Abstract
Objectives
The objective of this study is (1) to assess whether the presentation level of the antiphasic digits-in-noise (DIN) test affects the speech recognition threshold (SRT), (2) to evaluate how accurately simulated unilateral and bilateral conductive hearing loss is detected (CHL) and (3) to determine whether increasing the presentation level normalises the antiphasic DIN SRT.
Design
Participants performed antiphasic and diotic DINs at different presentation levels with unilateral, bilateral or no earplugs.
Study sample
Twenty-four and twelve normal hearing adults.
Results
Without earplugs, antiphasic DIN SRTs did not differ between 60 and 80 dB SPL. At 60 dB SPL, the antiphasic DIN correctly classified 92% of the unilateral earplug cases; the diotic DIN 25%. The binaural intelligibility level difference did not differ between the no-earplug condition and the condition with bilateral earplugs when the presentation was increased with the attenuation level.
Conclusions
In normal hearing participants, diotic and antiphasic DIN SRTs are independent of presentation level above a minimum level of 60 dB SPL. The antiphasic DIN is more sensitive than the diotic DIN for detecting unilateral CHL; not for bilateral CHL. The effect of CHL on DIN SRTs can be largely compensated by increasing the presentation level. Audibility plays an important role in the antiphasic and diotic DIN.
Introduction
Hearing loss can have an immense impact on quality of life and affects 6–8% of the world population (Wilson et al. Citation2017). Early identification of hearing loss is a key element to effective management. This requires systematic screening for detection of hearing loss. It has been demonstrated that hearing screening for children and adults can be done remotely via telecommunications and has the advantage to reach a large global audience without the need of an examiner (Culling et al. Citation2005; Jansen et al. Citation2010; Leensen et al. Citation2011; Smits et al. Citation2004; Smits et al. Citation2006; Swanepoel et al. Citation2019).
There are a number of online hearing screening methods available that are valid and sensitive to detecting sensorineural hearing loss (SNHL) (De Sousa, Smits, et al. Citation2020; Denys, De Laat, et al. Citation2019; Lancaster et al. Citation2008). A commonly used example is the digits-in-noise test (DIN), a self-test that individuals can take via internet or a smartphone app (Potgieter et al. Citation2018; Smits et al. Citation2013; Watson et al. Citation2012; Zokoll et al. Citation2012). The DIN assesses speech recognition ability in noise and uses digit triplets presented in speech-shaped noise in an adaptive procedure to measure the speech recognition threshold (SRT). Although digits are not entirely representative of speech in daily listening, there is a strong positive correlation between speech-in-noise tests with open-set materials (Plomp and Mimpen Citation1979) and the DIN test (R = 0.96) (Smits et al. Citation2013). The SRT is the signal-to-noise ratio, expressed in dB SNR, at which the listener recognises 50% of the digit triplets. The screening version of the DIN provides a pass or refer result based on the obtained SRT (Smits et al. Citation2004). Besides being an automated screening tool, the DIN is also used in clinics for diagnostic purposes (Cullington and Aidi Citation2017; Kaandorp et al. Citation2015; Smits et al. Citation2013) and has been subject to modifications to further improve the efficiency of the test (Dambha et al. Citation2022; Denys, Hofmann, et al. Citation2019; Motlagh Zadeh et al. Citation2019; Smits Citation2017). For an overview of the DIN test and its variants, we refer to the scoping review by Van den Borre et al. (Citation2021).
An important limitation of many remote hearing screening tests, including traditional DIN variants, is that they fail to detect conductive hearing loss (CHL) (Smits et al. Citation2004). CHL is caused by an obstruction to the sound transmission of the external or middle ear. Causes of CHL include cerumen (earwax) in the ear canal, otosclerosis and otitis media with effusion (OME). Standard monaural or diotic DINs are insensitive to CHL because the attenuation caused by CHL can be compensated by increasing the presentation level of the test, which is typically self-selected by the listener (De Sousa, Swanepoel, et al. Citation2020). De Sousa, Smits, et al. (Citation2020) demonstrated that a combination of remote pure-tone air conduction audiometry and a standard diotic DIN test can be used to distinguish SNHL from CHL: the CHL group has near-normal DIN SRTs with elevated pure-tone air conduction thresholds, whereas the SNHL group has poor DIN SRTs and elevated thresholds.
A recent DIN variant, the antiphasic DIN, has been shown to detect symmetric SNHL, as well as unilateral and CHL (De Sousa et al. Citation2021; De Sousa, Swanepoel, et al. Citation2020). In the antiphasic DIN, the speech signal (i.e. the digits) is phase-inverted between the ears and the noise is inter-aurally in-phase (N0Sπ). Traditionally, the DIN presents the speech and noise identically and simultaneously to both ears (diotic, N0S0). Unless the ears are sequentially (monaurally) tested, the diotic DIN has the additional limitation that it leaves unilateral loss undetected, as the outcome is based on the performance of the better ear. De Sousa, Swanepoel, et al. (Citation2020) demonstrated that antiphasic digit presentation significantly improved the sensitivity of the DIN for detecting all types of hearing loss. In a follow-up study, they suggested a two-step procedure, first an antiphasic DIN and then a diotic DIN, to classify hearing into three categories: (1) normal hearing, (2) bilateral SNHL and (3) unilateral or asymmetric SNHL or CHL (De Sousa et al. Citation2021).
The ability of the antiphasic DIN to detect CHL relies on a mechanism called binaural unmasking and, specifically, on inter-aural time difference (ITD) cues. In spatial hearing, normal hearing listeners can take full advantage from subtle differences between sound entering the left and right ear; the inter-aural level differences (ILDs) and ITDs. ITDs as small as 10 µs can be detected (Brughera et al. Citation2013) and play a role in listening in noise and localising sound. CHL can distort these acoustic temporal cues (Hartley and Moore Citation2003). The antiphasic DIN introduces ITDs by presenting stimuli with a maximum inter-aural phase difference of 180°. Note that, technically, we induce a fixed inter-aural phase difference (IPD) instead of a fixed, frequency-independent ITD. In normal hearing listeners, antiphasic SRTs are ∼5 dB better than diotic SRTs for the DIN (Smits et al. Citation2016). The benefit, the difference in SRT between antiphasic and diotic presentation, is called the binaural intelligibility level difference (BILD). Listeners with some form of hearing loss experience a smaller BILD than normal hearing listeners due to subtle timing irregularities between the ears at the level of the auditory brainstem. These listeners are therefore more likely to have worse SRTs on the antiphasic DIN.
