Abstract
Objective
The aim of the study was to investigate the effect of surgical masks and face shields on speech intelligibility of adults with moderate to severe hearing loss.
Design
This study measured speech tracking scores in quiet for life speech in three different conditions: without a mask, with a surgical mask and with a face shield. Acoustic effects of the masks and face shields on the speech signal were also investigated. Study sample: The study sample consists of 42 patients with moderate to severe hearing loss, 23 cochlear implant users and 19 hearing aid users.
Results
A significant average difference in speech perception scores was found for the use of a surgical mask compared to the listening situation “without mask”. The worse the speech understanding in quiet, the larger the impact of the surgical mask. For the worse performers even the face shield had a negative impact on speech perception. The sound distortion for the face shield compared to the surgical mask was greater.
Conclusion
This study shows that even for speech perception in quiet, surgical face masks, and face shields to a lesser extent, have a negative effect for patients with moderate to severe hearing loss.
Introduction
Hospitals worldwide have adopted universal masking to reduce the potential of transmission with COVID-19 by health workers and patients. With these surgical masks, speech sounds are attenuated and people cannot see the facial expressions and lip movements. Therefore, surgical masks are suspected to have a negative effect on the communication while, especially in hospitals, effective communication is very important. Some studies (Bandaru et al. Citation2020; Hampton et al. Citation2020; Cohn, Pycha, and Zellou Citation2021; Muzzi et al. Citation2021; Toscano and Toscano Citation2021) investigated the effect of surgical masks on speech understanding for normal hearing adults. All these studies found decreased speech perception scores in background noises when surgical masks were worn.
As wearing masks can even be a challenge for normal hearing people, these masks are expected to have a much larger impact on the communication for people with hearing loss (Mendel, Gardino, and Atcherson Citation2008; Chodosh, Weinstein, and Blustein Citation2020; McKee, Moran, and Zazove Citation2020; Naylor, Burke, and Holman Citation2020; Park Citation2020; Saunders, Jackson, and Visram Citation2020; Trecca, Gelardi, and Cassano Citation2020; West, Franck, and Welling Citation2020; Homans and Vroegop Citation2021; Littlejohn et al. Citation2021; Nguyen et al. Citation2021). Trecca, Gelardi, and Cassano (Citation2020) showed preliminary results on the impact of the use of surgical masks by medical personnel on the perceived difficulties of 59 adults with hearing loss during their hospital visit. Mild to severe problems were experienced by 86.4% of these patients. The main problem with the masks was the impossibility of lip reading (for 33 people) and noise reduction was the main problem for 26 people. Atcherson et al. (Citation2017) investigated the effect of conventional and transparent masks on speech perception in noise for persons with and without hearing loss. For normal hearing subjects, no differences between the masks was found, but subjects with hearing loss showed improved speech perception in noise when visual input was provided through the use of a transparent surgical mask compared with a conventional mask (Atcherson et al. Citation2017). A study to the acoustic effects of twelve different masks of Corey, Jones, and Singer (Citation2020) showed attenuation of sounds above 1000 Hz for all type of masks. However, transparent masks and face shields showed to have the worst acoustic performance, as they caused an increase in sound level below 1 kHz and a large attenuation of sound above 1 kHz (Corey, Jones, and Singer Citation2020). Maryn, Wuyts, and Zarowski (Citation2021) used pre-recorded vowels and sentences from 47 subjects that were played by a speech production model in several conditions. All masks influenced sound properties, but plastic masks influenced sound the most. Very recently, Vos et al. (Citation2021) showed a disruptive effect of wearing face shield in conjunction with a N95 mask on speech perception performance of adult cochlear implant users. In this study, pre-recorded sentences were used that were presented through a loudspeaker. Thibodeau et al. (Citation2021) recently investigated the influence of a transparent (custom made) mask and an opaque mask and showed that even persons with normal hearing recognised speech in background noise significantly better when the talker used a transparent mask compared to an opaque mask (Thibodeau et al. Citation2021). Kratzke mentioned another very relevant aspect; empathy shown by the physician was much more seen and valued by patients when surgeons wore a transparent mask instead of a surgical mask (Kratzke et al. Citation2021).
