Abstract
Objective
The proportions of older adults’ transitions through acknowledging their hearing loss to getting access to treatment are unknown. This was examined using data from a nationally representative cohort in England.
Design
Patient and healthcare factors associated with referrals were examined cross-sectionally, through primary to secondary care. Non-report predictors identified using multiple logistic regression models.
Study sample
8529 adults with hearing data in the English Longitudinal Study of Ageing Wave 7.
Results
Nearly 40% of those with acknowledged hearing loss did not tell a doctor or nurse (n = 857/2249). Women (OR 2.68, 95% CI 2.14–2.98), retirees (OR 1.30, 95% CI 1.17–1.44), those with foreign education (OR 2.74, 95% CI 2.47–3.04), lower education (OR 2.86, 95% CI 2.58–3.18), smokers (OR 4.39, 95% CI 3.95–4.87), and heavy drinkers (OR 1.67, 95% CI 1.58–1.85) were more likely to not report hearing loss. Of those who acknowledged and reported hearing difficulties, willingness to try hearing aid(s) was high (78.9%).
Conclusions
Unacknowledged, or acknowledged but not reported hearing loss by individuals, and non-referrals by primary healthcare professionals, are barriers to accessing hearing healthcare. Future research should report hearing aid use as the proportion of individuals who acknowledge their hearing loss, to avoid an overestimation of the non-use of hearing aids within study samples.
Introduction
Hearing loss is a significant public health issue, estimated to affect a large proportion of the population (McDaid, Park, and Chadha Citation2021). In England alone, hearing loss affects more than 40% of adults over 70 years of age, a percentage with marked regional variability between the northern and southern parts of the country (Tsimpida, Panagioti, and Kontopantelis Citation2022). Hearing loss in later life has a significant social and psychological impact on an individual’s life, posing a substantial risk to the functional abilities that enable healthy ageing (Young Citation2014; Tsimpida et al. Citation2021b).
Although there are associations between age and hearing loss, a recent study in England provided evidence that age is a less critical factor in the aetiology of hearing loss than previously believed (Tsimpida et al. Citation2020b). Reframing the discussion around hearing loss in later life to reflect that it is not an inevitable accompaniment of ageing, could encourage secondary preventative strategies around early identification of hearing problems. In addition, there is scientific evidence that the use of hearing aids to manage hearing loss improves the hearing-related and health-related quality of life for those with mild to moderate hearing loss (Ferguson et al. Citation2017), which is vital given the substantial burden of this long-term condition (Wilson et al. Citation2017).
Current evidence shows a wide variation in rates of hearing aid uptake that has been reported depending on the sample and the country assessed (Bisgaard and Ruf Citation2017; Bisgaard et al. Citation2022). Heterogeneity in the use of hearing aids may reflect differences between health systems and hearing aid provision between different countries, for example, availability and cost (Sawyer et al. Citation2020). However, hearing aid use is also low in countries where hearing aid provision for most people is covered by public health insurance, for example, in England, where the cost should not be a major barrier to hearing aid uptake, as hearing aids are provided in a universal healthcare setting and are free at the point of delivery (Barton et al. Citation2001). Today, hearing loss remains significantly underdiagnosed and untreated (Benova, Grundy, and Ploubidis Citation2015; Sawyer et al. Citation2019; Dillon et al. Citation2020). Currently, there is no national screening programme for early identification of hearing loss in adults through a routine free health check in primary care (Tsimpida et al. Citation2020a). The early identification of hearing loss and subsequent uptake of hearing aids is often delayed unnecessarily for many years (Hill et al. Citation2015).
Health system users in England may experience several barriers in their hearing pathway from primary to secondary care. Benova, Grundy, and Ploubidis (Citation2015), analysed data from Wave 2 of the English Longitudinal Study of Ageing (ELSA) (Zaninotto and Steptoe Citation2019), and broke down the hearing data questions in the ELSA into six distinct stages corresponding to the help-seeking process: self-diagnosis (Stage 1), the individual’s initiation of contact with a health provider in primary care (Stage 2), referral to an ear specialist (Stage 3), hearing aid recommendation (Stage 4), compliance with the recommendation to obtain a hearing aid (Stage 5) and adherence with the recommendation to use a hearing aid (Stage 6).
However, a previous study (Tsimpida et al. Citation2020a) revealed that participants may be misclassified as being in Stage 1, without being aware of having hearing loss. For example, an ELSA participant may report having great difficulty following a conversation if there is background noise (such as television, radio, or children playing), and consequently categorised as having self-reported difficulties; however, in a subsequent question, the participant may answer that their hearing is excellent, showing that they were not aware of having hearing loss when they completed the questionnaire.
To address the above discrepancy, a different approach was taken to identify those who are recorded as having hearing loss, based on the design of the questionnaire, and, in parallel, are aware of their hearing loss, as denoted by Tsimpida et al. (Tsimpida et al. Citation2020a). This issue had not been addressed in the study published by Benova, Grundy, and Ploubidis (Citation2015), as the validation of self-reported hearing data with pure-tone screening audiometry data was not possible in their study. Distinguishing between those who are and those who are not aware of their hearing loss is important when exploring the proportions of hearing aid uptake. Including those who are unaware of their hearing loss in calculations of hearing aid uptake, prevents accurate examination of the willingness to try hearing aids amongst those who are aware of their hearing loss. Participants without awareness of their hearing loss would have no reason to seek help for hearing difficulties. Additionally, both must be tackled by distinct strategies; in the case of low awareness, supporting early identification is required, whereas low uptake of hearing aids by individuals who are aware of their hearing loss, strategies to improve access to and uptake of hearing aids is needed.
