Abstract
Background
Single-sided deafness presents communication challenges for adults. There are a range of care options, including CROS hearing aids, available but little is known about patient preferences for these interventions.
Objective
The objective of this study was to understand the viewpoints of patients making decisions about audiological interventions they use.
Methods
A constructivist worldview using thematic analysis to undertake a constant comparative analysis of 8 semi-structured interviews.
Sampling
Participants were recruited from Portsmouth Hospitals University NHS Trust audiology service in England.
Findings
The results of the study describe ongoing iterative judgements being made by participants, informed by their access to information, effectiveness of audiological interventions, stigma, barriers to accessing care, and constant cost-benefit analyses being made. The key factors involved in decision-making by individuals with Single-sided deafness (SSD) are discussed.
Conclusions
This study represents the first in-depth exploration of the individual’s lifeworld related to which factors influence use of different audiological interventions by individuals with SSD. It highlights the complex and ongoing nature of how decisions are made by these individuals and identifies the need for greater information provision by clinicians, such as through use of a decision aid tool.
Background
Single-sided deafness (SSD) is a unilateral or asymmetric hearing loss where hearing in the worse hearing ear is of a severe-to-profound level and normal or near-normal in the better hearing ear (Van de Heyning et al. Citation2016; NICE Citation2018). The prevalence of SSD in the general population is variable but is estimated to be between 3% and 6%, increasing with age (Ross et al. Citation2010; Shargorodsky Citation2010). Incidence of congenital SSD in the new-born population is 1 in 3700 (Mehl and Thomson Citation2002).
Individuals with SSD can experience a reduced quality of life, increased social isolation, high levels of hearing-related disability, and difficulty in localisation of sound (Wie, Pripp, and Tvete Citation2010; Iwasaki et al. Citation2013; Brodie, Smith, and Ray Citation2018; Lucas, Katiri, and Kitterick Citation2018).
There are a range of interventions to improve access to sound available to individuals with SSD. These include both surgical and non-surgical options, depending on the aetiology of the hearing loss (Krishnan and Van Hyfte Citation2016). Audiological interventions consist of conventional hearing aids, contra-lateral-routing-of-signal (CROS) devices, bone-conducting devices (BCDs), and cochlear implants (CIs) (Dillion Citation2012; Krishnan and Van Hyfte Citation2016). CROS, BCD and CIs have been shown to improve quality of life and speech perception in background noise and to reduce listening difficulty compared to unaided controls (Akeroyd, Brennan-Jones, and Suller Citation2012; Blasco and Redleaf Citation2014; Kitterick, Lucas, and Smith Citation2015; Peters et al. Citation2015; Kitterick, Smith, and Lucas Citation2016; Snapp et al. Citation2017). The main interventions for SSD utilised by the National Health Service (NHS) in the United Kingdom are CROS, BCDs, and conventional hearing aids (NHS England Citation2016). The recommended care pathway for individuals with SSD in the NHS involves initially trialling a conventional hearing aid, followed by a CROS device, and then a BCD (NHS England Citation2016; NICE Citation2018). The current guidance for eligibility of adult patients for consideration of CI within the NHS includes a requirement for bilateral severe-profound hearing loss (NICE Citation2019). This means that the adult patient population with SSD accessing care through the NHS in the UK are ineligible for this intervention.
Previous research into factors influencing decision-making in audiology have largely focussed on the uptake of conventional hearing aids by older adults with presbycusis (Knudsen et al. Citation2010; Laplante-Lévesque, Hickson, et al. Citation2012; Meyer, Hickson, and Fletcher Citation2014; Pryce et al. Citation2016). However, this research demonstrates concordance with the existing evidence of factors affecting decision making by individuals with SSD. The results for both populations indicate a significant social component to decision-making, with significant others, cost, and stigma affecting uptake and help-seeking behaviour (Laplante-Lévesque, Hickson, and Worrall Citation2010; Laplante-Lévesque, Knudsen, et al. Citation2012; Pryce et al. Citation2016). Additionally, the provision of information about care options and available interventions are almost exclusively controlled by audiologists, with their communication skills and adherence to shared-decision making influencing patient awareness of care options (Poost-Foroosh et al. Citation2011; Pryce et al. Citation2016).
The existing research on decision-making by individuals with SSD has almost exclusively focussed on use of BCDs, specifically Bone Anchored Hearing Aids (BAHATM) (Zawawi et al. Citation2014; Siau et al., Citation2016; Ng et al. Citation2017). There is evidence of improved quality of life, localisation, and functional access to sound through use of a BAHATM (Ihler et al., Citation2014; Snapp et al. Citation2017). Patient uptake of a BCD is between 29% to 50% (Zawawi et al. Citation2014; Siau et al. Citation2015). The main identified reasons for rejection of a BCD were cosmetic concerns, indicating social influences, and a lack of subjective benefit by the user (Pennings, Gulliver, and Morris Citation2011; Zawawi et al. Citation2014; Siau et al. Citation2015; Ng et al. Citation2017). Little is known about the patient’s perspective of CROS devices despite their common and recommended use in management of this population’s hearing loss. This means that little is known about what informs patients’ decisions and uptake of hearing care. In turn, this means that clinicians do not have information about patient concerns, values, and preferences. Clinicians need this information to promote shared decision making and engage patients (Dahlberg, Todres, and Galvin Citation2009).
The present study aimed to describe how adult patients with Single-sided deafness (SSD) make decisions about their audiological care in the NHS by:
Identifying key features of decision-making in these patients regarding whether to proceed or refuse audiological interventions (hearing technology or no treatment) for their hearing loss.
Identifying patient preferences for their care and interactions with the NHS about audiological interventions.
Methods
This study used a qualitative methodology based on narrative and thematic analysis approaches (Charmaz Citation2008; Braun and Clarke Citation2013; Alemu et al. Citation2015). A social constructivist approach was taken to reflect the worldview that individuals have multiple lived experiences and differing perceptions of the world (Urquhart Citation2013; Charmaz Citation2017). As the study was conducted without research funding, no formal Patient Public Involvement (PPI) activities were undertaken. Ideally PPI should form a core part of research activity, informing both research design and conduct (Garfield et al. Citation2016; Jennings et al. Citation2018). Without adequate resourcing there is a risk of tokenistic PPI (Jinks et al. Citation2016). Full PPI requires training, time and support of PPI participants (Garfield et al. Citation2016; Jinks et al. Citation2016). Unfortunately, without external funding this was not possible in this case.
Potential participants were identified from an English NHS Trust (Portsmouth Hospitals University NHS Trust) Audiology department through review of patient notes and clinic letters. Recruitment occurred between January and February 2020. Purposive sampling was utilised to ensure a broad range of interventions and demographics were represented by the study sample (Braun and Clarke Citation2013). Once potential participants were identified they were invited to participate in the study. Those who volunteered were contacted by the researcher (TU) to be invited to interview.
Ethical approval was obtained from the Health Research Authority (25 November 2019) after proportionate review and approval by the East of England – Cambridge South Research Ethics Committee (25 November 2019 [REC reference: 19/EE/0283]).