In our hospital, the Erasmus Medical Centre, a tertiary referral centre in Rotterdam in the Netherlands, surgical IIR masks (disposable masks, produced according to the European standard NEN-EN 14683:2019) are generally used by healthcare professionals for patients not suspected for Covid-19. Healthcare workers can opt for face shields (Snijlab Citation2020) to improve their communication with patients with hearing loss instead of the surgical masks. However, for patients with (severe) hearing loss visiting the hospital, it is yet uncertain which option is best suited for their communication in daily clinical practice. Face shields may distort the sound to a larger extend, but lip reading remains possible. However, surgical masks attenuate sound to a lesser extent, but the mouth is totally covered. Until now, no study is performed to further investigate the benefit of visual cues via a face shield combined with attenuated auditory information for speech perception in quiet for a larger group of hearing impaired, but rehabilitated, participants.
The aim of our study was therefore to investigate the effect surgical masks and face shields, used in our clinic, on speech intelligibility of adults with mild to severe hearing loss. In the study a Speech Tracking Test (STT) with live speech, on a ‘COVID-19’ safe distance, was used in three different conditions; without masks, with a surgical IIR mask and with a face shield. A second aim of the study was to measure the acoustic effects of the masks and face shields on the speech signal.
Methods
Subjects
A total of 42 patients with hearing loss participated in this study. All participants used either one or two hearing aids (HAs) or a cochlear implant (CI) (n = 19 vs. 23). Age ranged from 31 to 85 years (group mean age = 65 years; SD = 12 years), 48% was female. All were under treatment at the Erasmus University Medical Centre for their hearing loss. Only patients fluent in Dutch language and with a (unaided) hearing loss of at least 35 dB HL in the best ear were included. The Medical Ethics Committee of the Erasmus MC has reviewed the research protocol and has judged that the rules laid down in the Medical Research Involving Human Subjects Act do not apply to this research proposal (MEC-2020-0870). The study was conducted according to the principles of the Declaration of Helsinki (64th WMA, 2013) and the general Data Protection Regulation.
Study design and procedures
A prospective observational design was used for the study. Participants were asked to participate during their regular visit at our outpatient clinic. After informed consent was given, participants completed the tests. The STT was performed in three conditions, without mask, with a surgical IIR mask and with a face shield. Speech perception in quiet was performed as part of the normal clinical routine on the same day as the STT.
Test materials
Hearing loss assessment
For patients with HAs, pure-tone audiograms had been obtained during clinical appointments. Hearing thresholds were measured with a clinical audiometer, calibrated according to ISO standard 389-1. In this study, we used the pure-tone air conduction thresholds averaged over the frequencies 0.5, 1, 2, and 4 kHz of the best ear (PTA). All thresholds were measured in a sound – attenuated booth. Measurements were conducted according to the Hughson-Westlake method based on ISO standard 8253-1.
Speech perception in quiet
Speech perception in quiet was tested during the normal clinical appointment of the participants. This was tested with the Dutch speech test of the Dutch Society of Audiology (Bosman and Smoorenburg Citation1995), which consists of phonetically balanced monosyllabics (consonant-vowel-consonant; CVC) (Bosman and Smoorenburg Citation1995). The word lists were presented at 65 dB SPL in best aided condition. Testing was performed in a sound-attenuated booth. A clinical audiometer (Decos audiology workstation, version 210.2.6) was used. Participants were placed in front of the loudspeaker at a distance of one metre.
Speech tracking test (STT)
For the STT (De Filippo and Scott Citation1978) a story was read to the participant (in live voice at a comfortable loudness level). The participant had to repeat the sentences correctly, the same sentence was repeated until it was correctly repeated by the participant, with a maximum of three repetitions per sentence. Words not correctly repeated or not heard at all were removed from the total number of words. After the story was read, the number of correct words per minute (w/m) was calculated. The score for normal-hearing subjects in this test is between 70 and 80 w/m. The participants were placed one and a half metre in front of the talker. We used a distance of 1.5 metre because it is a safety measure in the Netherlands during the COVID-19 pandemic. This means people are expected to stay at least 1.5 metre (or five feet) away from each other when interacting. The STT was performed in three conditions, with surgical mask, with face shield and without mask. Three different stories were used. The stories and conditions were randomised across all participants. The STT was performed by two experienced speech and language therapists. Testing was performed in a quiet consultation room in the hospital.
Measurement of acoustic effects
To measure the acoustic effects of the masks, a Type 4189 sound level metre (Brüel and Kjær) was placed on a distance 1.5 metre in front of the talker position. The microphone measured frequency responses from 12.5 Hz to 16 kHz, 1/3 octave, LZeq. Voice recordings took place in a quiet consultation room in the hospital, the same room as the STT. We measured the speech spectrum of both speech therapists reading the 3 different stories used for speech tracking. They were asked to use their habitual voice to read a total of 10 stories. We used three conditions (1) not wearing a mask, (2) wearing a face shield, and (3) wearing a standard surgical mask. A plastic face shield with forehead contact and a free inferior edge was used. One story was read twice without a mask as a test-retest. When wearing the face shield or surgical mask, the speech therapists took care of a good and tight fit.
