Abstract
Objective
Hearing loss is a growing public health issue that significantly impacts both health-related quality of life and working life. This study investigates how hearing rehabilitation with bone conduction hearing implants impacts health-related quality of life and working life in adults of working age with hearing impairment.
Design
This longitudinal study used data from Cochlear’s Implant Recipient Observational Study to assess hearing disabilities and job satisfaction in 18–65-year-old recipients of bone conduction hearing implants. Baseline data were collected pre-implantation and patients were followed-up at 12-months post-implantation.
Study sample
Patient demographics, Health Utilities Index Mark 3, the Speech Spatial and Qualities of Hearing Scale, and self-reported employment data are presented for a sample ranging from 30 to 43 patients, pre-implantation and at 12-months follow-up following implantation with a bone conduction hearing implant.
Results
Significant improvements in hearing and speech attribute, and overall health-related quality of life were observed between pre-and post-implantation. Overall hearing disability decreased post-implantation and job satisfaction improved.
Conclusions
Hearing rehabilitation using bone conduction hearing implants are shown to improve health-related quality of life, reduce hearing disability, and improve work performance and satisfaction. Results are representative of healthy and actively working users of bone conduction hearing implants.
Introduction
Hearing impairment (HI) is the most frequent sensory deficit in humans and it is estimated that by 2050 nearly 2.5 billion people will be living with some degree of hearing loss (Chadha, Kamenov, and Cieza Citation2021). Health-care professionals are frequently consulted by individuals with HI who experience difficulties at work, and studies have shown that HI, regardless of type and degree of hearing loss, is associated with poorer quality of life (Ringdahl and Grimby Citation2000; Gellerstedt and Danermark Citation2004; Hua et al. Citation2013).
Bone Conduction Hearing Devices (BCHDs) are systems that use the natural process of sound travelling through the bone and soft tissue directly to the cochlea. BCHDs consist of an external sound processor that captures and processes sound which is then converted into mechanical vibrations. These vibrations are transmitted to an implant that is anchored to the skull bone, through which they are further conducted to the cochlea. The transmission from the sound processor to the implant happens either percutaneously via an abutment or transcutaneously via a magnetic coupling. With transcutaneous BCHD, the transducer can be an external unit or implanted under the skin and soft tissue, which is referred to as passive versus active BCHD, respectively. For an overview of the different types of available BCHD, we refer to the recent publication by Håkansson et al. (Håkansson et al. Citation2019). BCHD are an effective method of hearing rehabilitation for people with a conductive hearing loss (CHL) or mixed hearing loss (MHL), as they bypass any limitations on sound transmission associated with pathologies or anomalies of the outer or middle ear (Ellsperman et al. Citation2021). These devices can also help patients who suffer from single-sided deafness (SSD) by transmitting sound received on the deaf side directly to the hearing cochlea (Hampton et al. Citation2022). BCHDs bypass the conductive part of the hearing loss and, as such, inherently close the air-bone gap. High levels of satisfaction in relation to sound amplification and speech perception when using BHCDs have been reported in patients with CHL or MHL (Hua, Goossens, and Lewis Citation2022). A recent health technology assessment also concluded that BCHD improve functional, and patient reported outcomes in adults and children with CHL/MHL and SSD (Ontario Health (Quality) Citation2020).
To date, there is no literature on adult users of BCHD in the labour market. However, in a recent literature review by Granberg and Gustafsson (Granberg and Gustafsson Citation2021), it is reported that people with HI show increased unemployment, early retirement due to poor health, and a higher degree of sick leave when compared to the population at large. Research has further confirmed these disadvantages and demonstrated that employees with HI report lower quality of life in terms of reduced participation, autonomy, higher degree of social isolation and problems in the workplace (Kramer, Kapteyn, and Houtgast Citation2006; Danermark and Gellerstedt Citation2004; Danermark and Gellerstedt Citation2004). In a qualitative study by Hua et al. (Citation2015), it was observed that even a mild-moderate aided HI (PTA4 < 40 dB HL bilaterally) can generate far-reaching consequences for employees. Results showed that most participants were aware that difficulties perceived at work, such as communication in groups, loud non-verbal noise, and tinnitus, had a direct negative impact on daily life. The most common feeling was a sense of exclusion, both at work and at home, and fatigue and withdrawal were also perceived as negative consequences of having a HI at work.