Currently, there is a lack of evidence around awareness and reporting of hearing loss or the barriers they may encounter in the help-seeking process. The lack of studies that explore the proportion of people seeking help for hearing-related problems and the subsequent proportions that are referred, diagnosed and treated or remained undiagnosed has been acknowledged by the UK National Screening Committee (NSC). In addition, the UK NSC has recognised the need for more high-quality evidence regarding the proportion of UK adults with hearing loss accessing treatment amongst the detected population in the UK (Solutions for Public Health Citation2021). Identifying potential individual and system-level barriers to treatment for hearing loss is essential to inform interventions and health policy strategies for hearing screening in England.
Therefore, this study aims: a) to investigate the characteristics of the patient pathway for adults with acknowledged hearing loss in England, and b) to examine patient and system-level factors associated with non-referrals from primary care to ear specialists for audiological examinations, based on a nationally representative cohort of older adults.
Materials and methods
Study population
We used data from the ELSA, a large population-based prospective cohort study that provides a nationally representative sample of adults in England aged 50 and older (Steptoe et al. Citation2013).
The full analytic cohort was composed of individuals who participated in the seventh wave of the ELSA (n = 9666), which collected information between June 2014 and May 2015. For our study, we analysed a sample of n = 8529 adults that had a hearing assessment using the HearCheck Screener, which tests for audibility of pure tone stimuli at 1.0 kHz and 3.0 kHz (Siemens Audiologische Technik GmbH Citation2007), and did not have an ear infection or a cochlear implant (Zaninotto and Steptoe Citation2019). All participants gave written, informed consent at the recruitment wave to participate in the ELSA and in each subsequent wave. Ethical approval was granted for the ELSA by the National Research and Ethics Committee (Natcen Social Research Citation2018; Zaninotto and Steptoe Citation2019).
Outcomes
Self-reported hearing loss
Self-reported hearing loss is defined in the ELSA as (a) having declared fair or poor hearing on a five-point Likert scale (excellent, very good, good, fair or poor), or (b) whether they had moderate or great difficulty in following a conversation if there is background noise (such as television, radio, or children playing) (Zaninotto and Steptoe Citation2019).
The concordance of the ELSA self-reported hearing loss with pure-tone screening audiometry has been examined in a previous study (Tsimpida et al. Citation2020a). The sensitivity of the self-reported measure in the ELSA Wave 7 was 69.8% (95% CI 67.9–71.7), which refers to the ability of the self-reported measure to correctly identify seven in ten people with psychoacoustically measured hearing loss greater than 35 dB HL at 3 kHz in the better-hearing ear (true-positive results). This is the level of hearing loss at which intervention has shown to be beneficial (Davis et al. Citation2007). The specificity of the self-reported hearing loss was 69.3% (95% CI 68.1–70.4).
We further categorised those 2249 with acknowledged self-reported hearing loss into those with moderate self-reported hearing loss (if they reported that their hearing was fair or had moderate difficulty following a conversation with background noise) and those with moderately severe or severe self-reported hearing loss (if they reported that their hearing was poor or had great difficulty following a conversation with background noise). That categorisation was based on the concordance of the ELSA self-reported hearing loss with pure-tone screening audiometry (Tsimpida et al. Citation2020b).
Current hearing aid use
As part of the ELSA data collection, participants who self-reported hearing loss were asked whether they ever wore a hearing aid, with the following possible answers: (a) Yes, most of the time, (b) Yes, some of the time, and (c) No. In this study, we defined hearing aid use in this study as responses (a) or (b) and hearing aid non-use as responses (c) (Zaninotto and Steptoe Citation2019).
Covariates
We used indicators of socioeconomic position (SEP) as covariates within our analyses. These were the highest educational attainment [no qualifications; foreign/other; O levels (refers to ordinary level, the final certification of secondary education and is usually taken between 14 and 16 years of age; A levels (stands for advanced level, the advanced level qualification for students aged 16 years and above; degree/higher education], tertiles of the self-reported occupation according to the National Statistics socioeconomic classification (NS-SEC) (routine and manual occupations; intermediate; managerial and professional) and the quintiles of the net household income and the total non-pension wealth (first quintile lowest; fifth quintile highest).
We also examined the demographic covariates of respondents (age and sex) as well as several lifestyle factors as covariates (physical activity and tobacco and alcohol consumption), because previous evidence has shown that these are key risk factors for hearing loss in older adults (Tsimpida et al. Citation2018; Tsimpida et al. Citation2021a). Levels of physical activity were described by a variable that examined the frequency at which the respondents do moderate sports or activities, with the possible answers being: (1) more than once a week, (2) once a week, (3) one to three times a month and (4) hardly ever or never. Tobacco consumption through any type of nicotine product was in three categories: current smokers, former smokers, and those that have never smoked. We constructed a continuous variable to represent the sum of units of alcohol that the participants consumed in the last seven days according to the Chief Medical Officer’s Drinking Guidelines (Department of Health Citation2016), which count each measure of spirits as one unit, and each glass of wine or pint of beer as 2 units. The constructed variable of units of alcohol during the last 7 d was further dichotomised into those that did or did not consume more than 14 units of alcohol during the previous 7 d (Department of Health Citation2016).
We dichotomised marital status into; currently married (married, first and only marriage; in a registered civil partnership; and remarried, in a second or later marriage) and not married (single, that is never married and never registered in a marriage; separated, but still legally married; divorced; and widowed). Retirement status was also dichotomised as currently being or not being retired.
Statistical analysis
Descriptive statistical measures are provided for hearing loss, hearing in noise, and hearing aid recommendations within the ELSA Wave 7 (n = 8,529). Participants’ self-reported hearing loss (moderate, moderately severe or severe) were reported as absolute (n) and relative (%) frequencies.
