Abstract
Objective
The objective of the study was to evaluate the effect of including synchronous remote fine-tuning and follow-up as a part of the aural rehabilitation process.
Design
A randomised controlled trial (RCT).
Study sample
Experienced hearing aid users who were due for renewed aural rehabilitation were randomised to either an intervention group (n = 46) or a control group (n = 49). Both groups underwent all stages of the conventional renewed aural rehabilitation process within our clinics, but the intervention group was also offered remote follow-up visits, including an opportunity for synchronous remote fine-tuning of hearing aids. The Hearing Handicap Inventory for the Elderly/Adults (HHIE/A), the Abbreviated Profile of Hearing Aid Benefit (APHAB), and the International Outcome Intervention for Hearing Aid Users (IOI-HA) were used as outcome measures.
Results
Both groups improved in self-rated hearing difficulties and hearing aid benefits measured with HHIE/A and APHAB. No significant differences were found between the intervention and the control group.
Conclusion
Including synchronous remote follow-up and fine-tuning as a part of an aural rehabilitation process may effectively complement clinical visits. Additionally, the synchronous remote follow-up has the potential to further develop person-centred care by enabling hearing aid users to identify individual needs directly in an everyday environment.
Introduction
It has been well documented in the literature that addressing hearing loss with sensory management, such as hearing aid fitting, as an intervention within aural rehabilitation (AR), can reduce activity and participation restrictions and improve health-related quality of life. Hearing aid (HA) fitting, together with informational and psychosocial counselling, conceptualises key elements needed to be included in AR when targeting good hearing health (Gotowiec et al. Citation2022). As AR is a life-long process these included elements may be repeated in different stages. To achieve beneficial outcomes with HA use, there is a need to address both audiological and non-audiological factors (Hickson et al. Citation2014). Hickson and colleagues found that factors such as support from significant others, experiences of hearing difficulties pre-HA-fitting, experiences of self-efficacy and benefit post-HA-fitting, and positive attitudes towards HAs are all indicative of successful HA use. Furthermore, factors such as degree of hearing loss, gender, motivation, and HA usage time may also predict hearing aid outcomes for both new and experienced HA users (Houmøller et al. Citation2022). For example, experienced HA users report higher motivation in HA use than first-time HA users.
Even though HA fitting is a beneficial intervention and a cost-effective approach within AR, HA-related problems may arise after the intervention. This includes problems with HA management, sound quality, and performance (Bennett et al. Citation2018). Sound quality can be addressed, for example, with fine-tuning by a clinician, who often bases changes to HA settings on the HA user’s self-reported experiences in a listening environment and the fine-tuning experience of the clinician. In a qualitative study evaluating the perspectives of experienced hearing aid users, Parmar et al. (Citation2021) identified that enabling accessible services and addressing person-specific aspects of hearing loss may benefit AR and HA outcomes (i.e. a person-centred approach). For example, the participants expressed a need for audiologists to include more specific questions regarding the impact of hearing loss on employment and home life to provide individual intervention options. A person-centred approach engages patients, significant others, and clinicians in sharing information and enables clinicians to address patients’ psychosocial concerns (Scholl et al. Citation2014). However, research reveals a discrepancy in the extent to which audiologists address patient concerns and self-reported psychosocial problems and identifies a continuous use of clinician-centred approaches in practice (Bennett et al. Citation2021). Gomez et al. (Citation2022) suggest, for example, that a smartphone-connected HA that enables manual adjustability and interactions through an application to a mobile device could empower the patient to manage their hearing loss. This relates closely to a person-centred approach. Furthermore, previous research suggests that including online interventions through counselling and communication programs may positively affect psychosocial concerns (Malmberg et al. Citation2017, Citation2022; Ferguson et al. Citation2021). Dillon et al. (Citation2020) showed recently that many HA users do not use or under-use their HAs over time. The authors emphasise the need to identify new methods that support HA users to adapt to their HAs and/or encourage users to use them consistently. Supporting and empowering HA users is a continuous process that needs to be an integral part of every person’s comprehensive hearing health journey (Gotowiec et al. Citation2022).
Accessibility to support has become more widespread within AR, and there is a great interest in digital solutions within clinical hearing care (Muñoz, Nagaraj, and Nichols Citation2021). Supporting hearing care by using online tools may positively expand AR. The benefits of online tools are supported by several studies, mostly addressing asynchronous solutions. For example, previous studies support the efficacy of online screening (Eksteen et al. Citation2019), online diagnostics (Barbour et al. Citation2019), interventions that increase HA users’ engagement in AR (Ferguson et al. Citation2021), and HA fitting and follow-up services (Pross, Bourne, and Cheung Citation2016). Research shows that supplementing AR with video information at home may increase social engagement for first-time HA users (Ferguson et al. Citation2021). Furthermore, online interventions may improve self-perceived hearing difficulties for experienced HA users (Malmberg et al. Citation2017, Citation2022) and improve HA benefits (Malmberg et al. Citation2018). In a study by Pross, Bourne, and Cheung (Citation2016), audiologists supervised HA fitting and adjustment using real-time video consultations with the HA user and an audiology technician. The consultations resulted in HA satisfaction that could be measured with in-person service. Tao et al. (2021) compared remote follow-up consultations to standard consultations and found that both modes of service delivery were appreciated by HA users, and both resulted in significantly improved outcome measures regarding communication and fitting. A recent study compared remote HA renewal based on a pre-existing audiogram and self-perceived hearing difficulties to a conventional renewal, showing that the remote mode of HA fitting is feasible (Kokkonen et al. Citation2022). Convery et al. (Citation2019) found that the use of an asynchronous mode, which enables HA users to remotely request, receive, and upload fine-tuning from a clinician, is a usable mode for experienced HA users.