De Sousa, Swanepoel, et al (Citation2020) studied the sensitivity of the antiphasic DIN for detecting hearing loss, including CHL, in patients using a between-subject design and self-selected presentation levels. The variability in presentation levels, the degree of CHL and difference in CHL between the left and right ear were large in this study population. To explore possible further gains in sensitivity of the DIN to detect CHL, the aim of the present study was to systematically assess the effect of CHL on the antiphasic DIN SRTs in a controlled setting. Normal hearing participants were tested in a laboratory setting with experimentally induced CHL. By simulating CHL, the participants form their own control group. However, longer-term plasticity of binaural interaction to CHL is not taken into account (Hogan and Moore Citation2003; Parry et al. Citation2019; Thornton et al. Citation2021).
In the present study, earplugs were used to simulate unilateral and bilateral CHL. Several studies have used earplugs as a method to experimentally induce CHL in animals (Hartley and Moore Citation2003; Knudsen et al. Citation1984; Lupo et al. Citation2011) and in humans (Kumpik et al. Citation2010; Niccum et al. Citation1987; Speaks et al. Citation1983). CHL induced by acoustic foam results in substantial changes in the magnitudes of both the ITD and ILD cues (Lupo et al. Citation2011). Hartley and Moore (Citation2003) examined the effect of earplugs on sound transmission in gerbils and found frequency-dependent delays ranging from ∼250 μs at lower frequencies (1–6 kHz) to ∼20 μs at higher frequencies (8–16 kHz), but with large between-animal variability despite the relatively controlled placement of the earplugs. They also found that the acoustic effect of middle ear effusions and earplugs is similar (Hartley and Moore Citation2003). In humans, a unilateral earplug has been shown to create mean delays of 150 ± 82 µs, with large between-subject variability but constant across test sessions (Kumpik et al. Citation2010). Thornton et al. (Citation2012) simulated CHL in animals by filling the middle ear with silicone oil and found that the magnitude of the sound transmission delays, measured by cochlear microphonic amplitudes and phases, was comparable to the delays produced by earplugs. They suggested that earplugs are a viable method to experimentally implement a clinically relevant laboratory model of chronic, yet reversible CHL expected to result from OME (Thornton et al. Citation2012).
Plomp (Citation1986) demonstrated that, for noise levels representative of natural listening conditions, the monaural SRT is unaffected by presentation level. Thus, once the external masking noise is the factor limiting the audibility of speech, the SRT will become constant. This is an essential property of the SRT when used for self-screening purposes. It means that one diagnostic cut-off SRT can be used and that the measurement conditions are not critical (Smits et al. Citation2004).
Two experiments were conducted in the present study. The objectives of Experiment 1 were, first, to determine whether the presentation level of the antiphasic DIN affects the SRT and, second, to assess the screening characteristics of the diotic and antiphasic DIN in terms of their relative ability to distinguish between unilateral and bilateral CHL. The objective of Experiment 2 was to assess whether increasing the overall presentation level by the attenuation level due to bilateral CHL affects the antiphasic DIN SRT. We hypothesised that the antiphasic SRT for normal hearing listeners is unaffected by presentation level. However, there is currently only limited evidence that this is the case (Goverts and Houtgast Citation2010; Speaks et al. Citation1983; Wilson et al. Citation1994). Several studies reported on the effect of CHL on the antiphasic SRT and BILD (De Sousa, Swanepoel, et al. Citation2020; Niccum et al. Citation1987; Olsen et al. Citation1976; Quaranta and Cervellera Citation1974). To our knowledge, no studies have explored whether compensation of the CHL by increasing the overall presentation level could fully compensate for a reduction in the antiphasic SRT or BILD.
Experiment 1
In the first experiment, the effect of presentation level on the antiphasic and diotic DIN SRTs was evaluated for participants with normal hearing, and unilateral and bilateral simulated CHL. The ability of the diotic and antiphasic DIN to discriminate between normal hearing, unilateral CHL and bilateral CHL was also assessed.
Participants
Twenty-four young native Dutch-speaking adults (mean age 23; range 18–27 years; 17 females) participated. Only individuals with pure tone thresholds ≤ 20 dB HL (ISO Citation2017, 389-1:2017) for all octave frequencies from 0.25 to 8 kHz and type A tympanograms in both ears were included. Participants were recruited from the University campus. They were paid and gave written informed consent. The study was approved by the medical research ethics committee VUmc (protocol number: 2020.489).
Materials and methods
Testing equipment
A standard clinical audiometer (Decos audiology) equipped with Sennheiser HDA200 headphones was used to measure pure-tone thresholds with and without earplugs. The same type of headphones was used to present DIN stimuli through a Sound Blaster Creative soundcard (THX) connected to a PC (Dell Optiplex 780). A Madsen Zodiac 2 tympanometer was used to assess middle-ear function. All testing took place in a soundproof booth.
DIN procedure
The stimuli from the standard Dutch DIN were used (Smits et al. Citation2013). Digits (0–9) were uttered by a trained male speaker and spectrally matched noise was created. Level corrections were applied to ensure equal recognition probabilities for the different digits. All digits were used, including the two-syllable Dutch digits seven /zevən/ and nine /nexən/, as recommended by Smits (Citation2016). A random set of 24 digit triplets was chosen from a set of 120 digit triplets for each SRT measurement. In the diotic DIN, both digits and noise were presented identically to both ears. In the antiphasic DIN, digits were presented phase-inverted between the ears and the noise was bilaterally in-phase. A one-down, one-up adaptive procedure was used to obtain the SRT. In this procedure, following each correct response, the SNR level was reduced by 2 dB and following each incorrect response, the SNR was increased by 2 dB. The overall presentation level, i.e. the level of the mixed speech and noise signal, was kept constant for each presentation, meaning that both the speech level and noise level changed for each 2-dB change in SNR. All three digits had to be correct for a response to be scored as correct. The initial overall sound level for the measurements in quiet (digits only) was 30 dB SPL for the condition without earplugs and with a unilateral earplug, and 50 dB SPL for the condition with bilateral earplugs. A similar one-down, one-up adaptive procedure was used. All equipment was calibrated prior to the experiment using a Brüel and Kjaer artificial ear (Type 4152) with a flat-plate adaptor. The initial SNR for all measurements in noise (digits + noise) was −2 dB. Note that the sound levels may vary at each ear, especially when wearing earplugs, as these are not real ear measures. SRTs were estimated as the average of the last 20 SNRs from a total of 25 SNRs (the 25th SNR was based on the SNR and response of the 24th presentation). Every DIN test took <2 min to complete.