We fitted multiple logistic regression models to identify predictors of non-reporting of acknowledged hearing loss within the sample of (a) those who self-reported hearing loss (n = 2249), (b) those who self-reported moderate hearing loss (n = 1,565), and (c) those who self-reported moderately severe or severe hearing loss (n = 684). Age was categorised into three groups (50–64; 65–74; and 75–89) to allow for a comparison with Tsimpida et al. (Tsimpida et al. Citation2020a). There were a number of missing data for covariates (shown in Table 1 in the Additional File). We performed analyses which showed that there was no pattern in the missing data regarding age, sex, education, occupation, income and wealth. Due to the low proportion of missingness, we excluded records with missing data from our analyses, concluding that this would be unlikely to affect the validity of our findings (Little and Rubin Citation2019; Mittag Citation2013).
Table 1. Summary of multiple logistic regression for variables predicting the non-report of an acknowledged hearing difficulty to a doctor or nurse in primary care in the English Longitudinal Study of Ageing (ELSA) Wave 7.
For all models, odds ratios and 95% confidence intervals are presented. We used the Hosmer -Lemeshow test as a post-estimation tool, which demonstrates the goodness-of-fit of logistic regression models. The two-tailed significance level was set at ≤0.05. All data were analysed using Stata/SE 16.1.
Results
Self-reported hearing loss
To obtain a clean sample of those with self-reported and actively recognised hearing loss, we used the categories from a previously published study (Tsimpida et al. Citation2020a), to exclude those who had responded that they had difficulty in following a conversation if there is background noise but reported at the same time that their hearing is very good, good, very good or excellent. That study revealed that of the 3425 participants recorded as having self-reported hearing loss (Stage 1 in Benova’s stages for help-seeking) (Benova, Grundy, and Ploubidis Citation2015), 65.7% (n = 2249) acknowledged hearing loss (Tsimpida et al. Citation2020a).
shows the characteristics of the sample for hearing loss, hearing in noise, and hearing aid recommendation in the ELSA Wave 7 (n = 8529: males = 3728 and females = 4801). The 38.2% of those with acknowledged hearing loss (n = 857/2249) did not tell a doctor or nurse in primary care about their hearing loss, missing the opportunity to be referred to an ear specialist to assess their hearing. Two participants of the 2249 responded “I do not know” and were excluded from the analysis.
Figure 1. The questions on hearing loss, hearing in noise, and hearing aid recommendation in the English Longitudinal Study of Ageing (ELSA) Wave 7 (n = 8529). aThe sum of those who rated their hearing as fair or poor on a 5-point Likert scale (with 1 indicating excellent; 2, very good; 3, good; 4, fair; and 5, poor) or responded that they have moderate or great difficulty in following a conversation if there is background noise (such as television, radio, or children playing). bTwo participants responded “I do not know” and were excluded from the analysis.
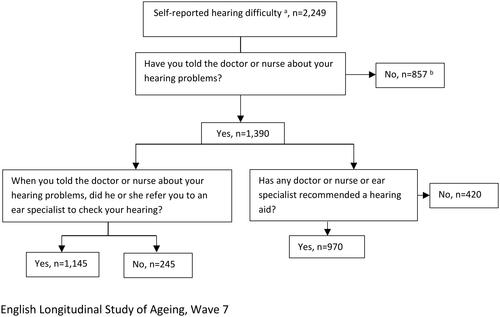
Out of the 1390 participants who told a doctor or nurse about their hearing problems, 82.4% were referred to secondary care for an audiological examination (n = 1145/1390). In addition, nearly a third of those individuals (30.2%, n = 420/1390) who told a doctor or nurse about their hearing loss, were not recommended a hearing aid by healthcare providers.
shows a summary of multiple logistic regression for variables predicting the non-report to a doctor or nurse in primary care of acknowledged hearing difficulty in the ELSA Wave 7. We also present the corrected odds ratios for sensitivity and specificity (Antunes Citation2019). The corrected odds ratio in the multiple logistic regression models showed that demographic, socioeconomic and lifestyle factors were associated with the non-reporting of acknowledged hearing loss to a doctor or nurse in primary care. Significant predictors for non-reporting, by those who had moderate or worse hearing loss (Model I), were females (OR 2.68, 95% CI 2.14–2.98), retirees (OR 1.30, 95% CI 1.17–1.44), having a foreign education (OR 2.74, 95% CI 2.47–3.04), having a lower education, defined as O level/CSE grade (OR 2.86, 95% CI 2.58–3.18), and having a current smoking habit (OR 4.39, 95% CI 3.95–4.87). In addition, those consuming alcohol above the low-risk-level guidelines, defined as 14 units of alcohol per week (Department of Health Citation2016), had a greater likelihood of non-reporting of a recognised hearing problem than those who consumed alcohol below the low-risk level guidelines (OR 1.67, 95% CI 1.58–1.85).
Current hearing aid use
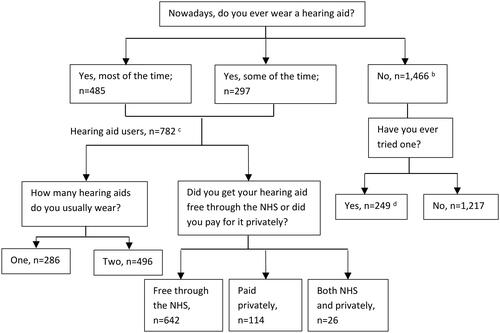
shows the responses to hearing aid uptake and use questions in the ELSA Wave 7 by those with self-reported hearing loss. Seven hundred and eighty-two participants reported that they currently wear a hearing aid [most of the time (62%, n = 485/782) or some of the time nowadays (38%, n = 297/782)]. The majority of hearing aid users got their hearing aids for free through the NHS (82%, n = 642/782).
