Abstract
Objective
To (i) identify the impact of COVID-19 on provision of UK audiology services across sectors (ii) compare teleaudiology service provision between private and public sectors before and after the introduction of restrictions and (iii) identify barriers to teleaudiology delivery amongst UK hearing care professionals in both sectors.
Design
A mixed-methods cross-sectional survey study design. Responses to the structured questionnaire were analysed using descriptive and non-parametric statistics.
Study Sample
UK based hearing care professionals (HCP) (n = 323) completed the survey (218 public sector; 89 private sector).
Results
Changes in working patterns varied greatly between different sectors, with 61% of national employed and 26% of independent HCPs being furloughed, compared with 1% in the public sector. Use of telehealth was under-utilised across all sectors and groups in UK hearing healthcare, despite 92% of public and 75% of private HCPs reporting feeling comfortable conducting remote consultations.
Conclusion
This study highlights a variation in teleaudiology adoption and key barriers across sector in the UK. A collaborative approach between hearing device manufacturers, research centres, HCPs and professional bodies is required for the creation of targeted guidance and training materials according to sector, to support clinicians in effective teleaudiology provision.
Introduction
Telehealth (also known as ehealth, telemedicine and telecare), is “the use of communication technologies to provide health care at a distance”. Teleaudiology is a subset of telehealth used to deliver remote audiological assessment or intervention (synchronously or asynchronously). Teleaudiology can also be applied to problem solving activities and empowering patients to actively engage in their healthcare management, aural rehabilitation and tinnitus management (Calvillo, Román, and Roa Citation2015; Coco Citation2020).
Recently a need to rethink the traditional delivery of clinical services has been prompted by the COVID-19 pandemic. This pandemic involved person-to-person transmission of a respiratory illness known as COVID-19 that originated in December 2019 and spread globally. To limit the spread of the virus, national lockdowns were introduced instructing people to stay at home and follow social distancing guidelines. The UK government announced the first of a series of national lockdown towards the end of March 2020 aiming to slow the spread of the disease and ease the growing pressure on the National Health Service. Audiology departments were forced to cancel many existing clinical activities and only see urgent patients to limit physical clinician-patient contact. To accommodate audiology patients, audiology departments across the United Kingdom began using telephone and video conferencing technology; for some this was the first time teleaudiology services were introduced. Joint clinical guidance from UK Audiology professional bodies (2020) has encouraged the use of remote care, where possible, to limit face to face consultations.
The successful adoption of telehealth services will depend on patient and clinician’s access to adequate technology as well as their willingness and ability to use it (Or and Karsh Citation2009; Gagnon et al. Citation2003). Teleaudiology delivery has grown from diagnostic testing and information sharing, to the fitting and maintenance of hearing aids and cochlear implants (Tao Citation2020; Swanepoel de and Hall Citation2010; Bush et al. Citation2016; Tao et al. Citation2020). Audiological screening can be carried out with self-test procedures either using pure tone stimuli or speech/digits in noise via telephone or computer headphones (You et al. Citation2020; Brown et al. Citation2019).
Clinicians can be considered the gatekeepers for telehealth adoption (Whitten and Mackert Citation2005), and the introduction of teleaudiology practices within audiology has received a mixed response. Singh et al. (Citation2014) surveyed a diverse population of Canadian hearing healthcare professionals (n = 202) where 67% of respondents worked in the private practice setting (Singh et al. Citation2014). Overall, respondents reported minimal effects of teleaudiology on hearing healthcare provision, but a positive impact on accessibility of services. Respondents’ views on teleaudiology varied according to the clinical task performed and the characteristics of the specific patient population. Additionally, significant differences were observed between private and public sector services; respondents working in publicly funded settings tended to report more positive attitudes towards teleaudiology than those from private work settings. A study by Reginato and Ferrari (Citation2014) found that despite some aspects of clinician-patient communication being affected by teleaudiology delivery, patient satisfaction was not adversely impacted in comparison with in-person service delivery (Reginato and Ferrari Citation2014).
A subsequent survey conducted by Eikelboom and Swanepoel (Citation2016) of audiology professionals from 28 countries, investigated their willingness and experience to use telehealth. Only 15.5% reported having experience using teleaudiology (Eikelboom and Swanepoel Citation2016). Additionally, respondents tended to report high confidence with use of technology (mean rating of 4.7 out 5) but were less familiar with what telehealth entails (3.7/5) and potential applications in audiology (3.2/5).
Understanding how hearing care professionals (HCPs) have adopted telehealth in response to the COVID-19 pandemic is important in assessing barriers to management of hearing loss in vulnerable populations. This could lead to development of tools and information provision to support HCPs in adopting telehealth practices in cases where it provides increased patient benefit. This is not only relevant in the current context of the COVID-19 pandemic, but also when considering the need to better serve people with hearing loss who have limited mobility/in rural settings. Saunders and Roughley (Citation2020), surveyed UK audiologists to explore their views of teleaudiology during the COVID-19 pandemic (Saunders and Roughley Citation2020). Of the 120 respondents, 75% were paediatric audiologists and it was unclear if private sector respondents were included in the sample. Findings revealed 33% of respondents had never used remote care appointments prior to the COVID-19 pandemic; reasons for this consisted of the following themes (1) clinical practices, (2) infrastructure, (3) patient preference. When asked whether remote care would have a positive effect on their practice, 88% of respondents said they believed remote care would improve flexibility of service provision, however, 54% of respondents believed remote care would have no impact on the confidence they have in service provision and 25% felt it may have negative consequences.
