Abstract
Objective
To study patient-reported hearing aid (HA) rehabilitation outcomes, social-communicative functioning, and expectations/experiences during eight months of HA use.
Design
Three self-reporting instruments, the International Outcome Inventory for Hearing Aids (IOI-HA), the Quantified Denver Scale of Communicative Function (QDS), and questionnaires tapping pre-rehabilitation expectations (HA-EXP-Q1) and post-rehabilitation experiences (HA-EXP-Q2) were administered.
Study sample
144 patients ages 23–66 with gradually acquired, adult-onset, mild-to-moderate sensorineural hearing loss affecting both ears who acquired their first HAs.
Results
According to self-reports, HA rehabilitation outcomes were good, and everyday social-communicative functioning improved after one month and after eight months of HA use. When the effects from demographic and audiological variables were analysed, younger age and positive expectations of HAs were associated with better outcomes and social-communicative functioning. The form or hearing loss severity, and the type or number of HAs did not affect outcomes.
Conclusion
Working-age HA users reported better HA outcomes than older adults in previous studies. Coping in work life may be a strong motivator for active HA use. Considering that younger age and positive expectations resulted in better outcomes, early rehabilitation that supports positive and realistic expectations of HA performance is essential.
Introduction
Hearing loss and hearing aid (HA) outcomes among working-age users
In the working-age population, that is, those ages 15–64 according to OECD Labor Force Statistics (Citation2021), hearing loss is the most frequent sensory disability (Cieza et al. Citation2020). Among employed people, hearing loss may affect work performance and increase the risk for early retirement or unemployment (Kramer, Kapteyn, and Houtgast Citation2006). Deterioration of hearing also may cause depression and reduce psychosocial well-being among young and middle-age people because impaired perception of sounds and speech hinders communication with others (Tambs Citation2004). Furthermore, untreated hearing loss in middle age may induce cognitive decline later in life (Lin et al. Citation2013).
The main remedy for avoiding negative consequences from gradually deteriorating hearing is the use of digital hearing aids (HAs). Despite the high incidence of hearing loss among working-age adults, previous research on HA rehabilitation mainly has focussed on older adults (over age 65; Barker et al. Citation2015). In studies on older adults, HA satisfaction and use are generally low, with around 50% being satisfied HA users. Much less is known about working-age patients’ HA outcomes. The few extant studies that have included participants ages 18 and up report high satisfaction (80%) and HA use (85%; Bertoli, Bodmer, and Probst Citation2010), whereas prevalence studies indicate that <20% of working-age people with hearing loss use HAs (Dawes et al. Citation2014). Previous findings on HA outcomes in working-age adults (ages 15–64) are limited, and in this study, we focus on HA outcomes in working-age adults who are still in the labour force to understand HA rehabilitation’s impact on their everyday lives and social-communicative functioning.
Measuring HA rehabilitation outcomes is complex because discrepancies exist between clinically measured and functional personal outcomes. Basic audiometric procedures, hearing thresholds measured with pure tone audiometry (PTA), and tests of speech recognition indicate clinically defined changes in measured hearing ability after HA rehabilitation. However, self-reporting HA outcome instruments, mainly in the form of questionnaires, assess HA users’ own evaluations and can measure everyday life domains that cannot be inspected using audiometric testing. Self-reports provide patients’ perspective, as well as a reliable way to measure HA rehabilitation’s real-life success in terms of HA use, benefits, satisfaction, and quality of life (Cox and Alexander Citation2002). Furthermore, self-reports can provide information on social-communicative functioning, that is, patients’ diminished or remaining hearing related activity limitations and participation restrictions (Knudsen et al. Citation2010). This study uses self-reporting instruments to examine HA outcomes in terms of benefits, satisfaction, quality of life and social-communicative functioning.
In previous studies, self-reported HA outcomes often were evaluated only once, or only during early phases of HA use (Barker et al. Citation2015). Immediate post-HA-fitting self-reports have been found to be less valid, as they may change over time (Vestergaard Citation2006). Very rarely did the studies compare pre-rehabilitation and post-rehabilitation self-reports of social-communicative functioning, or examine longer outcomes (Barker et al. Citation2015). Considering that clinical practice should be based on research evidence, a need exists for research that examines self-reported HA outcomes during longer follow-ups, as well as makes comparisons of social-communicative functioning before and after HA amplification, which is the present study’s goal. Furthermore, previous studies often have been based on samples of both experienced and first-time HA users, thereby including rather varied perspectives on HA rehabilitation. Unlike experienced users, first-time users may have difficulties adjusting to HAs in terms of altered sensory input, practical device maintenance, and psychosocial impact on self-image as HAs still are viewed as stigmatising (Meister et al. Citation2008). To get a more homogeneous sample with a presumably more shared perspective, we focus on studying HA outcomes in working-age patients who have acquired their first HAs.
Audiological and demographic factors affecting HA outcomes
To evaluate HA rehabilitation outcomes reliably, it is important to control for background factors that may affect results. Demographic factors—such as age and gender—and audiological factors, such as hearing loss severity and type and number of HAs—have been viewed as important contributors. Staehelin et al. (Citation2011) found that being under age 65 and female contribute to positive HA outcomes, whereas other studies have found no effects from age or gender (e.g. Knudsen et al. Citation2010). Considering the association between age and HA use, a review by Perez and Edmonds (Citation2012) found no association in five studies, a negative association in two, and a positive association in one. Due to these conflicting results, we examined effects from demographic factors, such as age and gender, using self-reporting instruments that provide a wider view of everyday outcomes than self-reported hours of HA use, which may not reflect outcomes reliably (Solheim and Hickson Citation2017). In a large self-reporting study of male (mean age: 73.3 years) and female (mean age: 74.2 years) HA users, women and users of bilateral HAs reported more positive outcomes than other users, but the hearing loss severity measured with PTA did not affect outcomes (Arlinger, Nordqvist, and Öberg Citation2017). Contrary to the latter finding, a review of several studies suggested that hearing loss severity is the key factor related to good HA outcomes (Knudsen et al. Citation2010). Due to these conflicting findings, we examined the effects from audiological background factors, hearing loss severity and form, and type and number of HAs in the sample that we examined.