Eight interviews were conducted face to face. Participants were 46–72 years old (mean age 62 years). All participants were Caucasian British. Six of the participants were female (75%) and two were male (25%). Participants were either currently using, planning to use, or had used, a range of audiological interventions including CROS/BICROS, conventional hearing aids, and BAHATM. For full details see . Participants had a range of aetiologies of their SSD, see for full details. These features were in keeping with the typical clinical caseload in this location in England. The researcher (TU) has audiological training and is accustomed to adapting communication to enable participants to hear. As these were individuals with SSD, the quiet interview environment was important but otherwise, no particular adaptations were required.
Table 1. Demographics of participants.
Interviews were conducted either at two clinical locations in the South West of England.
Interviews were semi-structured, utilising an initial interview guide. The open questions used as prompts were:
Tell me how you came to be using/not using your assistive listening devices/hearing aids
Tell me about your thoughts about hearing loss and using your assistive listening devices/hearing aids
Tell me about your feelings about hearing loss and using your assistive listening devices/hearing aids
What is important to you when deciding whether to use hearing devices/aids?
Has this changed over time?
Who else is important in helping you decide?
Is there anything else you would like to tell me?
Interviews progressed to explore themes and concepts as these emerged (Charmaz Citation2008; Urquhart Citation2013). Interviews were 16–55 min long. The interviews were audio recorded and transcribed verbatim by the researcher. Field notes and memos were made by the researcher during and after interviews to capture non-verbal expressions and body language of participants.
Data analysis
Data analysis took place alongside data collection. Data were analysed through line-by-line open coding (where meaning is assigned through a code to the interview transcripts). Open codes were compared between and within transcripts in an iterative process after each interview in accordance with the constant comparative method of data analysis (Charmaz Citation2008).
Results
The data were analysed for key meanings, and these were labelled “codes”. This enabled data to be broken down and compared between transcripts. The codes were eventually combined into themes which provided the basis for the descriptive findings.
“In-vivo” coding was utilised where possible to remain close to the participant’s meaning for the first three interviews (Charmaz Citation2008). Codes were initially developed by the researcher and were compared to a second researcher’s (HP) interpretation. The subsequent five interviews were analysed using theoretical coding, generated from the three initial interviews. Codes were correlated and utilised to define 12 initial thematic categories. These 12 categories were used to analyse interviews four to six, after which further theoretical integration resulted in 11 thematic categories, which were used to analyse interviews seven and eight. Integration of codes into broader descriptive themes resulted in six main themes that captured variance in the data set.
Findings
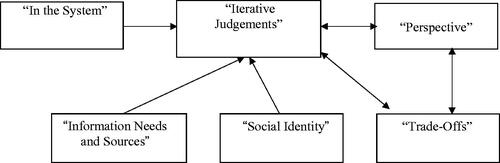
The final descriptive framework is based on thematic analysis within the data set. There were consistent factors, which were key in influencing participant’s decision-making. These included interactions with clinicians, access to care, access to information, awareness of the options of care available to them, and evaluation of the risks and benefits for these interventions (). These findings describe how decisions are made by participants.
Theme – iterative judgements
The theme “Iterative Judgements” informed and dictated decision-making throughout the process. This theme provided an overarching framework for the decision-making of all participants. This theme describes an ongoing process of constant evaluation, reassessment, and searching for options. This is an active process of considering risk versus benefit, alongside an awareness of having a limited number of options of hearing technology. All participants described their experience of using hearing aids as an ongoing process of trial and error or a journey through the options available to them. For example, “that’s still probably an area of trial and error” (P2) and “if we ever get to a stage of ‘don’t know what we’re going to do’ that might be very difficult” (P4). All participants expressed that they had experienced uncertainty about trialling various hearing aids, often due to a lack of clarity about the benefit this change may provide; “Would it work better than what I’ve got?” (P3). All but one participant (P1) framed their journey in terms of a proactive and ongoing search for interventions, even for those who were happy with their current hearing aids; “Very willing to try anything if it helps” (P3) and “Nothing appeals because you don’t know if it works or not” (P8). There is an ongoing search for improvement and several participants referred to both ongoing innovation in hearing aid technology and their hope for a cure; “And I'm hoping that with research and things like that, that things are going to improve, you know, because they're still quite antiquated” (P7). This search is an iterative process, based on the experience participants have of hearing aids and their past decisions to exclude or use other hearing aids. All participants described an ongoing evaluation of risks and benefits. This often involved evaluating the physical discomfort and practicalities of using a hearing aid against any benefit provided through using it; “they did try a few different things like that to find something comfortable” (P6). As part of this ongoing process, the risks and benefits involved in having surgery for a BCD were also considered by participants. Those participants who had previous experience of major surgery were less negative about the risks or perceived seriousness of the BCD as an intervention than those who did not have previous experience of surgery; “It could upset my brain in my head but that’s part and parcel… it doesn’t bother me” (P4), “Was like having a filling at the dentist” (P2), “I didn’t want the invasion… I didn’t want to lose my facial nerve” (P7), “It’s a very serious operation” (P8). The perceived permanence of a BCD was a consideration for all the participants who were using, or had considered using, a BCD; “the hair would never come back… [BAHATM] plugged in the side of your head” (P3). This was part of the view that the BAHATM represented a serious and, often, last case option if no other options had worked; “the magnet [BAHATM] is going to be my last-ditch attempt” (P4), “it’s a drastic measure” (P1).
This process of cost-benefit analyses was not static and often changed over time, as the management of their hearing loss changed priority for the participants. This change in prioritisation consisted of multiple factors. For those participants still in work, or who had had experience of working while they had a hearing loss, difficulties in this environment were a key factor in using hearing aids; “I trained as a nurse originally, I was going to retrain but I got on the wards and I just couldn't, you can't function” (P6). Participants who had retired, or were close to retiring, described that the perceived importance of using amplification often declined once out of work; “Had I been older and nearer retirement I wouldn’t have bothered” (P2), “I’m older now so I don’t need this and that” (P5). Alongside this, several older participants described the cost-benefit of hearing aids in terms of their expectations of benefit over their remaining lifespan, often negatively; “I don't know if any sort of surgery would have improved it, but I think at that age, it would have been perhaps worth having. Maybe not now, bit over the hill” (P6). In contrast to this, almost all participants detailed that having more free time once they had retired or no longer had young families was more favourable to exploring the options of hearing aids. This was because they had more time and management of their hearing loss became a greater priority once the pressures of family life were reduced; “Lots of things affected when you’re young…Having a young family and busy” (P5), “I was serious because when you're younger, other things matter don't they” (P8).
The use of different hearing aids as part of a journey back to being normal was explicitly described by three participants, two of whom had experienced sudden hearing losses and a third who developed hearing loss as a result of Meniere’s disease. The desire to be normal formed a core part of the drive to explore and use hearing aids for these participants; “I’m willing to try anything to get hearing back… I just want to be as normal as I can again” (P4), “I’d rather be as normal as I could” (P3).