Taken together, HI can have unfavourable consequences on the labour market, and studies focussing on job satisfaction and HRQoL on working aged BCHD users are currently very limited. Thus, the aim of the study was to compare job satisfaction and health-related quality of life (HRQoL) in working age adult users of BCHD pre-implantation and post-implantation at 12-month follow-up. A second aim was to examine the subjective assessment of functional hearing pre- and post-implantation in the same population.
Material and methods
The current study uses retrospective data collected as part of the Cochlear Implant Recipient Observational Study (IROS). IROS was a prospective, repeated measures, longitudinal study with intra-subject controls that uses subjective evaluation tools, including the Health Utilities Index Mark 3 (HUI-3) (Horsman et al. Citation2003) and the Speech, Spatial and Qualities of Hearing Scale (SSQ) (Gatehouse and Noble Citation2004), to assess patient-related benefit following the treatment of adults with permanent hearing loss with implantable hearing devices. The registry also collects baseline and follow-up socio-economic information, including employment status. The IROS database is registered on ClinicalTrials.gov with identifier NCT02004353 and its design, implementation and management has been published previously (Grutters et al. Citation2007).
Study population
The study included all patients of working age (18–65 years old) who were implanted with a bone conduction hearing aid and provided baseline and 12-month follow-up data for HUI-3, SSQ, and complete questionnaire data regarding employment status. The registry contains data on 1506 adult patients that have been implanted with a hearing device in total. Of these, 352 were implanted with a bone conduction hearing device. Regarding HUI-3, baseline data pre-implantation with a bone conduction implant was available for 252 patients and 76 of these patients had 12-month follow-up HUI-3 data available. Twelve of these patients were missing SSQ data at 12-month follow-up and were excluded. One additional patient did not complete follow-up and was also excluded. Out of the 63 remaining patients, 20 patients were excluded since they were either retired or not of working age, leaving 43 patients. Demographics and health outcomes data are presented for these patients at baseline and 12-month follow-up.
Questionnaires
Health utilities index mark 3
General HRQoL was measured using the HUI-3, a validated self-reported multi-attribute health status system, which consists of 15 items covering eight health dimensions: vision, hearing, speech, ambulation, dexterity, emotion, cognition, and pain/complaints (Horsman et al. Citation2003). The HUI-3 is sensitive to changes in HRQoL and is recommended for capturing changes in studies evaluating hearing interventions (Grutters et al. Citation2007). The structure of the data also permits the use of parametric testing to support comparisons across studies and datasets. By filling out the HUI-3 instrument, a unique health state can be generated as a sequence of numbers based on the level selected for each dimension. Utility values range from −0.36 (which is considered a health state worse than death) to 1.00 which indicates full/perfect health. A change in overall HRQoL score of 0.03 is considered clinically important and changes in single attribute scores of at least 0.03–0.05 have been shown to be clinically important (Horsman et al. Citation2003).
The speech, spatial and qualities of hearing scale
The SSQ questionnaire is a self-report test of auditory disability consisting of 49 items that question the listener’s abilities in many complex listening situations illustrative of real life. The SSQ is a widely used tool in hearing research and has been reported to be sensitive to changes in hearing disability following treatment with a variety of hearing therapies, including implantable and non-implantable hearing devices (Pennini and Almeida Citation2021; Briggs et al. Citation2022). This questionnaire comprises 14 scored items including speech hearing, 17 items on spatial hearing, and 18 items on other qualities and features of hearing. Individual mean scores are reported for each of these three domains and a global mean is also reported, which is calculated by averaging all response scores. Each item ranges from on a scale from 0 (minimum/not at all) to 10 (maximum/perfectly) across multiple domains presented in the three subscales.
Employment and job satisfaction
Patients were provided with a questionnaire covering vocation and employment opportunities at baseline and at 12-month follow-up. The questionnaire captured whether the patient was engaged in full-time or part-time work, in education, or retired. The questionnaire also captured whether the patient’s hearing abilities impacted their ability to perform their job satisfactorily. Patients were asked whether they felt that their hearing ability had a negative effect on their ability to do their daily work satisfactorily, which was scored as either; not at all (1), sometimes (2), most of the time (3), or always (4). After implantation, patients were asked whether they felt that their hearing ability through their hearing device had a negative effect on their ability to do their daily work satisfactorily. This was also scored using the same scale and answers were scored numerically from 1 to 4, where a lower score represents lower impact.
