “Identifying the Approaches Used by Audiologists to Address the Psychosocial Needs of Their Adult Clients.” International Journal of Audiology 60: 104–114.
- Bernard, H. 2002. Research Methods in Cultural Anthropology: Qualitative and Quantitative. Walnut Creek, CA: AltaMitra Press.
- Braun, V., and V. Clarke. 2006. “Using Thematic Analysis in Psychology.” Qualitative Research in Psychology 3 (2): 77–101. [Database] doi:https://doi.org/10.1191/1478088706qp063oa.
- Bravo, P., A. Edwards, P. J. Barr, I. Scholl, G. Elwyn, M. McAllister, and Cochrane Healthcare Quality Research Group, Cardiff University. 2015. “Conceptualising Patient Empowerment: A Mixed Methods Study.” BMC Health Services Research 15 (1): 252. doi:https://doi.org/10.1186/s12913-015-0907-z.
- Brooks, J., and N. King. 2014. Doing Template Analysis: Evaluating an End of Life Care Service. London: SAGE.
- Bulsara, C., I. Styles, A. M. Ward, and M. Bulsara. 2006. “The Psychometrics of Developing the Patient Empowerment Scale.” Journal of Psychosocial Oncology 24 (2): 1–16. doi:https://doi.org/10.1300/J077v24n02_01.
- Carson, A. J. 2005. “What Brings You Here Today?” The Role of Self-Assessment in Help-Seeking for Age-Related Hearing Loss.” Journal of Aging Studies 19 (2): 185–200. doi:https://doi.org/10.1016/j.jaging.2004.07.001.
- Castro, E. M., T. Van Regenmortel, K. Vanhaecht, W. Sermeus, and A. Van Hecke. 2016. “Patient Empowerment, Patient Participation and Patient-Centeredness in Hospital Care: A Concept Analysis Based on a Literature Review.” Patient Education and Counseling 99 (12): 1923–1939. doi:https://doi.org/10.1016/j.pec.2016.07.026.
- Cerezo, P. G., M. E. Juve-Udina, and P. Delgado-Hito. 2016. “Concepts and Measures of Patient Empowerment: A Comprehensive Review.” Revista da Escola de Enfermagem da U S P 50 (4): 667–674. doi:https://doi.org/10.1590/S0080-623420160000500018.
- Ciciriello, E., P. Bolzonello, R. Marchi, C. Falzone, E. Muzzi, and E. Orzan. 2016. “Empowering the Family during the First Months after Identification of Permanent Hearing Impairment in Children.” Acta Otorhinolaryngologica Italica : organo Ufficiale Della Societa Italiana di Otorinolaringologia e Chirurgia Cervico-Facciale 36 (1): 64–70. doi:https://doi.org/10.14639/0392-100X-1071.
- Convery, E., L. Hickson, C. Meyer, and G. Keidser. 2019. “Predictors of Hearing Loss Self-Management in Older Adults.” Disability and Rehabilitation 41 (17): 2026–2035. doi:https://doi.org/10.1080/09638288.2018.1457091.
- Convery, E., G. Keidser, L. Hickson, and C. Meyer. 2016. “Beyond Hearing Loss: Self-Management in Audiological Practice.” The Hearing Journal 69 (3): 22–24.
- Cox, R. M., G. C. Alexander, and G. A. Gray. 2005. “Who Wants a Hearing Aid? Personality Profiles of Hearing Aid Seekers.” Ear and Hearing 26 (1): 12–26. doi:https://doi.org/10.1097/00003446-200502000-00002.
- Eskildsen, N. B., C. R. Joergensen, T. G. Thomsen, L. Ross, S. M. Dietz, M. Groenvold, and A. T. Johnsen. 2017. “Patient Empowerment: A Systematic Review of Questionnaires Measuring Empowerment in Cancer Patients.” Acta Oncologica (Stockholm, Sweden) 56 (2): 156–165. doi:https://doi.org/10.1080/0284186X.2016.1267402.
