Abstract
Objective
This study aimed to explore the short- and long-term effects of a second cochlear implant (CI-2) on the reduction of tinnitus annoyance and tinnitus handicap.
Design
In a combined retrospective and prospective cohort study, tinnitus annoyance was measured before receiving the CI-2 (Pre), more than two years after (Post1) and more than seven years after (Post2), using the Tinnitus Handicap Inventory (THI), the Visual Analog Scale for the assessment of perceived tinnitus loudness (VAS-L) and annoyance (VAS-A), and a self-report questionnaire.
Study sample
Twenty sequentially bilaterally implanted adults with bothersome tinnitus.
Results
CI-2 implantation resulted in a statistically significant reduction of tinnitus handicap from severe at Pre to mild at Post1 (THI mean score reduced from 61.3 [SD = 19.4] to 29.3 [SD = 23.5]). The reduction in tinnitus annoyance was statistically significant from Pre to Post 2 (VAS-A reduced from 7.1 [SD = 1.5] to 3.4 [SD = 2.2]). The reduction in tinnitus loudness was not statistically significant.
Conclusions
The provision of a CI-2 for severely and profoundly hearing-impaired individuals with bothersome tinnitus is an effective method of providing long-term tinnitus relief.
Introduction
The term tinnitus describes the conscious perception of an auditory sensation in the absence of a corresponding external stimulus (Baguley, McFerran, and Hall Citation2013). The most common form of tinnitus is a subjective, auditory and distressing phantom phenomenon (Pattyn et al. Citation2016). Hazell (Citation1998) argued that tinnitus first becomes a problem when the sound represents a threat, when the sound is constantly intrusive, or when the patient experiences tinnitus as a stress factor.
Henry, Dennis, and Schechter (Citation2005) showed evidence in their review article that the prevalence of tinnitus in adults falls in the range of 10 to 15%. For severely and profoundly hearing-impaired individuals, a prevalence of tinnitus of between 66 and 86% was reported in a systematic review by Quaranta, Wagstaff, and Baguley (Citation2004). Martines et al. (Citation2010) argued that approximately one-third of the population in western societies experience tinnitus at least once in their life and approximately 1 to 5% develop serious psychological complications.
Tinnitus-related activity in the nervous system is hypothesised to be present in every human being. The tinnitus signal is usually perceived as a weak sound that is not bothersome or intrusive. It may be influenced by cochlear pathology. Tinnitus and hearing deficits are thus often related phenomena (Martines et al. Citation2010). The comorbidities of tinnitus, such as anxiety or depression, is often reported, as is the association with a reduced quality of life (Halford and Anderson Citation1991; Falkenberg, Tungland, and Skollerud Citation2003; Mo, Lindbaek, and Harris Citation2005; Falkenberg and Wie Citation2012). It is also reported that patients with tinnitus score low on self-esteem and well-being assessments (Krog, Engdahl, and Tambs Citation2010).
Cochlear implants (CIs) as a tinnitus treatment
In recent decades, a considerable number of treatment methods for tinnitus annoyance have been suggested and tested. Tinnitus retraining therapy (Jastreboff Citation2007), which focuses on the habituation of reactions evoked by tinnitus and the subsequent habituation of tinnitus perception, is one of the more successful methods. Cognitive behavioural therapy, which is a structured, time-limited psychological therapy that involves a systemic collaboration between therapist and patient to establish common goals in treatment (Beck Citation1979), is another. Good treatment effects have also been observed following the provision of unilateral and bilateral cochlear implants (CIs) to adults with severe and profound hearing impairment in addition to annoying tinnitus.
The tinnitus suppressing effect of CIs has been compared with the functionality of a tinnitus masker, which is provided to individuals with normal hearing or mild to moderate hearing loss to either ‘drown’ the tinnitus with other sounds or facilitate the habituation. Other explanations for the tinnitus-suppressing effect of CI stimulation include the direct electrical stimulation of the cochlear nerve and the reorganisation of the central auditory pathways and associative cerebral areas. It is also possible that the implantation surgery itself has a tinnitus-reducing effect, due to the positive expectations of the patients regarding receiving a CI (Bovo, Ciorba, and Martini Citation2011). The latter is in line with the neurophysiological explanation of tinnitus, which states that stress and negative events in a person’s life may activate the limbic and autonomic nervous systems and create negative emotions that can trigger the tinnitus annoyance, while positive events may do the opposite.