Earplugs
Disposable foam earplugs (Honeywell, type ‘Howard Leight Max Lite’) were used. These are commercially available and reportedly have attenuation levels of 30, 32 and 38 dB for the low (0.25 − 0.5 kHz), mid (1 − 2 kHz) and high (4 − 8 kHz) frequencies, respectively. The earplugs were carefully inserted by the participants according to the instructions. The placement of the earplugs was checked by the examiner and they were reinserted if necessary.
Test procedure
A within-subject repeated measures experimental study design was used. The participant was seated in a sound treated booth with a computer with which they performed the DIN tests. The tests were presented in three listening conditions: without earplugs, with a unilateral earplug and with bilateral earplugs. Pure-tone measurement with earplugs was done immediately before the DIN condition with bilateral earplugs, so that the plugs did not need to be reinserted and the attenuation did not change between threshold and DIN SRT measurement. Pure-tone audiometry without earplugs was always done at the beginning of the experiment. For the unilateral earplug condition, the plugged side (left or right ear) was alternated between participants and was always either followed or preceded by the two earplug condition so that the earplug did not need to be reinserted. The four remaining possible orders of the three listening conditions were counter-balanced across participants.
In each condition, one antiphasic digits-in-quiet test and three antiphasic DIN tests at fixed overall levels of 40, 60 and 80 dB SPL were presented. Subsequently, two diotic DIN tests were presented at 60 and 80 dB SPL. The order of the overall presentation levels was randomised across participants but was kept fixed for all three listening conditions. In the first condition, the participants started with an antiphasic DIN that was not scored to mitigate a potential DIN training effect (Smits et al. Citation2013).
Eighteen scores per participant were recorded: for each of the three listening conditions, antiphasic DIN SRTs were measured in quiet and in noise at 40, 60 and 80 dB SPL overall presentation level, and diotic DIN SRTs were measured at 60 and 80 dB SPL overall presentation level. The total duration of the testing procedure was ∼1 h, including short breaks between listening conditions.
Statistical analysis
Statistical analyses were conducted in R studio (version 3.4.2). Plots were created in GraphPrisma. Repeated measures analyses of variance (ANOVA) were performed to compare the means of three groups. Post-hoc paired t-tests were done for 2 by 2 comparisons and Bonferroni corrections were applied, setting the alpha level to 0.017 (i.e. 0.05/3). Pearson correlation coefficients were calculated for the associations between the SRTs and pure tone averages (PTAs, i.e. average threshold at 0.5, 1, 2 and 4 kHz).
Results
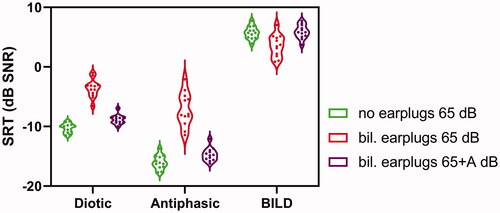
The mean pure-tone thresholds of the 48 ears of the 24 participants with and without earplugs are shown in (left panel). The pure-tone thresholds clearly show that the attenuation caused by the earplugs is frequency dependent. The mean PTA with earplugs was 34 ± 7 dB HL and without earplugs 4 ± 3 dB HL. The mean PTA attenuation of the 48 plugged ears was 30 ± 7 dB. The relatively large standard deviation shows that, despite careful placement of the earplugs, there was considerable variation in attenuation among participants. The average inter-aural difference in attenuation was 1 ± 5 dB (min = −9, max = 9).
Figure 1. Hearing thresholds of both ears with and without earplugs of the 24 participants from Exp. 1 (left panel) and of the 12 participants from Exp. 2 (right panel). Filled circles show the average thresholds of both ears per frequency. Dotted lines show the minimum and maximum thresholds per frequency, solid lines the standard deviation per frequency.
Antiphasic digit-triplet recognition in quiet
The speech-in-quiet scores differed between listening conditions (F2,24 = 453.3 p < 0.001). The average speech level for 50% recognition was ∼30 dB higher for the condition with earplugs than without, which is in line with the average attenuation of 30 dB of the earplugs. See Supplementary file for the results of the digits-in-quiet experiment (http://tandfonline.com/doi/suppl).
Effect of the fixed overall presentation level on SRT estimates
The overall presentation level is the level of the mixed speech and noise signal. Because the overall presentation level was constant, the speech level approaches this overall level for high SNRs. Thus, if the participant repeatedly answers incorrectly, the speech level will become approximately equal to the overall presentation level. This resulted in a ceiling effect in some listening conditions, especially at 40 and 60 dB SPL in the bilateral earplugs condition: the maximum speech level was reached, even though the participant was unable to recognise the digit triplets. The ceiling effect is shown in Supplementary Figure SII. To determine the effect of presentation level on SRT, we only included SRT estimates we considered valid and excluded some measurements. To ensure that the adaptive procedure used to determine the SRT works properly, the recognition probability at favourable SNRs should be near 100% (Smits and Houtgast Citation2006). We decided that this maximum speech level must be at least 10 dB higher than the speech level for 50% recognition in quiet to ensure that the recognition probability could reach values near 100% for the conditions in noise. Because of this limitation, we excluded all measurements of the diotic and antiphasic DIN at 40 dB SPL with bilateral earplugs and eight measurements (i.e. measures from eight individuals) at 60 dB SPL with bilateral earplugs. Because of the pairwise comparison, measures of these eight individuals from the 80 dB SPL condition were excluded as well.