In summary, the literature shows that there is a need to expand AR services and potential resources clinicians could use to achieve this expansion. Yet, to our knowledge, no study includes a synchronous mode with direct remote fine-tuning and online communication between the patient and the audiologist. Therefore, the main aim of the current study was to investigate the effect of including synchronous remote fine-tuning and online communication as part of AR from a clinical perspective. More specifically, we aimed to evaluate whether synchronous remote fine-tuning and online communication can affect HA users’ self-perceived hearing problems, hearing aid benefits, self-perceived accessibility, involvement, and participation in AR compared to a control group receiving standard care.
Materials and methods
The present study was approved by the Swedish Ethical Review Authority (Dnr. 2019-04021). The study was conducted as a randomised controlled trial (RCT) and registered at ClinicalTrials.gov, NCT04840277.
Participants and recruitment
The study was conducted at three different clinics within the Hearing Organisation, Västra Götaland County (VGC). The recruitment letter, including the study procedure and a consent form, was sent to experienced HA users (>20 years of age) on a waiting list for a renewed AR and HA fitting. The recruitment letter also stated that the participants would be randomised into two different groups, that participation was voluntary, and required the HA user to have access to and be able to use a mobile phone with capabilities for audio calls, video calls, messaging, and the installation of a mobile application. The last inclusion criterion was that the HA user was able to understand spoken and written Swedish. In addition, all potential participants were contacted by telephone to provide further information on study participation, if needed. Those who agreed to participate returned a signed consent form.
In all, sixteen (16) different audiologists contributed to the study recruitment process and conducted AR for recruited participants, either in the intervention group or control group. The 16 audiologists held regular meetings every month during the study procedure to share knowledge and experiences.
Outcome measures
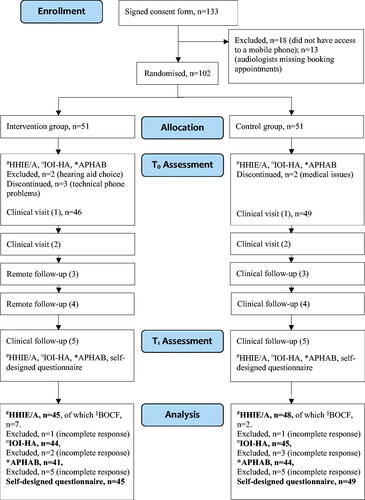
The renewed AR was evaluated for both groups using questionnaires in connection with the first and last clinic visits (see ).
Figure 1. Flowchart of the study procedure. #HHIE/A: Hearing Handicap Inventory for the Elderly/Adults; ¤IOI-HA: International Outcome Inventory for Hearing Aids; *APHAB: Abbreviated Profile of Hearing Aid Benefit; §BOCF: Baseline Observation Carried Forward.
The Hearing Handicap Inventory for the Elderly (HHIE; Ventry and Weinstein Citation1982) and the Hearing Handicap Inventory for the Adults (HHIA; Newman et al. Citation1990) were used as the main outcome measures to assess the self-perceived psychosocial and emotional effects of hearing loss. The HHIE in the current study targeted HA users above 65 years of age, while the HHIA targeted HA users under 65 years. The subscales of both questionnaires are Social, with 12 questions, and Emotional, with 13 questions. A higher value indicates greater self-perceived hearing problems.
The Abbreviated Profile of Hearing Aid Benefit (APHAB; Cox and Alexander Citation1995) was used as a secondary outcome measure. The APHAB consists of 24 questions and addresses self-perceived activity limitations in daily life situations associated with hearing loss, without wearing HA compared to wearing HA (i.e. hearing aid benefit) and comprises four subscales: Ease of Communication, Reverberation, Background Noise, and Aversiveness. A higher value indicates greater self-perceived limitation/restriction associated with hearing loss.
In addition, the International Outcome Inventory for Hearing Aids (IOI-HA; Cox et al. Citation2000) was also used as a secondary outcome measure to highlight various aspects of HA use. The IOI-HA addresses Use, Benefit, Residual Activity Limitation, Satisfaction, Residual Participation Restriction, Impact on Others, and Quality of Life. A higher value indicates a better outcome.