Aside from demographic and audiological factors, positive expectations concerning future use of HAs have been found to lead to successful HA rehabilitation outcomes (Saunders, Lewis, and Forsline Citation2009). However, first-time HA users may have unrealistically high expectations for similarly improved hearing in both quiet and noisy circumstances, whereas experienced users realise that HAs may work differently in quiet vs. noisy settings (Meister et al. Citation2008). For these reasons, it has been suggested that pre-rehabilitation expectations should be included in measuring HA outcomes (Vestergaard Citation2006). In this study, we compared the patients’ expectations before their HA fitting with their experiences after eight months of HA use. Furthermore, few opportunities for conversational encounters have been suggested as leading to irregular HA use (Meister et al. Citation2008). Thus, social status—that is, whether a person is living alone or with someone whom one can engage in conversations with—is examined in this study.
Aim and objectives
The study’s main aim was to examine self-reported, functional HA rehabilitation outcomes of working-age first-time HA users with gradually acquired mild-to-moderate sensorineural hearing loss. The research objectives were to examine first-time HA users’ self-reported evaluations of (1) their rehabilitation outcomes after one month and eight months of HA use, (2) their social-communicative functioning before and after HA adoption, and (3) their expectations before HA use and their experiences after having used HAs for eight months. The study’s objectives were achieved by administering self-reported outcome measures during an eight-month follow-up starting before HA fitting. To test whether demographic and audiological variables were associated with outcomes, we examined effects of age, gender, social status, hearing loss severity and form in PTA, and type and number of HAs.
Materials and methods
Participants
Working-age participants were recruited consecutively from patients at two university hospital hearing clinics in Southern Finland. The participants were informed before entering the study in their call-up letter for their pre-fitting consultations, and they provided voluntary written consent to participate in the study before their first visit to the clinic. With the participants’ consent, information on their hearing related medical conditions was gathered from hospital records. The medical inclusion criteria were adult-onset gradually acquired mild-to-moderate sensorineural hearing loss (BEHL 0.5, 1, 2, 4 kHz 20–70 dB) affecting both ears, excluding other hearing related medical conditions, such as sudden traumatic loss of hearing, Ménière’s disease, neurological impairments, and severe psychiatric disorders. Participants filled out a background questionnaire on their social status, including profession, employment, education, and living arrangements. Living arrangements referred to whether the participants were living with someone or were living alone.
Men and women were represented almost equally in the sample (see ), the age range of which was 23–66, with a mean age of 55.6 (SD = 7.6). All participants were employed at the time of data collection. A minority (8%) of participants reported having hearing problems for less than one year, with 34% having problems for more than 10 years before seeking help. The majority (58%) had been experiencing hearing problems for several years, but <10. Mean Better Ear Hearing Level (BEHL) was 33.5 dB (SD 8.0). Of the 144 total participants, 112 had mild (20–39 dB) and 32 moderate (40–69 dB) hearing loss. Sloping high-frequency hearing loss was found in PTA among 79 participants, while the curve was flat in 33 and U-shaped in 19. Of those whose clinical records included the information, 77 used binaural and 55 monaural HAs. The university hearing clinics paid for and dispensed the participants’ HAs through public national Finnish Health Services. The participants used three types of digital HAs. Behind-the-ear (BTE) HAs were the most commonly used (55% of participants), with receiver-in-the-ear (RITE) and in-the-ear (ITE) HAs used among 22% and 23%, respectively. Information on HA type was missing from 25 participants’ medical records.
Table 1. Background characteristics of participants with hearing loss (N = 144).
During the follow-up, 111 participants responded to the self-assessment questionnaires after one month and 103 after eight months. Based on Little’s (Citation1988) missing completely at random test, no evidence was found of systematic dropout or any other systematic missing value patterns in the observed data [Χ2 (160)=136.85, p = 0.91].
HA rehabilitation process
The participants’ HA rehabilitation process was conducted according to European and Finnish national guidelines. All had hearing loss greater than 20 dB averaged over a frequency range of 0.5–4 kHz in the better ear, which is the European standard criteria for HA rehabilitation (cf. EU Work Group on Genetics of Hearing Impairment; Martini, 1996). The participants’ rehabilitation process began at the primary health care level, either at municipal health centres or through occupational health care, after which they entered specialist services at hearing clinics that provided specialist physicians, ear-nose-and-throat (ENT) doctors who specialise in audiology, and audiometricians, who are specialised hearing health professionals. Audiometricians conducted the hearing measurements, pure tone, and speech audiometry in a soundproof booth and conducted the HA fittings.
After hearing measurements and ENT consultations, the HA fitting process with the patient began with an audiometrician according to the rehabilitation plan that the ENT doctor authorised. HA types and technological preferences were chosen based on each patient’s individual needs. Each individually fitted HA usually was provided for home trial for about one month, after which time, the audiometricians adjusted the HA based on patient reports. During adjustments, patients were asked about clarity, loudness, sharpness of sounds, physical comfort while wearing the HA, and the sound quality of other people’s voices and the patient’s own voice. Technical parameters were adjusted to address these and other subjective concerns. If further guidance was needed, it usually was provided by phone or during follow-up meetings, if necessary. If follow-up meetings took place, the need for assistive listening devices also was considered. The audiometricians checked the data log information concerning average daily use of the HA as a systematic part of the HA rehabilitation process. As the research permission parameters did not allow for examination of patients’ personal HA data log information, it was not collected for research purposes.