Data analysis
Data interpretation and analysis were performed with SPSS (v25). The data was normally distributed, therefore parametric statistical methods were used. To analyse the data between listening conditions, the Paired Samples T-Test was used. Correlations were calculated with the Pearson correlation coefficient. Differences in Speech Tracking Scores (STS) were calculated as STS without mask minus STS with mask or face shield. Differences between HA and CI users were calculated with the Independent Samples Test. The Benjamini–Hochberg method was used to control the false discovery rate for multiple comparisons, all displayed p-values are corrected. p-values < 0.05 were considered significant.
Results
Two patients were not able to perform the STT in the surgical mask condition, because they did not understand the sentences, therefore data for the surgical mask condition only contains 40 subjects. For 2 other patients no speech perception scores at 65 dBSPL were available, therefore correlations with speech perception scores were performed for 40 subjects.
Acoustic analysis
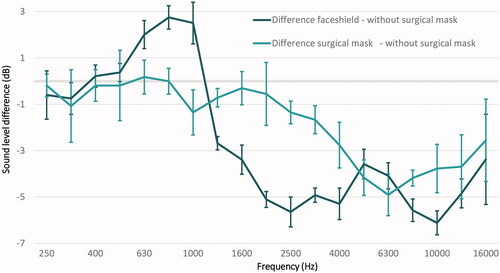
shows the difference in decibels of the face shield and surgical mask compared with the situation without a mask as reference. Because there were no differences below 250 Hz, we didn’t show these measurements in . The three different stories, test – retest, showed similar patterns and no significant differences.
Effects of protective equipment on the STS
shows the results for the STT for the condition without any protective equipment, the condition with a face shield and the condition with a surgical mask. The Paired Samples T-test indicated that a significant average difference in STS exist between the situation without mask (M = 73.9, SD = 12.9) and with surgical mask (M = 60.7, SD = 18.4), (t(39) = 5.996, p < 0.001) and between surgical mask (M = 60.7, SD = 18.4) and face shield (M = 71.0, SD = 13.9), t(39) = 5.262, p < 0.001). For the whole group of participants no difference was found between the condition without surgical mask (M = 72.3, SD = 15.0) and a face shield (M = 69.4, SD = 15.4), t(41) = 1.857, p = 0.07.
Figure 2. Box-whisker plot of the speech tracking score per listening condition. Boxes represent the median (thick horizontal line), lower and upper quartiles (end of boxes), minimum and maximum values (ends of whiskers), outliers (values between 1.5 and 3 times the interquartile range under the third quartile, circles). On the left all participants are included, on the right only the participants with a score <80% on the CVC test are included.
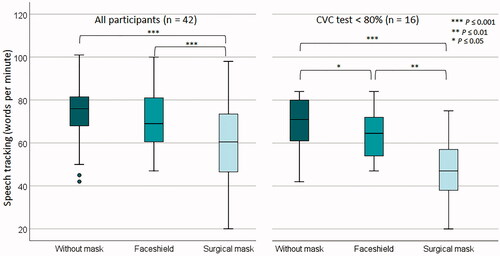
For subjects with CVC test phoneme score < 80% (n = 16), also a significant difference between no mask (M = 66.2, SD = 16.8) and face shield (M = 60.75, SD = 13.6) was found, t(15) = 2.432, p = 0.034.
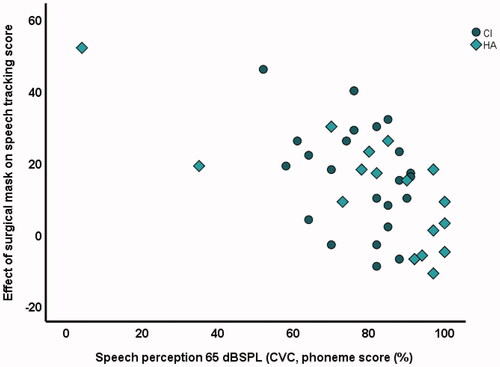
STS and patient related factors
As the surgical masks had the largest impact on speech perception, we investigated the correlation between patient related factors and STS for the effect of the surgical masks (and the lack of visual cues). shows the effect of the surgical mask per patient on the STS. We subtracted the speech tracking score with surgical mask from the score without mask. The larger the outcome, the larger the effect of the mask on STS. A significant correlation of −0.58 was found between CVC test scores in best aided condition (p < 0.001) and the impact of surgical masks. For the HA users, a significant correlation of 0.72 was found between the PTA and the effect of the surgical masks (p = 0.001). No significant correlations with age on the effect of the surgical mask on speech scores was found. No significant differences between HA and CI users on the effect of the masks was found.