Statistical analysis
The IBM® SPSS® Statistics Software Package (IBM Corporation, Armonk, NY) was used for statistical analysis. Differences in HUI-3 and SSQ scores were analysed using the Wilcoxon signed-rank test for paired observations since these scores were non-normally distributed (Kolmogorov–Smirnov test for normality, all p < 0.001). Employment impact scores, pre- and post-implantation, were analysed by Mann–Whitney U test since these outcomes were not paired and non-normally distributed. Effect sizes were calculated and presented according to Cohen’s D (d), where 0.2, 0.5, and 0.8, represent small, medium, and large effect sizes, respectively (Cohen Citation1988). Lastly, spearman rank order correlations (Rs) were used to examine for correlations between employment, quality of life, and hearing disability outcome measures.
Ethical considerations
The study was approved by Ethical Review Boards of participating centres in Colombia (Clínica Rivas, CEL 5277) and Poland (Uniwersytetu Medycznego w Łodzi, RNN/117/12/KE). The study was performed in adherence to ethical principles that have their origin in the Declaration of Helsinki and Good Clinical Practice ISO 14155:2020. All participants received verbal and written information regarding the study before providing written informed consent prior to participation.
Results
Demographics
Forty-three patients completed the HUI-3 pre-implantation and 43 of these individuals completed the questionnaire at 12-month follow-up, post-implantation. Regarding SSQ, all 43 patients completed the SSQ pre-implantation and at 12-month follow-up point. Thirty-seven subjects were resident in Colombia and the remaining 6 were residing in Poland. The mean age of subjects was 39.5 ± 14.8 (range: 18.1–64.4) and 26 were male and 17 were female. Regarding job satisfaction, 30 of the 43 patients with HUI-3 and SSQ data completed the patient questionnaire pre-implantation and at 12-month follow-up, post-implantation.
Health utilities index mark 3
HUI-3 results pre-implantation and at 12-month follow-up post-implantation are presented in . Mean attribute scores for all attributes other than emotion and cognition improved between baseline and follow-up. Mean utility score also improved from 0.611 to 0.697 between baseline and follow-up (). Statistically significant and clinically relevant mean improvements in hearing attribute (p = 0.003) and speech attribute (p = 0.003) between baseline and 12-month follow-up were captured by HUI-3 (). A statistically significant (p = 0.042), clinically relevant mean improvement in global score of 0.086 was reported between baseline and 12-month follow-up and the effect size was small (d = 0.269).
Figure 1. Distribution of HUI-3 comprehensive utility scores pre-implantation and at 12-month follow-up. Improvement in score between pre-implantation and follow-up was both clinically relevant and statistically significant (p ≤ 0.05).
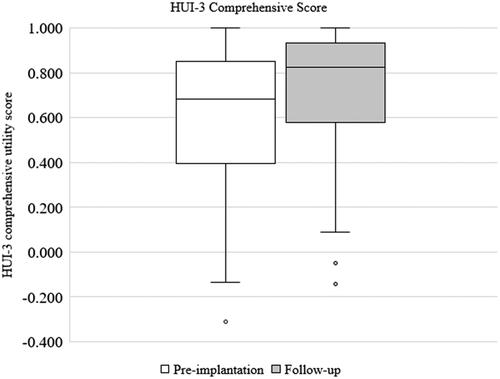
Table 1. Mean HUI-3 single attribute and utility scores pre-implantation (n = 43) and at 12-month follow-up (n = 43).