To broaden the scope of this work, this study aimed to establish how HCPs define telehealth and better understand how telehealth has been used before and after the outbreak of COVID-19 within both the private and public sectors.
The objectives of the current study were:
To understand how HCPs define telehealth
To investigate the ways telehealth has been used by HCPs pre and post COVID-19
To explore HCP’s barriers to telehealth uptake
Investigate differences of teleaudiology service provision between private and public sectors
Method
Study design
A mixed-methods cross-sectional survey study design was used to explore attitudes and barriers regarding the use of teleaudiology in the United Kingdom during the COVID-19 pandemic. Ethical approval was granted by the Faculty of Science and Engineering Research Ethics Panel at Anglia Ruskin University (Cambridge, UK, reference number FREP/SREP: 0520-01). The Equator network Checklist for Reporting Results of Internet e-Surveys was used to report the methods and results of the survey (See Supplementary materials).
Survey development
Items for the survey were based on a teleaudiology survey conducted by Eikelboom and Swanepoel (Citation2016). Additional questions were added to ensure both private sector and public sector audiology services were included. The final survey comprised of a maximum of 58 closed-ended questions and 4 open-ended questions and took approximately 20 minutes to complete. All except the open-ended questions were mandatory, although some of the questions were follow-up questions and only presented if responding “yes” to preceding questions by using skip logic. An example was if answering yes/no to identifying additional clinical tasks appropriate for teleaudiology that were not captured in the survey. The questionnaire focussed on two main themes, attitudes towards teleaudiology, which are reported here and experiences using telehealth, which will be reported separately.
The survey questions for this study captured the following categories (see appendix for all survey questions):
Demographic information: Age, gender, regional location, educational qualifications, work setting, work role pre and post- onset of COVID-19, duration of work, type of patients seen, time to commute to work
Understanding the term “Telehealth”
Barriers to the delivery of telehealth
The survey items were entered into Qualtrics (Qualtrics, Provo, UT) and were reviewed by team members to ensure functionality. The survey then went through two stages of review before commencing data collection. Initially, three independent clinical audiologists reviewed the questionnaire. They commented on the interpretability regarding the wording of the questions. They also determine whether the questions captured the aspects they aimed to evaluate (Taherdoost Citation2016). This review attempted to ensure the functionality of the online questionnaire and ensure it was clear and easy to complete such as being able to select multiple responses. This process indicated good face-validity of the survey.
Procedures
Eligibility criteria included HCPs working for both the National Health Service (NHS) and private sector living in the United Kingdom, aged 18 years or older who provided informed consent. The National Health Service (NHS) service provision is free at the point of access, including hearing assessments and intervention such as hearing aid fitting and follow up appointments. Within the private sector payment is made for these services although some private sector providers hold contracts with the NHS and so patients may be offered NHS equivalent audiology services, free at the point of access, within private sector. There are generally different training routes, registration bodies, professional networks and professional bodies that service each of these sectors. Private sector hearing healthcare professionals are registered as hearing aid dispensers by the Health and Care Professions Council (HCPC) whereas NHS hearing health care professionals can voluntarily register to the Registration Council for Clinical Physiologists (RCCP) as Audiologists and some audiologists with clinical scientist training register with the HCPC as clinical scientists.
The survey was open to anyone meeting the inclusion criteria. Recruitment was mostly via professional organisations’ mailing lists and social media outlets including the British Society of Audiology, British Academy of Audiology, British Society of Hearing Aid Audiologists. A snowball sampling approach was taken so that respondents could invite other HCPs to complete the survey (Berg Citation2006). The survey was launched on 5 May 2020 in the UK and was open from 11 May 2020 to 22 June 2020. Online informed consent was required before undertaking the survey and only one submission from each IP address was permitted by the survey software. No randomisation of the items was used and respondents were unable to change their responses once submitted. No personal health information or identification information was collected. Respondents did not receive payment for completing the survey.
Data analysis
Data cleaning was initially undertaken to remove cases that did not meet study eligibility for participants not resident in the United Kingdom. Data analysis incorporated a mixed approach, including both quantitative and qualitative methods. The R statistical package (RStudio Team Citation2020) was used for statistical analysis. Descriptive statistics, including frequencies, means, medians, and standard deviations were used to describe the data. A Wilcoxon rank sum test with continuity correction was conducted to compare Likert scale responses between groups (sector).
The open-ended questions were analysed using qualitative content analysis described by Graneheim and Lundman (Citation2004) (Graneheim and Lundman Citation2004). Qualitative data coding was performed using NVivo 12 software (NVivo Citation2018). Various steps were involved in the analysis process. These statements were actively read and re-read in search of initial ideas, meaning, and patterns (condensed meaning units). Repeated patterns were searched to identify categories and sub-categories. The responses that related to the same category were grouped together. Free text examples to support the descriptive analysis were included. The type of respondents mentioning the category was provided as some may have been more prominent depending on place of work (private or NHS) or level of experience (estimated by the age group).