Data collection procedure
The study was conducted within the research project Communication with the Help of HAs funded by the Academy of Finland, Grant No. 40317. The project’s research design was time-series, with multiple measures (). An eight-month (32-week) follow-up was considered as necessary because shorter follow-ups are found to be insufficient (Vestergaard Citation2006).
Table 2. Follow-up design and outcome measures before and during eight months of HA use.
Three kinds of self-reporting outcome instruments were used before and after HA use to provide the patients’ view of the HAs’ daily impact. The International Outcome Inventory for Hearing Aids (IOI-HA; Cox, Stephens, and Kramer, Citation2002) and the Quantified Denver Scale of Communicative Function (QDS) (Schow and Nerbonne Citation1980), both translated and modified into the Finnish language, were administered, as well as a pair of questionnaires to gauge participants’ expectations of HAs before (HA-EXP-Q1) and experiences after (HA-EXP-Q2) HA use (see Supplementary Material). Self-assessments with QDS and HA-EXP-Q1 were conducted before the first visit at the hearing clinic. After approximately one month of HA use, self-assessments were collected with QDS and IOI-HA, and after eight months, with QDS, IOI-HA, and HA-EXP-Q2. In addition to these self-reports, a sub-sample of patients (n = 20) gave their permission to have their HA rehabilitation encounters and some of their everyday conversational interactions in home and work contexts video-recorded. A small sample of volunteer patients (n = 13) also was interviewed, and the qualitative analyses of these sub-samples have been reported elsewhere (Koskela et al. Citation2016; Laakso et al. Citation2019; Ruusuvuori et al. Citation2020).
The IOI-HA (Cox, Stephens, and Kramer Citation2002) was chosen to examine functional HA outcomes because it is a concise, multidimensional, reliable, and valid self-reporting instrument used internationally to measure HA use and experienced HA benefits and satisfaction (e.g. Kramer et al. Citation2002). It also has been translated into more than 20 languages, including Finnish, allowing for comparisons of HA rehabilitation outcomes across studies (Cox, Stephens, and Kramer Citation2002). Seven items evaluated with the instrument were 1) HA use, 2) benefits from using HA, 3) residual activity limitations, 4) satisfaction with HA, 5) remaining personal restrictions, 6) impact on others, and 7) quality of life. Responses were elicited using a five-point scale (total 35), with higher scores reflecting a positive outcome. IOI-HA was administered twice after HA adoption. The observed Cronbach’s alphas ranged from .77 to .84 between the two measurement occasions.
The QDS (Schow and Nerbonne Citation1980) was chosen to examine social-communicative functioning because it has been found to be reliable and valid in assessing emotional and social-communicative dimensions of hearing loss disabilities across studies. QDS has good reported internal consistency (0.95) and test-retest reliability (0.73) (Tuley et al. Citation1990), does not take long to answer, and the questions are clear. Furthermore, it has been found to be reliable in measuring experienced outcomes over time (e.g. Hickson, Worrall, and Scarinci Citation2007). QDS items are declarative sentences describing emotional experiences (e.g. “I do not feel relaxed in a communicative situation”) and participation restrictions (e.g. “The members of my family sometimes leave me out of conversations”). Altogether, it comprises 25 items divided into four areas focussing on communication breakdown (Items 16–25), psychosocial well-being (items 5, 6, and 8–14), family relationships (Items 1–4), and self-isolation (Items 7 and 15). Responses are elicited through a five-point scale ranging from strongly disagree (1) to strongly agree (5). Higher scores (total score: 125) are consistent with greater difficulties. QDS was used at all three evaluation points both before and after HA adoption. Observed Cronbach’s alphas ranged from .93 to .94 for the three measurement occasions.
Two specific questionnaires were created for this study to examine the participants’ expectations before HA use and experiences after starting HA use: HA-EXP-Q1 and HA-EXP-Q2, see Supplementary Material. With similar pre- and post-items, these two short self-reporting instruments examined future expectations and past experiences using HAs in everyday life, including two-party and multi-party conversations. The questionnaire comprised six items concerning corresponding expectations/experiences on (1) managing hearing in everyday life, (2) handling and using a HA, (3) hearing in two-party conversations, (4) hearing in multi-party conversations, (5) hearing speech on radio and TV, and (6) participation in conversations. Each item was created based on the relevant factors presented in the literature (e.g. Knudsen et al. Citation2010). Responses were elicited using a five-point scale ranging from “I completely disagree” (1) to “I completely agree” (5), with higher scores (total: 30) reflecting positive expectations/experiences concerning HA use. HA-EXP-Q1 was administered before HA adoption and HA-EXP-Q2 after eight months of HA use. The observed Cronbach’s alphas ranged from 0.81 to 0.88 between the two measurement occasions.
Statistical analyses
The first phase of the analysis comprised an initial examination of the data, with ranges and means of background variables calculated. During the next phase, a linear mixed model (Hox Citation2010) was used to reveal possible significant changes in self-assessment scores at different evaluation points during the follow-up, and with respect to the background variables: age; gender; social status; hearing loss severity measured with BEHL in PTA; form of audiogram in PTA; and type and number of HAs. In statistical analyses, the background variable social status was defined by living arrangements, that is, whether the participant was living alone or with someone, because living arrangements were viewed as crucial in differentiating participants’ social status in terms of opportunities to use HAs in everyday social conversations. Based on Akaike’s (Citation1974) and Bayesian (Schwarz Citation1978) criteria, a random intercept model was used in all analyses so that the subjects were treated as random effects. The random intercept model corresponds to standard repeated measures analysis of variance, but with better handling of missing data (Hox Citation2010). The associations of different self-reporting measures, social-communicative restrictions (QDS scores), benefits and satisfaction with HAs (IOI-HA scores), and expectation (HA-EXP-Q1) and experience (HA-EXP-Q2) scores were inspected using similar linear mixed models, as in previous analyses. Furthermore, Pearson product moment correlation also was used to estimate associations between IOI-HA scores and experiences with HA use (HA-EXP-Q2 scores) to examine HA-EXP-Q questionnaires’ validity. All analyses were conducted using SPSS for Windows (Version 26).