In the last couple of decades, a body of evidence has been established that unilateral CIs provided to bilaterally hearing impaired persons have a dampening effect on tinnitus. The review study by Quaranta, Wagstaff, and Baguley (Citation2004) found that CI use was associated with a reduction of tinnitus intensity and awareness in up to 86% of patients, and sometimes with an exacerbation of it (up to 9%). In the study by Bovo, Ciorba, and Martini (Citation2011), 51 post-lingually, profoundly hearing-impaired adults were asked to scale tinnitus loudness and annoyance before, and six months after CI activation with the Tinnitus Handicap Inventory (THI) questionnaire. In total, 36% of the participants reported total loudness suppression and another 42% reported a reduction. Annoyance scores were reduced in 75% of patients and the THI-score was reduced in 72% of patients. In a study by Kim et al. (Citation2013), the THI-score was decreased for all patients (n = 35) after receiving a CI and the tinnitus was eliminated in about half of the patients. The most severe cases had the greatest benefit. Finally, Liu et al. (Citation2016) showed that cochlear implantation led to a decrease in average THI-scores in a group of 234 participants.
There is, not surprisingly, also increasing evidence that simultaneously implanted bilateral CIs have a corresponding tinnitus-suppressing effect. It must be noted that sequential and simultaneous bilateral CIs are only offered as treatment of profound hearing impairment in a limited number of countries. Ramakers et al. (Citation2015) found an overall reduction of tinnitus in their systematic review on the effect of bilateral cochlear implantation on tinnitus, but none of the included primary studies offered a high level of evidence. van Zon et al. (Citation2016) investigated the effect of both unilateral and simultaneous bilateral cochlear implantation on tinnitus perception in a group of 38 profoundly hearing impaired patients. They found a significant decrease in the THI for both groups. However, for six participants, five in the bilateral and one in the unilateral group, the tinnitus increased or was induced by the cochlear implantation itself.
In some cases, bilaterally hearing impaired CI recipients have first been provided with a unilateral implant and have later been offered a second CI, if the tinnitus has not, or has only partly, been reduced after the first implantation. Investigation into the effect of a second CI on tinnitus has been sparsely conducted. Summerfield et al. (Citation2006) showed that the changes in tinnitus observed by providing 24 severely hard-of-hearing patients with bilateral CIs do not significantly differ from the changes that accompany a unilateral CI. In contrast, Olze et al. (Citation2012) found that treatment with a second CI led, not only to better hearing and a reduction of tinnitus annoyance, but also to an increased quality of life and increased psychological well-being; this study was conducted with a group of 40 patients whose inter-implant interval was 3.6 ± 4.0 years and who completed a German self-report tinnitus questionnaire before and after the activation of the first and second CI. In a multi-centre study by Ramakers et al. (Citation2017), the effect of a second implant after three years was investigated for 38 bilaterally, simultaneously and sequentially implanted adults. In the simultaneous group, tinnitus scores fluctuated three years after implantation, and a total suppression of tinnitus burden occurred in four out of nine participants. In the sequential group, the tinnitus had disappeared or decreased in four out of seven participants after a three-year follow-up period.
In summary, the abovementioned studies have shown that there often is a decrease in tinnitus after unilateral cochlear implantation, although an increasing burden of tinnitus has also been reported. The effect of a second implant on tinnitus reduction for those who experience remaining or increased tinnitus in their contralateral ear has been subject to little investigation, and this study thus adds to the sparsely conducted research in this field.
Aim
This study aimed to explore the effect of a second CI on tinnitus, measured before receiving a second CI, in the short term (>2 years) and in the long term (>7 years), for severely and profoundly hearing-impaired persons with a single-sided CI suffering from annoying tinnitus.
Materials and methods
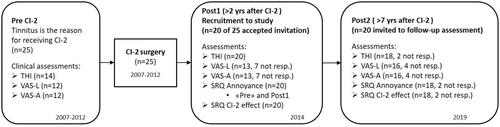
We chose a combined retrospective and prospective design for this study. Tinnitus annoyance was measured before receiving the CI-2 (Pre), more than two years after (Post1) and more than seven years after (Post2). Retrospective data collected before the participants received CI-2 was retrieved from medical records, and prospective data was collected after they agreed to participate. The prospective data collection included questions on tinnitus annoyance experienced before receiving CI-2.