Results
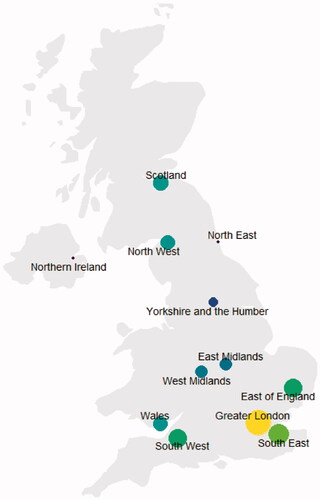
Of the 339 hearing care professionals that completed the survey, 323 met the eligibility criteria (12 non-UK respondents, and 4 did not provide consent and did not proceed further). 28% (n = 89) of respondents were from the private sector (18% from independent clinics & 10% from national chains), 67% (n = 218) from the public sector, providing free care & hearing technology within the NHS, and 5% from other work settings. illustrates the proportion of respondents from each of the 12 UK regions as indicated from their survey responses.
Figure 1. The number of responses from hearing care professionals according to UK region (n = 323). Both the gradient of the filled circle and the size of the circle indicate the number of respondents from the corresponding region (blue→yellow and small→large indicating an increasing number of respondents from <20 to >60).
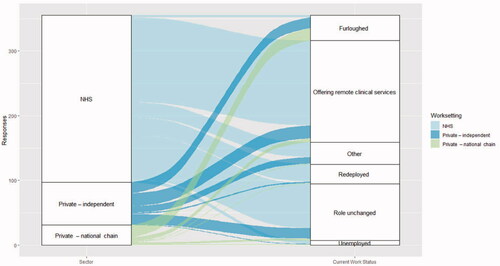
Changes in work status following onset of COVID-19
Hearing care professionals across sector frequently reported changes in work status following the onset of COVID-19, as shown in . Some respondents experienced no change: 27% NHS (n = 69), 24% (n = 16) private-independent and 10% (n = 3) private-national. Some were redeployed to other duties 10% (n = 27) NHS, 3% (n = 2) private-independent, and 3% (n = 1) private-national. Very few NHS HCPs reported being furloughed (1%, n = 3) in contrast to 26% (n = 17) of independent private clinicians, and 61% (n = 19) of those working for national hearing care providers. Adoption of remote hearing care services across sector was variable; the highest uptake reported by the NHS (51%, n = 131), followed by independent clinics (30%, n = 20) & national providers (19%, n = 6).
Understanding of telehealth
When asked “What do you understand by the term telehealth?”, open ended responses were given by 238 respondents, with most providing examples of how telehealth is carried out. Following analysis, two categories emerged: (1) use of technology and (2) remote support ().
Table 1. Respondent's answer to the question "What do you understand by the term telehealth?".
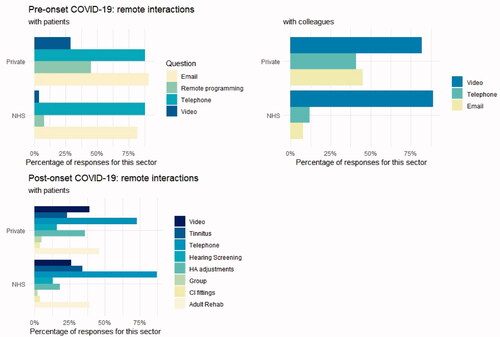
Service delivery pre-onset of COVID-19
This section of the survey on service delivery pre and post-onset of COVID-19 was completed by 221 respondents (165 NHS and 56 from the private sector.)
Before the onset of COVID-19, HCPs in both sectors reported conducting patient consultations over the phone (NHS: 88%, n = 145 and private: 88%, n = 49) and using email (NHS: 82%, n = 135 and private: 91%, n = 51). 45% (n = 25) of private HCPs reported conducting some remote programming, in comparison with only 8% (n = 14) of NHS HCPs. Overall, the use of video consultations with patients was less widely reported (NHS: 4%, n = 7, and private: 29%, n = 16) but most respondents had video-conferenced colleagues (NHS: 89%, n = 147 and private: 82%, n = 46). NHS HCPs appeared to email colleagues less (8%, n = 14) than their private sector counterparts (45%, n = 25). The same could be observed of telephone interactions between colleagues (NHS: 12%, n = 19 and private: 41%, n = 23) ).
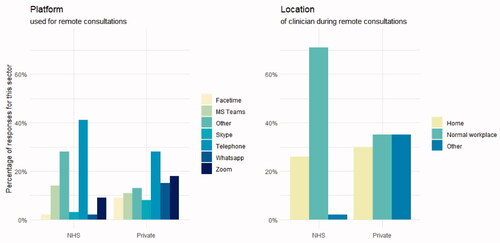
Service delivery following the onset of COVID-19
Post-onset of COVID-19, respondents from both sectors continued use of telephone consultations (NHS: 87%, n = 142 and private: 73%, n = 41) with an apparent increase in respondents having conducted video consultations with patients (NHS: 26%, n = 42 and private: 39%, n = 22). Use of remote hearing screening tools was evident (NHS: 13%, n = 21 and private: 16%, n = 9). There was limited use of remote group rehabilitation sessions (NHS: 2%, n = 4 and private: 5%, n = 3) and remote CI fittings (4% for both NHS & private sectors, n = 7 and 2 respectively). However, some HCPs were providing tinnitus services remotely ((NHS: 34%, n = 56 and private: 23%, n = 13). The use of remote hearing device fitting was reported (NHS: 39%, n = 63 and private: 46%, n = 26) but less so for adjusting hearing aid settings (NHS: 18%, n = 30 and private: 36%, n = 20).