The speech, spatial and qualities of hearing scale
SSQ results between pre-implantation (n = 43) and 12-month follow-up (n = 43) are presented. Mean speech domain scores improved by 2.26 between baseline and 12-month follow up (). The improvement was both clinically relevant and statistically significant (p ≤ 0.001) and the effect size was large (d = 0.860). Mean spatial domain scores improved by 2.36 between baseline and 12-month follow up (). This change was both clinically relevant and statistically significant (p ≤ 0.001) and the effect size was large (d = 0.910). Mean qualities of hearing domain scores improved by 1.61 between baseline and 12-month follow up (). This change was clinically relevant and statistically significant (p ≤ 0.001), and the effect size was large (d = 0.810). Mean global SSQ score improved by 2.06 between baseline and 12-month follow up ( and ). This change was clinically relevant and statistically significant, and the effect size was large (d = 0.890).
Figure 2. Distribution of SSQ global scores pre-implantation and at 12-month follow-up. The improvement in score between pre-implantation and follow-up was both clinically relevant and statistically significant (p ≤ 0.001).
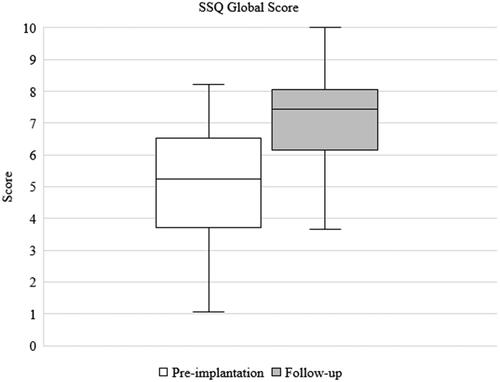
Table 2. Mean Speech Spatial and Qualities of Hearing Scale domain scores at baseline and follow-up (n = 43).
Employment and job satisfaction
Thirty individuals completed the patient questionnaire at baseline and follow-up. At baseline, patients scored their mean impact of their baseline hearing situation on their work at 2.48 (1.06), indicating that on average, their hearing impairment impacted their ability to work sometimes/most of the time (). At follow-up, patients scored their mean impact of hearing on their work at 1.40 (0.72), indicating that on average, their hearing impairment negatively impacted their ability to work not at all/sometimes. The difference in mean score of 1.08 between baseline and follow-up was statistically significant (p ≤ 0.001) and the effect size was very large (d = 3.47). Patients were also asked whether their hearing ability through their hearing device impacted their ability to perform their job satisfactorily, to which 22/30 patients reported that their hearing device allowed them to perform their employment ‘much better’ at follow-up (). Only a single patient reported a deterioration in performance at work post-implantation.
Table 3. Summary of patient responses to employment questionnaire from HUI-3 and SSQ cohort who were employed at baseline and follow-up.
Correlations between employment, health-related quality of life, and hearing disability
Spearman’s rank-order correlation was run to determine the relationship between job satisfaction and SSQ and HUI-3 scores. The analysis uncovered a moderate, positive correlation between SSQ Qualities scores and job satisfaction scores, which was statistically significant (Rs = .500, p = 0.008). No other correlations were statistically significant (p > 0.05), but weak, positive correlations between job satisfaction and SSQ speech scores (Rs = .243, p = 0.222), SSQ global scores (Rs = .320, p = 0.104), HUI-3 hearing attribute scores (Rs = .257, p = 0.196), and HUI-3 utility scores (Rs = .244, p = 0.221) were also found.
Discussion
The aim of the study was to examine job satisfaction, hearing difficulties and HRQoL in a group of working aged BCHD users pre-implantation and at 12-months post-implantation. HUI-3 data showed statistically significant and clinically important improvements in comprehensive health state and hearing and speech attributes post-implantation of the BCHD. This was supported with the findings of the SSQ questionnaire, where statistically significant and clinically important improvements in all domains were observed between pre- and post-implantation. Moreover, the results also revealed that job amenability improved after BCHD implantation. The findings of the current study are interesting since data demonstrates that, in addition to improved hearing and HRQoL, BCHD implantation can also have a positive impact on job satisfaction for users of working age.
Regarding HRQoL, statistically significant or clinically important changes were not captured via the vision, ambulation, dexterity, emotion, cognition, and pain attribute scores. While the lack of significance might be expected, it should also be noted that these scores were already high at the pre-operative phase (>0.9), indicating good HRQoL. In a study by Grimby and Ringdahl (Citation2000), 35 full-time employees (22–64 years old) using HAs were compared to another group of employees with HI working either part-time or retired. The aim of the study was to measure HRQoL, personal harmony, work-induced problems and to identify typical personal traits in both groups. Interestingly, the results revealed that full-time employees generally reported better HRQoL compared to those who were working part-time or retired, and on a level similar to their normally-hearing peers. This shows that having a job can be rewarding for individuals with HI and might contribute to an improved HRQoL similar to that of normally-hearing controls.