Effect of presentation level
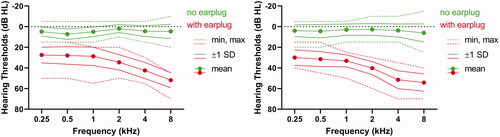
The remaining DIN SRTs for the different overall presentation levels, i.e. the ones that were considered valid as explained in the previous paragraph, are presented in for each listening condition. In the no earplug hearing condition (left panel), the SRTs were not significantly different between the 60 and 80 dB SPL presentation level, both for the antiphasic (p = 0.46) and diotic DIN (p = 0.71). This suggests that, at least above 60 dB SPL, the SRT was independent of presentation level for both DINs. The antiphasic DIN SRTs were worse at 40 dB SPL, most likely due to inaudibility of parts of the speech.
Figure 2. Violin plots of the antiphasic and diotic SRTs for 40 (green), 60 (orange) and 80 dB SPL (blue) overall presentation levels for no earplugs (left panel), a unilateral earplug (mid panel) and bilateral earplugs (right panel).
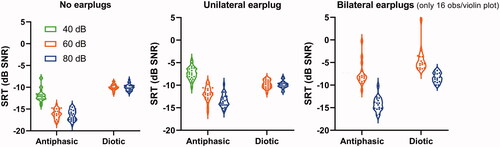
In the condition with bilateral earplugs (right panel), SRTs were lower (better) at 80 dB SPL presentation level than at 60 dB SPL for both the antiphasic and diotic DIN. Note that the effective level was ∼30 and 50 dB SPL due to the attenuation of the earplugs, and inaudibility probably had an effect at these lower presentation levels. In the unilateral earplug condition (mid panel), the diotic DIN SRTs were similar at 60 and 80 dB SPL; the antiphasic DIN SRTs seemed affected by audibility in this condition as well.
Screening characteristics
The lower panels of show the diotic SRT, antiphasic SRT and BILD as a function of the poorer ear PTA for the three listening conditions at a presentation level of 60 dB SPL. The vertical dotted lines at 20 dB HL distinguish normal hearing and hearing loss in the poorer ear. The horizontal dotted lines in represent the SRT of the pass/fail criteria, which are −8.9 dB SNR for the diotic DIN, −14.8 dB SNR for the antiphasic DIN and 4.1 dB SNR for the BILD. These measures were obtained by taking the 95th percentile (inclusive) of the SRTs in the normal hearing (i.e. no earplugs) condition at 60 dB SPL presentation level. The dotted lines divide the plots into quadrants. The lower left and upper right quadrant represents the correctly classified cases. The lower right quadrant represents false negatives and the upper left quadrant the false positives. The percentages and numbers of correctly classified cases are presented in . The upper panels in show data for the 80 dB SPL presentation levels. The percentages of correctly classified participants are lower for 80 dB SPL than for 60 dB SPL (). A large effect of presentation level was found for the BILD where 8% of the participants with bilateral CHL had a BILD outside normal limits for 80 dB SPL, whereas this percentage was 75% for 60 dB SPL. shows that screening characteristics for CHL were generally better for the antiphasic DIN than for the diotic DIN and BILD.
Figure 3. Scatter plots of the SRTs and the poorer ear PTA for the diotic SRT, antiphasic SRT and the BILD in function of the poorer ear PTA for presentation levels of 80 and 60 dB SPL (top and lower panels, respectively). The horizontal lines represent the SRT cut-off and the vertical lines distinguish normal hearing and hearing loss in the poorer ear.
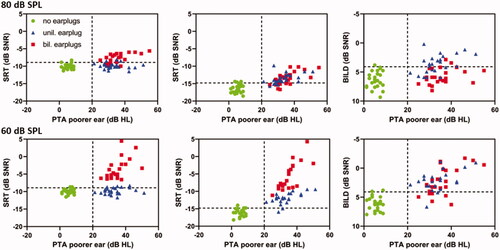
Table 1. Percentages and absolute numbers (n, number of participants out of 24) of correctly classified cases of the diotic and antiphasic DIN for unilateral and bilateral CHL at different presentation levels and the BILD.
Experiment 2
Experiment 1 showed that the antiphasic DIN SRTs significantly improved for the condition with bilateral earplugs by increasing the presentation level from 60 to 80 dB SPL. In addition, it showed that at a relatively high presentation level of 80 dB SPL, audibility probably still played a role with bilateral earplugs. Following these results, an important question arose: Can the antiphasic DIN SRTs in people with (simulated) CHL further improve by increasing the overall presentation level to fully compensate for the attenuation of the CHL? To answer this question, an additional experiment was conducted.
Participants
Twelve new participants were recruited (mean age 27; range 19–42 years; 6 females). Pure-tone thresholds were better than 20 dB HL for all octave frequencies from 0.25 to 8 kHz, except for one subject with a threshold of 25 dB HL at 8 kHz in one ear. All participants had bilateral type A tympanograms and gave written informed consent.
Materials and methods
The testing equipment (audiometer, soundcard, headphones, tympanometer and earplugs) was the same as in Experiment 1.
A within-subject repeated measures study design was used. Pure-tone thresholds (without earplugs) were measured prior to performing the DIN tests. There were two listening conditions: without earplugs and with bilateral earplugs. The order of the conditions was counter-balanced across participants. The pure-tone thresholds with earplugs were measured right before the condition with bilateral earplugs. In the condition without earplugs, the participants performed two antiphasic and two diotic DIN tests (test–retest) at an overall presentation level of 65 dB SPL. In the condition with bilateral earplugs, the participants also performed two antiphasic and two diotic DINs at 65 dB SPL, and additionally, two antiphasic and two diotic DINs at 65 dB SPL incremented by the average PTA attenuation of both ears (denoted 65 + A dB SPL). The attenuation (A) was computed by subtracting the average PTA of both plugged ears with the average PTA of both unplugged ears. This way, the presentation level was determined for each participant individually, aiming to fully compensate for the attenuation due to the simulated CHL. The initial SNR for the measurements in noise was −2 dB SPL. In the first condition, the participants started with a DIN that was not scored to surpass a potential training effect. The total duration of the testing procedure was ∼45 min.
Statistical analysis
Statistical analyses were conducted in R studio (version 3.4.2) and plots were created in GraphPrisma. Paired Wilcoxon signed-rank tests were used to compare groups due to the small sample size (n = 12). The average of the test–retest measure was taken to calculate the individual SRTs.