Figure 2. The questions on hearing aid uptake and use in the English Longitudinal Study of Ageing (ELSA) Wave 7 among those with self-reported hearing lossa (n = 2249). aThe sum of those who rated their hearing as fair or poor on a 5-point Likert scale (with 1 indicating excellent; 2, very good; 3, good; 4, fair; and 5, poor) or responded that they have moderate or great difficulty in following a conversation if there is background noise (such as television, radio, or children playing). bOne participant responded “I do not know” and was excluded from the analysis.
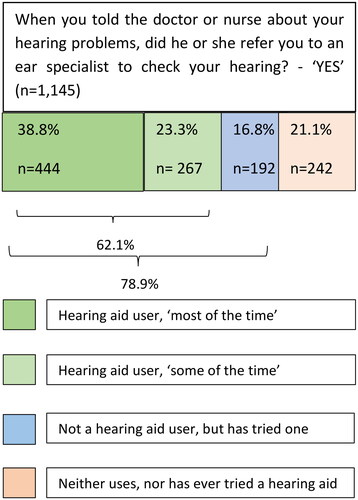
shows additional analyses on those who acknowledged their hearing loss, told a doctor or nurse in primary care about their hearing loss and were referred to an ear specialist to check their hearing. Out of a total of n = 1145 participants that had been referred for an ear examination, 62% (n = 444 + 267 = 711) (as shown in ), reported they used hearing aids, and adhered to treatment most of the time (n = 444), or some of the time, (n = 267). In addition, 16.8% (n = 192/1145) of those who had been referred for an ear examination had tried hearing aids, although they do not currently wear one. Therefore, the majority (78.9%) of individuals who acknowledged their hearing loss, told a doctor or nurse and were referred for an ear examination used or tried a hearing aid.
Figure 3. Behaviour on hearing aids use among 1145 participants who acknowledged hearing loss, disclosed it to a doctor or nurse in primary care, and were referred to an ear specialist to check their hearing (data from the English Longitudinal Study of Ageing (ELSA) Wave 7, a nationally representative cohort of 8529 older adults aged 50 years old and above in England).
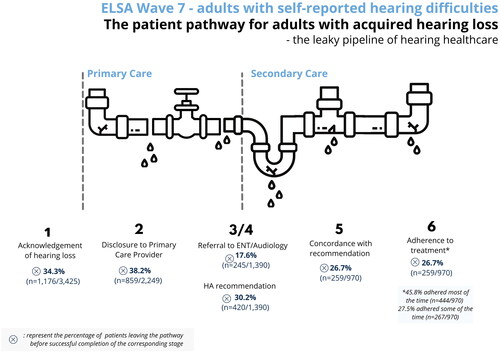
summarises the above findings, which are presented as 6 Stages in the hearing pathway and depicts the percentage of those who leave the pathway before successfully completing each stage.
Figure 4. Proportions of participants in the English Longitudinal Study of Ageing (ELSA) Wave 7 with self-reported hearing lossa who leave the hearing pathway before the successful completion of the corresponding stage. aThe sum of those who rated their hearing as fair or poor on a 5-point Likert scale (with 1 indicating excellent; 2, very good; 3, good; 4, fair; and 5, poor) or responded that they have moderate or great difficulty in following a conversation if there is background noise (such as television, radio, or children playing).
Discussion
Summary of the main findings
This study examined individual and healthcare system factors associated with primary to secondary care referrals in a nationally representative study of older adults in England. We found that 38.1% of those with an acknowledged hearing loss did not tell a doctor or nurse about their hearing problems, missing the opportunity to be referred to an ear specialist to assess their hearing. Several demographic, socioeconomic and lifestyle factors were associated with the non-reporting of hearing loss to a doctor or nurse in primary care. Almost one out of five patients who told a primary care healthcare provider about their hearing loss did not receive an onward referral to secondary care for a further hearing assessment, as per recommendation No. 12 in NICE Guideline NG98 (NICE Citation2018). A large proportion (78.9%) of those who acknowledged, and reported hearing loss and being referred to secondary care, were willing to try and use hearing aids.
Comparison with previous literature
Our study adds to previous studies that found that GPs refer only a small percentage of those mentioning any hearing loss in primary care to secondary care (Yueh et al. Citation2003; Davis et al. Citation2007; Wallhagen and Pettengill Citation2008; Schneider et al. Citation2010). However, we found that nearly one in five (17.5%) who told a doctor or nurse about their hearing problems were not referred to secondary care; this is a much lower percentage than the 50% reported in a previous study by Davis et al. (Citation2007) who examined patients from six GP practices in Nottingham, (not a nationally representative sample). A more recent study by Sawyer et al. (Citation2020) also explored data from the ELSA, but did not find that onward referral from GPs were a barrier at all; they found that only 4.5% of those reporting hearing loss reported not being referred for a hearing assessment.
To our knowledge, our study is the first to examine socioeconomic, and lifestyle predictors of unreported but acknowledged hearing loss in primary care, based on a representative sample of older adults in England. Sawyer et al. (Citation2020) examined the biopsychosocial classification of seeking hearing health in the ELSA and found that socioeconomic position was not associated with any stage in the help-seeking process. However, their study examined different stages in the hearing pathway to the present research and followed an alternative methodology to the published ELSA Wave 7 protocol (publicly available at https://www.elsa-project.ac.uk/study-documentation).
Strengths and limitations
Our study presents the first evaluation from a representative sample of older adults in England of help-seeking for hearing problems, hearing aid recommendation, uptake and use by older adults who acknowledge and report difficulties in their hearing. These findings provide novel insights, as previously published studies in England do not differentiate between those with acknowledged and unacknowledged hearing loss to attribute proportion-based estimates of hearing aid uptake and use (Benova, Grundy, and Ploubidis Citation2015; Scholes et al. Citation2018). This may contribute to the wide variation in rates of hearing aid uptake that has been reported (Bisgaard and Ruf Citation2017; Bisgaard et al. Citation2022).