Discussion
This study investigated the effect of IIR surgical masks and face shields on speech perception in adult patients with moderate to severe hearing loss. Our research shows that the face shields had the greatest acoustic impact on the vocal sound. However, this effect seems to be compensated during live speech, as the mouth remains visible. Despite the lesser acoustic impact of the surgical mask, the inability to see facial expressions and to read lips have a major impact on speech understanding. The worse the hearing, the greater the impact of the surgical mask. A lot of previous research has been performed into the impact of sound quality for the normal and hearing impaired listener, but the visual aspect has not been taken into account very often, especially not for speech perception in quiet.
Acoustic analysis
Compared with the surgical mask, the face shield had the poorest acoustic performance, which is comparable with other studies who investigated the acoustic effect of surgical masks (Corey, Jones, and Singer Citation2020; Maryn, Wuyts, and Zarowski Citation2021; Vos et al. Citation2021). For the surgical mask the largest attenuation was found for frequencies higher than 2 kHz, with a maximum of 5 dB. For the face shields, we found an amplification of the sound between 500 and 1000 Hz with a maximum of 3 dB, for frequencies above 1 kHz an attenuation of the sound was found with a maximum of 6 dB. This specific pattern of the amplification and attenuation of the sound spectrum is comparable with the study of Corey, Jones, and Singer (Citation2020).
Effect of protective equipment on STS
We found significantly worse STS for the listening situations with surgical masks compared to the listening situations with face shield and the listening situation without a surgical mask. No significant differences were found between the face shield and the listening situation without a mask. This is in contrast to the study by Vos et al. (Citation2021), who found no differences between the surgical mask and the listening condition without a mask, but found a worse score for speech perception by adding a face shield to the condition with a mask. However, no visual speech cues were available in their study. Probably, due to the availability of visual cues in our study, the face shield did not affect speech perception in our study. Our results are in line with the study by Atcherson et al. (Citation2017) and Thibodeau et al. (Citation2021) who found improved speech perception in noise when visual input was provided through the use of a transparent mask compared to a conventional mask. (Atcherson et al. Citation2017; Thibodeau et al. Citation2021) Thus, face shields are likely to distort sound to a greater degree, but with the availability of visual input, this effect can be compensated, as also stated by Atcherson (Atcherson, McDowell, and Howard Citation2021). However, for the worse performers on the CVC test (<80%), even the face shield has already a significant impact on the STS, so likely patients with poor auditory functioning need both auditory and visual cues for optimal functioning.
Patient related factors and the impact of surgical masks
The study showed that the impact of the surgical mask on STS was negatively correlated with the routine clinical speech test (CVC test). The worse the speech perception in quiet at 65 dB SPL on this test, the larger the impact of the surgical mask. This is comparable with the study of Vos et al. (Citation2021) who also found a correlation of the effect of masks and speech perception. And, as mentioned earlier, for the worse performers even the face shield has already an impact on their STS, even with the visual cues present.
Strengths and limitations
The strength of our study is the fact that we investigated the effect of the masks with live speech and at a distance of 1.5 m, which is one of the current safety measures, to simulate a clinical consultation as much as possible. The speech was produced by speech therapists, which is less controlled compared with pre-recorded sentences, but on the other hand more like reality presents itself. The inclusion of 42 participants includes CI and HA users and has therefore also shown that the auditory functioning influences the speech tracking score more than the type of rehabilitation.
A limitation of the study is that we did not include background noise in the test environments. Quiet situations are rare in everyday life and one can expect the effect of masks will be even larger in situations with background noise. However, our test situation did mimic the situation of seeing a practitioner in our hospital, as it was performed in the same rooms as clinical consultations take place.
The subjects were allowed to hear the sentences up to three times. In this research setting this was possible, but we have to take into account that the scores would be poorer if a clinician is not aware of the fact that the patient is hearing impaired and doesn’t perform a comprehension check. In that case, if the patient does not ask for repetition either, communication problems will be even larger than measured in the current study with the STT. Because of the COVID pandemic, tests had to be performed during the normal clinical consult, therefore, because of time constraints, we could not include more test conditions, like the combination of the face shield and the surgical mask. Also, we were not able to perform test retest with the participants. However, we did perform a test retest with the acoustic analysis and did not find significant differences in the sound spectrum.