The platform for remote consultations was most frequently the telephone (NHS: 41%, n = 96 and private: 46%, n = 26) with varied use of videoconferencing platforms. NHS respondents selecting other (28%, n = 64) tended to report using the NHS Attend Anywhere platform. The majority of NHS HCPs remained working in their normal workplace (71%, n = 130) whilst private HCPs were split over working from home (30%, n = 25), their normal workplace (35%, n = 29) or another location (35%, n = 29) ).
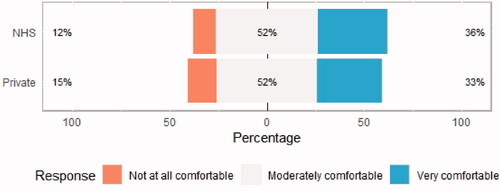
Comfort with conducting remote consultations
Fewer respondents completed this section of the questionnaire: 178 NHS and 27 private sector. Overall, 92% (n = 157) of NHS & 85% (n = 23) of private sector HCPs reported feeling moderately or very comfortable with conducting remote consultations, as shown in .
Rating of potential barriers to effective delivery of telehealth
These sections were completed by 239 respondents (202 NHS and 37 private). Attitudes towards potential barriers in the effective delivery of telehealth within hearing care were assessed using a 4-point Likert scale (with N/A as an additional option). The responses are summarised for the private sector in , and the NHS in . Across both sectors, over 50% of HCPs rated the following as somewhat of/not a barrier to telehealth delivery: (1) lack of confidence using technology, (2) confidentiality & data protection, (3) lack of support from senior management, (4) lack of training on telehealth, (5) risk of the job becoming automated, (6) limited information/lack of protocol in telehealth, & (7) internet access in the workplace.
Figure 6. Rating of potential barriers to the delivery of telehealth by hearing care professionals in the private sector.
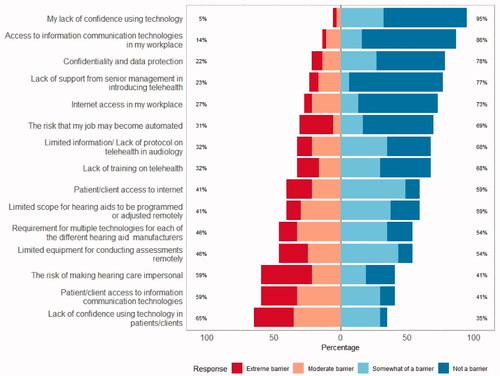
Figure 7. Rating of potential barriers to the delivery of telehealth by NHS hearing care professionals.
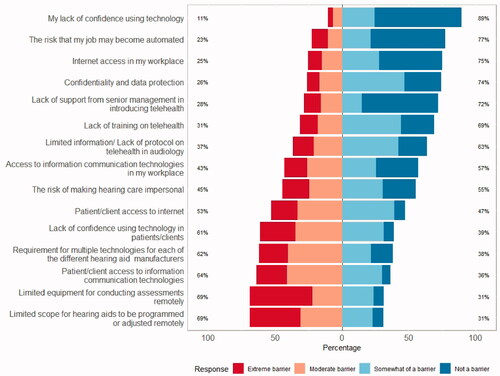
6 out of 15 proposed barriers to telehealth delivery were considered moderate/extreme by more than 50% (n = 101) of NHS respondents: (1) patient/client access to internet, (2) lack of confidence using technology in patients/clients, (3) requirement for multiple technologies for each of the different HA manufacturers, (4) patient/client access to information communication technologies, (5) limited equipment for conducting assessments remotely, (6) limited scope for HAs to be programmed/adjusted remotely.
Private HCPs appeared to perceive fewer proposed barriers as moderate/extreme barriers to delivery of telehealth. Only 3 received more than 50% (n = 13) ratings of moderate/extreme barrier to delivery of telehealth. These barriers were: (1) risk of making hearing care impersonal, (2) patient/client access to information communication technologies and (3) lack of confidence using technology in patients/clients.
Both NHS & private HCPs perceived patient/client access to information communication technologies as a barrier to telehealth delivery and lack of confidence using technology in patients/clients. Otherwise, the barriers concerning NHS respondents tended to focus on technology requirements or limitations (for patient access, conducting assessments & hearing aid programming). Private sector HCPs tended to rate these barriers as somewhat of/not a barrier but were more concerned about the risk of making hearing care impersonal.
A Wilcoxon rank sum test with continuity correction was conducted to compare ratings of barriers between NHS & Private sectors (excluding those respondents working in both), summarised in .
Table 2. Results of a Wilcoxon rank sum test with continuity correction was conducted to compare ratings of barriers between NHS & Private sectors.