Participants
Twenty-five adult patients provided with sequential bilateral CIs due to tinnitus annoyance were invited to participate in this study. They received the sequential CI between 2007 and 2012, and the study invitation was sent in 2014. Thus, all had used bilateral CIs for more than two years at the time they were asked to participate. Twenty of the patients responded to the invitation— four men and sixteen women. All participants had undergone CI surgery at the Department of Otorhinolaryngology, Head and Neck Surgery, Oslo University Hospital, and all who were granted a second CI as tinnitus treatment were invited to participate. Their mean age at the time of the first CI was 47.4 years (SD = 15.0; range = 23.0–72.5 years). Mean inter-implant interval was 4.9 years (SD = 4.3, range = 0.9–19.4 years). The participants’ demographic information is given in .
Table 1. Demographics in the cohort of patients provided with sequential bilateral CIs due to tinnitus annoyance (N = 20).
Informed written consent was obtained from all participants according to the guidelines of the Declaration of Helsinki (World Medical Association Citation2018). The Regional Committees for Medical and Health Research Ethics in Norway and the data protection officer at Oslo University Hospital approved the project.
Procedure
First, tinnitus was classified for clinical purposes before the CI-2 surgery for the 20 participants, using two instruments: the Tinnitus Handicap Inventory (THI) and the Visual Analogue Scale for the assessment of chronic tinnitus annoyance (VAS-A) and loudness (VAS-L). Second, THI, VAS-A and VAS-L was used for the same 20 participants as part of this project two and seven years after the activation of CI-2. In addition, a self-report questionnaire (SRQ) developed for this study was used to assess each patient’s experience with a second CI related to tinnitus annoyance and loudness.
Complete THI-scores before CI-2 activation (Pre), more than two years after receiving the CI-2 (Post1) and after a further 5 years (Post2) were available for 12 participants, and complete VAS-A- and VAS-L-scores at Pre, Post1 and Post2 were available for 9 participants. The largest part of the missing data is from the period before implantation of CI-2 and is due to the THI and VAS not tested or the completed questionnaires not retrieved, although the tinnitus handicap was documented in the patient files for all participants. For details, see and .
Table 2. Individual and group results for THI total, VAS Loudness, VAS Annoyance, SRQ Annoyance and SRQ CI-2 effect at Pre, Post1 and Post2 time-points (N = 20).
Materials
The THI is a 25-item self-report inventory of tinnitus impact on daily living (Newman, Jacobson, and Spitzer Citation1996). Guidelines for the grading of tinnitus severity with the THI were developed by McCombe et al. (Citation2001), who suggested the tinnitus handicap scale: slight (0–16), mild (18–36), moderate (38–56), severe (58–76), and catastrophic (78–100). The THI has been widely validated and translated into many languages. The Danish validation (Zachariae et al. Citation2000) suggests that the Danish THI-Total scale may be a reliable and valid indicator of general tinnitus-related distress that can be used in a clinical setting to quantify the impact of tinnitus on daily living. The Danish THI has been translated into Norwegian and the Norwegian version was recently validated (Heggdal et al. Citationin press). The Norwegian translation of the THI has been in clinical use for more than 15 years.
The VAS was chosen to measure tinnitus loudness (VAS-L) and annoyance (VAS-A). The participants were asked to set marks on two horizontal lines with endpoints anchored by “tinnitus not audible” and “tinnitus not annoying” (corresponding to 0), and “tinnitus extremely annoying” and “tinnitus extremely loud” (corresponding to 10). The VAS is frequently used to measure changes in tinnitus annoyance and loudness, and Adamchic et al. (Citation2012) found good test reliability and validity for the VAS-L and VAS-A; the minimally clinically identifiable difference (MCID) estimates were between 10 and 15 points when VAS results were measured using the endpoints 0 and 100, corresponding to MCID estimates between 1 and 1.5 when using the endpoints 0 and 10.