Results
Self-reported HA rehabilitation outcomes in the group of working-age first-time HA users were generally positive. The International Outcome Inventory for Hearing Aids (IOI-HA) reported that participants experienced HAs as functional devices (). The participants’ self-reported mean IOI-HA total scores, and the seven mean item scores registered at approximately 4 out of the maximum of 5, which is high, after one month and after eight months of HA use. IOI-HA total scores after eight months of HA use ranged from 14 to 35 (maximum 35), with a median of 28. IOI-HA mean total scores remained stable during the follow-up, and no statistically significant difference was found between the two evaluation points after one month (mean: 27.52) and after eight months (mean: 27.61) of HA use.
Figure 1. Self-reported mean single item values (max 5) after one month and after eight months of HA use as measured by the International Outcome Inventory of Hearing Aid Use (IOI-HA). activity: residual activity limitations; benefit: benefits of using HA; HA use: hearing aid use; IOIHA1: after one month of HA use; IOIHA2: after eight months of HA use; impact: impact on others; personal: remaining personal restrictions; QOL: quality of life; satisfaction: satisfaction with HA; total: total IOI-HA score.
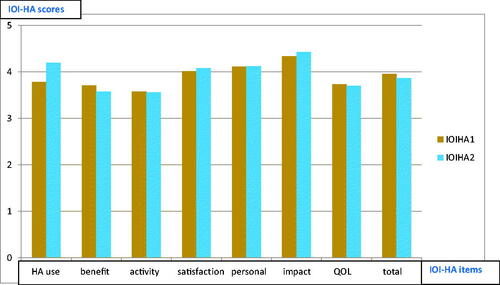
Of the seven dimensions, HA use at eight months, satisfaction with HA, personal restrictions, and impact on others scored 4 or above. The scores were below 4 for HA use at one month, benefits of using HA, residual activity limitations, and quality of life. The first item of the IOI-HA, daily use of HA, increased during the eight-month follow-up and, on average, was four to eight hours a day (the HA use IOI-HA score was 4.2, as shown in ). Almost half the participants used HA more than eight hours. No one at one-month IOI-HA and four at eight-month IOI-HA (3.8%) reported not using their HAs. In addition to IOI-HA, the participants were asked at the eight-month follow-up where they regularly used their HAs, with 80% reporting regular use at home and 69% at work.
Age was a statistically significant background variable [F(1, 121)=4.06, p = 0.04]: Younger working-age participants reported better outcomes in IOI-HA than older ones, both after one month and after eight months of HA use. None of the other background variables—that is, gender, social status, hearing loss severity or form, or type and number of HAs—exerted a statistically significant effect on self-reported IOI-HA outcomes, though gender came close to statistical significance (p = 0.09). After eight months, the mean total scores were lower for male (26.14) than for female participants (28.02).
For the QDS, self-reported difficulties in social-communicative functioning decreased statistically significantly during the eight-month follow-up [F(2, 217)=18.40, p < 0.001; ]. Before HA use, the participants’ total QDS scores ranged from 25 to 115 (mean: 66.75; SD: 18.95); after one month, from 27 to 104 (mean: 61.63; SD: 16.88); and after eight months, from 28 to 103 (mean: 57.80; SD: 17.08).
Figure 2. Change in self-reported social-communicative restrictions and 95% confidence intervals for male and female participants, and participants in total according to the mean single item score (max 5) from the QDS. Evaluation time points: 1: before HA, 2: after one month of HA use, and 3: after eight months of HA use.
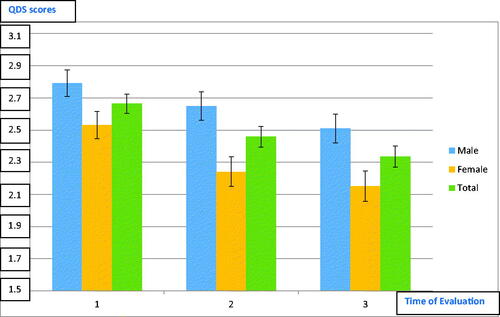
Of the background variables, a statistically significant main effect for gender was found [F(1, 135)=9.40, p = 0.003; ]. Female participants reported less social-communicative difficulties than males. This difference was found before, after one month, and after eight months of HA use. Age also exerted a statistically significant main effect: Older participants reported fewer social-communicative difficulties than the younger participants at all evaluation points [F(1,162)=11.51, p = 0.001]. It should be noted that HA type (BTE, ITE, and RITE) almost exerted a statistically significant effect on social-communicative functioning (p = 0.071; see Figure at Supplementary Material). Users of ITE (in the ear) HAs did not experience a gradually declining change in social-communicative difficulties as did users of BTE (behind the ear) and RITE (receiver in the ear) HAs. All interactions between time and the other background variables—that is, social status, hearing loss severity and form, and number of HAs—were statistically non-significant (p > 0.10). Furthermore, the results did not change after controlling for background variables in a specific analysis.
Pre-rehabilitation expectations (HA-EXP-Q1) concerning HAs’ utility in real-life situations were high before acquiring HAs (). Post-rehabilitation experiences (HA-EXP-Q2) after using HAs for eight months were lower, but the difference was not statistically significant, suggesting that expectations for HA use were fulfilled. A significant main effect for age was found when predicting self-reporting expectations and experiences [F(1,172)=7.59, p = 0.006]. Younger participants reported higher expectations and experiences compared with older ones. None of the other background variables affected self-reported expectations and experiences.