All participants described that there were limited available hearing aid options; “You haven’t got a choice of hearing aids” (P8), “The only other options I had was the CROS aid…I wasn’t offered any other choice” (P7), “I didn’t have any options” (P6), “I haven’t had a choice of hearing aids” (P3). A perception of limited options appeared to contribute to the constant re-evaluation of the effectiveness of each option, as well as analysis of risks and benefits of the other options. This highlights the impact of limited options on cost-benefit analyses undertaken by participants influenced by, and influencing, the theme “Trade-offs”.
Participants described an ongoing process of constant re-evaluation of their hearing aid options, with effectiveness a key consideration. However, this is a multi-factorial process influenced by concerns about the seriousness of surgery, the priority given to management of hearing loss by participants, barriers to care, and information about their options. These factors clearly relate to the role of the other themes in decision-making, with the theme “Iterative Judgements” forming the core integrating influence. These factors are within the wider context of participants viewing their hearing aid use as an ongoing process of trial-and-error and as having few options available to them. This creates a sense of high threshold of investment, and in creating an impetus for change, if hearing aids provide some level of benefit. This was especially apparent given uncertainty often being present about other options, due to issues accessing information and expert opinion [See “Information Needs and Sources” for more details].
Theme – in the system
Multiple aspects of the theme “In the System” influenced decision-making, interlinked with the themes “Information Needs and Sources” and “Perspective” through the core theme of “Iterative Judgements”. Participants expressed a medicalised view of their hearing loss and of the process of exploring and trialling different hearing aids. A hearing loss was described as a deficit to be corrected; “I’m willing to try anything to get hearing back… I just want to be as normal as I can again” (P4).
The use of medical language by all participants exhibits the influence of clinicians in providing information, as well as the way this information was internalised by participants. This is related to the accessibility of care and the theme of “Information Needs and Sources”. Access to information was repeatedly described by participants as being key to decision-making and that this information was often only available once already accessing hearing-related care. A medicalised view of hearing loss and intervention options appears implicit in the hope of some participants for a cure or future developments in technology to improve hearing aid function. This concept is related to the key theme of “Iterative Judgements” and the sub-themes of “Searching for Improvements” and “Hope”.
Access to care was described by all but one participant as being poor and difficult to access both appointments and clinicians; “Took quite a while for them to refer me to Audiology” (P4), “The appointment system is quite difficult” (P7). Difficulties accessing care (for example, audiology and ENT services) were described as barriers by participants; “I dropped off the radar” (P1), “Went with that rather than going through the various stages” (P2).
The burden of multiple appointments and of ongoing investigations, for health concerns other than hearing loss and those related to their hearing loss, appears to contribute to the participant’s views of their need to prioritise different aspects of healthcare over addressing their hearing difficulties; “Being in [another hospital] so frequently in the last two years” (P2). In this instance, Participant 2 described that their other health concerns required frequent appointments at other hospitals, resulting in Participant 2 not accessing hearing-related care as they perceived this as an additional burden that they were unable to meet. This again relates closely to the key theme of “Iterative Judgements” in that this is a constant re-evaluation and reprioritisation of their health needs and the effort required to meet these needs, rather than a static or defined threshold which clearly motivates help-seeking by participants.
The perceived barriers to access (including the burden of multiple appointments for hearing and non-hearing related care, dismissal of concerns by professionals, and of accessing appropriate services) and barriers to understanding (through use of technical and complex language) all contributed to ongoing evaluations of the costs of seeking help. This was for both initial help-seeking and subsequent explorations of different intervention options. Participants expressed a general conclusion that the threshold for seeking help depended on their ability to cope with their hearing loss. They expressed that the difficulty and burden of navigating the health-care system, even if they were already accessing care, was outweighed only if benefit from their current hearing aid was not sufficient for their needs.
Theme – social identity
Preferences were informed by the theme of “Social Identity”. This relates to the social stigma and appearance of the various interventions available to participants. This was expressed by participants through implicit and explicit concerns about how use of the hearing aid would change, or had changed, how other people perceived or treated them; “People that don’t know me would treat me differently” (P1). No participant described the appearance of any of the interventions positively. Participants expressed negative or ambivalent views about the appearance and visibility of all interventions, even if they had not trialled the intervention itself; “Probably at the beginning, I wouldn't have liked to go around with them [being] visible” (P6). For some participants, the appearance of the various hearing aids was a factor in rejecting them; “Didn’t like the idea of having something on the outside of my head” (P7), “I don’t want to be recognised as old” (P5), “I just didn’t fancy the, the peg in the head” (P3). All but two participants (Participants 2 and 6) explicitly described stigma associated with hearing aids as factoring into their process of decision-making. However, even these two participants acknowledged that appearance played a role in shaping their perceptions of hearing technologies: “Probably at the beginning, I wouldn't have liked to go around with them [being] visible” (P6).
A reoccurring and consistent concern was visibility and how discrete the hearing aid would be, often compared in a trade-off with benefit versus the perceived negative of the hearing aid’s appearance; “You don’t see many people going round with a BAHATM. People might have thought there was something else going on as well” (P3). This has a clear relationship and influence on the core theme of “Iterative Judgements” alongside the theme of “Trade-Offs”. Those participants who did explicitly express stigma about hearing aids often did so in relation to prejudices about hearing aids being ugly, prominent, and used only by old people, with an implicit rejection of these on this premise; “Deafness is an old age thing…Deaf bat… This big monstrosity” (P5), “[hearing aids look] like artificial limbs” (P7), or a “box on your head” (P8).
This informed their “Iterative Judgements” in that participants were variable in their willingness to trial various interventions, often reaching a key decision-point where potential or actual benefit outweighed the cost of stigma; “Nowadays, I don’t care, they help me to, sort of, function” (P6), “I had my hair long so I could cover them up” (P4) . This key decision-point was a trade-off between effectiveness of their current intervention, perceived benefit of alternative options, and the social cost of stigma or appearance. There was evidence of both consideration of external social judgments and stigma (e.g. “Deafness is an old age thing” P5) and of internal changes in self-perception (e.g. “you tend to think of them as being an old person having, you know, hearing aids” P7).
Theme – information needs and sources
The preferences for “Information Needs and Sources” had an influence on the process of decision- making by participants. Participants received and sought out a range of information from clinicians, the lived experiences of peers, and from other information sources, such as charities. This theme has a clear impact on the key theme of “Iterative Judgements”, as participants expressed a desire for reliable and complete information. This information provides the basis for their consideration and perception of various interventions. Information was viewed by some participants as not being fully available with evident frustration or confusion about not feeling, or being, fully informed of all options at various points in their care pathway; “Don’t know whether this is as good as you can get” (P3), “Never heard of the BAHATM before” (P7), “You have to raise concerns for somebody to give you the options” (P6). However, this was partly the result of previous experiences with health services over many years and ongoing development of new technologies which were not originally available on the NHS or at the time of their initial hearing loss; “I… don’t know how long ago they brought them out” (P6).