The test showed that differences between groups were significant for the following: (2) Limited scope for hearing aids to be programmed or adjusted remotely (p < 0.001), (3) Requirement for multiple technologies for each of the different hearing aid manufacturers (p = 0.005), (4) Limited equipment for conducting assessments remotely (p < 0.001), (5) Access to information communication technologies in my workplace (p < 0.001), and (6) Confidentiality and data protection (p = 0.015).
Content analysis of the free text responses to the question “please add any further information regarding your experiences, thoughts or suggestions for teleaudiology” revealed five overarching categories surrounding challenges in delivering teleaudiology, namely, (i) teleaudiology barriers for certain services, (ii) service delivery difficulties (iii) safety concerns (iv) communication and (v) accessibility barriers, as seen in .
Respondents indicated that teleaudiology was difficult when dealing with patients with mental health difficulties, complex patients, doing diagnostics, paediatrics, mould adjustments and verifying hearing aid fittings. Teleaudiology also posed various service delivery challenges including the availability of suitable technology, being able to provide technical support, the availability of IT services to support, and the additional financial burden of obtaining the equipment. Data protection was considered more challenging, as well as ensuring staff had the required competence and confidence to use teleaudiology. Respondents were also concerned that changing working patterns would mean increased evening and weekend working and expectations of “out of hours” availability.
Safety concerns regarding teleaudiology included missing safeguarding cases, not having quality standards for teleaudiology, possibly missing pathologies and not detecting non-organic hearing loss. There were also concerns that the move to teleaudiology was not evidence-based. It was noted that the accessibility to teleaudiology would be particularly difficult for some with sight problems or severe hearing loss. Communication barriers were also mentioned due to technological failures during appointments and that building rapport and patient interaction was more difficult using teleaudiology ().
Table 3. Content analysis of the challenges of teleaudiology to audiology service delivery.
Discussion
National lockdown restrictions in response to the COVID-19 pandemic have forced UK hearing care services to use teleaudiology approaches even during periods when restrictions were lifted. It is likely that social distancing rules will remain in place for the foreseeable future and therefore the use of telehealth services will continue or increase further. Telehealth services have been available for many years and a small number of studies have been carried out to investigate HCP’s attitudes and opinions of teleaudiology (Singh et al. Citation2014; Eikelboom and Swanepoel Citation2016; Saunders and Roughley Citation2020; Ravi et al. Citation2018).
The results of the present survey highlight the use of teleaudiology before and after the outbreak of COVID-19, by private and public sector HCPs in the UK, including the views of HCPs and the barriers to carrying out remote consultations. A large proportion of respondents carried out telephone or email consultations with patients before the pandemic but rarely used video conferencing and remote hearing aid fitting/adjustment tool; consistent with findings by Singh et al. (Citation2014) but in contrast to reports by Saunders and Roughley (Citation2020) that only 32% of UK HCPs used teleaudiology before the pandemic. Previous surveys of American HCPs also reported a low number of clinicians using teleaudiology pre-COVID-19 (Schonfeld Citation2016). This discrepancy may be due to differences in HCPs’ understanding of the term telehealth which could lead to potential underestimates of usage.
Following implementation of COVID-19 restrictions, respondents in this survey continued utilising telephone consultations widely (73–87%) with some increase in video consultations (26%–39%). This appears to again contrast the Saunders and Roughley (Citation2020) report on use of remote consultation (39.1% paediatrics, 39.0% adult evaluations, 34.9% adult hearing aid fittings/follow ups, 65.7% tinnitus management and 29.1% vestibular care). It may again be that those respondents did not always consider telephone consultations a form of remote care and the responses were collated from 66 respondents in contrast with the 283 responses in this survey.
Although the COVID-19 pandemic has prompted the increased use of teleaudiology services provision, again this study highlights the variation in HCP’s views of teleaudiology tools across sector in the UK. The pandemic has also impacted the work patterns of private sector HCPs differently to HCPs in the public sector, with more working from home or furloughed (granted temporary paid leave under the government “Coronavirus job retention scheme”) throughout the national lockdown period. During the national lockdown, over nine million jobs were furloughed in the UK (Adams-Prassl et al. Citation2020). Within the hearing healthcare private sector, a higher proportion of HCPs from national chain organisations were furloughed compared to those from independent clinics ().
Overall, the majority of respondents reported feeling moderately comfortable with carrying out remote consultations (). Previous studies have reported that HCP’s willingness to use teleaudiology is dependent on the type of clinical activity performed as well as the patient population demographic (Singh et al. Citation2014; Saunders and Roughley Citation2020). The present study is the first to compare private sector and public sector teleaudiology provision in the UK. Results found HCPs of both sectors reporting similar levels of comfort in carrying out remote consultations. This is in contrast to practice in the US where publicly funded HCPs were found to have more positive attitude towards teleaudiology compared to private sector HCPs (Singh et al. Citation2014). It is also the first to ask UK based HCP respondents to define the term telehealth. The findings highlight a variation in understanding, with some respondents citing examples limited to telephone consultations whereas others reported use of the full range of communication technologies. Additionally, very few respondents cited examples of asynchronous telehealth service provision within their definition of telehealth. Asynchronous telehealth is also known as store-and-forward e.g. a patient may email symptoms (diary of hearing difficulties or hearing aid management difficulties) to the health professional (HCP) (Deshpande et al. Citation2009).