The final clinical visits for both groups included a self-designed questionnaire concerning the HA users’ perceived experiences of, and involvement in, hearing care throughout the study period (see ). Questions such as, “How well did you understand the information you were given during your AR?”, “What information regarding your AR do you consider most important?”, “Did you have an opportunity to ask questions if needed?”, and “Would you consider yourself involved in your AR?”, were asked (see Supplementary Appendix 1). The self-designed questionnaire included twelve questions with a response scale from 1 (totally disagree) to 4 (totally agree) for nine questions and three free-text questions. For those, the HA users were encouraged to express 1) individual experiences of essential information given during the AR, 2) personal perspectives on patient involvement in AR, and 3) an example of patient involvement in AR during the study.
Conventional aural rehabilitation
The conventional AR within Hearing Organisation includes up to four clinical visits, consisting of elements such as diagnostic tests, collection of relevant information about the person with hearing impairment, and informational counselling during the first visit. Sensory management, such as HA fitting (HAs of a wide assortment, with/without compatibility to remote mobile applications) and psychosocial counselling are addressed during the second visit. HA maintenance, continued psychosocial counselling, and fine-tuning are addressed during the third and fourth visits. If the HA user experiences hearing deterioration after completing AR, a new diagnostic test is necessary to proceed with the rehabilitation. The HA user is then a candidate for a renewed AR and HA fitting, i.e. repeating the above elements.
Study procedure
The participants who were interested in participating in the study were randomised into two groups after responding to the HHIE/A, APHAB, and IOI-HA: an intervention group (group 1, n = 51) and a control group (group 2, n = 51). Both groups underwent all stages of conventional AR at our clinics. The control group was offered five clinical visits (see ), while the intervention group was offered two initial clinical visits, two remote follow-ups, and a final clinical follow-up (see ).
All 16 audiologists were instructed to follow the procedure for conventional AR for both the intervention and control group and to include time for the participant to respond to questionnaires in connection with the first clinical visit (HHIE/A, APHAB, and IOI-HA). In addition to conventional AR, both groups received information about the study during the first visit and were able to ask questions regarding participation. The intervention group was required to install a mobile application during their second clinical visit to enable the remote follow-ups. The mobile application was specific for each HA supplier, free of charge, and was available for iPhone and Android mobile phones. Five different mobile applications and HA suppliers were selected based on the participant’s hearing loss and individual needs. The audiologist interacted with each application through a web platform that was linked to the HA manufacturer. In addition, the intervention group had the opportunity to test-run a remote follow-up on-site during the second visit. Finally, both groups responded to the questionnaires, HHIE/A, APHAB, IOI-HA, and a self-designed questionnaire during the last clinical visit (fifth visit).
Analysis
Two participants in the intervention group were excluded from the study after the audiologist and HA user jointly chose the HA without remote adjustment capability (see , hearing aid choice). Further on, some participants dropped out due to technical problems (intervention group, n = 3) and medical issues (control group, n = 2) and were also excluded from the study. In total, 46 participants in the intervention group and 49 in the control group attended the final clinical follow-up (see ). On some occasions, the correct HHIE/A was not administered for post-measurement (n = 9). As the HHIE/A questionnaires differ on three questions, baseline observation carried forward (BOCF) was applied to these three questions at post-measurement for these occasions. The method is used to compensate for missing data, meaning that if post-observation is missing, baseline observation is carried forward. Participants who did not complete all questions of an outcome measure (i.e. incomplete response in ) in accordance with the original references (Ventry and Weinstein Citation1982; Cox et al. Citation2000; Newman et al. Citation1990) were excluded from the analysis (see ).
Both groups were examined at two measurement time points: pre-treatment (T0) and post-treatment (T1). To ensure a between-group effect at the 5% significance level, 60 participants were estimated to be included in the study. The power calculation is based on the expected standardised mean difference for the HHIE-total scale.
Variance analysis (ANOVA = Analysis of Variance) was used to investigate the mean difference between the HHIE/A T0 to T1, exploring the main effect of time and group, and the interaction effect between group and time. T-tests with Bonferroni correction were applied where the interaction effect or main effect was demonstrated. Chi2 tests were also used to compare the proportions showing clinically relevant changes T0 to T1 for HHIE/A and APHAB, and for comparing responses in the self-designed questionnaire between the two groups. Effect size (Cohen’s d) is presented for the main and the secondary outcome measures. Mann-Whitney U test was used to investigate differences between T0 to T1 for APHAB and IOI-HA.
Results
The HHIE/A analysis for the total scale and subscales is presented in . Bonferroni-adjusted t-tests indicate that both the intervention group and control group significantly improved their HHIE/A scores at T1 measurements compared to T0. No significant interaction effect was found between the groups. The analysis shows large and medium within-group effect sizes for both groups and medium between-group effect sizes.
Table 2. Observed means (OM) and standard deviations (SD) for HHIE/A (n = 93), APHAB (n = 85), and IOI-HA (n = 89) are presented for both groups before intervention (T0) and after intervention (T1).