An SRQ was constructed for this study and designed to assess the self-reported effect of the CI-2 on tinnitus, to compensate for the missing THI and VAS data pre CI-2. The questionnaire was quality checked by an educational and a technical audiologist, each with more than 20 years’ clinical experience, before using it in the research project. It contained the following questions about tinnitus annoyance before and after CI-2 activation (SRQ Annoyance):
To what extent did you experience your tinnitus as annoying before the second implant? (response at time-point Post1 and referred to as the variable SRQ Annoyance ‘Pre’.)
To what extent did you experience your tinnitus as annoying after the second implant? (responses at time-points Post1 and Post2.)
The response alternatives were as follows: 1 – no annoyance, 2 – moderate annoyance and 3 – considerable distress.
The questionnaire also contained the following question on the overall effect of the CI-2 on tinnitus loudness (SRQ CI-2 effect):
What effect did the second implant have on the tinnitus loudness? (response at time-point Post2.)
The response alternatives for this question were as follows: 1 – reducing effect, 2 – no effect and 3 – amplifying effect.
Statistical analyses
Repeated measures analyses of variance (RMANOVAs) were used to determine the mean differences of the THI, VAS-A, and VAS-L at the time-points Pre, Post1, and Post2, and this reduced the data sets to 12 participants for the outcome measure THI and to nine participants for the outcome measures VAS-L and VAS-A. A Greenhouse–Geisser correction was used if the sphericity assumption was violated (which was the case for THI and VAS-A, but not for VAS-L). Statistical significance was defined as p < 0.05, and post-hoc testing using Student’s t tests was used to discover which specific pairwise means differed. A Bonferroni correction was used to keep the Type I error at 5% overall.
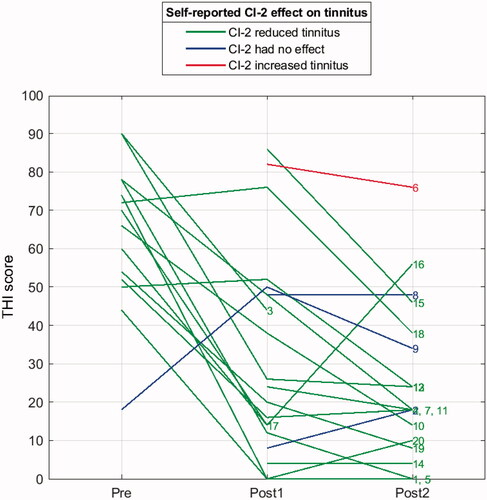
The reported answers from the SRQ were only counted and reported as distributions (). Answers on SRQ question 3 at Post 2, which reported the effect of CI-2 on tinnitus burden, were used to colour the lines in , which shows the individual THI answers at the time-points (Pre, Post1, and Post2). The lines showing a descending THI value from Pre via Post1 to Post2 should match a reported effect of CI-2 (e.g., answer to SRQ question 3 equal to 1 [reducing effect] is shown with green lines).
Figure 2. The Pre, Post1 and Post2 THI-scores for all 20 participants. The colours of the lines show the self-reported CI-2 effect (SRQ-score) on tinnitus from Post1 to Post2; the red line represents the participant who experienced increased tinnitus, the blue lines represent those who experienced no effect following CI-2 implantation and the green lines represent those who experienced a reduction in their tinnitus handicap after the CI-2 implantation. The number to the right of each line represents the patient identification, presented in .
All statistical analyses were performed by using SPSS v. 26.0 (SPSS Inc., Chicago, IL, United States).
Results
Individual and group characteristics
An overview of individual and group characteristics for the THI, VAS-A, VAS-L and SRQ is shown in .
The line–plot of individual THI–scores in shows that all participants except three experienced a decrease in perceived tinnitus two years after their CI-2 activation, and all except three experienced a further reduction or had a stable score after an additional five years (i.e., from Post1 to Post2). Among the three who had an increased score, only one had a relatively large increase in THI-score, going from a score of 14 to 56. Still, this participant reported that the CI-2 had a positive effect on tinnitus (SRQ = 1), illustrated by a green line in . Furthermore, the SRQ CI-2 effect measured at time-point Post 2 revealed that after receiving the CI-2, 16 participants experienced a reduction of tinnitus, 3 experienced no reduction and 1 experienced an increase.