Furthermore, in a previous study (Hua et al. Citation2013), we compared HRQoL between employees with mild-moderate HI using conventional hearing aids (n = 20), normally-hearing controls (n = 20) and a matched population (n = 597) using the Short Form-36 (SF-36) questionnaire. The SF-36, similar to the HUI-3, measures physical and mental health status domains such as: physical and social functioning, bodily pain, general and mental health, vitality, physical and emotional limitations. Previous results, after removing outliers scoring two SDs outside the mean, showed that no significant differences were observed in any SF-36 subscales. Hence, previous and current results corroborate that working aged adults with HI have a relatively good HRQoL when excluding health dimensions related to hearing specifically. The current findings are in alignment with the findings of the SSQ, which demonstrated statistically significant improvement in all three hearing domains, and the effect size was generally large for each outcome pre- versus post-implantation with the BCHD. The results are in agreement with other studies examining the effect of bone conduction hearing therapy (Briggs et al. Citation2022; den Besten et al. Citation2019; Hougaard et al. Citation2017). When controlling for correlations between outcome measures, no significant correlations were observed, except for job satisfaction and the Qualities sub-score of SSQ. One could speculate that a larger study sample might have revealed different results as weak positive, but not statistically significant, correlations were observed between the employed measurements. Thus, more research is needed to unravel the complex interplay between hearing, HRQoL and employment status for workers with HI in the labour market.
In a recent review on HI and working life by Granberg & Gustafsson (Granberg and Gustafsson Citation2021), the authors highlighted the need of intersectionality in the literature and pointed out the effects of cochlear implantation on working life. The authors observed that cochlear implantation had a positive (self-rated) impact on job satisfaction, employment status and opportunities, professional skills and how much the individuals were able to work. Cochlear implantation could also generate increased motivation to go to work, decreased feelings of discrimination and increased feelings of being more competent to perform work. In comparison, similar findings for bone conduction hearing therapy, both percutaneous and transcutaneous, cannot be highlighted in the literature due to the lack of research, even though this therapy encompasses treatment of CHL, MHL, and SSD. Alternatively, some BCHD candidates may be treated with middle ear reconstructive surgery. However, a recent systematic review has also demonstrated that hearing rehabilitation through middle ear reconstructive surgery is unsuccessful in 29.3% of patients and results in post-operative complications in 14% of patients (Lewis et al. Citation2021). This indicates that bone conduction hearing therapy can be an alternative and effective treatment, and that more data comparing hearing devices with reconstructive surgeries is needed. Thus, the current finding showing that BCHD implantation can significantly improve job satisfaction is of interest. Moreover, when calculating the effect size of BCHD implantation on job satisfaction, the effect is considered huge (d = 3.47 (Sawilowsky Citation2009);). While the current study design cannot explain why the effect was so large regarding this particular outcome, the majority (22/30) of BCHD recipients reported that their hearing ability through their hearing device enabled them to perform their work ‘much better’. Comparing effect sizes between groups with different treatments (e.g., middle ear surgery, conventional hearing aids, BCHD, cochlear implants, etc.) on job satisfaction/work performance would be desirable in future research. This type of information could be used to guide public health initiatives to promote a more sustainable working life for individuals with HI.