Future research should also incorporate noisy conditions, especially for HA or CI users, with good auditory functioning in quiet. The results from our study showed that the participants with the worst speech understanding had the most difficulty when the visual cues were absent. A limitation of our study is that we included relatively few people who had speech understanding below 60–70% at 65 dB SPL.
Besides, assistive listening devices can possibly overcome the problems raised by the masks, as suggested by Corey, Jones, and Singer Citation2020. As face shields are not as effective as surgical masks against COVID-19 transmission (CDC Citation2021), future studies to safety-approved transparent surgical masks are essential to be able to guarantee the safety of the practitioners and their patients.
Conclusion
This study shows that even for speech perception in quiet, surgical face masks have a negative effect for patients with moderate to severe hearing loss. Although face shields have the greatest acoustic impact, this effect seems to be compensated during live speech because the face remains visible. The worse the auditory performance with CI or HA, the greater the impact of the surgical mask. And for the participants with a CVC-score <80%, even the face shield has a negative impact. Physicians definitely need to be more aware of the impact of masks in their communication, especially for patients with hearing loss.
Acknowledgements
We would like to thank Barbara van Oel and Debbie Smit for performing all tests and Geert Geleijnse for supporting the measurements of the acoustic effects of the surgical masks and face shields.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Atcherson, S. R., B. R. McDowell, and M. P. Howard. 2021. “Acoustic Effects of Non-Transparent and Transparent Face Coverings.” Journal of the Acoustical Society of America 149 (4): 2249. doi:https://doi.org/10.1121/10.0003962.
- Atcherson, Samuel R., Lisa Lucks Mendel, Wesley J. Baltimore, Chhayakanta Patro, Sungmin Lee, Monique Pousson, M. Joshua Spann, et al. 2017. “The Effect of Conventional and Transparent Surgical Masks on Speech Understanding in Individuals with and without Hearing Loss.” Journal of the American Academy of Audiology 28 (1): 58–67. doi:https://doi.org/10.3766/jaaa.15151.
- Bandaru, S. V., A. M. Augustine, A. Lepcha, S. Sebastian, M. Gowri, et al. 2020. “The Effects of N95 Mask and Face Shield on Speech Perception among Healthcare Workers in the Coronavirus Disease 2019 Pandemic Scenario.” J Laryngol Otol 134 (10): 1–4.
- Bosman, A. J., and G. F. Smoorenburg. 1995. “Intelligibility of Dutch CVC Syllables and Sentences for Listeners with Normal Hearing and with Three Types of Hearing Impairment.” Audiology 34 (5): 260–284. doi:https://doi.org/10.3109/00206099509071918.
- CDC C.f.D.C.a.P. 2021. Guidance for Wearing Masks; Help Slow the Spread of COVID-19.
- Chodosh, J., B. E. Weinstein, and J. Blustein. 2020. “Face Masks Can Be Devastating for People with Hearing Loss Innovation is Urgently Needed to Ensure Clear Communication in Medical Settings.” British Medical Journal 370: m2683. doi: https://doi.org/10.1136/bmj.m2683
- Cohn, M., A. Pycha, and G. Zellou. 2021. “Intelligibility of Face-Masked Speech Depends on Speaking Style: Comparing Casual, Clear, and Emotional Speech.” Cognition 210: 104570. doi:https://doi.org/10.1016/j.cognition.2020.104570.
- Corey, R. M., U. Jones, and A. C. Singer. 2020. “Acoustic Effects of Medical, Cloth, and Transparent Face Masks on Speech Signals.” Journal of the Acoustical Society of America 148 (4): 2371. doi:https://doi.org/10.1121/10.0002279.
- De Filippo, C. L., and B. L. Scott. 1978. “A Method for Training and Evaluating the Reception of Ongoing Speech.” Journal of the Acoustical Society of America 63 (4): 1186–1192. doi:https://doi.org/10.1121/1.381827.
- Hampton, T., R. Crunkhorn, N. Lowe, J. Bhat, E. Hogg, W. Afifi, S. De, et al. 2020. “The Negative Impact of Wearing Personal Protective Equipment on Communication during Coronavirus Disease 2019.” Journal of Laryngology and Otology 134 (7): 577–581. doi:https://doi.org/10.1017/S0022215120001437.