Figure 3. Mean item scores (max 5) of self-reported expectations before HA use and experiences after eight months of HA use. Expect: expectations concerning HA use in HA-EXP-Q1; Exper: experiences concerning HA use in HA-EXP-Q2; Daily: managing everyday life; Handling: easy handling of HA; F to F: better hearing in two-party face-to-face conversation; Group: better hearing in multiparty group conversation; radioTV: better hearing when listening to radio/TV; Partic: easy participation in conversation.
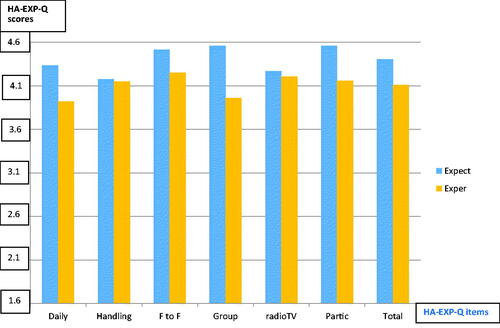
Of the separate HA-EXP-Q1 items, pre-rehabilitation expectations concerning HA benefits in managing daily life, two-party and group conversation, and participation in conversation were less fulfilled in HA-EXP-Q2 than in handling of HA, and hearing the radio/TV. Correlations between the questionnaire on experiences (HA-EXP-Q2) and the IOI-HA at the eight-month follow-up point were statistically significant (0.73; see Figure at Supplementary Material). Thus, the results gained with HA-EXP-Q2 were in line with the results from IOI-HA2, suggesting that the HA-EXP-Q2 questionnaire is valid for evaluating HA rehabilitation outcomes.
Finally, when the associations between different self-reporting measures were inspected using similar linear mixed models, as in previous analyses, it was found that high self-reported pre-rehabilitation expectations (HA-EXP-Q1) exerted a statistically significant positive effect on the success of HA rehabilitation measured by IOI-HA total score [F(1, 114)=13.8, p = 0.001]. Other statistically significant associations between the outcome measures were not found.
Discussion
HA outcomes measured by IOI-HA
Our findings indicated that HA rehabilitation was successful for working-age first-time HA users with adult-onset, gradually acquired, mild-to-moderate sensorineural hearing loss. The answers to the International Outcome Inventory for Hearing Aids (IOI-HA) indicated positive and stable HA outcomes both after one month and after eight months of HA use. At eight months, the mean IOI-HA total score (3.9) was higher than in previous studies of older populations (e.g. Wu et al. Citation2019).
The mean sub-item IOI-HA score for HA use (4.2) in our study was similar to that of many previous studies (e.g. Arlinger, Nordqvist, and Öberg Citation2017; Meister et al. Citation2015). In our study, most participants reported using their HAs regularly at home and at work, and there were only a few non-users (3.8%) at the end of the eight-month follow-up. This corresponds with previous studies including younger participants (e.g. 85% regular HA users in Bertoli, Bodmer, and Probst Citation2010), but differs from prior studies on older adults who use HAs less regularly (Barker et al. Citation2015). Thus, our study suggests that working-age HA users may be more committed to regular HA use than older adults, and that coping in work life may be a strong motivator for active HA use.
The mean sub-item IOI-HA score for HA satisfaction (4.4) was clearly higher than in most previous studies (e.g. 3.6 in Kramer et al. Citation2002; 3.3 in Wu et al. Citation2019), with the exception of the study by Meister et al. (Citation2015), with which it is identical. In Meister et al. (Citation2015), the participants were younger than in most previous studies on older adults, and comprised, as in our study, a more homogeneous sample of patients with mild-to-moderate hearing loss. This suggests that younger participants are more satisfied with their HAs than older adults.
In our study, age was a significant background factor within the working-age population: The younger working-age participants reported better IOI-HA outcomes than older ones. This finding contradicts those from previous studies that found no relation between age and IOI-HA outcome in more heterogeneous populations, including older adults and experienced HA users (e.g. Arlinger, Nordqvist, and Öberg Citation2017). The finding of better outcomes among younger working-age participants emphasises the importance of early detection of hearing loss and the timely provision of HAs, which recent studies found promote better psychosocial well-being (Tsimpida et al. Citation2021).
Similarly, as in many other studies (e.g. Arlinger, Nordqvist, and Öberg Citation2017), hearing loss severity measured with PTA was not connected to self-reported HA outcomes in IOI-HA, reflecting the fact that functional personal outcomes may differ from clinically measured audiological outcomes. Considering that we studied participants with mild and moderate hearing loss, this finding does not challenge the fact that hearing loss severity can affect HA outcomes in studies that include participants with more severe hearing losses (e.g. Houmøller et al. Citation2022).
Based on previous studies (e.g. Arlinger, Nordqvist, and Öberg Citation2017), we expected bilateral HA fitting to be connected to better IOI-HA outcomes than unilateral fitting, but our study did not support these prior findings. This may be related to the fact that most participants in our study had mild hearing loss, and many preferred unilateral fitting.
Social-Communicative functioning before and after HA rehabilitation
We found a statistically significant reduction in self-reported social-communicative difficulties in the QDS after one month and after eight months of HA use, indicating stable, positive outcomes in social-communicative functioning. The sustained improvement in social-emotional and communicative functions among working-age first-time HA users corresponds with previous studies of older adults in longer follow-ups (e.g. Mulrow, Tuley, and Aguilar Citation1992). None of the background variables—that is, age, gender, social status, hearing loss severity or form (PTA), and type and number of HAs—affected improvement in social-communicative functioning. This also was found in some prior studies on older adults (e.g. Hickson, Worrall, and Scarinci Citation2007) and further emphasises the importance of studying social-communicative functioning as an independent dimension of rehabilitation outcomes.