Furthermore, according to Weinstein, Spitzer, and Ventry (Citation1986), when administering the HHIE/A with “paper and pen” without an audiologist present, an individual change from T0 to T1 for the total HHIE/A scale should be 36% to be considered clinically relevant. In the intervention group, 44% showed such improvement, and in the control group, 52%. No significant difference was found between the groups (χ2 [1, n = 93] = 0.56, p = 0.46).
The APHAB analysis is presented in , comparing values at T0/unaided to T1/aided. Both groups show significant improvements for all subscales except the Background noise subscale for the intervention group. Mostly large and medium within-group effect sizes were found. Also, according to Cox (Citation1997), individual changes from T0 to T1 should be a score of 22 for the subscales Ease of Communication, Background Noise, and Reverberation and a score of 31 for the subscale Aversiveness to be clinically relevant. In the present study, 78% of the participants in the intervention group showed such a change for the Ease of Communication subscale, 7% for the Reverberation subscale, and 5% for the Background Noise subscale. The corresponding results for the control group were 88% for the Ease of Communication subscale (no significant difference compared to the intervention group χ2 [1, n = 85] = 0.69, p = 0.41), 25% for the Reverberation subscale, and 16% for the Background Noise subscale. For the subscale, Aversiveness, 34% in the intervention group showed improvements with scores ≥31 and 27% in the control group (no significant difference between groups χ2 [1, n = 85] = 0.15, p = 0.69).
The analysis for each IOI-HA question is presented in , showing significant improvements for each question and both groups and mostly large and medium within-group effect sizes.
The self-designed questionnaire, which addresses self-perceived usability, involvement, and participation in AR, showed positive results. The average score for all nine questions was from 3.6 to 3.9 for the intervention group and from 3.8 to 4.0 for the control group (response scale from 1 to 4). No significant differences were found between the groups when comparing the responses for each question (see Supplementary Appendix 1). The first free-text question was answered by 74 HA users. Most responses concerned positive aspects relating to the importance of shared decision-making and fruitful communication between the audiologist and the HA user. The second free-text question was answered by 68 participants, and responses highlighted the importance of feeling heard and understood, having the opportunity to ask questions, and getting understandable health information. A total of 61 HA users gave examples of experiences of patient involvement in AR. Most of the examples concerned the interaction with the audiologist, where HA users felt involved regardless of whether the meeting took place remotely or in the clinic. For example, one participant in the intervention group who experienced hearing difficulties when listening to music appreciated the ability to fine-tune remotely and simultaneously, while playing piano in her living room. Finally, the monthly discussions among the 16 audiologists who conducted AR concerned the challenges and advantages of the new technology; for example, many audiologists initially expressed concern about not being in the same room as the HA user, but they ultimately perceived advantages when gaining insight into the HA user’s everyday life.
Discussion
The results of this study highlight the advantages of expanding AR services using online resources to support hearing care, which is in line with previous research evaluating online support for HA users (Convery et al. Citation2019; Ferguson et al. Citation2021; Kokkonen et al. Citation2022; Muñoz, Nagaraj, and Nichols Citation2021; Malmberg et al. Citation2022). This study explored a synchronous mode with direct remote fine-tuning and online communication between the patient and the audiologist compared to a control group receiving standard care. We aimed to evaluate HA users’ self-perceived hearing problems, hearing aid benefits, self-perceived accessibility, involvement, and participation in AR.
Most of the study participants were men, aged between 65 and 85 years, i.e. experienced HA users (see ). Previous research including online interventions also shows gender differences in participation (Malmberg et al. Citation2017, Citation2022). As the study addresses new technology, one potential explanation could be that women did not feel that they had the technical competence required to participate in the study. However, a literature review showed that gender differences play a minor role when using new technology (Goswami and Dutta Citation2016). Gomez et al. (Citation2022) found that despite gender, the barriers to using technology, for example, smartphone connected HAs, are related to perceived literacy skills and the ability to use smartphones. The participants in the current study were informed about the requirement to be able to use a mobile phone, which may indicate that more men than women consider themselves to have high digital literacy skills. The participants had, on average, mild to moderate hearing loss, representing the most common patient category at our clinics.
Table 1. Demographics of the participants, showing the mean and standard deviations in brackets, or number (n) and % in brackets.