Results
The participants’ pure-tone thresholds with and without earplugs are shown in (right panel). The measured average PTA attenuation across participants was 39 ± 5 dB HL, which is almost 10 dB higher than in Experiment 1. The average inter-aural difference in attenuation was 1 ± 5 dB (min = −4, max = 10).
The antiphasic and diotic DIN SRTs are presented in . At a 65 dB SPL overall presentation level, the antiphasic and diotic SRTs were clearly higher (worse) with bilateral earplugs compared with no earplugs (both p < 0.001), which is in line with the results from Experiment 1. When the presentation level was increased with the amount of attenuation caused by the earplugs, the median SRTs improved by 6.8 dB for the antiphasic and 5.3 dB for the diotic DIN. However, these SRTs were still significantly different from the SRTs without earplugs at 65 dB SPL (antiphasic DIN: difference = 1.4 dB, p = 0.027; diotic DIN: difference = 1.1 dB, p = 0.003). The BILD was not significantly different for the condition without earplugs at 65 dB SPL and with earplugs at 65 + A dB SPL (p = 0.791). Thus, the antiphasic advantage in normal hearing ears did not differ significantly from that in ears with bilateral earplugs when the attenuation was fully compensated. The overall test–retest variability was R = 0.924.
Discussion
Effect of presentation level on DIN SRTs in normal hearing listeners
The antiphasic and diotic DIN SRTs are independent of presentation level in normal hearing listeners, at least above a minimum presentation level of 60 dB SPL. This was demonstrated as the antiphasic and diotic SRTs in the normal hearing condition did not differ significantly at overall presentation levels of 60 and 80 dB SPL. The independence of the presentation level of the diotic SRT has already been established in previous research (Plomp Citation1986), but not for the antiphasic SRT.
Effect of presentation level on DIN SRTs in listeners with simulated CHL
In the condition with bilateral earplugs, the SRTs were better at 80 dB SPL than at 60 dB SPL for both the antiphasic DIN and the diotic DIN. This is due to inaudibility of parts of the speech in both the antiphasic and diotic DIN for the lower presentation level. So the effect of earplugs can at least partly be compensated by increasing the volume. In addition, the scores of the diotic DIN presented at 80 dB SPL were significantly worse with bilateral earplugs compared with no earplugs or a unilateral earplug. Typically, a person with symmetrical CHL would be able to overcome the attenuation of the standard diotic signals by increasing the overall presentation level and thereby achieve near-normal standard SRTs (De Sousa et al, Swanepoel, et al. Citation2020). The presentation level of 80 dB SPL from Experiment 1 was not high enough to compensate for the average earplug attenuation of 30 dB.
Experiment 2 was conducted to determine whether the antiphasic and diotic SRT would further improve by increasing the presentation level in listeners with CHL induced by earplugs. In line with the results from Experiment 1, the SRTs were significantly poorer with earplugs than without for both the antiphasic and diotic DIN (both p < 0.001) at an overall presentation level of 65 dB SPL. However, when the presentation level was increased with the individually measured attenuation of the earplugs, the scores greatly improved in the condition with bilateral earplugs: the average antiphasic SRT decreased by 6.8 dB and the diotic DIN by 5.3 dB. Although the scores without earplugs at 65 dB SPL were still slightly better than with earplugs at 65 + A dB SPL, the BILD did not significantly differ in the no earplug condition compared with the 65 + A dB SPL condition with bilateral earplugs. These results show that CHL can be compensated to a large extent by increasing the presentation level and thus the audibility. Not only is this the case for the diotic DIN, but also for the antiphasic DIN.
These results are surprising given the findings of De Sousa, Swanepoel, et al. (Citation2020), who found that the antiphasic DIN was able to detect bilateral CHL. Two possible reasons for the difference between our results and the results from De Sousa, Swanepoel, et al. (Citation2020) are, first, the self-selected presentation level, and second, the likelihood of asymmetry in hearing loss of the patients with CHL in the study population of De Sousa and colleagues. Although the variance in attenuation among the participants of this study is high, the inter-aural differences are very small. It is plausible that in a clinical group of patients with CHL, the inter-aural attenuation differences are generally greater than the maximum of 10 dB found in our experimental data with earplugs. Indeed, bilateral CHL as a result of otosclerosis is usually asymmetric (Crompton et al. Citation2019) and acute otitis media is typically unilateral in adults (Searight et al. Citation2021). In children, the ratio of unilateral/bilateral OME is unclear: one study reported a 39/61 ratio (n = 2026) for unilateral/bilateral OME (Leibovitz et al. Citation2007), another study 58/42 (n = 232) (Uitti et al. Citation2013). Still, bilateral OME does not necessarily mean symmetrical CHL. Early research found that a difference in inter-aural presentation level affects the masking-level difference (MLD) in normal hearing listeners (Feldmann Citation1965; Zerlin Citation1966). Thus, the results from De Sousa and colleagues may be explained by inter-aural threshold differences causing both inter-aural differences in presentation level and disturbed inter-aural timing cues in a clinical population with CHL. In addition, the self-selected presentation level in their study will be typically based on the better ear or the limitation of the equipment, which could deteriorate the antiphasic SRT.
Note that the degree of simulated CHL in this study is quite high compared with most clinical cases of CHL. Studies show that young children with otitis media with effusion (OME) often have little to no hearing loss despite flat or reduced-peak tympanograms (Fria et al. Citation1985; Gravel and Wallace Citation2000; Roberts et al. Citation2004) and, if they do, the hearing loss is usually mild, with average thresholds of 18 − 35 dB HL (Cai and McPherson Citation2017). However, the purpose of the antiphasic test as a screening tool is to detect more severe hearing losses. Therefore, this study used earplugs with attenuation levels of 30–39 dB.
Additionally, note that the configuration of the audiogram is not representative of most clinical cases. People with OME have greater hearing losses in the lower frequencies than in the higher frequencies, in contrast to the participants in our study. Arguably, for greater hearing loss in the lower frequencies a smaller BILD would be expected. Therefore, we expect our results to be similar for clinical CHL cases. However, this needs to be confirmed with a group of CHL patients. In the present study, we used a controlled setting which has the advantage to control for many confounding factors (e.g. degree and kind of hearing loss, age, cognitive abilities) and we were able to manipulate CHL within participants. Previous publications (De Sousa, Swanepoel, et al. Citation2020; De Sousa et al. Citation2021) lacked essential information, such as the effect of presentation level on antiphasic SRT, while the test has been implemented in several countries.