There were variable levels of perceived access and the completeness of information about the different interventions available to support decision-making. All participants expressed frustration at a perceived lack of, or difficulty in, accessing information, some of which was experienced during historic interactions with clinicians; “At no time did they ever say have something to help” (P1), “Don’t know what they [hearing aids] do” (P3), “Never had any discussion about type” (P2). This related to the desire for reliable and trustworthy information expressed by most participants, which was perceived as being of limited availability outside of expert opinion and specific information sources, such as the NHS and charities; “there's so much advertising about hearing aids… And they, I think, they're giving you the wrong information” (P7). Participants felt that at their current state in their pathway they were well informed, often singling out clinicians for the quality of information provided; “[I] had all the information from Clinician A” (P8).
Participants detailed difficulty in accessing expert opinions as part of the barriers to care discussed in the theme “In the System”. The clinician has a role as a gatekeeper of information, due to perceptions of their expertise, in expectation setting and understanding of the available interventions; “Clinician A… has been totally honest all the way through” (P4) and “they know an awful lot more about these things than you do” (P3). Participants all described experiences of being dismissed by health-care professionals at various points; “Maybe they could see I wasn’t interested so didn’t give me much option” (P5) and “[The audiologist] said you can try them but they won’t work” (P4).
Additionally, participants described conducting their own research to gather information on the various interventions; “I just…Googled it” (P4), “I read in a magazine about the BAHATM” (P6). This was despite acknowledgement of this information being perceived as not trustworthy.
There was a consistently expressed experience of searching for, or encountering, the lived experience of others. This was in the form of peers, online and face-to-face support groups, and family and friends; “I did research a little bit, to look to see…how people got on with it” (P3), “An acoustic neuroma support group and a Facebook support group… conversations with people on there and … a BAHATM support … group” (P2). There were contrasting experiences, at the extremes being a highly positive or negative experience for different participants; “it’s been really, really good… they are very informative” (P7), “I wish I'd never gone there…opened a field of terror” (P2). The lived experience of peers was given more weight by participants in their decision making, as while some participants did discuss the experience of friends and family with hearing aids, this was not central to decision-making.
There was a sense of abandonment expressed by participants after hearing aid fittings, often explained by perceived demands on clinician’s time and the health service as a whole, which interrelates with the theme “In the System”; “Here’s the hearing aid, off you go, come back in three months” (P7), “Get your hearing aids off you go” (P6). Once in the system, participants described variable levels of shared-decision making in their care, ranging from proactivly seeking out options for hearing aids to a passive role, whereby clinicians occupied a dominant role in directing and leading on care decisions; “Why was I given this one and not the other one” (P2).
Participants all expressed a preference for information on all the available options. Further to this, access to information and knowledge of available options factored into participant’s cost-benefit analysis, with fewer options leading to greater consideration of when, or if, to change to using a different hearing technology (e.g. “You have to raise concerns for somebody to give you the options” P6).
Theme – perspective on coping with hearing loss
Participant’s preferences were to improve coping with their hearing loss. This informed their expectations of any hearing aids they used, often with effectiveness in providing benefit being key to their decision-making. This related to the theme “Trade-Offs” in that benefit from the hearing aid is a key positive that is balanced against perceived costs, such as stigma, and any hearing aid must be effective to be worth the costs of using it.
All participants described functional difficulties resulting from their hearing loss; “it has severely impacted my life…I experience isolation” (P4), “I couldn’t function” (P6). The hearing in the better ear was described as having mitigated the impact of their hearing loss by two participants; “[I have] such good hearing in my other ear it compensated” (P7), “Hasn’t really affected me” (P5).
The difficulties reported were not different between participants who experienced a sudden or progressive hearing loss. Almost all participants did not identify a key decisional moment as being a single driver of seeking help. This is especially true in those individuals who have lived with their SSD for many years and described an ongoing process of trialling hearing aids. However, those participants who had experienced a sudden loss of hearing also described help-seeking in these terms; “This is the last bit that we’ve got to sort out” (P4), “Struggled on” (P2). This was often related to a constant search for improvement of hearing or hearing aids as part of participant’s iterative judgements.
Four participants expressed the influence of their other health conditions on forming their perspective of their hearing loss. All four stated that their hearing loss had less impact on their life than their other conditions; “Been through Meniere’s” (P3), “Only thing I would like to get rid of is the tinnitus” (P5), “I don’t feel disabled with my hearing problem” (P7).
The ability of participants to cope dictated their threshold for help-seeking. Increased hearing related disability was the main driver of seeking help. The cost of hearing-related difficulties were considered when forming cost-benefit judgments about use of different hearing technologies. There were constant attempts by participants to balance the benefits (for example, improved awareness of sound and localisation) and costs which included stigma, difficulty accessing information, anxiety about surgery, and the burden of ongoing appointments.
Theme – Trade-Offs
The theme of “Trade-Offs” revealed a core aspect of decision making. Participants explicitly expressed that effectiveness of hearing aids was a core goal of using them. Comparisons with previous experiences of using, or not having, hearing aids formed the basis of judging subjective benefit from each hearing aid.
Conventional hearing aids and wired CROS aids were often described as not providing much benefit with the trade-off of often also being uncomfortable and associated with stigma (see the theme “Social Identity” for further details). Wireless BI/CROS aids were described as providing some degree of benefit in the form of improved localisation and access to sound on their poorer hearing side by most participants who had used these; “it’s brilliant… It was a revelation” (P6), “Does help is all I’d say” (P3).
The two participants who had received an implanted BAHATM found it provided significant benefit through improved access to sound in various situations, improved localisation, and help with hearing in noise. However, one of these participants had had to have theirs removed due to infection of the abutment: “it's fabulous. Absolutely life changing” (P2), “BAHATM by far the best… absolutely brilliant” (P4). Those participants who did not proceed with the option of an implanted BAHATM were influenced by their experience of a soft-band trial and lack of effectiveness from this; “Ruled out the BAHATM because it didn’t work” (P7). Further to this, considerations over the process of surgery, appearance, and permanence of the BAHATM influenced decision-making, reflecting the broad multi-factorial process involved in participant’s choices of hearing aid. This is described further in “Iterative Judgements”, as well as demonstrating the strong interplay of factors such as stigma and effectiveness on decision- making. This process of ongoing evaluation of trade-offs is pivotal in the iterative decision-making by participants. Benefits and costs are constantly evaluated and re-examined by participants, both of current, past, and future options. This is informed by all other categories and forms a constant feedback to the process of “Iterative Judgments” based on benefit from the hearing technology used by participants.
Discussion
This decision-making framework for individuals with SSD is the first to be generated in the literature with an inductive grounding in participant derived data. The framework for decision-making encompasses a range of lifestyles, ages, and aetiologies of SSD. These multiple factors have led to the creation of a broad framework which captures and accurately reflects the diversity of experiences and aspects of participant decision-making.
There is increasing recognition of the importance of the patient’s lifeworld in clinical decision making (Braun and Clarke Citation2019). The lived experience of patients in healthcare involves, according to Habermas’ theory of communicative action (Habermas Citation1984), the holistic subjective, emotional, and objective background to making a decision (Walseth and Schei Citation2011). All these domains were clearly expressed as being fundamental to decision-making by participants in this study. Instances of non-congruence between participants and healthcare professionals were often the result of social and emotional aspects of participant’s lifeworlds not being fully understood or considered by clinicians. The understanding of patient’s needs beyond the traditional objective focus of the bio-medical model is often lacking in clinical encounters (Walseth and Schei Citation2011; Meyer, Hickson, Lovelock, et al. Citation2014). This lack of holistic engagement has been reported previously, whereby audiologists dominate clinical conversations and often do not fully engage with patient concerns and preferences to facilitate shared decision-making (Dillon and Pryce Citation2020; Manchaiah et al. Citation2019).