The results of primary outcome measures HHIE/A in the current study revealed rather large subjective hearing-related problems at T0 for both groups, even though the participants had previously undergone AR. This could be due to the actual HL deterioration, which may be the reason for renewed AR, or due to potential HA-related problems, such as sound quality and HA performance (Bennett et al. Citation2018). The results for the HHIE/A-total scale and the Social and Emotional subscales showed significant improvements from T0 to T1 for both groups, indicating benefits in AR when addressing the participants’ self-perceived hearing problems. The positive outcomes of AR for persons with HL have been well established in previous research. However, the intervention group showed lower scores in both T0 and T1 for the HHIE/A scale compared to the control group (see ). As some of the participants in the intervention group were excluded or discontinued due to technical issues, the challenges experienced when using technology in hearing care could explain the lower scores in the intervention group (Angley, Schnittker, and Tharpe Citation2017). Furthermore, a difference is noted in within-group ES for the HHIE/A Emotional and Social subscales (see ), indicating that audiologists may better address the HA user’s emotional difficulties related to HL when offering standard care and may better address the HA user’s social difficulties when offering synchronous remote fine-tuning and online communication. It may also indicate that the HA user is better at expressing emotional/social difficulties related to HL in the corresponding rehabilitation setting. In a previous study that addressed remote HA adjustment by combining remote assistance with face-to-face sessions, the participants showed high satisfaction when evaluating subjective experiences of HA fitting (Penteado et al. Citation2014). Research shows that audiologists provide psychosocial support to people with HL, yet many perceive skill deficits when addressing such concerns in a clinical setting (Bennett et al. Citation2021). Furthermore, synchronous remote communication challenges the therapeutic relationship between the audiologist and the patient. Previous research highlights the importance of the audiologist’s attitude towards online services and professional development for study outcomes (Glista et al. Citation2021). Although the current study did not address the participating audiologists’ engagement, this should be taken into consideration when interpreting the study results. The audiologist needs to maintain soft variables in communication and not focus solely on technology, which has been highlighted in previous research (Bennett et al. Citation2018). For example, in case of any delay in image or sound transmission, small, subtle physical signs may disappear (Penteado et al. Citation2014). Penteado and colleagues recommend that audiologists receive training and support in order to perform remote HA fitting and adjustments. The 16 audiologists who conducted AR in the present study initially expressed concern about distancing the HA users during the online meetings, but on the contrary, they actually perceived that they gained greater insight into HA users’ everyday communication when using online meetings. This was discussed during some of the regular meetings every month during the study procedure. Many audiologists involved with the intervention group reported that it was an advantage to have the opportunity to better understand HA users’ everyday challenges, which may have encouraged higher engagement in AR for both the audiologists and the HA user. Conceivably, the HA user may be better able to express and identify hearing-related problems when addressing these issues from a location where the difficulties occur. This is in line with the person-centred approach, which encourages reciprocal involvement between the patient and audiologist when addressing psychosocial concerns (Scholl et al. Citation2014). Also, according to Parmar et al. (Citation2021), experienced HA users appreciate the personalised approach and that the audiologists communicate distinct aspects of hearing loss.
Overall, the APHAB questionnaire showed positive outcomes for the participants in both groups when comparing the unaided results with the aided results, which is indicative of improvements in communication abilities and the perception of sound in daily life situations. Previous research shows that the outcomes for the Ease of Communication and Reverberation subscales may be dependent on the degree of hearing loss (Brännström et al. Citation2020). The current results show large within-group effect sizes for the Ease of Communication subscale for both groups, however, compared to the participants in the current study, the participants in Brännström et al. (Citation2020) had no previous HA experiences. Conversely, one may assume that experienced HA users would better recognise speech, however, a previous study reveals that the length of hearing aid use is not significantly associated with speech recognition in silence/noise (Petry, Santos, and Costa Citation2010). Furthermore, the control group showed significantly more positive differences than negative differences, from T0 to T1 on the APHAB Background Noise subscale compared to the intervention group. The control group has a slightly lower degree of hearing loss compared to the intervention group (see ). The Background Noise subscale reflects speech recognition such as the two previously mentioned subscales, and this subscale may also be dependent on the degree of HL. On the contrary, Brännström et al. (Citation2020) did not find the same associations for this subscale. The APHAB is a clinical instrument, and the results show more clinically relevant improvements for the control group compared to the intervention group for the subscales Ease of communication, Background Noise, and Reverberation. One explanation for the findings in the current study may be that the participants in the intervention group had higher expectations for AR than the control group, due to the evaluation of novel technology. van Lente (Citation2012) argues that expectations for novel technologies could determine individual effort in research. On the other hand, Gomez et al. (Citation2022) showed that novel HA technology itself, obtained via a mobile application, is not what empowers the user. It is the modifiability and self-management of hearing loss that empowers the user. Self-management of hearing loss can increase confidence and motivation and improve HA users’ self-efficacy and daily life participation (Gomez et al. Citation2022; Gotowiec et al. Citation2022). Also, the subscale, Aversiveness, showed more clinically relevant improvements for the intervention group compared to the control group. As this subscale measures negative reactions to environmental sounds, these results could show that audiologists better address psychosocial concerns when assessing AR remotely, as shown in the outcomes for HHIE/A.