- Ferguson, M. A., P. T. Kitterick, L. Y. Chong, M. Edmonson-Jones, F. Barker, and D. J. Hoare. 2017. “Hearing Aids for Mild to Moderate Hearing Loss in Adults.” Cochrane Library of Systematic Reviews 9: CD012023. doi:https://doi.org/10.1002/14651858.CD012023.pub2.
- Ferguson, M. A., D. W. Maidment, R. Gomez, N. Coulson, and H. Wharrad. 2020. “The Feasibility of an m-Health Educational Programme (m2Hear) to Improve Outcomes in First-Time Hearing Aid Users.” International Journal of Audiology : 1–12.
- Ferguson, M., A. Woolley, and K. J. Munro. 2016. “The Impact of Self-Efficacy, Expectations, and Readiness on Hearing Aid Outcomes.” International Journal of Audiology 55 (sup3): S34–S41. doi:https://doi.org/10.1080/14992027.2016.1177214.
- Fumagalli, Lia Paola, Giovanni Radaelli, Emanuele Lettieri, Paolo Bertele’, and Cristina Masella. 2015. “Patient Empowerment and Its Neighbours: Clarifying the Boundaries and Their Mutual Relationships.” Health Policy (Amsterdam, Netherlands) 119 (3): 384–394. doi:https://doi.org/10.1016/j.healthpol.2014.10.017.
- Garstecki, D. C., and S. F. Erler. 1998. “Hearing Loss, Control, and Demographic Factors Influencing Hearing Aid Use among Older Adults.” Journal of Speech, Language, and Hearing Research : JSLHR 41 (3): 527–537. doi:https://doi.org/10.1044/jslhr.4103.527.
- Gatehouse, S. 1999. “Glasgow Hearing Aid Benefit Profile: Derivation and Validation of a Client-Centered Outcome Measure for Hearing Aid Services.” Journal of the American Academy of Audiology 10: 80–103.
- Gibson, C. H. 1991. “A Concept Analysis of Empowerment.” Journal of Advanced Nursing 16 (3): 354–361. doi:https://doi.org/10.1111/j.1365-2648.1991.tb01660.x.
- Gomez, R., and M. Ferguson. and 2020. “Improving Self-Efficacy for Hearing Aid Self-Management: The Early Delivery of a Multimedia-Based Education Programme in First-Time Hearing Aid Users.” International Journal of Audiology 59 (4): 272–281. doi:https://doi.org/10.1080/14992027.2019.1677953.
- Gomez, R., and S. Madey. and 2001. “Coping-with-Hearing-Loss Model for Older Adults.” The Journals of Gerontology Series B: Psychological Sciences and Social Sciences 56 (4): P223–P225. doi:https://doi.org/10.1093/geronb/56.4.P223.
- Grenness, C., L. Hickson, A. Laplante-Lévesque, and B. Davidson. 2014. “Patient-Centred Audiological Rehabilitation: Perspectives of Older Adults Who Own Hearing Aids.” International Journal of Audiology 53 (sup1): S68–S75. doi:https://doi.org/10.3109/14992027.2013.866280.
- Guba, E. G., and Y. S. Lincoln. 1989. Fourth Generation Evaluation. Newbury Park, CA: Sage.
- Harvey, M. A. 2020. “The Hearing Health Care Journey: Putting Beans in Your Cups." In Seminars in Hearing (Vol. 41, No. 1, p. 68). New York: Thieme Medical Publishers.
- Heffernan, E., N. S. Coulson, H. Henshaw, J. G. Barry, and M. A. Ferguson. 2016. “Understanding the Psychosocial Experiences of Adults with Mild-Moderate Hearing Loss: An Application of Leventhal’s Self-Regulatory Model.” International Journal of Audiology 55 (sup3): S3–S12. doi:https://doi.org/10.3109/14992027.2015.1117663.