In the present study, there are strengths and limitations that should be discussed. First, concerns have previously been raised regarding generic HRQoL measures since these may lack the necessary sensitivity to identify the consequences of HI and clinical changes (Bess Citation2000). The HUI-3 was employed in the current study as it is a validated and frequently used instrument that is sensitive to changes in hearing status. Moreover, the hearing and speech specific domains in HUI-3 did capture differences in the current study. The hearing specific finding was further complemented by SSQ data, which captured differences in all three hearing domains. Second, the current study only examined changes in job satisfaction, HRQoL and subjective hearing in a limited group of BCHD users who already are relatively healthy and actively working. The current study did not control for each respondents’ daily work environment (e.g., occupational noise exposure), additional diseases and disabilities (i.e., comorbidities) which could have impacted the interpretation of the HRQoL results. Also, out of the 43 respondents, only 30 filled in the questionnaire regarding job satisfaction and work performance. Thus, the current results should be interpreted with caution and can only considered representative of healthy working aged BCHD users. On the other hand, our findings are consistent with those reported by Granberg and Gustafsson (Granberg and Gustafsson Citation2021), where cochlear implantation had a positive effect on working life, resulting in improved communication and job satisfaction for individuals with HI. Third, patients only recorded data over a follow-up period of 12-months. Hence, it is not possible to predict whether the post-implantation effect is stable over the longer-term. Another aspect that may have influenced the results is that there may be important cultural differences/similarities across the two included countries (i.e., Colombia and Poland) that might have influenced the current outcomes. Future studies examining the effects of hearing device implantation from a longer-term perspective and/or cultural aspects would therefore be desirable.
Limited availability of comparable data on utility gains with BCHD prevents comparison between interventions and accurate cost effectiveness calculations. This is important since surgical methods of hearing rehabilitation can be costly and may not reduce the health care burden over the long-term (Lewis et al. Citation2022). However, these studies are typically limited to reporting direct costs only and future studies must also consider indirect costs. Future studies should strive to capture both hearing related and general HRQoL data in individuals with HI. Ideally, these data should be collected in conjunction with detailed pre- and post-intervention audiometric testing as specified by the American Academy of Otolaryngology–Head and Neck Surgery (Gurgel et al. Citation2012). High-quality HRQoL data are important to inform cost-effectiveness models, permitting comparisons between interventions to optimise care. The resultant cost-effectiveness data could support policy makers in managing healthcare spending and facilitate the creation of more standardised, evidence-based care.
Taken together, the results from the present study showed that hearing and speech domains in HUI-3 and speech, spatial and qualities domains in SSQ are significantly improved post-implantation in working aged BCHD users. A significant improvement was also observed for several aspects of employment in this group after BCHD treatment. Literature on working life and BCHD users is generally sparse, and there is a need for intersectionality on this topic (Granberg and Gustafsson Citation2021). Hence, this was the first attempt at describing this population post-implantation. Future research should examine the similarities/differences between employees with conventional hearing aids, BCHD and/or cochlear implants. Additional research focussing on topics such as the need for recovery after work, perceived effort/problems in different work situations/noises and strategies to manage working life in BCHD users would also be of interest.
Conclusion
Hearing rehabilitation with BCHD reduces hearing disability and improves HRQoL for recipients, resulting in significant improvements across all domains assessed with the SSQ and a clinically important utility gain of 0.086 between pre-implantation and 12-month follow-up as measured with the HUI-3. Additionally, 73.3% of patients in this study performed much better at work post-implantation, supporting the conclusion that implantation with BCHD reduces the negative burden hearing loss places on one’s ability to carry out their employment, resulting in significant improvements in working ability and job satisfaction.
| Abbreviations | ||
| BCHD | = | bone conduction hearing device |
| CHL | = | conductive hearing loss |
| HA | = | hearing aid |
| HI | = | hearing impairment |
| HRQoL | = | Health-related quality of life |
| MHL | = | mixed hearing loss |
| SSD | = | single-sided deafness |
Acknowledgements
The authors would like to thank Herbert Mauch, Jasmin Kaur, Colin Irwin, and Josie Wyss for design, implementation, and management of the IROS register from which study data were derived. The authors would also like to thank participating patients and clinicians; Dr Adriana Rivas, Dr Rafael Jaramillo, Dr Margarita Schwarz Langer, Dr Jose Eduardo Guzman, Dr Julian Alejandro Ramirez Osorio, Dr Santiago Hernandez, Dr Jorge Almario, Dr Jose Gabriel Lora, Dr Adelaida Plazas, Dr Henry Leonardo Martinez, Dr Jose Omar Gutierrez, Dr Mario Gonzalez, Dr Jose Alberto Prieto, Dr Jaime Arturo Torres, Prof. Wioletta Pietruszewska, Dr Piotr Winiarski, Dr Jozef Mierzwinski, and Dr Tomasz Pychynski.