Overall, HCPs did not feel their access to internet and confidence in technology were barriers to teleaudiology uptake but reported barriers involving patient’s access and confidence in information communication technology and the internet. This is despite the steady decline in the number of internet non-users in the UK (17% of the population in 2011 and 7% in 2019) (Office for National Statistics. Internet Users Citation2019). HCPs also felt patient’s access to information communication technologies and their limited access to remote hearing aid adjustment software were barriers to the delivery of telehealth. However, these barriers differed between private sector and public sector HCPs ( and ). Barriers concerning NHS respondents centred around technology issues, consistent with Saunders and Roughley (Citation2020) findings that UK audiologists felt that lack of technological advancements was a barrier to performing teleaudiology diagnostic assessments. Technology and infrastructure have also been reported as barriers to telehealth uptake for audiology services globally (Eikelboom and Swanepoel Citation2016; Schonfeld Citation2016) and for non- audiology related telehealth services (Regina Molini-Avejonas et al. Citation2015). Flexibility within resource management and data storage in the private sector are likely to influence the significant differences between private and public sector audiology services observed in this study. In addition, private sector HCPs tend to have access to and are supported by multiple hearing device manufacturers. This could explain the significant differences between NHS and private providers rating of the “Requirement for multiple technologies for each of the hearing aid manufacturers” as a barrier to telehealth delivery ().
Muñoz et al. (Citation2020) reported rehabilitative audiology, including remote hearing aid fitting and adjustment, to be an area of significant potential for teleaudiology. Hearing aid fitting, adjustment, testing and counselling can be carried out through teleaudiology (Campos and Ferrari Citation2012). Many hearing aid manufacturers include teleaudiology features within their programming software so that adjustments can be carried out during a remote consultation. This method has been found to be successful and as effective as face to face consultations for adult patients (Novak et al. Citation2016) but more research is needed to assess this technique within the paediatric patient population and for populations with additional needs. Private sector respondents cited the risk of making hearing care impersonal as a barrier to carrying out remote consultations. Patients impression of telehealth has been generally positive (Barsom et al. Citation2021; Whealin et al. Citation2017) but these studies have been for non-audiology patients and there are likely to be specific characteristics of patients with hearing and tinnitus, e.g. difficulty communicating over telephone or video conferencing, that will influence the clinician-patient rapport.
In the present study respondents were invited to give their suggestions and additional comments about the use of teleaudiology. This opportunity allowed HCPs to report personal accounts of how teleaudiology has been used as well as specific barriers and considerations for future practice. Although some overlap was present between free text responses and the multiple-choice options identifying barriers to teleaudiology adoption, some additional barriers were reported. Firstly, there are some services that cannot be performed remotely e.g. ear mould modifications and the assessment and management of a patient with additional needs. Additionally, face to face consultations give clinicians the opportunity to informally assess a patient’s general wellbeing and provide onward referral to various other services if appropriate e.g. safeguarding services, social services or other medical practitioners. Remote consultations may restrict the availability of such incidental findings. Therefore, teleaudiology provision should be considered on a case-by-case basis. Respondents also reported the lack of quality standards or clinical guidance as a barrier to teleaudiology uptake. The British Academy of Audiology (BAA) and Manchester Centre for Audiology and Deafness (ManCAD) have produced a number of “Remote Working” documents which introduces HCPs to teleaudiology and gives brief practical guidance for hearing assessment and hearing aid fitting. In October 2020, the French Society of Audiology (FSA) published best practice recommendations for “Telemedicine in Audiology” (Thai-Van et al. Citation2020). The guidance addresses remote consultation conditions for hearing assessment, training of HCPs and specific considerations for the assessment and management of paediatric and elderly populations. Recommended procedures or best practice guidelines for teleaudiology provision should include practice advice for service provision and the triaging process as accessibility may vary between patient populations and their clinical needs. Finally, HCPs were concerned that the move to teleaudiology was not evidenced-based. A systematic review by Tao et al. (Citation2018) evaluated fourteen studies related to the use of teleaudiology for hearing aid fitting and follow up procedures and found that none demonstrated a high level of evidence (Tao et al. Citation2018). Teleaudiology has significant potential to help hearing healthcare services reach underserved communities but the evidence base requires strengthening (Swanepoel de and Hall Citation2010) to ensure effective, consistent, sustainable implementation in clinical practice.
Strengths and limitations
One of the main strengths of this study is the inclusion of a range of respondents both in terms of regional location and sector. There are also some limitations. Due to the nature of a snowball sampling approach, we are not able to report a survey response rate, and there is the inherent bias of a non-random selection procedure (Berg Citation2006). Also, due to the length of the survey, there were some respondents who did not complete it in full.
Conclusion
Understanding how hearing care professionals have adopted telehealth in response to the COVID-19 pandemic is important in assessing barriers to management of hearing loss in vulnerable populations and for populations living in underserved areas. This study highlights a variation in teleaudiology adoption across sector in the UK. A collaborative approach between hearing device manufacturers, research centres, HCPs and professional bodies would be beneficial for the creation of guidance and training materials for clinicians undertaking remote consultations in the UK. Additionally, consideration should be given to the variation in barriers across sector to better target resources and training materials. This could include a nationally coordinated approach to remove the technological barriers to teleaudiology, particularly for NHS services. Long term evaluation of teleaudiology provision, including the exploration of patient perspectives, and a future investigation of residual barriers to uptake is required to evaluate the impact of teleaudiology services, sustainability, and cost effectiveness. The present findings can facilitate comparison between teleaudiology service provision between countries and future work can include an investigation of international practice patterns.