In our study, age exerted a statistically significant main effect on social-communicative functioning: Older working-age participants reported fewer social-communicative restrictions than younger ones, both before and after HA use. Similarly, gender emerged as an interesting background variable: Female participants self-reported fewer social-communicative restrictions compared with male participants both pre- and post-rehabilitation. The observed age and gender differences have not been reported in prior studies that examined self-reported social-communicative functioning as such, but our study corresponds with general findings that women report more positive HA outcomes than men (e.g. Arlinger, Nordqvist, and Öberg Citation2017). The reason for this difference deserves further study.
Expectations and experiences with HA use
Before HA fitting, first-time HA users’ expectations of HAs were high, particularly among younger participants. The participants’ experiences after eight months of HA use did not differ from their expectations statistically significantly, suggesting that pre-rehabilitation expectations mainly were fulfilled. It should be noted that the expectations concerning participation in conversational encounters were less fulfilled, indicating that first-time HA users’ expectations in this respect may have been unrealistic. Unrealistic expectations of HA use also have been found in previous research (e.g. Meister et al. Citation2008). As in Saunders, Lewis, and Forsline (Citation2009), in our study, high expectations were associated with better overall HA outcomes. Thus, our study supports using pre-fitting expectations to predict HA outcomes. Our results also indicate that the simple six-item EXP-HA-Q questionnaires developed for this study can be useful for measuring HA outcomes, as they correlated strongly with IOI-HA. EXP-HA-Q1 and EXP-HA-Q2 may amend other measures in providing systematic and clinically usable data about expectations and real-life experiences in different communicative situations, such as two-party and group conversations.
Data reliability
Our sample of 144 first-time HA users with gradually acquired sensorineural hearing loss was homogeneous with respect to age (working age), as well as hearing loss type (adult-onset gradual sensory-neural) and severity (mild-to-moderate). The data also were equally representative of male and female participants. Although the sample is not very large, it clearly represents a less-studied population that is still in the labour force with an age range of 23–66. Furthermore, all participants were first-time HA users, so the data were more consistent and reliably interpretable than if the data comprised both new and experienced HA users.
The longitudinal study design was thorough in following up working-age first-time HA users three times—before their HA fitting, after one month of HA use, and after eight months of HA use. Most previous studies have reported shorter follow-ups or did not include any pre-rehabilitation measures (see, e.g. Barker et al. Citation2015). The use of three different kinds of self-reporting assessment instruments strengthened the study’s design and allowed for an examination of different dimensions of HA outcomes. These self-reporting instruments have been found to work well in measuring experienced HA outcomes, as well as changes in social-communicative functioning (e.g. Kramer et al. Citation2002). However, in measuring hours of actual HA use time, self-reporting instruments have been found to be less-reliable compared with intrinsic data logging directly from the aid (Solheim and Hickson Citation2017). We collected self-reported hours of HA use with IOI-HA at two separate evaluation points: after one month and after eight months of HA use. The hour totals were consistent within one participant; thus, in this respect the estimates appear to be reliable.
The loss of participants in a follow-up study presented a potential problem. In our study, the number of participants decreased from the initial 144 respondents to 103 between the one-month and eight-month follow-ups. However, the loss of information in this study occurred randomly due to factors such as address changes, inattention (leaving the back of the questionnaire unanswered), and missing details in hospital records. Nevertheless, this type of random missing information does not jeopardise or bias the results from a follow-up (Kristman, Manno, and Côté Citation2003). All analytical assumptions were assessed using traditional linear model diagnostics, and based on the findings, the assumptions were met in all analyses.
Conclusions, clinical relevance, and future studies
Both high HA satisfaction (IOI-HA) and improvement in social-communicative functioning (QDS) measures indicated that HA rehabilitation was successful for the working-age participants studied. The qualitative analysis of video-recorded everyday conversations from a sub-sample supported this finding, in which the HA users did not differ from their partners with normal hearing in frequency of hearing related problems (Laakso et al. Citation2019). Thus, short self-reporting tools can be used in clinical practice to gather information on the everyday life success of HA rehabilitation. Considering that HA outcomes were good and stable from one month until eight months, it may be sufficient to measure self-reported outcomes once after HA fitting. However, the outcome measurement’s optimal timing still deserves further study. Despite the good average outcome, four non-users were left at eight months. In the interview study conducted with a smaller sample within this study (Koskela et al. Citation2016), the participants’ experiences with the rehabilitation process ranged from smooth to ambivalent. Ambivalent rehabilitation outcomes should be studied with a larger sample of non-users and irregular HA users to get a better picture of this phenomenon’s social dimensions.
In this study, only younger age and high expectations of HA use were found to be associated with better HA outcomes; thus, HAs should be provided early when hearing deteriorates. Furthermore, positive expectations of HA use should be encouraged in professional encounters. Overall, based on our results, HA rehabilitation outcomes appear to be more dependent on patients’ expectations towards HAs than on audiological variables or type and number of HAs. This further emphasises the fact that hearing health professionals should pay special attention to interviewing and listening to their patients’ views on HA use. Similar to previous studies, our findings suggest that measuring pre-rehabilitation expectations can be useful in predicting HA outcomes in clinical practice (cf. Vestergaard Citation2006).
Considering that most audiological and demographic background factors did not influence HA outcomes, professional patient interaction in rehabilitation encounters and its relation to differences in HA outcomes could be examined further. Several researchers have recommended a more patient-centered approach that includes shared decision-making in HA rehabilitation to improve HA outcomes (e.g. Afzarini et al. 2019), but only a few studies have addressed the actual fitting process, indicating a great need for more empirical research. Our examination of the video-recorded rehabilitation encounters from a sub-sample of the participants (Ruusuvuori et al. Citation2020) demonstrated how more patient-centered styles of recommending HAs to patients resulted in more shared decision making, increasing the patients’ adherence to HA use.