The findings of this study reflect the influence non-audiological factors, as also found in previous research, have on decision-making, such as convenience (the time burden of multiple appointments and difficulty of accessing care) (Laplante-Lévesque, Hickson, and Worrall Citation2010; Dillon and Pryce Citation2020). Cosmetic or appearance related concerns have been major reasons given consistently for rejecting a BAHATM (Siau et al. Citation2015; Ng et al. Citation2017; Wendrich et al., Citation2017). This study confirms this and explores further the balance between external social pressures and internal self-perception changes which make up these concerns. Use of hearing aids and BCDs are influenced by concerns over appearance, associated with changes about self-image and perceived negative stereotypes (Laplante-Lévesque, Hickson, and Worrall Citation2010; Southall, Gagné, and Jennings Citation2010; Lucas, Katiri, and Kitterick Citation2018). Stigma has been reported in older adults with acquired hearing loss, whereby their hearing loss means they feel negatively perceived and stigmatised by others, reducing willingness to seek help and to use hearing aids (Southall, Gagné, and Jennings Citation2010; Meyer and Hickson Citation2012). This study provides an insight into the pervasive stigma described by participants with SSD and a similar influence of the influence of social perception, as detailed in “Social Identity”. Reluctance to use hearing aids results in part from changes in self-perception, “ageism,” “vanity,” and the belief that hearing aids make users look old (Wallhagen Citation2010; Preminger and Laplante-Lévesque Citation2014). This study provides evidence that these changes in self-perception occur in individuals with SSD as well. The rejection or acceptance of a BCD due to stigma has not previously been able to be related to the social and internal consideration of participant’s lifeworld, such as ageism (Siau et al. Citation2015, Citation2016; Ng et al. Citation2017). As such, this study provides novel insights into this aspect of participant’s experiences and the influence these have on their subjective and emotional lifeworld domains relating to decision making. This is especially through the identical concerns identified in “Social Identity” theme when compared to previous research in older adults with hearing loss.
Previous research indicates that a patient’s journey to the point of help-seeking involves a build-up to “critical junctures” which are partly formed by “cues to action” composed of an inability to cope or a triggering event (Carson Citation2005; Southall, Gagné, and Jennings Citation2010). This critical juncture can then lead to the decision to seek help for hearing loss. This is concordant with the findings of “Iterative Judgements” as being ongoing and constant evaluations of trade-offs (Southall, Gagné, and Jennings Citation2010). This constant evaluation of trade-offs relating to use of hearing technology forms the core aspect of how decisions were made by participants and reflects similar processes in patients deciding whether to proceed with implantation of a CI (Dillon and Pryce Citation2020). The threshold of help-seeking for participants was varied but all described a desire to reduce their hearing disability as a main motivation for seeking help. This supports previous reports of hearing disability driving help- seeking in individuals with SSD or age-related hearing (Meyer, Hickson, Lovelock, et al. Citation2014; Ng, et al. Citation2017)
Effectiveness of hearing aids was identified as a key consideration in decision making. Participants considered potential and actual benefit from their options of hearing technology in an ongoing process, as described in the theme “Iterative Judgements”. This supports findings that benefit was the most frequently reported reason for proceeding with implantation of a BAHATM and, equally, limited benefit was the main reason for rejection of a BAHATM (Pennings, Gulliver, and Morris Citation2011; Saroul et al. Citation2014; Siau et al. Citation2015, Citation2016; Ng, et al. Citation2017; Wendrich et al., Citation2017). Supporting the importance of subjective benefit is that the benefit from use of a conventional hearing aid in older adults with acquired hearing loss was key to their continued use of the hearing aid (Meyer, Hickson, and Fletcher Citation2014; Korkmaz et al. Citation2016). This study is the first to explore the holistic consideration by individuals with SSD of effectiveness of various hearing technologies, rather than solely regarding rejection or acceptance of a BAHATM. The importance of benefit from the hearing technology resides in the wider context of trade-offs between usability, effectiveness, preference for other hearing aids (conventional or CROS aids) and the risks of surgery (Siau et al., Citation2016; Ng, et al. Citation2017; Wendrich et al., Citation2017). These inter-related factors are detailed in the theme “Trade-offs” and concord with previous research, supporting the inter-relationship of multiple factors in decision-making as indicated in this study’s decision-making framework.
While some participants did not express anxiety about surgery, often due to previous experience of surgery, others did not proceed with BAHATM implantation due to these concerns. This is consistent with other studies which have shown anxiety about the prospect of surgery being a common reason for rejecting a BAHATM (Faber et al. Citation2012; Siau et al., Citation2016; Ng, et al. Citation2017; Wendrich et al., Citation2017). The risks associated with surgery have also been found to influence decision making in individuals considering CI surgery (Dillon and Pryce Citation2020). Alongside this, the perceived permanence of the intervention was an explicit consideration of the iterative nature of decision-making for participants, most often regarding implantation of the BAHATM. This demonstrates the multi-factorial nature of decision-making and the interplay between the perceptions of surgery and permanence (“Iterative Judgments”) and potential benefits and effectiveness (“Trade-offs”). This represents the first time that the perceived permanence of interventions (such as BCDs) has been reported as a consideration for individuals with SSD, similar to previous concerns reported by adults with acquired age-related hearing loss (Laplante-Lévesque, Hickson, and Worrall Citation2010).
The principles of shared decision making (SDM) state that patients should be fully informed about all treatment options and information provision to patients is integral to this (Coulter and Collins Citation2011 ). SDM is a core principle of the NHS Long-Term Plan (Department of Health, 2019). However, audiologists have been found in a clinical setting to not explicitly present patients with all treatment options and instead attempt to problem solve, as well as not fully consider the patient’s goals, emotional content of consultations, and patient preferences (Pryce et al. Citation2016, Citation2018). This relates to the subjective aspects of a patient’s lifeworld and participants in this study consistently expressed that they felt they had not had good access to information at some point in their care journey. This lack of information does not support SDM and indicates that at some point in their care participants were unable to fully engage with professionals to make informed decisions, similar to the conclusions of previous investigations (Southall, Gagné, and Jennings Citation2010). The theme “Information Needs and Sources” highlights that participant’s access to information was a core part of their ability to make decisions about their care. Information has also been found to be key to decision making in individuals considering CI (Dillon and Pryce Citation2020).
This study provides detailed reasoning and descriptions of the value that participants with SSD attach to information, such as that it is from a trustworthy source which most participants identified as being health-care professionals. This expands on Ng, et al. (Citation2017) findings that clinicians and the internet are the main source of information for patients with SSD about their hearing technology options. As found in this study, other research indicates access to information has been variable and has had an influence on an individual’s decision to proceed with BAHATM implantation or continuing to use conventional or CROS hearing aids (Ng, et al. Citation2017).