- Homans, N. C., and J. L. Vroegop. 2021. “Impact of Face Masks in Public Spaces during COVID-19 Pandemic on Daily Life Communication of Cochlear Implant Users.” Larynscope Investig 6: 531–539.
- Kratzke, I. M., M. E. Rosenbaum, C. Cox, D. W. Ollila, and M. R. Kapadia. 2021. “Effect of Clear vs Standard Covered Masks on Communication with Patients during Surgical Clinic Encounters: A Randomized Clinical Trial.” JAMA Surgery 156 (4): 372–378. doi:https://doi.org/10.1001/jamasurg.2021.0836.
- Littlejohn, J., A. Venneri, A. Marsden, and C. J. Plack. 2021. “Self-Reported Hearing Difficulties Are Associated with Loneliness, Depression and Cognitive Dysfunction during the COVID-19 Pandemic.” International Journal of Audiology 1–5. doi:https://doi.org/10.1080/14992027.2021.1894492
- Maryn, Y., F. L. Wuyts, and A. Zarowski. 2021. “Are Acoustic Markers of Voice and Speech Signals Affected byNose-and-Mouth-Covering Respiratory Protective Masks?” Journal of Voice.
- McKee, M., C. Moran, and P. Zazove. 2020. “Overcoming Additional Barriers to Care for Deaf and Hard of Hearing Patients during COVID-19.” JAMA Otolaryngology – Head & Neck Surgery 146 (9): 781–782. doi:https://doi.org/10.1001/jamaoto.2020.1705.
- Mendel, L. L., J. A. Gardino, and S. R. Atcherson. 2008. “Speech Understanding Using Surgical Masks: A Problem in Health Care?” Journal of the American Academy of Audiology 19: 686–695.
- Muzzi, E., C. Chermaz, V. Castro, M. Zaninoni, A. Saksida, et al. 2021. “Short Report on the Effects of SARS-CoV-2 Face Protective Equipment on Verbal Communication.” European Archives of Oto-rhino-laryngology.
- Naylor, G., L. A. Burke, and J. A. Holman. 2020. “COVID-19 Lockdown Affects Hearing Disability and Handicap in Diverse Ways: A Rapid Online Survey Study.” Ear and Hearing 41 (6): 1442–1449. doi:https://doi.org/10.1097/AUD.0000000000000948.
- Nguyen, Duy Duong, Patricia McCabe, Donna Thomas, Alison Purcell, Maree Doble, Daniel Novakovic, Antonia Chacon, et al. 2021. “Acoustic Voice Characteristics with and without Wearing a Facemask.” Scientific Reports 11 (1): 5651. doi:https://doi.org/10.1038/s41598-021-85130-8.
- Park, J. 2020. “Unraveling the Invisible but Harmful Impact of COVID-19 on Deaf Older Adults and Older Adults with Hearing Loss.” Journal of Gerontological Social Work 598–601.
- Saunders, G. H., I. R. Jackson, and A. S. Visram. 2020. “Impacts of Face Coverings on Communication: An Indirect Impact of COVID-19.” International Journal of Audiology 1–12. doi:https://doi.org/10.1080/14992027.2020.1851401
- Snijlab. 2020. The NGS2020 Face Shield: https://www.ngs2020.nl/
- Thibodeau, L. M., R. B. Thibodeau-Nielsen, C. M. Q. Tran, and R. T. de Souza Jacob. 2021. “Communicating during COVID-19: The Effect of Transparent Masks for Speech Recognition in Noise.” Ear Hear 42 (4): 722–781.
- Toscano, J. C., and C. M. Toscano. 2021. “Effects of Face Masks on Speech Recognition in Multi-Talker Babble Noise.” PLOS One 16 (2): e0246842. doi:https://doi.org/10.1371/journal.pone.0246842.
- Trecca, E. M. C., M. Gelardi, and M. Cassano. 2020. “COVID-19 and Hearing Difficulties.” American Journal of Otolaryngology 41.
- Vos, T. G., M. T. Dillon, E. Buss, M. A. Rooth, A. L. Bucker, et al. 2021. “Influence of Protective Face Coverings on the Speech Recognition of Cochlear Implant Patients.” Laryngoscope 131 (6): E2038–E2043.
- West, J. S., K. H. Franck, and D. B. Welling. 2020. “Providing Health Care to Patients with Hearing Loss during COVID-19 and Physical Distancing.” Larynscope Investig 5: 396–398.