In our study, it is clear that a large proportion of people would be unlikely to access hearing healthcare because they had unacknowledged hearing loss. We found that, for those individuals who had the opportunity to access hearing healthcare, the percentage of individuals reporting the use of hearing aids was encouragingly large. If this population were considered together with those who had unacknowledged hearing loss, the proportion of hearing aid use would appear much smaller. To obtain a more accurate proportion of hearing aid uptake amongst adults who acknowledge and report hearing loss, participants in studies should be asked “if they have ever told a doctor or nurse about their hearing loss”. For example, Scholes et al. (Citation2018) reports that among those with hearing loss, 30% of men and 27% of women were currently using hearing aids. However, it is unclear what proportion of participants were unaware of their hearing loss prior to participation in the study, and therefore highly unlikely to have sought help for hearing loss. Considering the proportions of adults with acknowledged and unacknowledged hearing loss separately is likely to be much more useful for future work in this area; the proportion of those with acknowledged hearing loss may be more helpful in understanding barriers and facilitators to accessing hearing healthcare. On the other hand, considering the proportions of those with unacknowledged hearing loss is also important for health policy changes towards the early identification of hearing loss cases, and the development of public health interventions for increasing awareness around hearing health. As suggested by the UK National Screening Committee (Solutions for Public Health Citation2021), the accurate evidence on the proportion of uptake of treatment in populations might provide a better estimate for the acceptability of hearing aids and our study provides a more robust way for this proportion to be calculated.
However, our study has several limitations. First, the cross-sectional analyses did not allow for causal or temporal relationships among the factors associated with the non-reporting of hearing loss to a health professional and the potential effect of existing comorbid health conditions that may downgrade hearing loss as a health priority.
In addition, it was not possible to analyse hearing aid uptake among those who did not report hearing difficulty (but could have experienced hearing loss), as they did not have the opportunity to respond to these questions. As shown in our study, a number of older adults may experience hearing loss without reporting it to a doctor or nurse in primary care. The recently launched technical guidelines by the World Health Organisation recommend screening in primary care for older adults who do not report hearing loss so as to address such cases of unacknowledged hearing loss (WHO Citation2021).
The assessment of hearing acuity via a hearing screening device in the ELSA Wave 7 was performed only on those who did not have an ear infection or a cochlear implant. Of the 9666 participants in the ELSA Wave 7, n = 208 had an ear infection, and n = 50 had a cochlear implant, and we were not able to obtain any data on them. In addition, the validation of self-reported hearing loss was constrained by the HearCheck Screener’s technical characteristics, as it generates high-frequency sounds at 3 kHz at 75 dB HL, 55 dB HL, and 35 dB HL. Therefore, no information for mild hearing loss has been obtained, and further evidence in future studies regarding the transitions of people with mild hearing loss is needed.
We need to take into consideration that the data in a survey may not directly reflect individual choices and decisions, as communication partners can influence decision-making surrounding hearing loss treatment both positively and negatively, for instance, regarding the decision whether or not to obtain a hearing aid (Schulz et al. Citation2016). Furthermore, the steps in the help-seeking behaviour process were informed by the available variables in the ELSA dataset and not by the author’s interpretations or other theoretical models that have previously discussed the processes that individuals have to navigate to acknowledge their hearing loss (Barnett et al. Citation2017; Laplante-Lévesque et al. Citation2015).
The majority of the participants in our study (82.1%, n = 642/782) reported that they got their hearing aids for free through the NHS. Participants who paid privately amounted to 14.6% (n = 114/782), while 3.3% (n = 26/782) got their hearing aids both through the NHS and privately (see ). However, the current data did now allow us to explore additional barriers that may be faced when paying privately to get a hearing aid, or the reasons to choose the private option since a hearing aid can be obtained through the NHS for free.
We did not analyse the characteristics of those who reported hearing difficulty but were not referred to secondary care by a primary care professional. Identifying potential reasons for health professionals’ behaviour is an area for future investigation through qualitative and geographical research, as this may occur due to other factors, such as limited healthcare resources in some regions of England where the prevalence of hearing loss is high (Tsimpida, Panagioti, and Kontopantelis Citation2022). Likewise, the reasons behind the non-reporting of hearing loss revealed in our study may reflect a stigma to admitting hearing problems, potential barriers in health communication with providers or low health literacy skills among specific population groups. A previous study showed that women, those with low education, smokers and heavy drinkers were at a higher risk of not recognising their hearing had deteriorated and were thus less likely to seek help (Tsimpida et al. Citation2020a). Therefore, these population groups not only are not only at a higher risk of not recognising the symptoms of hearing loss but are also more likely to not report them once they are aware of their hearing loss. Further information about the experiences of these population subgroups in England, along with any personal predictors on hearing aid uptake, use, and benefits (Ferguson, Woolley, and Munro Citation2016; Nixon et al. Citation2021; Van Leeuwen et al. Citation2021) should be further explored, as it was not possible to obtain this information through this dataset.
Lastly, the ELSA provides data for individuals living in private households, and data for individuals living in residential and nursing homes are not included (Marmot et al., Citation2003). Furthermore, the study does not offer any information on participants from ethnic minorities, as there is no ethnicity variable in the ELSA.
Research and policy implications
In 2021, the UK NSC (Solutions for Public Health Citation2021) acknowledged that the limitation of the review on screening for hearing loss in adults was the insufficiency of good quality evidence to clearly judge an outcome or effect relating to the key questions about screening adults for hearing loss. For example, no studies were identified that explored the proportion of people seeking help for hearing-related problems and the subsequent proportions that were referred, diagnosed and treated or remained undiagnosed. A larger volume of high-quality evidence is needed on the proportion of uptake of treatment in the detected population in the UK.