The role of the clinician as a gatekeeper of information is supported by this previous research and that participants in this study found clinicians a key source of information. Previous studies indicate that audiologists have a powerful position as an expert within consultations, in keeping with the biomedical model (Southall, Gagné, and Jennings Citation2010; Pryce, Hall, and Marks et al. Citation2018). Audiologists dominate clinical conversations and often do not fully engage with patient concerns and preferences to facilitate shared decision-making, especially as technical and complex language is a barrier to patient understanding (Manchaiah et al. Citation2019). This previous research supports the findings from this study, demonstrating that participants with SSD need good access to information, as this influences their decision-making, alongside reduction of barriers to understanding through simple language. This aspect of accessing care through information, consideration of participant’s preferences, and medicalisation is a recurrent part of the theme “In The System”.
This qualitative study provides further theoretical evidence for the preferences of patients in audiology. The findings are concordant with other studies of patient preferences (Pryce et al. Citation2016; Pryce et al. Citation2018). The themes were checked by comparing researcher interpretations (TU & HP) and reflection on the researcher role enabled reflexivity. Member checking was not used as this study aimed to provide novel theoretical insight (Thomas Citation2017) and not description. The researchers were audiology professionals, trained in qualitative research methods but were unknown to the participants. There was limited variation in participant demographics, other than age. Future research should examine the potential for socioeconomic factors to influence decision-making. In other research demographics and socio-economic status have been found to influence decision-making about hearing aid use in older adults with acquired hearing loss (Vestergaard Knudsen et al., Citation2010; Meyer and Hickson Citation2012; Tahden et al. Citation2018).
Conclusions
Individuals with SSD have a complex multi-factorial and iterative process of decision-making from the findings of this study, which is supported by a wide range of previous research. This study represents a novel contribution of how individuals with SSD make decisions about their hearing technology and the various factors that influence this, namely with an integration of external and internal aspects of an individual’s life world (Habermas Citation1984; Walseth and Schei Citation2011). This study also demonstrates that the information needs of individuals with SSD require more rigorous methods to ensure these are met in clinical encounters. Further research to develop a decision aid for intervention options for individuals with SSD, as has successfully been done for patients with tinnitus (Pryce, Hall, and Shaw et al. Citation2018), would be an appropriate further step to support their decision-making process.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Akeroyd, M. A., C. G. Brennan-Jones, and S. L. Suller. 2012. “Bone-Anchored Hearing Aids for People withBilateral Hearing Impairment: A Systematic Review.” Clinical Otolaryngology 37 (1) : 77–77. doi:https://doi.org/10.1111/j.1749-4486.2012.02429.x.
- Alemu, G, et al. 2015. “The Use of a Constructivist Grounded Theory Method to Explore the Role of Socially-Constructed Metadata (Web 2.0) Approaches.” Qualitative and Quantitative Methods in Libraries (QQML) 4: 517–540. doi: ISSN 2241–1925.
- Blasco, M. A., and M. I. Redleaf. 2014. “Cochlear Implantation in Unilateral Sudden Deafness Improves Tinnitus and Speech Comprehension: Meta-Analysis and Systematic Review.” Otology & Neurotology : Official Publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology 35 (8): 1426–1432. doi:https://doi.org/10.1097/MAO.0000000000000431.
- Braun, V., and V. Clarke. 2013. Successful Qualitative Research: A Practical Guide for Beginners. London: SAGE.
- Braun, V., and V. Clarke. 2019. “Novel Insights into Patients’ Life-Worlds: The Value of Qualitative Research.” The Lancet. Psychiatry 6 (9): 720–721. doi:https://doi.org/10.1016/S2215-0366(19)30296-2.
- Brodie, A., B. Smith, and J. Ray. 2018. “The Impact of Rehabilitation on Quality of Life after Hearing Loss: A Systematic Review.” European Archives of Oto-Rhino-Laryngology : Official Journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery 275 (10): 2435–2440. doi:https://doi.org/10.1007/s00405-018-5100-7.
- Carson, A. J. 2005. “What Brings You Here Today?” the Role of Self-Assessment in Help-Seeking for Age-Related Hearing Loss.” Journal of Aging Studies 19 (2): 185–200. doi:https://doi.org/10.1016/j.jaging.2004.07.001.
- Charmaz, K. 2008. “Constructivism and the Grounded Theory Method.” In Handbook of Constructionist Research, edited by J. Holstein and J. Gubrium, 397–412. New York: The Guildford Press.
- Charmaz, K. 2017. “The Power of Constructivist Grounded Theory for Critical Inquiry.” Qualitative Inquiry 23 (1): 34–45. doi:https://doi.org/10.1177/1077800416657105.
- Coulter, A., and Collins, A. 2011. Making Shared Decision-Making A Reality. London: King's Fund.
- Dahlberg, Karin, Les Todres, and Kathleen Galvin. 2009. “Lifeworld-Led Healthcare is More than Patient-Led Care: An Existential View of Well-Being.” Medicine, Health Care, and Philosophy 12 (3): 265–271. doi:https://doi.org/10.1007/s11019-008-9174-7.
- Dillion, H. 2012. Hearing Aids. 2nd ed. Stuttgart: Thieme Publishers.
- Dillon, B., and H. Pryce. 2020. “What Makes Someone Choose Cochlear Implantation? An Exploration of Factors That Inform Patient Decision Making.” International Journal of Audiology 59 (1): 24–32. doi:https://doi.org/10.1080/14992027.2019.1660917.
- Faber, Hubert T., Hanneke Kievit, Maarten J. F. de Wolf, Cor W. R. J. Cremers, Ad F. M. Snik, and Myrthe K. S. Hol. 2012. “Analysis of Factors Predicting the Success of the Bone Conduction Device Headband Trial in Patients with Single-Sided Deafness.” Archives of Otolaryngology-Head & Neck Surgery 138 (12): 1129–1135. doi:https://doi.org/10.1001/jamaoto.2013.754.
- Garfield, S., S. Jheeta, F. Husson, A. Jacklin, A. Bischler, C. Norton, and B. D. Franklin. 2016. “Lay Involvement in the Analysis of Qualitative Data in Health Services Research: A Descriptive Study.” Research Involvement and Engagement 2 (1): 1–12. doi:https://doi.org/10.1186/s40900-016-0041-z.
- Habermas, J. 1984. The Theory of Communicative Action. London: Heinemann.
- Ihler, Friedrich, Laura Volbers, Jenny Blum, Christoph Matthias, and Martin Canis. 2014. “Preliminary Functional Results and Quality of Life after Implantation of a New Bone Conduction Hearing Device in Patients with Conductive and Mixed Hearing Loss.” Otology & Neurotology: Official Publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology 35 (2): 211–215. doi:https://doi.org/10.1097/MAO.0000000000000208.
- Iwasaki, Satoshi, Hajime Sano, Shinya Nishio, Yutaka Takumi, Makito Okamoto, Shin-ichi Usami, Kaoru Ogawa, et al. 2013. “Hearing Handicap in Adults with Unilateral Deafness and Bilateral Hearing Loss.” Otology & Neurotology: Official Publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology, 34 (4): 644–649. doi:https://doi.org/10.1097/MAO.0b013e318287f1fe.