The SRQ Annoyance ‘Pre’ (), which contains a retrospective view of the tinnitus annoyance before the patients received CI-2, shows that 17 participants reported 3 (considerable distress) and three reported 2 (moderate annoyance). At time-point Post1, only three reported SRQ tinnitus annoyance 3 (considerable distress), 11 reported annoyance 2 (moderate annoyance), and six reported annoyance 1 (no annoyance). At time-point Post2, the self-reports are quite similar to the self-reports at Post1; two still reported SRQ tinnitus annoyance 3 (considerable distress), 10 reported annoyance 2 (moderate annoyance) and six reported annoyance 1 (no annoyance). Two did not report on SRQ Annoyance at time-point Post2.
Short–term and long–term effects
shows a box-and-whisker plot of subgroups of the participants who had a complete set of THI (n = 12), VAS-A (n = 9) and VAS-L (n = 9) assessments at the Pre, Post1 and Post2 time-points.
Figure 3. Box-and-whisker plots showing the THI-, VAS-A- and VAS-L-scores at the Pre, Post1 and Post2 time-points for the participants with complete THI (n = 12), VAS-A (n = 9), and VAS-L (n = 9) assessments throughout the study period. One asterisk (*) indicates a statistically significant difference, with p < 0.05. The means are marked with x in the same plots for each assessment (i.e., Pre, Post1 and Post2).
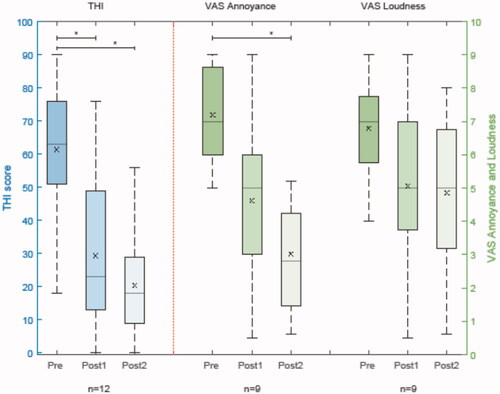
A RMANOVA with Greenhouse–Geisser correction determined that the mean THI- scores differed significantly between Pre, Post1 and Post2 (F[1.17, 18.89] = 15.4, p < 0.0005). Since time-points revealed a significant main effect, post-hoc tests using Student’s t tests and Bonferroni correction were used to understand the effect; the tests revealed that the decrease in THI-score from Pre to Post1, from 61.3 (SD = 19.4) to 29.3 (SD = 23.5), was statistically significant (p = 0.014); however, the further decrease in THI-score to 20.3 (SD = 16.3) from Post1 to Post2 was not statistically significant (p = 0.496).
The mean VAS-A differed significantly between Pre, Post1 and Post2 (F[1.32, 10.58] = 11.43, p = 0.004). Post-hoc tests using Bonferroni correction revealed that the decrease in the VAS-A from Pre to Post1 from 7.1 (SD = 1.5) to 4.9 (SD = 2.5) was not statistically significant (p = 0.165). The mean VAS-A was also reduced from Pre to Post2, from 7.1 (SD = 1.5) to 3.4 (SD = 2.2), and this was statistically significant (p = 0.002). The mean VAS-L did not differ significantly between Pre, Post1 and Post2 (F[1.93, 15.45] = 1.9, p = 0.184). The mean VAS-L was 6.8 (SD = 1.8) at Pre, and it reduced to 5.4 (SD = 2.4) at Post1 and to 5.0 (SD = 2.6) at Post2.
Discussion
The present study found a significant long–term reduction in self-perceived tinnitus severity following the implantation of a second CI in a population of patients with persistent bothersome tinnitus following first CI activation. The THI-score measured before and a minimum of two years after the implantation of a second CI showed a decrease from a severe to a mild tinnitus handicap. The mean decrease in the VAS-A (4.2 from Pre to Post2) is about three times larger than the MCID estimate of between 1 and 1.5 for the VAS-A and VAS-L, reported by Adamchic et al. (Citation2012). A minimum of seven years after CI-2 implantation, a long–term effect was confirmed for both general tinnitus handicap (THI) and tinnitus annoyance (VAS-A). For tinnitus loudness (VAS-L), a significant long–term effect of CI-2 activation was not found.