- Hickson, L., C. Meyer, K. Lovelock, M. Lampert, and A. Khan. 2014. “Factors Associated with Success with Hearing Aids in Older Adults.” International Journal of Audiology 53 (sup1): S18–S27. doi:https://doi.org/10.3109/14992027.2013.860488.
- Jenkins, E. K., A. Slemon, R. J. Haines-Saah, and J. Oliffe. 2018. “A Guide to Multisite Qualitative Analysis.” Qualitative Health Research 28 (12): 1969–1977. doi:https://doi.org/10.1177/1049732318786703.
- Johnsen, A. T., N. B. Eskildsen, T. G. Thomsen, M. Grønvold, L. Ross, and C. R. Jørgensen. 2017. “Conceptualizing Patient Empowerment in Cancer Follow-Up by Combining Theory and Qualitative Data.” Acta Oncologica (Stockholm, Sweden) 56 (2): 232–238. doi:https://doi.org/10.1080/0284186X.2016.1267403.
- King, N. 1998. Template analysis.
- Knudsen, Line V., Ariane Laplante-Lévesque, Lesley Jones, Jill E. Preminger, Claus Nielsen, Thomas Lunner, Louise Hickson, Graham Naylor, and Sophia E. Kramer. 2012. “Conducting Qualitative Research in Audiology: A Tutorial.” International Journal of Audiology 51 (2): 83–92. doi:https://doi.org/10.3109/14992027.2011.606283.
- Knudsen, L. V., C. Nielsen, S. E. Kramer, L. Jones, and A. Laplante-Lévesque. 2013. “Client Labor: Adults with Hearing Impairment Describing Their Participation in Their Hearing Help-Seeking and Rehabilitation.” Journal of the American Academy of Audiology 24 (3): 192–204. doi:https://doi.org/10.3766/jaaa.24.3.5.
- Knudsen, L. V., M. Oberg, C. Nielsen, G. Naylor, and S. E. Kramer. 2010. “Factors Influencing Help Seeking, Hearing Aid Uptake, Hearing Aid Use and Satisfaction with Hearing Aids: A Review of the Literature.” Trends in Amplification 14 (3): 127–154. doi:https://doi.org/10.1177/1084713810385712.
- Kricos, P. B. 2006. “Audiologic Management of Older Adults with Hearing Loss and Compromised Cognitive/Psychoacoustic Auditory Processing Capabilities.” Trends in Amplification 10 (1): 1–28. doi:https://doi.org/10.1177/108471380601000102.
- Kvale, S., and S. Brinkmann. 2009. InterViews: Learning the Craft of Qualitative Research Interviewing (2nd ed.). Los Angeles, CA: Sage Publications.
- Laplante-Lévesque, A., L. D. Jensen, P. Dawes, and C. Nielsen. 2013. “Optimal Hearing Aid Use: Focus Groups with Hearing Aid Clients and Audiologists.” Ear and Hearing 34 (2): 193–202. doi:https://doi.org/10.1097/AUD.0b013e31826a8ecd.
- Maidment, D. W., Y. H. Ali, and M. A. Ferguson. 2019. “Applying the COM-B Model to Assess the Usability of Smartphone-Connected Listening Devices in Adults with Hearing Loss.” Journal of the American Academy of Audiology 30 (5): 417–430. doi:https://doi.org/10.3766/jaaa.18061.
- Maidment, D. W., R. Heyes, R. Gomez, N. S. Coulson, H. Wharrad, and M. A. Ferguson. 2020. “Evaluating a Theoretically Informed and Cocreated Mobile Health Educational Intervention for First-Time Hearing Aid Users: Qualitative Interview Study.” JMIR mHealth and uHealth 8 (8): e17193. doi:https://doi.org/10.2196/17193.
- McAllister, M.,. G. Dunn, K. Payne, L. Davies, and C. Todd. 2012. “Patient Empowerment: The Need to Consider It as a Measurable Patient-Reported Outcome for Chronic Conditions.” BMC Health Services Research 12 (1): 157. doi:https://doi.org/10.1186/1472-6963-12-157.