Therefore, our study provides novel evidence that may have important health policy implications and underscores the need for evidence-based hearing screening programmes in England. The early detection of hearing loss by primary care professionals in routine assessments may not only promote better diagnosis of hearing loss and better hearing health but also prevent or delay the onset of conditions known to relate to untreated hearing loss, such as social isolation and depression (Tsimpida et al. Citation2021b). Our findings highlight opportunities for targeted interventions in England to raise awareness of primary prevention and initial symptoms of hearing loss, aiming to improve the reporting of hearing loss to primary care health professionals, which can lead to further hearing assessment for individuals. Public health campaigns may help improve public awareness of the importance of addressing hearing loss early (David, Zoizner, and Werner Citation2018; Tsimpida et al. Citation2020a). Adults aged 50–75 years have been identified in a recent study as a key target group for a potential hearing awareness campaign (Alperstein and Beach Citation2022). Future studies exploring the reasons for the underutilisation of hearing aids, including cultural or language barriers (Ismail et al. Citation2019), and studies targeting specific socioeconomic groups that are particularly unlikely to access hearing services and use hearing aids (Scholes et al. Citation2018), are of particular importance.
Our findings also support the need for effective interventions to improve primary care providers’ hearing loss awareness in England (Maru et al. Citation2021). In a recent study, only 40% of primary care providers believed hearing loss is treatable, and only 17% believed it is preventable (Sydlowski et al. Citation2022), which shows that primary healthcare professionals’ current awareness and literacy surrounding hearing loss are poor. Knowledge regarding the types of message framing in clinical communication between people with hearing loss and primary care providers is limited and needs further exploration. Training modules for hearing loss awareness from the early stages of medical education and throughout their medical career (i.e. continuous professional development seminars) would be beneficial (Maru et al. Citation2021).
Recent developments in the Royal College of General Practitioners (RCGP) Core Curriculum now stress the importance of early intervention, effective communication, and improved access for people who are deaf or have hearing loss, aligned with NICE Guidance (Ftouh et al. Citation2018), which states that audiological assessments should be arranged for adults presenting with hearing loss for the first time (or in whom hearing loss is suspected). To help ensure this can be achieved, future work should assess in detail health provider and system factors to better understand why one in five people in our study were not referred by professionals for an ear examination. The feasibility of multilevel interventions (at the patient, provider, and system level) to improve access and continuity of care for people with hearing loss is an area for future investigations.
The hearing measures in the ELSA are directly comparable to seven other national surveys with harmonised physical and anthropometric measurements that are publicly available in the “Gateway to Global Ageing” [https://g2aging.org/]. Our study, the first to address the research aims of this manuscript in a nationally representative dataset, offers a unique opportunity for researchers to examine the same research questions in other countries and undertake cross-national comparisons with significant health policy implications.
Conclusions
Several barriers in the pipeline of hearing care exist at the patient, provider, and system levels. Our study revealed that the majority (78.9%) of individuals who acknowledge and report hearing loss are happy to use or try a hearing aid. Our findings indicate that the percentage of hearing aid users should be calculated as a proportion of those who actively acknowledge and report having hearing loss, otherwise this may lead to an underestimation of those who could potentially use a hearing aid, putting the blame on individuals while the actual reason for the underutilisation may lie with health system failures and wider determinants of health. Development of interventions to improve both the acknowledgement and reporting of hearing loss by both individuals and primary healthcare providers is encouraged by our findings, as a promising avenue for addressing preventable barriers to accessing hearing healthcare.
Ethical approval
Ethical approval for all the ELSA waves was granted by the National Research and Ethics Committee (MREC/01/2/91).
Consent form
Written informed consent was obtained from all individual participants included in ELSA (not relating specifically to this study). Details of the ELSA study design, sample and data collection are publicly available at the ELSA’s project website [https://www.elsa-project.ac.uk/].
Author contributions
DT and SR developed the idea, and all authors designed the study. DT was responsible for conducting the analyses, interpreting the results, and drafting the manuscript. DT, SR, MP and HH critically revised the manuscript. All authors have read and approved the final manuscript and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Supplemental Material
Download PDF (163.5 KB)Disclosure statement
DT is owner of a “Design Patent” for hearing aid (International Design Classification Version: 13-2021, Registered Design No: 6196408). All other authors declare that they have no competing interests. The views expressed in this article are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health and Social Care.
Data availability statement
The English Longitudinal Study of Ageing dataset is publicly available via the UK Data Service (http://www.ukdataservice.ac.uk). Statistical code is available from the corresponding author upon request at [email protected].
Additional information
Funding
References
- Alperstein, S., and E. F. Beach. 2022. “Prioritizing the Target Audience for A Hearing Awareness Campaign in Australia Using the TARPARE Model.” Health Promotion International: daac041. doi:10.1093/heapro/daac041. Epub ahead of print.
- Antunes, J. L. F. 2019. “How to Correct the Odds Ratio for Lack of Sensitivity and Specificity.” Community Dentistry and Oral Epidemiology 47 (6):449–453. doi:10.1111/cdoe.12489.
- Barnett, M., B. Hixon, N. Okwiri, C. Irungu, J. Ayugi, R. Thompson, J. B. Shinn, and M. L. Bush. 2017. “Factors Involved in Access and Utilization of Adult Hearing Healthcare: A Systematic Review.” The Laryngoscope 127 (5):1187–1194. doi:10.1002/lary.26234.
- Barton, G., A. Davis, I. W. S. Mair, A. Parving, U. Rosenhall, and M. Sorri. 2001. “Provision of Hearing Aid Services: A Comparison Between the Nordic Countries and the United Kingdom.” Scandinavian Audiology 30 (3):16–20. doi:10.1080/010503901750409394.