Our results are in line with those of Olze et al. (Citation2012), looking specifically at their results for participants with high tinnitus questionnaire (TQ) scores, which are comparable to the THI-scores in the present study. Olze et al. (Citation2012) split the group of participants into two subgroups; those with a TQ score above or equal to 47 (high score) and those with a TQ score below 47 (low score). The study found that those with high tinnitus annoyance obtained a statistically significant reduction in TQ score, while those with moderate tinnitus annoyance did not obtain a significant TQ score reduction. Generally, all participants in our study had a high THI-score (above 44) prior to CI-2 activation, with the exception of one participant, who had a mild tinnitus handicap (i.e., a THI-score of 18). Our results show that in average, the whole group of participants experienced an improvement in tinnitus annoyance after CI-2 activation.
Our study, that of Olze et al. (Citation2012) and that of Ramakers et al. (Citation2015) all indicated that bilaterally severely and profoundly hearing impaired patients often benefit from two CIs to suppress their tinnitus. However, Summerfield et al. (Citation2006), reached the opposite conclusion; they found that the first implant decreased the tinnitus annoyance of the participants, while the second implant increased their tinnitus annoyance. This may be due, at least in part, to the use of a non-validated questionnaire in that study. Comparing our study with the three other studies mentioned above, we see that the sample sizes are all rather small and that the instruments that have been used to measure tinnitus annoyance do not allow for direct comparisons.
Our study includes a time span of approximately seven years between the provision of the CI-2 and the last assessment of tinnitus annoyance. This is more than twice the time span covered by the studies of Ramakers et al. (Citation2017), who investigated tinnitus outcomes three years after simultaneous and sequential cochlear implantation (N = 38), and Kraaijenga et al. (Citation2019), who investigated tinnitus outcomes two years after bilateral implantation (N = 38). Thus, the current study adds significantly to the knowledge of the field and confirms that the implantation of a second CI provides a durable tinnitus relief.
Limitations
This combined retrospective and prospective study had several limitations. Although tinnitus severity was an inclusion criterion for a second CI, tinnitus severity is self-reported and may be due to selection bias. In the data collection period, Norwegian guidelines only allowed for a second implant in patients with both profound hearing loss and another handicap, such as severe tinnitus, and as such, we cannot exclude the possibility of an over-reporting of tinnitus.
Furthermore, the outcomes should be interpreted with caution due to the small sample sizes of the groups, the lack of a control group and the self-report data being collected only in the subgroup of patients who received a second CI during the study period. The study included 20 participants, but for the comparison of the mean scores at the Pre, Post1 and Post2 time-points in the analysis of the VAS-A and VAS-L, only the 9 participants who had completed ratings at all three time–points were included. This rather small number of participants could cause non-significant results even if differences exist, and we need more participants to detect the mean differences.
The misclassification of THI- and VAS-scores is unlikely to have occurred, as these questionnaires have been validated; however, the SRQ was constructed for this study and has not been validated. The SRQ results are therefore possibly less reliable.
Conclusions
Tinnitus annoyance is often reduced after a severely or profoundly hearing–impaired person receives a unilateral CI; however, contralateral hearing loss can still be accompanied by tinnitus, which requires a second implant. Our study confirms that a second CI is an adequate treatment for tinnitus handicap and tinnitus annoyance in patients with a unilateral CI and contralateral hearing impairment with accompanying tinnitus. The long–term results show that the implantation of a second CI provides a durable tinnitus relief.
Disclosure statment
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be interpreted as a potential conflict of interest.
Acknowledgements
The authors are grateful to the CI users who participated in this study.
References
- Adamchic, I., B. Langguth, C. Hauptmann, and P. A. Tass. 2012. “Psychometric Evaluation of Visual Analog Scale for the Assessment of Chronic Tinnitus.” American Journal of Audiology 21 (2): 215–225. doi:https://doi.org/10.1044/1059-0889(2012/12-0010).
- Baguley, D., D. McFerran, and D. Hall. 2013. “Tinnitus.” The Lancet 382 (9904): 1600–1607. doi:https://doi.org/10.1016/S0140-6736(13)60142-7.
- Beck, A. T. 1979. Cognitive Therapy of Depression. New York: Guilford Press.