- Mead, N., and P. Bower. 2002. “Patient-Centred Consultations and Outcomes in Primary Care: A Review of the Literature.” Patient Education and Counseling 48 (1): 51–61. doi:https://doi.org/10.1016/s0738-3991(02)00099-x.
- Munoz-Baell, I. M., and M. T. Ruiz. 2000. “Empowering the Deaf. Let the Deaf Be Deaf.” Journal of Epidemiology and Community Health 54 (1): 40–44. doi:https://doi.org/10.1136/jech.54.1.40.
- O’Brien, B. C., I. B. Harris, T. J. Beckman, D. A. Reed, and D. A. Cook. 2014. “Standards for Reporting Qualitative Research: A Synthesis of Recommendations.” Academic Medicine 89 (9): 1245–1251. doi:https://doi.org/10.1097/ACM.0000000000000388.
- Poost-Foroosh, L., M. B. Jennings, L. Shaw, C. N. Meston, and M. F. Cheesman. 2011. “Factors in Client–Clinician Interaction That Influence Hearing Aid Adoption.” Trends in Amplification 15 (3): 127–139. doi:https://doi.org/10.1177/1084713811430217.
- Pryce, H., A. Hall, A. Laplante-Lévesque, and E. Clark. 2016. “A Qualitative Investigation of Decision Making during Help-Seeking for Adult Hearing Loss.” International Journal of Audiology 55 (11): 658–665. doi:https://doi.org/10.1080/14992027.2016.1202455.
- Risling, T., J. Martinez, J. Young, and N. Thorp-Froslie. 2017. “Evaluating Patient Empowerment in Association with eHealth Technology: scoping Review.” Journal of Medical Internet Research 19 (9): e329. doi:https://doi.org/10.2196/jmir.7809.
- Sexton, J. 2017. “Empowering Adolescents Who Are Deaf and Hard of Hearing.” North Carolina Medical Journal 78 (2): 129–130. doi:https://doi.org/10.18043/ncm.78.2.129.
- Shearer, N. B., N. Cisar, and E. A. Greenberg. 2007. “A Telephone-Delivered Empowerment Intervention with Patients Diagnosed with Heart Failure.” Heart & Lung : The Journal of Critical Care 36 (3): 159–169. doi:https://doi.org/10.1016/j.hrtlng.2006.08.006.
- Small, N., P. Bower, C. A. Chew-Graham, D. Whalley, and J. Protheroe. 2013. “Patient Empowerment in Long-Term Conditions: Development and Preliminary Testing of a New Measure.” BMC Health Services Research 13 (1): 263. doi:https://doi.org/10.1186/1472-6963-13-263.
- Wallerstein, N. 2006. What is the Evidence on Effectiveness of Empowerment to Improve Health? Copenhagen, Denmark: WHO Europe.
- Wänström, G., M. Öberg, E. Rydberg, T. Lunner, A. Laplante-Lévesque, and G. Andersson. 2014. “The Psychological Process from Avoidance to Acceptance in Adults with Acquired Hearing Impairment.” Hearing, Balance and Communication 12 (1): 27–35. doi:https://doi.org/10.3109/21695717.2013.875243.
- World Health Organization. 2004. ICD-10: International Statistical Classification of Diseases and Related Health Problems: Tenth Revision. https://icd.who.int/browse10/2019/en
- Yeh, H.-Y., W.-F. Ma, J.-L. Huang, K.-C. Hsueh, and L.-C. Chiang. 2016. “Evaluating the Effectiveness of a Family Empowerment Program on Family Function and Pulmonary Function of Children with Asthma: A Randomized Control Trial.” International Journal of Nursing Studies 60: 133–144. doi:https://doi.org/10.1016/j.ijnurstu.2016.04.013.
- Zimmerman, M. A. 1995. “Psychological Empowerment: Issues and Illustrations.” American Journal of Community Psychology 23 (5): 581–599. doi:https://doi.org/10.1007/BF02506983.