Disclosure statement
H. H. and A. T. L. are current employees of Cochlear Limited, a manufacturer and supplier of bone conduction hearing devices.
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Bess, F. H. 2000. “The Role of Generic Health-Related Quality of Life Measures in Establishing Audiological Rehabilitation Outcomes.” Ear and Hearing 21 (4 Suppl):74s–79s. doi:10.1097/00003446-200008001-00009
- Briggs, R., C. S. Birman, N. Baulderstone, A. T. Lewis, I. H. Y. Ng, A. Östblom, A. Rousset, et al. 2022. “Clinical Performance, Safety, and Patient-Reported Outcomes of an Active Osseointegrated Steady-State Implant System.” Otology & Neurotology 43 (7): 827–834. doi:10.1097/MAO.0000000000003590.
- Chadha, S., K. Kamenov, and A. Cieza. 2021. “The World Report on Hearing, 2021.” Bulletin of the World Health Organization 99 (4): 242–242A. doi:10.2471/BLT.21.285643.
- Cohen, J. 1988. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: L. Erlbaum Associates. xxi, 567.
- Danermark, B., and L. C. Gellerstedt. 2004. “Psychosocial Work Environment, Hearing Impairment and Health.” International Journal of Audiology 43 (7): 383–389. doi:10.1080/14992020400050049.
- Danermark, B., and L. C. Gellerstedt. 2004. “Social Justice: Redistribution and Recogntion – A Non-Reductionist Perspective on Disability.” Disability & Society 19 (4): 339–353. doi:10.1080/09687590410001689458.
- den Besten, C. A., P. Monksfield, A. Bosman, P. H. Skarzynski, K. Green, C. Runge, S. Wigren, et al. 2019. “Audiological and Clinical Outcomes of a Transcutaneous Bone Conduction Hearing Implant: Six-Month Results from a Multicentre Study.” Clinical Otolaryngology 44 (2): 144–157. doi:10.1111/coa.13248.
- Ellsperman, S. E., E. M. Nairn, and E. Z. Stucken. 2021. “Review of Bone Conduction Hearing Devices.” Audiology Research 11 (2): 207–219. doi:10.3390/audiolres11020019.
- Gatehouse, S., and W. Noble. 2004. “The Speech, Spatial and Qualities of Hearing Scale (SSQ).” International Journal of Audiology 43 (2): 85–99. doi:10.1080/14992020400050014.
- Gellerstedt, L., and B. Danermark. 2004. “Hearing Impairment, Working Life Conditions, and Gender.” Scandinavian Journal of Disability Research 6 (3): 225–245. doi:10.1080/15017410409512654.
- Granberg, S., and J. Gustafsson. 2021. “Key Findings about Hearing Loss in the Working-Life: A Scoping Review from a Well-Being Perspective.” International Journal of Audiology 60 (sup2):60–70. doi:10.1080/14992027.2021.1881628.
- Grimby, A., and A. Ringdahl. 2000. “Does having a Job Improve the Quality of Life among Post-Lingually Deafened Swedish Adults with Severe-Profound Hearing Impairment?” British Journal of Audiology 34 (3): 187–195. doi:10.3109/03005364000000128.
- Grutters, J. P. C., M. A. Joore, F. van der Horst, H. Verschuure, W. A. Dreschler, and L. J. C. Anteunis. 2007. “Choosing Between Measures: Comparison of EQ-5D, HUI2 and HUI3 in Persons with Hearing Complaints.” Quality of Life Research 16 (8): 1439–1449. doi:10.1007/s11136-007-9237-x.
- Gurgel, R. K., R. K. Jackler, R. A. Dobie, and G. R. Popelka. 2012. “A New Standardized Format for Reporting Hearing Outcome in Clinical Trials.” Otolaryngology-Head and Neck Surgery 147 (5): 803–807. doi:10.1177/0194599812458401.
- Håkansson, B., S. Reinfeldt, A.-C. Persson, K.-J F. Jansson, C. Rigato, M. Hultcrantz, and M. Eeg-Olofsson. 2019. “The Bone Conduction Implant – A Review and 1-Year Follow-Up.” International Journal of Audiology 58 (12): 945–955. doi:10.1080/14992027.2019.1657243.