- Bovo, R., A. Ciorba, and A. Martini. 2011. “Tinnitus and Cochlear Implants.” Auris, Nasus, Larynx 38 (1): 14–20. doi:https://doi.org/10.1016/j.anl.2010.05.003.
- Falkenberg, E.-S., O. P. Tungland, and S. Skollerud. 2003. “Habituation Therapy of Chronic Distressing Tinnitus: A Presentation of a Treatment Programme and an Evaluation Study of Its Effects.” Audiological Medicine 1 (2): 132–137. doi:https://doi.org/10.1080/16513860301715.
- Falkenberg, E.-S., and O. B. Wie. 2012. “Anxiety and Depression in Tinnitus Patients: 5-Year Follow-up Assessment after Completion of Habituation Therapy.” International Journal of Otolaryngology 2012: 1–7. doi:https://doi.org/10.1155/2012/375460.
- Halford, J. B. S., and S. D. Anderson. 1991. “Anxiety and Depression in Tinnitus Sufferers.” Journal of Psychosomatic Research 35 (4-5): 383–390. doi:https://doi.org/10.1016/0022-3999(91)90033-k.
- Hazell, J. W. P. 1998. “Management of Tinnitus.” In Diseases of the Ear, edited by H. Ludman & T. Wright, 202–215. London: Arnold.
- Heggdal, P. O. L., L. P. Aarsnes, K. J. Brännström, and H. J. Aarstad. in press. “Psychometric Properties of the Norwegian Translation of the Tinnitus Handicap Inventory (THI-NOR).” International Journal of Audiology 1–6. doi:https://doi.org/10.1080/14992027.2021.1922769
- Henry, J. A., K. C. Dennis, and M. A. Schechter. 2005. “General Review of Tinnitus: prevalence, Mechanisms, Effects, and Management.” Journal of Speech, Language, and Hearing Research : JSLHR 48 (5): 1204–1235. doi:https://doi.org/10.1044/1092-4388(2005/084).
- Jastreboff, P. J. 2007. “Tinnitus Retraining Therapy.” In Progress in Brain Research, edited by B. Langguth, G. Hajak, T. Kleinjung, A. Cacace & A.R. Møller, 415–423. Amsterdam: Elsevier.
- Kim, D.-K., S.-C. Bae, K.-H. Park, B.-C. Jun, D.-H. Lee, S.-W. Yeo, and S.-N. Park. 2013. “Tinnitus in Patients with Profound Hearing Loss and the Effect of Cochlear Implantation.” European Archives of Oto-Rhino-Laryngology : Official Journal of the European Federation of Oto-Rhino-Laryngological Societies (Eufos) 270 (6): 1803–1808. doi:https://doi.org/10.1007/s00405-012-2193-2.
- Kraaijenga, V. J. C., G. G. J. Ramakers, Y. E. Smulders, A. van Zon, R. H. Free, J. H. M. Frijns, W. J. Huinck, R. J. Stokroos, and W. Grolman. 2019. “No Difference in Behavioral and Self-Reported Outcomes for Simultaneous and Sequential Bilateral Cochlear Implantation: Evidence from a Multicenter Randomized Controlled Trial.” Frontiers in Neuroscience 13 (54): 1–17. doi:https://doi.org/10.3389/fnins.2019.00054.
- Krog, N. H., B. Engdahl, and K. Tambs. 2010. “The Association between Tinnitus and Mental Health in a General Population Sample: Results from the HUNT Study.” Journal of Psychosomatic Research 69 (3): 289–298. doi:https://doi.org/10.1016/j.jpsychores.2010.03.008.
- Liu, Ying, Hong Wang, Dong Xu Han, Ming Hua Li, Yu Wang, and Yu Li Xiao. 2016. “Suppression of Tinnitus in Chinese Patients Receiving Regular Cochlear Implant Programming.” The Annals of Otology, Rhinology, and Laryngology 125 (4): 303–310. doi:https://doi.org/10.1177/0003489415611907.
- Martines, F., D. Bentivegna, E. Martines, V. Sciacca, and G. Martinciglio. 2010. “Assessing Audiological, Pathophysiological and Psychological Variables in Tinnitus Patients with or without Hearing Loss.” European Archives of Oto-Rhino-Laryngology 267 (11): 1685–1693. doi:https://doi.org/10.1007/s00405-010-1302-3.