It cannot be concluded from our data that the antiphasic DIN SRTs for unilateral or bilateral simulated CHL are independent from presentation levels. Given the mean attenuation of 30 dB from Experiment 1, presentation levels of 90 dB SPL and 110 dB SPL would be needed to reach similar sensation levels as for the condition without earplugs (i.e. 60 and 80 dB SPL, respectively). Such high presentation levels are not considered safe for the unilateral CHL condition.
Screening characteristics
This study confirms the results from De Sousa, Swanepoel, et al. (Citation2020) that the antiphasic DIN is more sensitive to detecting unilateral CHL than the diotic DIN. At 60 dB SPL, the antiphasic DIN correctly classified 92% of the unilateral earplug cases and the diotic DIN only 25%. At 80 dB SPL, these numbers dropped to 83% for the antiphasic DIN and 13% for the diotic DIN. However, the antiphasic DIN was not more sensitive to detecting bilateral CHL than the diotic DIN. At 60 dB SPL, all bilateral earplug cases were detected with both the diotic and antiphasic DIN as inaudibility of the speech affected the SRTs in both conditions. When increasing the presentation level to 80 dB SPL, the antiphasic DIN correctly identified 71% of the bilateral earplug cases and the diotic DIN 79% of the cases. It appears that when the inter-aural threshold difference is large (i.e. in the case of a unilateral earplug) the antiphasic DIN is more sensitive than the diotic DIN for detecting CHL, but when the inter-aural difference is small (bilateral earplugs), the sensitivity of the antiphasic and diotic DIN are similar. Note that with low-pass filtered stimuli, for example low-pass filtered digits, a larger antiphasic advantage could have been expected as the masking level difference is largely based on spectral energy below 1 kHz.
Implications for online hearing screening
Our findings have important implications for the way the antiphasic DIN is typically implemented and how accurately CHL may be detected. In the current version of the DIN as a home hearing screening test, the participants set the desired presentation level while listening to digit triplets in quiet. The desired level is largely based on the better ear, and in asymmetric CHL the antiphasic test is likely to detect the loss when the self-selected presentation level is not set too high. However, participants with considerable CHL on both sides are expected to set the desired presentation level much higher, which will improve their results. The results of this study imply that it is important that the presentation level is not set too high or too low when taking the screening test. Maybe this could be achieved by using stimulus files in the test application that result in relatively low presentation levels with the device’s volume control set to maximum, or alternatively by having another person with subjective normal hearing set the desired level. On the other hand, the self-selected presentation level on the device could be an indication of the degree of hearing impairment. Although it is often not possible to know the exact level, the placement of the selected level within the volume range of the device can be recorded.
Conclusion
Our results show that: (1) in normal hearing listeners, the diotic and antiphasic DIN SRTs are independent of presentation level above a minimum level, (2) the antiphasic DIN is more sensitive than the diotic DIN for detecting simulated unilateral CHL, but not for detecting simulated bilateral CHL and (3) increasing the presentation level can, to a large extent, compensate for the effect of a simulated bilateral CHL on the antiphasic DIN SRTs for participants with small inter-aural threshold differences.
Supplemental Material
Download MS Word (123 KB)Acknowledgements
The authors thank Hans van Beek for creating the software of the experiments. David Moore receives support from the NIHR Manchester Biomedical Research Centre.
Disclosure statement
D.W.S. and D.R.M. have a relationship with the hearX Group which includes equity, consulting and potential royalties.
Data availability statement
The data that support the findings of this study are available from the corresponding author, S. Polspoel, upon reasonable request.
Additional information
Funding
References
- Brughera, A., L. Dunai, and W. M. Hartmann. 2013. “Human interaural time difference thresholds for sine tones: the high-frequency limit.” The Journal of the Acoustical Society of America 133 (5): 2839–2855. doi:10.1121/1.4795778.
- Cai, T, and B. McPherson. 2017. “Hearing loss in children with otitis media with effusion: a systematic review.” International Journal of Audiology 56 (2): 65–76. doi:10.1080/14992027.2016.1250960.
- Crompton, M., B. A. Cadge, J. L. Ziff, A. J. Mowat, R. Nash, J. A. Lavy, H. R. F. Powell, C. P. Aldren, S. R. Saeed, and S. J. Dawson. 2019. “The epidemiology of otosclerosis in a British cohort.” Otology & Neurotology 40 (1): 22–30. doi:10.1097/MAO.0000000000002047.
- Culling, J. F., F. Zhao, and D. Stephens. 2005. “The viability of speech-in-noise audiometric screening using domestic audio equipment.” International Journal of Audiology 44 (12): 691–700. doi:10.1080/14992020500267017.
- Cullington, H. E, and T. Aidi. 2017. “Is the digit triplet test an effective and acceptable way to assess speech recognition in adults using cochlear implants in a home environment?” Cochlear Implants International 18 (2): 97–105. doi:10.1080/14670100.2016.1273435.
- Dambha, T., W. Swanepoel, F. Mahomed-Asmail, K. C. De Sousa, M. A. Graham, and C. Smits. 2022. “Improving the efficiency of the digits-in-noise hearing screening test: a comparison between four different test procedures.” Journal of Speech, Language, and Hearing Research 65 (1): 378–391. doi:10.1044/2021_JSLHR-21-00159.
- De Sousa, K. C., C. Smits, D. R. Moore, H. C. Myburgh, and W. Swanepoel. 2020. “Pure-tone audiometry without bone-conduction thresholds: using the digits-in-noise test to detect conductive hearing loss.” International Journal of Audiology 59 (10): 801–808. doi:10.1080/14992027.2020.1783585.
- De Sousa, K. C., C. Smits, D. R. Moore, H. C. Myburgh, and W. Swanepoel. 2021. “Diotic and antiphasic digits-in-noise testing as a hearing screening and triage tool to classify type of hearing loss.” Ear Hear 43(3):1037–1048. doi:10.1097/AUD.0000000000001160.