- Jennings, H., M. Slade, P. Bates, E. Munday, and R. Toney. 2018. “Best Practice Framework for Patient and Public Involvement (PPI) in Collaborative Data Analysis of Qualitative Mental Health Research: methodology Development and Refinement.” BMC Psychiatry 18 (1): 1–11. doi:https://doi.org/10.1186/s12888-018-1794-8.
- Jinks, C., P. Carter, C. Rhodes, R. Taylor, R. Beech, K. Dziedzic, S. Blackburn, R. Hughes, and B. N. Ong. 2016. “Patient and Public Involvement in Primary Care research – An Example of Ensuring its Sustainability.” Research Involvement and Engagement 2 (1): 1. doi:https://doi.org/10.1186/s40900-016-0015-1.
- Kitterick, P. T., L. Lucas, and S. N. Smith. 2015. “Improving Health-Related Quality of Life in Single-Sided Deafness: A Systematic Review and Meta-Analysis.” Audiology and Neurotology 20 (suppl 1): 79–86. doi:https://doi.org/10.1159/000380753.
- Kitterick, P. T., S. N. Smith, and L. Lucas. 2016. “Hearing Instruments for Unilateral Severe-to-Profound Sensorineural Hearing Loss in Adults: A Systematic Review and Meta-Analysis.” Ear and Hearing 37 (5): 495–507. doi:https://doi.org/10.1097/AUD.0000000000000313.
- Knudsen, Line Vestergaard, Marie Oberg, Claus Nielsen, Graham Naylor, and Sophia E. Kramer. 2010. “Factors Influencing Help Seeking, Hearing Aid Uptake, Hearing Aid Use and Satisfaction with Hearing Aids: A Review of the Literature.” Trends in Amplification 14 (3): 127–154. doi:https://doi.org/10.1177/1084713810385712.
- Korkmaz, Mehmet Hakan, Ömer Bayır, Serap Er, Eray Işık, Güleser Saylam, Emel Çadallı Tatar, Ali Özdek, et al. 2016. “Satisfaction and Compliance of Adult Patients Using Hearing Aid and Evaluation of Factors Affecting Them.” European Archives of Oto-Rhino-Laryngology 273 (11): 3723–3732. doi:https://doi.org/10.1007/s00405-016-4046-x.
- Krishnan, L. A., and S. Van Hyfte. 2016. “Management of Unilateral Hearing Loss.” International Journal of Pediatric Otorhinolaryngology 88: 63–73. doi:https://doi.org/10.1016/j.ijporl.2016.06.048.
- Laplante-Lévesque, Ariane, Line V. Knudsen, Jill E. Preminger, Lesley Jones, Claus Nielsen, Marie Öberg, Thomas Lunner, et al. 2012. “Hearing Help-Seeking and Rehabilitation: Perspectives of Adults with Hearing Impairment.” International Journal of Audiology 51 (2): 93–102. doi:https://doi.org/10.3109/14992027.2011.606284.
- Laplante-Lévesque, A., L. Hickson, and L. Worrall. 2010. “Factors Influencing Rehabilitation Decisions of Adults with Acquired Hearing Impairment.” International Journal of Audiology 49 (7): 497–507. doi:https://doi.org/10.3109/14992021003645902.
- Laplante-Lévesque, A., L. Hickson, and L. Worrall. 2012. “What Makes Adults with Hearing Impairment Take up Hearing Aids or Communication Programs and Achieve Successful Outcomes?” Ear and Hearing 33 (1): 79–93. doi:https://doi.org/10.1097/AUD.0b013e31822c26dc.
- Lucas, L., R. Katiri, and P. T. Kitterick. 2018. “The Psychological and Social Consequences of Single-Sided Deafness in Adulthood.” International Journal of Audiology 57 (1): 21–30. doi:https://doi.org/10.1080/14992027.2017.1398420.
- Manchaiah, Vinaya, Monica L. Bellon-Harn, Ashley L. Dockens, Jamie H. Azios, and William E. Harn. 2019. “Communication between Audiologist, Patient, and Patient’s Family Members during Initial Audiology Consultation and Rehabilitation Planning Sessions: A Descriptive Review.” Journal of the American Academy of Audiology 30 (9): 810–819. doi:https://doi.org/10.3766/jaaa.18032.
- Mehl, A. L., and V. Thomson. 2002. “The Colorado Newborn Hearing Screening Project, 1992–1999: On the Threshold of Effective Population-Based Universal Newborn Hearing Screening.” Pediatrics 109 (1): e7–e7. doi:https://doi.org/10.1542/peds.109.1.e7.
- Meyer, Carly, Louise Hickson, Karen Lovelock, Michelle Lampert, and Asad Khan. 2014. “An Investigation of Factors That Influence Help-Seeking for Hearing Impairment in Older Adults.” International Journal of Audiology 53 (sup1): S3–S17. doi:https://doi.org/10.3109/14992027.2013.839888.
- Meyer, C., and L. Hickson. 2012. “What Factors Influence Help-Seeking for Hearing Impairment and Hearing Aid Adoption in Older Adults?” International Journal of Audiology 51 (2): 66–74. doi:https://doi.org/10.3109/14992027.2011.611178.
- Meyer, C., L. Hickson, and A. Fletcher. 2014. “Identifying the Barriers and Facilitators to Optimal Hearing Aid Self-Efficacy.” International Journal of Audiology 53 (sup1): S28–S37. doi:https://doi.org/10.3109/14992027.2013.832420.
- Ng, Z. Y., S. Allen, I. Mulla, S. Archbold, and M. Gregory. 2017. Bone Conducting Hearing Implants for Adults. The Ear Foundation/Oticon Foundation. Decision-making%20for%20BCHI.pdf
- NHS England 2016. Clinical Commissioning Policy: Bone conducting hearing implants (BCHIs) for hearing loss (all ages) – Clinical Commissioning Policy 16041/P, England.
- NICE 2018. “Hearing Loss Overview.” Accessed September 2020. https://www.nice.org.uk/guidance/ng98
- NICE 2019. “Cochlear Implants for Children and Adults with Severe to Profound Deafness.” Accessed March 2021. https://www.nice.org.uk/guidance/ta566/chapter/1-Recommendations
- Pennings, R. J. E., M. Gulliver, and D. P. Morris. 2011. “The Importance of an Extended Preoperative Trial of BAHA in Unilateral Sensorineural Hearing Loss: A Prospective Cohort Study.” Clinical Otolaryngology: official Journal of ENT-UK ; Official Journal of Netherlands Society for Oto-Rhino-Laryngology & Cervico-Facial Surgery 36 (5): 442–449. doi:https://doi.org/10.1111/j.1749-4486.2011.02388.x.
- Peters, Jeroen P. M., Adriana L. Smit, Inge Stegeman, and Wilko Grolman. 2015. “Review: Bone Conduction Devices and Contralateral Routing of Sound Systems in Single-Sided Deafness.” The Laryngoscope 125 (1): 218–226. doi:https://doi.org/10.1002/lary.24865.