- Benova, L., E. Grundy, and G. B. Ploubidis. 2015. “Socioeconomic Position and Health-Seeking Behavior for Hearing Loss Among Older Adults in England.” The Journals of Gerontology Series B 70 (3):443–452. doi:10.1093/geronb/gbu024.
- Bisgaard, N., and S. Ruf. 2017. “Findings from EuroTrak Surveys from 2009 to 2015: Hearing Loss Prevalence, Hearing Aid Adoption, and Benefits of Hearing Aid Use.” American Journal of Audiology 26 (3S):451–461. doi:10.1044/2017_AJA-16-0135.
- Bisgaard, N., S. Zimmer, M. Laureyns, and J. Groth. 2022. “A model for Estimating Hearing Aid Coverage World-Wide Using Historical Data on Hearing Aid Sales.” International Journal of Audiology 61 (10):841–849. doi:10.1080/14992027.2021.1962551.
- David, D., G. Zoizner, and P. Werner. 2018. “Self-Stigma and Age-Related Hearing Loss: A Qualitative Study of Stigma Formation and Dimensions.” American Journal of Audiology 27 (1):126–136. doi:10.1044/2017_AJA-17-0050.
- Davis, A., P. Smith, M. Ferguson, D. Stephens, and I. Gianopoulos. 2007. “Acceptability, Benefit and Costs of Early Screening for Hearing Disability: A Study Of Potential Screening Tests and Models.” Health Technology Assessment 11 (42):1–294.
- Department of Health. 2016. “UK Chief Medical Officers’ Low Risk Drinking Guidelines,” August 11. https://www.gov.uk/%0Ahttps://www.gov.uk/government/uploads/system/uploads/attachment_data/file/545937/UK_CMOs__report.pdf.
- Dillon, H., J. Day, S. Bant, and K. J. Munro. 2020. “Adoption, Use and Non-Use of Hearing Aids: A Robust Estimate Based on Welsh National Survey Statistics.” International Journal of Audiology 59 (8): 567–573. doi:10.1080/14992027.2020.1773550.
- Ferguson, M. A., P. T. Kitterick, L. Y. Chong, M. Edmondson-Jones, F. Barker, et al. 2017. “Hearing Aids for Mild to Moderate Hearing Loss in Adults.” The Cochrane Database of Systematic Reviews 9: CD012023.
- Ferguson, M. A., A. Woolley, and K. J. Munro. 2016. “The Impact of Self-Efficacy, Expectations, and Readiness on Hearing aid Outcomes.” International Journal of Audiology 55: S34–S41. doi:10.1080/14992027.2016.1177214.
- Ftouh, S., K. Harrop-Griffiths, M. Harker, K. J. Munro, and T. Leverton. 2018. “Hearing Loss in Adults, Assessment and Management: Summary of NICE Guidance.” BMJ 361: k2219.
- Hill, S., K. Holton, and C. Regan. 2015. Action Plan on Hearing Loss. London: NHS Engl Dep Heal.
- Ismail, A. H., K. J. Munro, C. J. Armitage, and P. D. Dawes. 2019. “What Do Hearing Healthcare Professionals Do to Promote Hearing Aid Use and Benefit Among Adults? A Systematic Review.” International Journal of Audiology 58 (2):63–76. doi:10.1080/14992027.2018.1531154.
- Laplante-Lévesque, A., K. J. Brännström, E. Ingo, G. Andersson, and T. Lunner. 2015. “Stages of Change in Adults Who Have Failed an Online Hearing Screening.” Ear and Hearing 36 (1):92–101. doi:10.1097/AUD.0000000000000085.
- Van Leeuwen, L. M., T. P. M. Goderie, M. F. van Wier, B. I. Lissenberg-Witte, U. Lemke, and S. E. Kramer. 2021. “Uptake of Hearing Aids and Hearing Assistive Technology in a Working Population: Longitudinal Analyses of The Netherlands Longitudinal Study on Hearing.” Ear and Hearing 42 (4):793–802. doi:10.1097/AUD.0000000000000983.
- Little, R. J. A, and D. B. Rubin. 2019. Statistical Analysis With Missing Data. Hoboken: John Wiley & Sons.
- Marmot, M., J. Banks, R. Blundell, C. Lessof, and J. Nazroo. 2003. Health, Wealth and Lifestyles of the Older Population in England. London: Institute of Fiscal Studies.
- Maru, D., J. Stancel-Lewis, G. Easton, and W. E. J. Leverton. 2021. “Communicating With People With Hearing Loss: COVID-19 and Beyond.” BJGP Open 5 (1):BJGPO.2020.0174. doi:10.3399/BJGPO.2020.0174.
- McDaid, D., A.-L. Park, and S. Chadha. 2021. “Estimating the Global Costs of Hearing Loss.” International Journal of Audiology 60 (3):162–170. doi:10.1080/14992027.2021.1883197.
- Mittag, N. 2013. Imputations: Benefits, Risks and a Method for Missing Data. Chicago: Harris School of Public Policy, University of Chicago.
- Natcen Social Research. 2018. ELSA User Guide to the Main Interview Datasets. London: Natcen Social Research.
- NICE. 2018. Hearing Loss in Adults: Assessment and Management. London: National Institute for Health and Care Excellence.
- Nixon, G., J. Sarant, D. Tomlin, and R. Dowell. 2021. “Hearing Aid Uptake, Benefit, and Use: The Impact of Hearing, Cognition, and Personal Factors.” Journal of Speech, Language, and Hearing Research 64 (2):651–663. doi:10.1044/2020_JSLHR-20-00014.
- Sawyer, C. S., C. J. Armitage, K. J. Munro, G. Singh, and P. D. Dawes. 2019. “Correlates of Hearing Aid Use in UK Adults: Self-Reported Hearing Difficulties, Social Participation, Living Situation, Health, and Demographics.” Ear and Hearing 40 (5):1061–1068. doi:10.1097/AUD.0000000000000695.