- De Sousa, K. C., W. Swanepoel, D. R. Moore, H. C. Myburgh, and C. Smits. 2020. “Improving sensitivity of the digits-in-noise test using antiphasic stimuli.” Ear and Hearing 41 (2): 442–450. doi:10.1097/AUD.0000000000000775.
- Denys, S., J. De Laat, W. Dreschler, M. Hofmann, A. van Wieringen, and J. Wouters. 2019. “Language-independent hearing screening based on masked recognition of ecological sounds.” Trends in Hearing 23:2331216519866566. doi:10.1177/2331216519866566.
- Denys, S., M. Hofmann, A. van Wieringen, and J. Wouters. 2019. “Improving the efficiency of the digit triplet test using digit scoring with variable adaptive step sizes.” International Journal of Audiology 58 (10): 670–677. doi:10.1080/14992027.2019.1622042.
- Feldmann, H. 1965. “The role of interaural intensity differences and time delay for signal detection in noise.” International Audiology 4 (2): 29–34. doi:10.3109/05384916509074096.
- Fria, T. J., E. I. Cantekin, and J. A. Eichler. 1985. “Hearing acuity of children with otitis media with effusion.” Archives of Otolaryngology 111 (1): 10–16. doi:10.1001/archotol.1985.00800030044003.
- Goverts, S. T, and T. Houtgast. 2010. “The binaural intelligibility level difference in hearing-impaired listeners: the role of supra-threshold deficits.” The Journal of the Acoustical Society of America 127 (5): 3073–3084. doi:10.1121/1.3372716.
- Gravel, J. S, and I. F. Wallace. 2000. “Effects of otitis media with effusion on hearing in the first 3 years of life.” Journal of Speech, Language, and Hearing Research : JSLHR 43 (3): 631–644. doi:10.1044/jslhr.4303.631.
- Hartley, D. E, and D. R. Moore. 2003. “Effects of conductive hearing loss on temporal aspects of sound transmission through the ear.” Hearing Research 177 (1-2): 53–60. doi:10.1016/S0378-5955(02)00797-9.
- Hogan, S. C, and D. R. Moore. 2003. “Impaired binaural hearing in children produced by a threshold level of middle ear disease.” Journal of the Association for Research in Otolaryngology: JARO 4 (2): 123–129. doi:10.1007/s10162-002-3007-9.
- ISO (2017). ISO 389-1, Acoustics — Reference zero for the calibration of audiometric equipment — Part 1: Reference equivalent threshold sound pressure levels for pure tones and supra-aural earphones. International Organization for Standardization.
- Jansen, S., H. Luts, K. C. Wagener, B. Frachet, and J. Wouters. 2010. “The French digit triplet test: a hearing screening tool for speech intelligibility in noise.” International Journal of Audiology 49 (5): 378–387. doi:10.3109/14992020903431272.
- Kaandorp, M. W., C. Smits, P. Merkus, S. T. Goverts, and J. M. Festen. 2015. “Assessing speech recognition abilities with digits in noise in cochlear implant and hearing aid users.” International Journal of Audiology 54 (1): 48–57. doi:10.3109/14992027.2014.945623.
- Knudsen, E. I., S. D. Esterly, and P. F. Knudsen. 1984. “Monaural occlusion alters sound localization during a sensitive period in the barn owl.” The Journal of Neuroscience 4 (4): 1001–1011. https://www.ncbi.nlm.nih.gov/pubmed/6716127.
- Kumpik, D. P., O. Kacelnik, and A. J. King. 2010. “Adaptive reweighting of auditory localization cues in response to chronic unilateral earplugging in humans.” The Journal of Neuroscience 30 (14): 4883–4894. doi:10.1523/JNEUROSCI.5488-09.2010.
- Lancaster, P., M. Krumm, J. Ribera, and R. Klich. 2008. “Remote hearing screenings via telehealth in a rural elementary school.” American Journal of Audiology 17 (2): 114–122. doi:10.1044/1059-0889(2008/07-0008).
- Leensen, M. C., J. A. de Laat, A. F. Snik, and W. A. Dreschler. 2011. “Speech-in-noise screening tests by internet, part 2: improving test sensitivity for noise-induced hearing loss.” International Journal of Audiology 50 (11): 835–848. doi:10.3109/14992027.2011.595017.
- Leibovitz, E., E. Asher, L. Piglansky, N. Givon-Lavi, R. Satran, S. Raiz, Y. Slovik, A. Leiberman, and R. Dagan. 2007. “Is bilateral acute otitis media clinically different than unilateral acute otitis media?” Pediatric Infectious Disease Journal 26 (7): 589–592. doi:10.1097/INF.0b013e318060cc19.
- Lupo, J. E., K. Koka, B. J. Hyde, H. A. Jenkins, and D. J. Tollin. 2011. “Physiological assessment of active middle ear implant coupling to the round window in Chinchilla lanigera.” Otolaryngology-Head and Neck Surgery 145 (4): 641–647. doi:10.1177/0194599811409674.
- Motlagh Zadeh, L., N. H. Silbert, K. Sternasty, W. Swanepoel, L. L. Hunter, and D. R. Moore. 2019. “Extended high-frequency hearing enhances speech perception in noise.” Proceedings of the National Academy of Sciences 116 (47): 23753–23759. doi:10.1073/pnas.1903315116.
- Niccum, N., C. Speaks, J. Katsuki-Nakamura, and D. Van Tasell. 1987. “Effects of simulated conductive hearing loss on dichotic listening performance for digits.” The Journal of Speech and Hearing Disorders 52 (4): 313–318. doi:10.1044/jshd.5204.313.
- Olsen, W. O., D. Noffsinger, and R. Carhart. 1976. “Masking level differences encountered in clinical populations.” Audiology 15 (4): 287–301. doi:10.3109/00206097609071789.
- Parry, L. V., M. R. D. Maslin, R. Schaette, D. R. Moore, and K. J. Munro. 2019. “Increased auditory cortex neural response amplitude in adults with chronic unilateral conductive hearing impairment.” Hearing Research 372:10–16. doi:10.1016/j.heares.2018.01.016.