The IOI-HA demonstrates solely positive differences from T0 to T1 for all seven Items (see ). Similar results are attained in a previous study when renewing HAs in experienced HA users (Houmøller et al. Citation2022). Previous experience in HA use may in turn serve as motivation for continuous usage and HA benefits. For example, large within-group ESs are shown for both groups for Items 3 and 6, indicating improvements in experiences of activity limitation and impact on the environment. This is in line with a recent study, which presented high HA satisfaction rates in various listening situations in HA users who have owned more than one hearing aid and who are recently fitted with an HA (Picou Citation2010). Also, the within-group ES reveals greater improvements for the group receiving standard care in terms of satisfaction and participation restriction compared to the intervention group. This may be due to the lower T0 scores in the control group for the two questions or that audiologists address emotional concerns to a greater degree than social concerns during standard care, as is shown by the HHIE/A Social subscale. A previous study showed similar results in satisfaction when comparing remote HA follow-ups with standard face-to-face consultations (Tao et al. Citation2021). It may also be that audiologists assess social and emotional values differently depending on the mode of delivery. As remote service delivery is a rapidly growing field within AR (Muñoz, Nagaraj, and Nichols Citation2021), efforts to train and empower audiologists to retain soft variables in communication during the remote mode should be pursued as well. A recent study highlights the importance of ensuring audiologists have the opportunity to practice using tele-audiology for remote follow-ups in HA support (Glista et al. Citation2021). Other variables presented in the study that may influence the use of a remote mode are, for example, ease of service delivery, accessible technology, and access to help (Glista et al. Citation2021). Furthermore, a small between-group ES was noted for Item 7 in the IOI-HA, which showed greater improvements in the control group’s quality of life scores (see ). Earlier research points to the importance of preventing and controlling emotional problems that reduce health-related quality of life (Estancial Fernandes, Lima, and Barros Citation2019). Subsequently, question 7 indicates that the emotional concerns of both the intervention group and control group may have been sufficiently addressed in the study.
The self-designed questionnaire showed overall positive results for both groups regarding usability, involvement, and participation in AR. Usability has been recognised as a key prerequisite in the effective integration of online hearing health care in clinical practice (Convery et al. Citation2019), which may increase the accessibility of AR. Furthermore, the advantages of providing person-centred hearing care by an audiologist are well established in previous research (Bennett et al. Citation2021; Gotowiec et al. Citation2022; Parmar et al. Citation2021; Picou Citation2010; Scholl et al. Citation2014). However, the completed questionnaire was directly handed to the audiologist who was actively providing AR, which could lead the participant to answer the questionnaire in more favourable terms to the audiologist. This could be avoided if the questionnaires were, for example, left in a mailbox.
Consequently, it is likely that augmented technology used within hearing healthcare will influence and challenge the AR process and the opportunities for audiologists and persons with hearing loss to identify relevant audiological and non-audiological factors that could contribute to improved hearing care. The ability for audiologists to virtually enter HA users’ living rooms and everyday lives may expand the boundaries of hearing healthcare and guide the HA user in identifying specific individual goals, which may support the continuing process of empowering HA users (Gotowiec et al. Citation2022). Future research should assess challenges that may arise when addressing patient-specific aspects of using synchronous remote fine-tuning and follow-ups and examine what factors could enhance the provision of emotional and psychosocial support. In addition, further research should address the audiologists’ and patients’ views on perceived literacy skills and their influence on encouraging online hearing services, as well as the safety and effectiveness of a fully remote AR.
Strengths and limitations
The strength of this study is that it is a prospective randomised controlled study on a subject with, to the best of our knowledge, no previous reports.
Certain limitations should be considered when interpreting the results of the current study. Firstly, the RCT approach is used to reduce recruitment bias. However, all participants showed an interest in participating in the study, while some may have been more interested in the technology than others. It is possible that participants in the control group felt disappointed that they were not a part of the group evaluating novel capabilities, which may have affected their overall experience of the AR. Secondly, even though both the intervention and control groups were large enough to account for bias that may affect the outcomes of the study, the participants differed in HA-use experience, which could in turn affect their use of, for example, communication strategies or their motivation within AR (Houmøller et al. Citation2022). Additionally, more experienced HA users may have established HA management skills that influence their listening preferences.
Another limitation is that the participants in the intervention group were required to have access to a mobile phone and to install an application. This criterion excluded participants who used mobile devices with dated technology. Still, technology use is widespread among HA users (Picou Citation2010). Also, the intervention requires certain skills to use the technology, and previous research shows that older patients may need more support to feel confident when using technology as a part of hearing care (Angley, Schnittker, and Tharpe Citation2017). The participants in the current study may have needed, but not expressed the need for, such support.
Conclusions
This study found that providing a synchronous mode with direct remote fine-tuning and online communication between the patient and the audiologist as a complement to AR can significantly improve self-perceived hearing problems and hearing aid benefits. These conclusions correspond to the provision of standard care within our clinics. The study results also showed that both groups reported a high degree of patient involvement and appreciated being heard and understood by the audiologist. These findings suggest that the synchronous mode could effectively be included as a complement to AR, although more research is needed to explore the potential advantages and disadvantages of addressing the individual needs of HA users synchronously in their everyday lives.