Supplemental Material
Download MS Word (64.3 KB)Acknowledgments
We would like to thank the British Society of Audiology, British Academy of Audiology and the British Society of Hearing Aid Audiologists for distributing this survey. Many thanks to the individuals who helped review and pilot the survey. Our thanks are extended to the respondents who completed the survey.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Adams-Prassl, A., T. Boneva, M. Golin, and C. Rauh. 2020. “Furloughing.” Fiscal Studies 41 (3): 591–622. doi:https://doi.org/10.1111/1475-5890.12242.
- Barsom, E. Z., M. Jansen, P. J. Tanis, A. W. H. van de Ven, M. Blussé van Oud-Alblas, C. J. Buskens, W. A. Bemelman, et al. 2021. “Video Consultation during Follow up Care: effect on Quality of Care and Patient- and Provider Attitude in Patients with Colorectal Cancer.” Surgical Endoscopy 35 (3): 1278–1287. doi:https://doi.org/10.1007/s00464-020-07499-3.
- Berg, S. 2006. “Snowball Sampling—I.” In Encyclopedia of Statistical Sciences, edited by S. Kotz, C. B. Read, N. Balakrishnan, B. Vidakovic and N. L. Johnson. doi:https://doi.org/10.1002/0471667196.ess2478.pub2
- Brown, L., F. Mahomed-Asmail, K. C. D. Sousa, and D. W. Swanepoel. 2019. “Performance and Reliability of a Smartphone Digits-in-Noise Test in the Sound Field.” American Journal of Audiology 28 (3S): 736–741. doi:https://doi.org/10.1044/2019_AJA-HEAL18-18-0161.
- Bush, M. L., R. Thompson, C. Irungu, and J. Ayugi. 2016. “The Role of Telemedicine in Auditory Rehabilitation: A Systematic Review.” Otology & Neurotology 37 (10): 1466–1474. doi:https://doi.org/10.1097/mao.0000000000001236.
- Calvillo, J., I. Román, and L. M. Roa. 2015. “How Technology is Empowering Patients? A Literature Review.” Health Expect 18 (5): 643–652. doi:https://doi.org/10.1111/hex.12089.
- Campos, P., and D. Ferrari. 2012. “Teleaudiology: Evaluation of Teleconsultation Efficacy for Hearing Aid Fitting.” Jornal da Sociedade Brasileira de Fonoaudiologia 24: 301–308. doi:https://doi.org/10.1590/S2179-64912012000400003.
- Coco, L. 2020. “Teleaudiology: Strategies, Considerations during a Crisis and Beyond.” The Hearing Journal 73 (5): 26,28,29. doi:https://doi.org/10.1097/01.Hj.0000666404.42257.97.
- Deshpande, A., S. Khoja, J. Lorca, A. McKibbon, C. Rizo, D. Husereau, and A. R. Jadad. 2009. “Asynchronous Telehealth: A Scoping Review of Analytic Studies.” Open Med 3 (2): e69–91.
- Eikelboom, R. H., and W. Swanepoel. 2016. “International Survey of Audiologists' Attitudes toward Telehealth.” American Journal of Audiology 25 (3s): 295–298. doi:https://doi.org/10.1044/2016_aja-16-0004.
- Gagnon, M.-P., G. Godin, C. Gagné, J.-P. Fortin, L. Lamothe, D. Reinharz, A. Cloutier, et al. 2003. “An Adaptation of the Theory of Interpersonal Behaviour to the Study of Telemedicine Adoption by Physicians.” International Journal of Medical Informatics 71 (2–3): 103–115. doi:https://doi.org/10.1016/s1386-5056(03)00094-7.
- Graneheim, U. H., and B. Lundman. 2004. “Qualitative Content Analysis in Nursing Research: concepts, Procedures and Measures to Achieve Trustworthiness.” Nurse Education Today 24 (2): 105–112. doi:https://doi.org/10.1016/j.nedt.2003.10.001.
- Muñoz, K., N. K. Nagaraj, and N. Nichols. 2020. “Applied Tele-Audiology Research in Clinical Practice during the past Decade: A Scoping Review.” International Journal of Audiology : 1–9. doi:https://doi.org/10.1080/14992027.2020.1817994.
- Novak, R. E., A. G. Cantu, A. Zappler, L. Coco, C. A. Champlin, and J. C. Novak. 2016. “The Future of Healthcare Delivery: IPE/IPP Audiology and Nursing Student/Faculty Collaboration to Deliver Hearing Aids to Vulnerable Adults via Telehealth.” Journal of Nursing & Interprofessional Leadership in Quality & Safety 1 (1). Retrieved from http://digitalcommons.library.tmc.edu/uthoustonjqualsafe/vol1/iss1/1
- NVivo. 2018. Qualitative data analysis software, version 12. QSR International Pty Ltd.
- Office for National Statistics. 2019. “Internet users. 2015–2019.” https://www.ons.gov.uk/businessindustryandtrade/itandinternetindustry/bulletins/internetusers/2015#disability.