- Plomp, R. 1986. “A signal-to-noise ratio model for the speech-reception threshold of the hearing impaired.” Journal of Speech and Hearing Research 29 (2): 146–154. doi:10.1044/jshr.2902.146.
- Plomp, R, and A. M. Mimpen. 1979. “Improving the reliability of testing the speech reception threshold for sentences.” Audiology 18 (1): 43–52. doi:10.3109/00206097909072618.
- Potgieter, J. M., W. Swanepoel, H. C. Myburgh, and C. Smits. 2018. “The South African English smartphone digits-in-noise hearing test: effect of age, hearing loss, and speaking competence.” Ear & Hearing 39 (4): 656–663. doi:10.1097/AUD.0000000000000522.
- Quaranta, A, and G. Cervellera. 1974. “Masking level difference in normal and pathological ears.” Audiology 13 (5): 428–431. doi:10.3109/00206097409071702.
- Roberts, J., L. Hunter, J. Gravel, R. Rosenfeld, S. Berman, M. Haggard, J. Hall, C. Lannon, D. Moore, L. Vernon-Feagans, et al. 2004. “Otitis media, hearing loss, and language learning: controversies and current research.” Journal of Developmental and Behavioral Pediatrics: JDBP 25 (2): 110–122. doi:10.1097/00004703-200404000-00007.
- Searight, F. T., R. Singh, and D. C. Peterson. 2021. Otitis Media With Effusion. In StatPearls. https://www.ncbi.nlm.nih.gov/pubmed/30855877
- Smits, C. 2016. “Comment on ‘International collegium of rehabilitative audiology (ICRA) recommendations for the construction of multilingual speech tests’, by Akeroyd et al.” International Journal of Audiology 55 (4): 268–269. doi:10.3109/14992027.2015.1131339.
- Smits, C. 2017. “Improving the efficiency of speech-in-noise hearing screening tests.” Ear and Hearing 38 (6): e385–e388. doi:10.1097/AUD.0000000000000446.
- Smits, C, and T. Houtgast. 2006. “Measurements and calculations on the simple up-down adaptive procedure for speech-in-noise tests.” The Journal of the Acoustical Society of America 120 (3): 1608–1621. doi:10.1121/1.2221405.
- Smits, C., T. S. Kapteyn, and T. Houtgast. 2004. “Development and validation of an automatic speech-in-noise screening test by telephone.” International Journal of Audiology 43 (1): 15–28. doi:10.1080/14992020400050004.
- Smits, C., P. Merkus, and T. Houtgast. 2006. “How we do it: the Dutch functional hearing-screening tests by telephone and internet.” Clinical Otolaryngology 31 (5): 436–440. doi:10.1111/j.1749-4486.2006.01195.x.
- Smits, C., S. Theo Goverts, and J. M. Festen. 2013. “The digits-in-noise test: assessing auditory speech recognition abilities in noise.” The Journal of the Acoustical Society of America 133 (3): 1693–1706. doi:10.1121/1.4789933.
- Smits, C., C. S. Watson, G. R. Kidd, D. R. Moore, and S. T. Goverts. 2016. “A comparison between the Dutch and American-English digits-in-noise (DIN) tests in normal-hearing listeners.” International Journal of Audiology 55 (6): 358–365. doi:10.3109/14992027.2015.1137362.
- Speaks, C., K. Bauer, and J. Carlstrom. 1983. “Peripheral hearing loss: implications for clinical dichotic listening tests.” The Journal of Speech and Hearing Disorders 48 (2): 135–139. doi:10.1044/jshd.4802.135.
- Swanepoel, W., K. C. De Sousa, C. Smits, and D. R. Moore. 2019. “Mobile applications to detect hearing impairment: opportunities and challenges.” Bulletin of the World Health Organization 97 (10): 717–718. doi:10.2471/BLT.18.227728.
- Thornton, J. L., K. L. Anbuhl, and D. J. Tollin. 2021. “Temporary unilateral hearing loss impairs spatial auditory information processing in neurons in the central auditory system.” Frontiers in Neuroscience 15:721922. doi:10.3389/fnins.2021.721922.
- Thornton, J. L., K. M. Chevallier, K. Koka, J. E. Lupo, and D. J. Tollin. 2012. “The conductive hearing loss due to an experimentally induced middle ear effusion alters the interaural level and time difference cues to sound location.” Journal of the Association for Research in Otolaryngology 13 (5): 641–654. doi:10.1007/s10162-012-0335-2.
- Uitti, J. M., M. K. Laine, P. A. Tahtinen, O. Ruuskanen, and A. Ruohola. 2013. “Symptoms and otoscopic signs in bilateral and unilateral acute otitis media.” Pediatrics 131 (2): e398-405–e405. doi:10.1542/peds.2012-1188.
- Van den Borre, E., S. Denys, A. van Wieringen, and J. Wouters. 2021. “The digit triplet test: a scoping review.” Int J Audiol 60(12):946–963. doi:10.1080/14992027.2021.1902579.
- Watson, C. S., G. R. Kidd, J. D. Miller, C. Smits, and L. E. Humes. 2012. “Telephone screening tests for functionally impaired hearing: current use in seven countries and development of a US version.” Journal of the American Academy of Audiology 23 (10): 757–767. doi:10.3766/jaaa.23.10.2.
- Wilson, B. S., D. L. Tucci, M. H. Merson, and G. M. O'Donoghue. 2017. “Global hearing health care: new findings and perspectives.” Lancet 390 (10111): 2503–2515. doi:10.1016/S0140-6736(17)31073-5.
- Wilson, R. H., C. A. Zizz, and J. L. Sperry. 1994. “Masking-level difference for spondaic words in 2000-msec bursts of broadband noise.” Journal of the American Academy of Audiology 5 (4): 236–242. https://www.ncbi.nlm.nih.gov/pubmed/7949295.
- Zerlin, S. 1966. “Interaural time and intensity difference and the MLD.” The Journal of the Acoustical Society of America 39 (1): 134–137. doi:10.1121/1.1909861.
- Zokoll, M. A., K. C. Wagener, T. Brand, M. Buschermohle, and B. Kollmeier. 2012. “Internationally comparable screening tests for listening in noise in several European languages: the German digit triplet test as an optimization prototype.” International Journal of Audiology 51 (9): 697–707. doi:10.3109/14992027.2012.690078.