In clinical practice, self-reports of HA outcomes should be amended with remote data logging from HAs, which can offer ecologically valid information about individual use patterns in different everyday contexts at home and at work (cf. Solheim and Hickson Citation2017). It has been observed recently that data-logged HA use time is associated with IOI-HA outcomes in both first-time and experienced HA users (Houmøller et al. Citation2022). Thus, along with gathering the patient perspective on HA satisfaction and social-communicative functioning, data logging can identify patients who use their HAs rarely, so that hearing health professionals can provide appropriate rehabilitative support for them.
Ethical approval
Recruitment was accomplished in accordance with the Declaration of Helsinki, which guides research involving human subjects. The hospital district’s research ethics committee and both hospitals’ hearing clinics approved the study. Participation in the study was voluntary, and accepting or declining participation did not affect patient care.
Supplemental Material
Download MS Word (31.6 KB)Supplemental Material
Download MS Word (20.3 KB)Supplemental Material
Download MS Word (14.2 KB)Supplemental Material
Download MS Word (14.2 KB)Acknowledgements
The authors thank the hearing clinics and all the participants for their participation in this study. The authors also thank their late colleague – Eila Lonka, PhD – for her valuable contribution in designing the research and the questionnaires on expectations and experiences. Last, but not least, they acknowledge the significant contributions by research assistants Vappu Carlson, Mervi Karhunen, Vilma Martikainen, Tiina Pakka, Juha Ranta, Kati Turunen, and Teija Vaittinen.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article. This article presents independent research, in which the funding source was not involved in any way.
References
- Akaike, H. 1974. “A new look at the statistical model identification.” IEEE Transactions on Automatic Control 19 (6):716–723. doi:10.1109/TAC.1974.1100705.
- Arlinger, S., P. Nordqvist, and M. Öberg. 2017. “International outcome inventory for hearing aids: data from a large Swedish quality register database.” American Journal of Audiology 26 (3S):443–450. doi:10.1044/2017_AJA-16-0123.
- Barker, F., E. Mackenzie, L. Elliot, and S. DeLusignan. 2015. “Outcome measurement in adult auditory rehabilitation: A scoping review of measures used in randomized controlled trials.” Ear and Hearing, 5:1–7. doi:10.1097/AUD.0000000000000167.
- Bertoli, S., D. Bodmer, and R. Probst. 2010. “Survey on hearing aid outcome in Switzerland: Associations with type of fitting (bilateral/unilateral), level of hearing aid signal processing, and hearing loss.” International Journal of Audiology 49 (5):333–346. doi:10.3109/14992020903473431.
- Cieza, A., K. Causey, K. Kamenov, S. Wulf Hanson, S. Chatterji, and T. Vos. 2020. “Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: A systematic analysis for the Global Burden of Disease Study 2019.” The Lancet 396 (10267):2006–2017. doi:10.1016/S0140-6736(20)32340-0.
- Cox, R, and G. Alexander. 2002. The International Outcome Inventory for Hearing Aids (IOI-HA): Psychometric properties of the English version. International Journal of Audiology, 41, 30–35. doi:10.3109/14992020209101309.
- Cox, R. M., D. Stephens, and S. E. Kramer. 2002. “Translations of the international outcome inventory for hearing aids (IOI-HA).” International Journal of Audiology 41 (1):3–26. doi:10.3109/14992020209101307.
- Dawes, P., H. Fortnum, D. R. Moore, R. Emsley, P. Norman, K. Cruickshanks, A. Davis, et al. 2014. “Hearing in middle age: A population snapshot of 40–69-year-olds in the UK.” Ear and Hearing 35:44–51. doi:10.1097/AUD.0000000000000010.
- Hickson, L., L. Worrall, and N. Scarinci. 2007. “A randomized controlled trial evaluating the active communication education program for older people with hearing loss.” Ear and Hearing 28 (2):212–230. doi:10.1097/AUD.0b013e31803126c8.
- Houmøller, S. S., A. Wolff, S. Möller, V. K. Narne, S. K. Narayanan, C. Godballe, D. D. Hougaard, et al. 2022. “Prediction of successful hearing aid treatment in first-time and experienced hearing aid users: Using the International Outcome Inventory for Hearing Aids.” International Journal of Audiology 61 (2):119–129. doi:10.1080/14992027.2021.1916632.
- Hox, J. J. 2010. Multilevel analysis: Techniques and applications. New York: Routledge.
- Knudsen, L. V., M. Öberg, C. Nielsen, G. Naylor, and S. E. Kramer. 2010. “Factors influencing help seeking, hearing aid uptake, hearing aid use, and satisfaction with hearing aids: A review of the literature.” Trends in Amplification 14 (3):127–154. doi:10.1177/1084713810385712.
- Koskela, I., J. Ruusuvuori, P. Juvonen-Posti, N. Nevala, P. Husman, T. Aaltonen, E. Lonka, and M. Laakso. 2016. “Dilemmatic group memberships of hard-of-hearing employees during the process of acquiring and adapting to the use of hearing aids.” International Journal of Rehabilitation Research. Internationale Zeitschrift Fur Rehabilitationsforschung. Revue Internationale de Recherches de Readaptation 39 (3):226–233. doi:10.1097/MRR.0000000000000173.
- Kramer, S. E., S. T. Goverts, W. A. Dreschler, M. Boymans, and J. M. Festen. 2002. “International outcome inventory for hearing aids (IOI-HA): Results from the Netherlands.” International Journal of Audiology 41 (1):36–41. doi:10.3109/14992020209101310.