Supplemental Material
Download MS Word (28.6 KB)Acknowledgments
The authors thank the participants in this study and the clinicians and operation managers at the Hearing Organization, VRG, Sweden. The authors are also grateful to Maria Hoff for her valuable input when planning this study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Angley, P., J. E. Schnittker, and A. M. Tharpe. 2017. “Remote Hearing Support: The Next Frontier.” American Academy of Audiology 28 (10):893–900.
- Barbour, D. L., R. T. Howard, X. D. Song, N. Metzger, K. A. Sukesan, J. C. DiLorenzo, B. R. D. Snyder, J. Y. Chen, E. A. Degen, J. M. Buchbinder, et al. 2019. “Online machine learning audiometry.” Ear & Hearing 40 (4):918–926. doi:10.1097/AUD.0000000000000669.
- Bennett, R. J., C. Barr, J. Montano, R. H. Eikelboom, G. H. Saunders, M. Pronk, J. E. Preminger, M. Ferguson, B. Weinstein, E. Heffernan, et al. 2021. “Identifying the approaches used by audiologists to address the psychosocial needs of their adult clients.” International Journal of Audiology 60 (2):104–114. doi:10.1080/14992027.2020.1817995.
- Bennett, R. J., A. Laplante-Lévesque, M. Carly, and R. H. Eikelboom. 2018. “Exploring Hearing Aid Problems: Perspectives of Hearing Aid Owners and Clinicians.” Ear & Hearing 39 (1):172–187. doi:10.1097/AUD.0000000000000477.
- Brännström, K. J., K. Andersson, O. Sandgren, and S. Whitling. 2020. “Clinical Application and Psychometric Properties of a Swedish Translation of the Abbreviated Profile of Hearing Aid Benefit.” Journal of the American Academy of Audiology 31 (09):656–665.
- Convery, E., G. Keidser, L. Hickson, and C. Meyer. 2019. “Factors associated with successful setup of a self-fitting hearing aid and the need for personalized support.” Ear & Hearing 40 (4):794–804. doi:10.1097/AUD.0000000000000663.
- Cox, R. 1997. “Administration And Application of the APHAB.” The Hearing Journal 50 (4):32–48. doi:10.1097/00025572-199704000-00002
- Cox, R., and G. Alexander. 1995. “Abbreviated Profile of Hearing Aid Benefit.” Ear & Hearing 16 (2):176–186. doi:10.1097/00003446-199504000-00005
- Cox, R., M. Hyde, S. Gatehouse, W. Noble, H. Dillon, R. Bentler, and L. Hallberg. 2000. “Optimal Outcome Measures, Research Priorities, and International Cooperation.” Ear & Hearing 21 (4):106–115.
- Dillon, H., J. Day, B. Bant, and K. J. Munro. 2020. “Adoption, use and non-use of hearing aids: a robust estimate based on Welsh national survey statistics.” International Journal of Audiology 59 (8):567–573. doi:10.1080/14992027.2020.1773550.
- Eksteen, S., S. Launer, H. Kuper, R. H. Eikelboom, A. Bastawrous, and D. W. Swanepoel. 2019. “Hearing and vision screening for preschool children using mobile technology, South Africa.” Bulletin of the World Health Organization 97 (10):672–680. doi:10.2471/BLT.18.227876.
- Estancial Fernandes, C. S., M. G. Lima, and M. B. A. Barros. 2019. “Emotional problems and health-related quality of life: population-based study.” Quality of Life Research : An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation 28 (11):3037–3046. doi:10.1007/s11136-019-02230-9.
- Ferguson, M. A., D. W. Maidment, R. Gomez, N. Coulson, and H. Wharrad. 2021. “The feasibility of an m-health educational programme (m2Hear) to improve outcomes in first-time hearing aid users.” International Journal of Audiology 60 (sup1):S30–S41. doi:10.1080/14992027.2020.1825839.
- Glista, R., R. O'Hagan, S. Moodie, and S. Scollie. 2021. “An examination of clinical uptake factors for remote hearing aid support: a concept mapping study with audiologists.” International Journal of Audiology 60 (sup1):S13–S22.
- Gomez, R., A. Habib, D. W. Maidment, and M. A. Ferguson. 2022. “Smartphone-Connected Hearing Aids Enable and Empower Self-Management of Hearing Loss: A Qualitative Interview Study Underpinned by the Behavior Change Wheel.” Ear & Hearing 43 (3):921–932. doi:10.1097/AUD.0000000000001143.
- Goswami, A., and S. Dutta. 2016. “Gender Differences in Technology Usage—A Literature Review.” Open Journal of Business and Management 04 (01):51–59. doi:10.4236/ojbm.2016.41006.
- Gotowiec, S., J. Larsson, P. Incerti, T. Young, K. Smeds, F. Wolters, P. Herrlin, and M. Ferguson. 2022. “Understanding patient empowerment along the hearing health journey.” International Journal of Audiology 61 (2):148–158. doi:10.1080/14992027.2021.1915509.