- Hampton, T., K. Milinis, E. Whitehall, and S. Sharma. 2022. “Association of Bone Conduction Devices for Single-Sided Sensorineural Deafness With Quality of Life: A Systematic Review and Meta-analysis.” JAMA Otolaryngology – Head & Neck Surgery 148 (1): 35–42. doi:10.1001/jamaoto.2021.2769.
- Horsman, J., W. Furlong, D. Feeny, and G. Torrance. 2003. “The Health Utilities Index (HUI): Concepts, Measurement Properties and Applications.” Health and Quality of Life Outcomes 1 (1): 54. doi:10.1186/1477-7525-1-54.
- Hougaard, D. D., S. K. Boldsen, A. M. Jensen, S. Hansen, and P. C. Thomassen. 2017. “A Multicenter Study on Objective and Subjective Benefits with a Ttranscutaneous Bone-Anchored Hearing Aid Device: First Nordic Results.” European Archives of Oto-Rhino-Laryngology 274 (8): 3011–3019. doi:10.1007/s00405-017-4614-8.
- Hua, H., A. Anderzén-Carlsson, S. Widén, and B. Lyxell. 2015. “Conceptions of Working Life among Employees with Mild-Moderate Aided Hearing Impairment: A Phenomenographic Study.” International Journal of Audiology 54 (11): 873–880. doi:10.3109/14992027.2015.1060640.
- Hua, H., J. Karlsson, S. Widén, C. Möller, and B. Lyxell. 2013. “Quality of Life, Effort and Disturbance Perceived in Noise: A Comparison between Employees with Aided Hearing Impairment and Normal Hearing.” International Journal of Audiology 52 (9): 642–649. doi:10.3109/14992027.2013.803611.
- Hua, H., T. Goossens, and A. T. Lewis. 2022. “Increased Maximum Power Output may Improve Speech Recognition with Bone Conduction Hearing Devices.” International Journal of Audiology 61 (8): 670–677. doi:10.1080/14992027.2021.1959953
- Kramer, S. E., T. S. Kapteyn, and T. Houtgast. 2006. “Occupational Performance: Comparing Normally-Hearing and Hearing-Impaired Employees using the Amsterdam Checklist for Hearing and Work.” International Journal of Audiology 45 (9): 503–512. doi:10.1080/14992020600754583.
- Lewis, A. T., D. Backous, B. Y. Choi, R. Jaramillo, K. Kong, T. Lenarz, J. Ray, A. Thakar, K. Järbrink, M. K. S. Hol. 2022. “Healthcare Consumption among Subjects with Otitis Media Undergoing Middle Ear Surgery-Analysis of Cost Drivers.” European Archives of Oto-Rhino-Laryngology doi:10.1007/s00405-022-07483-8.
- Lewis, A., B. Vanaelst, H. Hua, B. Yoon Choi, R. Jaramillo, K. Kong, J. Ray, et al. 2021. “Success Rates in Restoring Hearing Loss in Patients with Chronic Otitis Media: A Systematic Review.” Laryngoscope Investigative Otolaryngology 6 (3): 522–530. doi:10.1002/lio2.576.
- Ontario Health (Quality). 2020. “Implantable Devices for Single-Sided Deafness and Conductive or Mixed Hearing Loss: A Health Technology Assessment.” Ontario Health Technology Assessment Series 20 (1): 1–165.
- Pennini, P. T. M., and K. Almeida. 2021. “Speech, Spatial and Qualities of Hearing Scale in Assessing the Benefit in Hearing Aid Users.” CoDAS 33 (2): e20190196. doi:10.1590/2317-1782/20202019196.
- Ringdahl, A., and A. Grimby. 2000. “Severe-Profound Hearing Impairment and Health-Related Quality of Life among Post-Lingual Deafened Swedish Adults.” Scandinavian Audiology 29 (4): 266–275. doi:10.1080/010503900750022907.
- Sawilowsky, S. S. 2009. “New Effect Size Rules of Thumb.” Journal of Modern Applied Statistical Methods 8 (2): 597–599. doi:10.22237/jmasm/1257035100.