- Sawyer, C. S., C. J. Armitage, K. J. Munro, G. Singh, and P. D. Dawes. 2020. “Biopsychosocial Classification of Hearing Health Seeking in Adults Aged Over 50 Years in England.” Ear and Hearing 41 (5): 1215–1225. doi:10.1097/AUD.0000000000000839.
- Schneider, J., B. Gopinath, M. J. Karpa, C. M. McMahon, E. Rochtchina, S. R. Leeder, and P. Mitchell. 2010. “Hearing Loss Impacts on the Use of Community and Informal Supports.” Age and Ageing 39 (4):458–464. doi:10.1093/ageing/afq051.
- Scholes, S., J. Biddulph, A. Davis, and J. S. Mindell. 2018. “Socioeconomic Differences in Hearing Among Middle-Aged and Older Adults: Cross-Sectional Analyses Using the Health Survey for England.” BMJ Open 8 (2):e019615. doi:10.1136/bmjopen-2017-019615.
- Schulz, K. A., N. Modeste, J. Lee, R. Roberts, G. H. Saunders, and D. L. Witsell. 2016. “Factors Influencing Pursuit of Hearing Evaluation: Enhancing the Health Belief Model with Perceived Burden from Hearing Loss on Communication Partners.” International Journal of Audiology 55 (sup3):S69–S78. 10.3109/14992027.2015.1136437.
- Siemens Audiologische Technik GmbH. 2007. “Hear Check Screener User Guide.” PUBLICIS. http://www.connevans.info/image/connevans/38shearcheck.pdf.
- Solutions for Public Health. 2021. “Screening for Hearing Loss in Adults.” External Review Against Programme Appraisal Criteria for the UK National Screening Committee. https://view-health-screening-recommendations.service.gov.uk/hearing-loss-adult/.
- Steptoe, A., E. Breeze, J. Banks, and J. Nazroo. 2013. “Cohort Profile: The English Longitudinal Study of Ageing.” International Journal of Epidemiology. 42 (6):1640–1648. doi:10.1093/ije/dys168.
- Sydlowski, S. A., J. P. Marinelli, C. M. Lohse, and M. L. Carlson. 2022. “Hearing Health Perceptions and Literacy Among Primary Healthcare Providers in the United States: A National Cross-Sectional Survey.” Otology & Neurotology 43 (8):894–899. doi:10.1097/MAO.0000000000003616.
- Tsimpida, D., E. Kontopantelis, D. Ashcroft, and M. Panagioti. 2018. “Socioeconomic and Lifestyle Factors Associated With Hearing Loss in Older Adults: A Cross-Sectional Study of the English Longitudinal Study of Ageing (ELSA).” BMJ Open 9 (9): e031030.
- Tsimpida, D., E. Kontopantelis, D. M. Ashcroft, and M. Panagioti. 2020a. “Comparison of Self-reported Measures of Hearing With an Objective Audiometric Measure in Adults in the English Longitudinal Study of Ageing.” JAMA Network Open 3 (8):e2015009–e2015009. doi:10.1001/jamanetworkopen.2020.15009.
- Tsimpida, D., E. Kontopantelis, D. M. Ashcroft, and M. Panagioti. 2020b. “Regional Patterns and Trends of Hearing Loss in England: Evidence from the English Longitudinal Study of Ageing (ELSA) and Implications for Health Policy.” BMC Geriatrics 20 (1):1–14. doi:10.1186/s12877-020-01945-6.
- Tsimpida, D., E. Kontopantelis, D. M. Ashcroft, and M. Panagioti. 2021a. “Conceptual Model of Hearing Health Inequalities (HHI Model): A Critical Interpretive Synthesis.” Trends in Hearing 25:1–19.
- Tsimpida, D., E. Kontopantelis, D. M. Ashcroft, and M. Panagioti. 2021b. “The Dynamic Relationship Between Hearing Loss, Quality of Life, Socioeconomic Position and Depression and the Impact of Hearing Aids: Answers from the English Longitudinal Study of Ageing (ELSA).” Social Psychiatry and Psychiatric Epidemiology 57 (2): 353–362.
- Tsimpida, D., M. Panagioti, and E. Kontopantelis. 2022. “Forty Years On: A New National Study of Hearing in England and Implications for Global Hearing Health Policy.” Int. J. Audiol 62 (1): 62–70.
- Wallhagen, M. I., and E. Pettengill. 2008. “Hearing Impairment: Significant But Underassessed in Primary Care Settings.” Journal of Gerontological Nursing 34 (2):36–42. doi:10.3928/00989134-20080201-12.
- Wilson, B. S., D. L. Tucci, M. H. Merson, and G. M. O'Donoghue. 2017. “Global Hearing Health Care: New Findings and Perspectives.” The Lancet 390 (10111):2503–2515. doi:10.1016/S0140-6736(17)31073-5.
- World Health Organization. 2021. Hearing Screening: Considerations for Implementation. Available at: https://www.who.int/publications/i/item/9789240032767.
- Young, A. 2014. Older Deaf People and Social Care: A Review. Southampton: Royal Association for Deaf People (RAD) [Sonus], 50.
- Yueh, B., N. Shapiro, C. H. MacLean, and P. G. Shekelle. 2003. “Screening and Management of Adult Hearing Loss in Primary Care: Scientific Review.” JAMA 289 (15):1976–1985. doi:10.1001/jama.289.15.1976.
- Zaninotto, P., and A. Steptoe. 2019. “English Longitudinal Study of Ageing.” In Encyclopedia of Gerontology and Population Aging, 1–7. Singapore: Springer. https://www.elsa-project.ac.uk/study-documentation.