- Hickson, L., C. Meyer, K. Lovelock, M. Lampert, and A. Khan. 2014. “Factors associated with success with hearing aids in older adults.” International Journal of Audiology 53 (sup1):S18–S27. doi:10.3109/14992027.2013.860488.
- Houmøller, S. S., A. Wolff, S. Möller, V. K. Narne, C. S. Narayanan, K. Godballe, D. D. Hougaard, G. Loquet, M. Gaihede, D. Hammershøi, et al. 2022. “Prediction of successful hearing aid treatment in first-time and experienced hearing aid users: Using the International Outcome Inventory for Hearing Aids.” International Journal of Audiology 61 (2):119–129. doi:10.1080/14992027.2021.1916632.
- Kokkonen, J., H. Kaski, S. Mäkinen, and F. Svärd. 2022. “Remote hearing aid renewal using pre-existing audiograms during the covid-19 pandemic.” International Journal of Audiology. doi:10.1080/14992027.2022.2082329. Online ahead of print.
- Malmberg, M., K. Anióse, J. Skans, and M. Öberg. 2022. “A randomised, controlled trial of clinically implementing online hearing support.” International Journal of Audiology. doi:10.1080/14992027.2022.2059712. Online ahead of print.
- Malmberg, M., T. Lunner, K. Kähäri, and G. Andersson. 2017. “Evaluating the short-term and long-term effects of an internet-based aural rehabilitation programme for hearing aid users in general clinical practice: a randomised controlled trial.” BMJ Open 7 (5):e013047. doi:10.1136/bmjopen-2016-013047
- Malmberg, M., E. Sundewall Thorén, M. Öberg, T. Lunner, G. Andersson, and K. Kähäri. 2018. “Experiences of an Internet-Based Aural Rehabilitation (IAR) Program for Hearing Aid Users: A Qualitative Study.” International Journal of Audiology 57 (8):570–576. doi:10.1080/14992027.2018.1453171.
- Muñoz, K., N. K. Nagaraj, and N. Nichols. 2021. “Applied tele-audiology research in clinical practice during the past decade: a scoping review.” International Journal of Audiology 60 (sup1):S4–S12. doi:10.1080/14992027.2020.1817994.
- Newman, C. W., B. E. Weinstein, G. P. Jacobson, and G. A. Hug. 1990. “The Hearing Handicap Inventory for adults; psychometric adequacy and audiometric correlates.” Ear and Hearing 11 (6):430–433. doi:10.1097/00003446-199012000-00004.
- Parmar, B. J., K. Mehta, D. A. Vickers, and J. K. Bizley. 2021. “Experienced hearing aid users’ perspectives of assessment and communication within audiology: a qualitative study using digital methods.” International Journal of Audiology 61 (11): 956–964.
- Penteado, S. P., R. F. Bento, L. R. Battistella, S. M. Silva, and P. Sooful. 2014. “Use of the satisfaction with amplification in daily life questionnaire to assess patient satisfaction following remote hearing aid adjustments (telefitting).” Journal of Medical Internet Research, Medical Informatics 2 (2):e18.
- Petry, T., S. N. Santos, and M. J. Costa. 2010. “Speech recognition according to the length of hearing aid use.” Brazilian Journal of Otorhinolaryngology 76 (4):462–468. doi:10.1590/S1808-86942010000400010.
- Picou, E. M. 2010. “MarkeTrak 10 (MT10) Survey Results Demonstrate High Satisfaction with and Benefits from Hearing Aids.” Seminars in Hearing 41 (1):21–36.
- Pross, S. E., A. L. Bourne, and S. W. Cheung. 2016. “TeleAudiology in the Veterans Health Administration.” Otology & Neurotology 37 (7):847–850. doi:10.1097/MAO.0000000000001058
- Scholl, I., J. M. Zill, M. Harter, and J. Dirmaier. 2014. “An integrative model of patient-centeredness - a systematic review and concept analysis.” Public Library of Science One 9 (9):e107828.
- Tao, K. F. M., T. C. Moreira, D. M. P. Jayakody, D. W. Swanepoel, C. G. Brennan-Jones, L. Coetzee, and R. H. Eikelboom. 2021. “Teleaudiology hearing aid fitting follow-up consultations for adults: single blinded crossover randomised control trial and cohort studies.” International Journal of Audiology 60 (sup1):S49–S60. doi:10.1080/14992027.2020.1805804.
- van Lente, H. 2012. “Navigating foresight in a sea of expectations: lessons from the sociology of expectations.” Technology Analysis & Strategic Management 24 (8):769–782. doi:10.1080/09537325.2012.715478.
- Ventry, I. M., and B. E. Weinstein. 1982. “The Hearing Handicap Inventory for the elderly: a new tool.” Ear & Hearing, 3 (3):128–134. doi:10.1097/00003446-198205000-00006.
- Weinstein, B. E., J. B. Spitzer, and I. M. Ventry. 1986. “Test-retest reliability of the Hearing Handicap Inventory for the Elderly.” Ear & Hearing 7 (5):295–299. doi:10.1097/00003446-198610000-00002