- Or, C. K., and B. T. Karsh. 2009. “A Systematic Review of Patient Acceptance of Consumer Health Information Technology.” Journal of American Medical Information Associatoin 16 (4): 550–560. doi:https://doi.org/10.1197/jamia.M2888.
- Ravi, R., D. R. Gunjawate, K. Yerraguntla, and C. Driscoll. 2018. “Knowledge and Perceptions of Teleaudiology among Audiologists: A Systematic Review.” Journal of Audiology and Otology 22 (3): 120–127. doi:https://doi.org/10.7874/jao.2017.00353.
- Regina Molini-Avejonas, D., S. Rondon-Melo, C. A. de La Higuera Amato, and A. G. Samelli. 2015. “A Systematic Review of the Use of Telehealth in Speech, Language and Hearing Sciences.” Journal of Telemedicine and Telecare 21 (7): 367–376. doi:https://doi.org/10.1177/1357633x15583215.
- Reginato, T. T. P., and D. V. Ferrari. 2014. “Teleaudiologia: comunicação profissional-paciente na programação e adaptação de aparelhos de amplificação Sonora individuais via teleconsulta.” Audiology - Communication Research 19 (3): 299–309. doi:https://doi.org/10.1590/S2317-643120140003000015.
- RStudio Team. 2020. RStudio: Integrated Development for R. PBC, Boston, MA RStudio.
- Saunders, G. H., and A. Roughley. 2020. “Audiology in the Time of COVID-19: Practices and Opinions of Audiologists in the UK.” Internation Journal of Audiology 60 (4): 255–262. doi:https://doi.org/10.1080/14992027.2020.1814432.
- Schonfeld, Y. The Use Of Telehealth By Audiologists: A Survey. Towson, Maryland: Towson University; 2016.
- Singh, G., M. K. Pichora-Fuller, M. Malkowski, M. Boretzki, and S. Launer. 2014. “A Survey of the Attitudes of Practitioners Toward Teleaudiology.” International Journal of Audiology 53 (12): 850–860. doi:https://doi.org/10.3109/14992027.2014.921736.
- Swanepoel de, W., and J. W. Hall. 3rd. 2010. “A Systematic Review of Telehealth Applications in Audiology.” Telemedicine Journal of E-Health 16 (2): 181–200. doi:https://doi.org/10.1089/tmj.2009.0111.
- Taherdoost, H. 2016. “Validity and Reliability of the Research Instrument; How to Test the Validation of a Questionnaire/Survey in a Research.” International Journal of Academic Research in Management 5: 28–36. doi:https://doi.org/10.2139/ssrn.3205040.
- Tao, K. 2020. Teleaudiology Hearing Aid Consultations for Adults: Towards Innovating the Service-Delivery in Clinical Practice. : The University of Western Australia.
- Tao, K. F. M., TdC. Moreira, D. M. P. Jayakody, D. W. Swanepoel, C. G. Brennan-Jones, L. Coetzee, et al. 2020. “Teleaudiology Hearing Aid Fitting Follow-up Consultations for Adults: single Blinded Crossover Randomised Control Trial and Cohort Studies.” International Journal of Audiology 1–12. doi:https://doi.org/10.1080/14992027.2020.1805804.
- Tao, K. F. M., C. G. Brennan-Jones, D. M. Capobianco-Fava, D. M. P. Jayakody, P. L. Friedland, D. W. Swanepoel, R. H. Eikelboom, et al. 2018. “Teleaudiology Services for Rehabilitation with Hearing Aids in Adults: A Systematic Review.” Journal of Speech, Language, and Hearing Research 61 (7): 1831–1849. doi:https://doi.org/10.1044/2018_JSLHR-H-16-0397.
- Thai-Van, H., D. Bakhos, D. Bouccara, N. Loundon, M. Marx, T. Mom, I. Mosnier, S. Roman, C. Villerabel, C. Vincent, and F. Venail. 2020. “Telemedicine in Audiology. Best Practice Recommendations from the French Society of Audiology (SFA) and the French Society of Otorhinolaryngology-Head and Neck Surgery (SFORL).” European Annals of Otorhinolaryngology, Head and Neck Diseases S1879-7296(20)30244-1. doi:https://doi.org/10.1016/j.anorl.2020.10.007
- Whealin, J. M., L. King, P. Shore, and J. Spira. 2017. “Diverse Veterans’ Pre- and Post-Intervention Perceptions of Home Telemental Health for Posttraumatic Stress Disorder Delivered via Tablet.” The International Journal of Psychiatry in Medicine 52 (1): 3–20. doi:https://doi.org/10.1177/0091217417703291.
- Whitten, P. S., and M. S. Mackert. 2005. “Addressing Telehealth's Foremost Barrier: provider as Initial Gatekeeper.” International Journal of Technology Assessment in Health Care. 21 (4): 517–521. Epub 2005/11/03. doi:https://doi.org/10.1017/s0266462305050725.
- You, S., W. Han, S. Kim, S. Maeng, and Y. J. Seo. 2020. “Reliability and Validity of Self-Screening Tool for Hearing Loss in Older Adults.” Clinical Interventions in Aging 15: 75–82. doi:https://doi.org/10.2147/cia.S238053.