- Kramer, S. E., T. S. Kapteyn, and T. Houtgast. 2006. “Occupational performance: Comparing normally-hearing and hearing-impaired employees using the Amsterdam Checklist for Hearing and Work.” International Journal of Audiology 45 (9):503–512. doi:10.1080/14992020600754583.
- Kristman, V., M. Manno, and P. Côté. 2003. “Loss to follow-up in cohort studies: How much is too much?” European Journal of Epidemiology 19 (8):751–760. doi:10.1023/b:ejep.0000036568.02655.f8.
- Laakso, M., I. Salmenlinna, T. Aaltonen, I. Koskela, and J. Ruusuvuori. 2019. “Open-class repair initiations in conversations involving middle-age individuals with mild to moderate hearing impairment.” International Journal of Language & Communication Disorders 54 (4):620–633. doi:10.1080/08351813.2019.1572379.
- Lin, F. R., K. Yaffe, J. Xia, Q.-L. Xue, T. B. Harris, E. Purchase-Helzner, S. Satterfield, H. N. Ayonayon, L. Ferrucci, and E. M. Simonsick, Health ABC Study Group 2013. “Hearing Loss and Cognitive Decline in Older Adults.” JAMA Internal Medicine 173 (4):293–299. doi:10.1001/jamainternmed.2013.1868.
- Little, R. J. A. 1988. “A test of missing completely at random for multivariate data with missing values.” Journal of the American Statistical Association 83 (404):1198–1202. doi:10.2307/2290157.
- Meister, H., S. Rählmann, M. Walger, S. Margolf-Hackl, and J. Kießling. 2015. “Hearing aid fitting in older persons with hearing impairment: The influence of cognitive function, age, and hearing loss on hearing aid benefit.” Clinical Interventions in Aging 10:435–443. doi:10.2147/CIA.S77096.
- Meister, H., M. Walger, D. Brehmer, U.-C. von Wedel, and H. von Wedel. 2008. “The relationship between pre-fitting expectations and willingness to use hearing aids.” International Journal of Audiology 47 (4):153–159. doi:10.1080/14992020701843111.
- Mulrow, C. D., M. R. Tuley, and C. Aguilar. 1992. “Sustained benefits of hearing aids.” Journal of Speech, Language, and Hearing Research 35 (6):1402–1406. doi:10.1044/jshr.3506.1402.
- OECD Labor Force Statistics. 2021. Working Age Population (Indicator) doi:10.1787/d339918b-en.
- Perez, E, and B. A. Edmonds. 2012. “A systematic review of studies measuring and reporting hearing aid usage in older adults since 1999: A descriptive summary of measurement tools.” PLoS One 7 (3):e31831. doi:10.1371/journal.pone.0031831.
- Ruusuvuori, J., T. Aaltonen, E. Lonka, I. Salmenlinna, and M. Laakso. 2020. “Discussing hearing aid rehabilitation at the hearing clinic: Patient involvement in deciding upon the need for a hearing aid.” Health Communication 35 (9):1146–1161. doi:10.1080/10410236.2019.1620410.
- Saunders, G. H., M. S. Lewis, and A. Forsline. 2009. “Expectations, prefitting counseling, and hearing aid outcome.” Journal of the American Academy of Audiology 20 (5):320–334. doi:10.3766/jaaa.20.5.6.
- Schow, R. L, and M. A. Nerbonne. 1980. “Hearing handicap and Denver scales: Applications, categories, interpretation.” Journal of the American Academy of Audiology 13:66–77. doi:10.1177/108471380100500303.
- Schwarz, G. E. 1978. “Estimating the dimension of a model.” Annals of Statistics 6:461–464. doi:10.1214/aos/1176344136.
- Solheim, J, and L. Hickson. 2017. “Hearing aid use in the elderly as measured by datalogging and self-report.” International Journal of Audiology 56 (7):472–473. doi:10.1080/14992027.2017.1303201.
- Staehelin, K., S. Bertoli, R. Probst, C. Schindler, J. Dratva, and E. Z. Stutz. 2011. “Gender and hearing aids: Patterns of use and determinants of nonregular use.” Ear and Hearing 32 (6):e26–e37. doi:10.1097/AUD.0b013e3182291f94.
- Tambs, K. 2004. “Moderate effects of hearing loss on mental health and subjective well-being: Results from the Nord-Trøndelag hearing loss study.” Psychosomatic Medicine 66 (5):776–782. doi:10.1097/01.psy.0000133328.03596.fb.
- Tsimpida, D., E. Kontopantelis, D. M. Ashcroft, and M. Panagioti. 2021. “The dynamic relationship between hearing loss, quality of life, socioeconomic position, and depression and the impact of hearing aids: Answers from the English Longitudinal Study of Aging (ELSA).” Social Psychiatry and Psychiatric Epidemiology 57 (2):353–362. doi:10.1007/s00127-021-02155-0.
- Tuley, M. R., C. D. Mulrow, C. Aguilar, and R. Velez. 1990. “A critical reevaluation of the quantified Denver scale of communication function.” Ear and Hearing 11 (1):56–61. doi:10.1097/00003446-199002000-00011.
- Vestergaard, M. D. 2006. “Self-report outcome in new hearing aid users: Longitudinal trends and relationships between subjective measures of benefit and satisfaction.” International Journal of Audiology 45 (7):382–392. doi:10.1080/14992020600690977.
- Wu, X., Y. Ren, Q. Wang, B. Li, H. Wu, Z. Huang, and X. Wang. 2019. “Factors associated with the efficiency of hearing aids for patients with age-related hearing loss.” Clinical Interventions in Aging 14:485–492. doi:10.2147/CIA.S190651.