- Poost-Foroosh, Laya, Mary Beth Jennings, Lynn Shaw, Christine N. Meston, and Margaret F. Cheesman. 2011. “Factors in client-clinician interaction that influence hearing aid adoption.” Trends in Amplification 15 (3): 127–139. doi:https://doi.org/10.1177/1084713811430217.
- Preminger, J. E., and A. Laplante-Lévesque. 2014. “Perceptions of Age and Brain in Relation to Hearing Help-Seeking and Rehabilitation.” Ear and Hearing 35 (1): 19–29. doi:https://doi.org/10.1097/AUD.0b013e31829c065c.
- Pryce, H., A. Hall, R. Shaw, B.-A. Culhane, S. Swift, J. Straus, and B. Claesen. 2018. “Patient Preferences in Tinnitus Outcomes and Treatments: A Qualitative Study.” International Journal of Audiology 57 (10): 784–790. doi:https://doi.org/10.1080/14992027.2018.1484184. 30388941
- Pryce, H., A. Hall, E. Marks, B.-A. Culhane, S. Swift, J. Straus, and R. L. Shaw. 2018. “Shared Decision-Making in Tinnitus Care- AN Exploration of Clinical Encounters.” British Journal of Health Psychology 23 (3): 630–645. doi:https://doi.org/10.1111/bjhp.12308. 29575484
- Pryce, Helen, Amanda Hall, Ariane Laplante-Lévesque, and Elizabeth Clark. 2016. “A Qualitative Investigation of Decision Making during Help-Seeking for Adult Hearing Loss.” International Journal of Audiology 55 (11): 658–665. doi:https://doi.org/10.1080/14992027.2016.1202455.
- Pryce, Helen, Marie-Anne Durand, Amanda Hall, Rachel Shaw, Beth-Anne Culhane, Sarah Swift, Jean Straus, et al. 2018. “The Development of a Decision Aid for Tinnitus.” International Journal of Audiology 57 (9): 714–716. doi:https://doi.org/10.1080/14992027.2018.1468093.
- Ross, Danielle S., Susanna N. Visser, W. June Holstrum, Tielin Qin, and Aileen Kenneson. 2010. “Highly Variable Population-Based Prevalence Rates of Unilateral Hearing Loss After the Application of Common Case Definitions.” Ear and Hearing 31 (1): 126–133. doi:https://doi.org/10.1097/AUD.0b013e3181bb69db.
- Saroul, N., M. Akkari, Y. Pavier, L. Gilain, and T. Mom. 2014. “Baha-Mediated Rehabilitation of Patients with Unilateral Deafness: Selection Criteria.” Audiology & Neuro-Otology 19 (2): 85–90. doi:https://doi.org/10.1159/000354272.
- Shargorodsky, J. 2010. “Change in Prevalence of Hearing Loss in US Adolescents.” JAMA 304 (7): 772–778. doi:https://doi.org/10.1001/jama.2010.1124.
- Siau, D., B. Dhillon, R. Andrews, and K. M. J. Green. 2015. “Bone-Anchored Hearing Aids and Unilateral Sensorineural Hearing Loss: Why Do Patients Reject Them?” The Journal of Laryngology and Otology 129 (4): 321–325. doi:https://doi.org/10.1017/S0022215115000602.
- Siau, Richard T. K., Baljeet Dhillon, Derrick Siau, and Kevin M. J. Green. 2016. “Bone-Anchored Hearing Aids in Conductive and Mixed Hearing Losses: Why Do Patients Reject Them?” European Archives of Oto-Rhino-Laryngology: Official Journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS): affiliated with the German Society for Oto-Rhino-Laryngology – Head and Neck Surgery 273 (10): 3117–3122. doi:https://doi.org/10.1007/s00405-016-3941-5.
- Snapp, Hillary A., Fred D. Holt, Xuezhong Liu, and Suhrud M. Rajguru. 2017. “Comparison of Speech-in-Noise and Localization Benefits in Unilateral Hearing Loss Subjects Using Contralateral Routing of Signal Hearing Aids or Bone-Anchored Implants.” Otology & Neurotology 38 (1): 11–18. doi:https://doi.org/10.1097/MAO.0000000000001269.
- Southall, K., J. P. Gagné, and M. B. Jennings. 2010. “Stigma: A Negative and a Positive Influence on Help-Seeking for Adults with Acquired Hearing Loss.” International Journal of Audiology 49 (11): 804–814. doi:https://doi.org/10.3109/14992027.2010.498447.
- Tahden, Maike A. S., Anja Gieseler, Markus Meis, Kirsten C. Wagener, and Hans Colonius. 2018. “What Keeps Older Adults with Hearing Impairment from Adopting Hearing Aids?” Trends in Hearing 22: 2331216518809737. doi:https://doi.org/10.1177/2331216518809737.
- Urquhart, C. 2013. Grounded Theory for Qualitative Research: A Practical Guide. UK: SAGE.
- Van De Heyning, P., D. Távora-Vieira, G. Mertens, V. Van Rompaey, G. P. Rajan, J. Müller, J. M. Hempel, et al. 2016. “Towards a Unified Testing Framework for Single-Sided Deafness Studies: A Consensus Paper.” Audiology & Neuro-Otology 21 (6): 391–398. doi:https://doi.org/10.1159/000455058. 28319951
- Thomas, David R. 2017. “Feedback from Research Participants: Are Member Checks Useful in Qualitative Research?” Qualitative Research in Psychology 14 (1): 23–41. doi:https://doi.org/10.1080/14780887.2016.1219435.
- Wallhagen, M. I. 2010. “The Stigma of Hearing Loss.” The Gerontologist 50 (1): 66–75. doi:https://doi.org/10.1093/geront/gnp107.
- Walseth, L. T., and E. Schei. 2011. “Effecting Change Through Dialogue: Habermas’ Theory of Communicative Action as a Tool in Medical Lifestyle Interventions.” Medicine, Health Care, and Philosophy 14 (1): 81–90. doi:https://doi.org/10.1007/s11019-010-9260-5.
- Wendrich, Anne W., Tiuri E. Kroese, Jeroen P. M. Peters, Guido Cattani, and Wilko Grolman. 2017. “Systematic Review on the Trial Period for Bone Conduction Devices in Single-Sided Deafness: Rates and Reasons for Rejection.” Otology & Neurotology: Official Publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology 38 (5): 632–641. doi:https://doi.org/10.1097/MAO.0000000000001405.
- Wie, O. B., A. H. Pripp, and O. Tvete. 2010. “Unilateral Deafness in Adults: Effects on Communication and Social Interaction.” The Annals of Otology, Rhinology, and Laryngology 119 (11): 772–781.
- Zawawi, Faisal, Ghassan Kabbach, Marie Lallemand, and Sam J. Daniel. 2014. “Bone-Anchored Hearing Aid: Why Do Some Patients Refuse It?” International Journal of Pediatric Otorhinolaryngology 78 (2): 232–234. doi:https://doi.org/10.1016/j.ijporl.2013.11.010.