- McCombe, A., D. Baguley, R. Coles, L. McKenna, C. McKinney, and P. Windle-Taylor. & 2001. “British Association of Otolaryngologists, Head and Neck Surgeons. 2001. Guidelines for the Grading of Tinnitus Severity: The Results of a Working Group Commissioned by the British Association of Otolaryngologists, Head and Neck Surgeons.” Clinical Otolaryngology and Allied Sciences 26 (5): 388–393. doi:https://doi.org/10.1046/j.1365-2273.2001.00490.x.
- Mo, B., M. Lindbaek, and S. Harris. 2005. “Cochlear Implants and Quality of Life: A Prospective Study.” Ear and Hearing 26 (2): 186–194. doi:https://doi.org/10.1097/00003446-200504000-00006.
- Newman, C. W., G. P. Jacobson, and J. B. Spitzer. 1996. “Development of the Tinnitus Handicap Inventory.” Archives of Otolaryngology-Head & Neck Surgery 122 (2): 143–148. doi:https://doi.org/10.1001/archotol.1996.01890140029007.
- Olze, H., S. Grabel, H. Haupt, U. Forster, and B. Mazurek. 2012. “Extra Benefit of a Second Cochlear Implant with Respect to Health-Related Quality of Life and Tinnitus.” Otology & Neurotology : official Publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology 33 (7): 1169–1175. doi:https://doi.org/10.1097/MAO.0b013e31825e799f.
- Pattyn, T., F. Van Den Eede, S. Vanneste, L. Cassiers, D. J. Veltman, P. Van De Heyning, and B. C. G. Sabbe. 2016. “Tinnitus and Anxiety Disorders: A Review.” Hearing Research 333: 255–265. doi:https://doi.org/10.1016/j.heares.2015.08.014.
- Quaranta, N., S. Wagstaff, and D. M. Baguley. 2004. “Tinnitus and Cochlear Implantation.” International Journal of Audiology 43 (5): 245–251. doi:https://doi.org/10.1080/14992020400050033.
- Ramakers, G. G. J., V. J. C. Kraaijenga, Y. E. Smulders, A. van Zon, I. Stegeman, R. J. Stokroos, R. H. Free, et al. 2017. “Tinnitus after Simultaneous and Sequential Bilateral Cochlear Implantation.” Frontiers in Surgery 4: 1–8. doi:https://doi.org/10.3389/fsurg.2017.00065.
- Ramakers, G. G. J., A. van Zon, I. Stegeman, and W. Grolman. 2015. “The Effect of Cochlear Implantation on Tinnitus in Patients with Bilateral Hearing Loss: A Systematic Review.” The Laryngoscope 125 (11): 2584–2592. doi:https://doi.org/10.1002/lary.25370.
- Summerfield, A. Q., G. R. Barton, J. Toner, C. McAnallen, D. Proops, C. Harries, H. Cooper, et al. 2006. “Self-Reported Benefits from Successive Bilateral Cochlear Implantation in Post-Lingually Deafened Adults: Randomised Controlled Trial.” International Journal of Audiology 45 (sup1): 99–S107. doi:https://doi.org/10.1080/14992020600783079.
- van Zon, Alice, Yvette E. Smulders, Geerte G. J. Ramakers, Inge Stegeman, Adriana L. Smit, Gijsbert A. Van Zanten, Robert J. Stokroos, et al. 2016. “Effect of Unilateral and Simultaneous Bilateral Cochlear Implantation on Tinnitus: A Prospective Study.” The Laryngoscope 126 (4): 956–961. doi:https://doi.org/10.1002/lary.25493.
- World Medical Association [WMA] 2018. WMA Declaration of Helsinki—Ethical principles for medical research involving human subjects. Retrieved from https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/
- Zachariae, R., F. Mirz, L. V. Johansen, C. B. Pedersen, S. E. Andersen, P. Bjerring, and C. B. Pedersen. 2000. “Reliability and Validity of a Danish Adaptation of the Tinnitus Handicap Inventory.” Scandinavian Audiology 29 (1): 37–43. doi:https://doi.org/10.1080/010503900424589.