Abstract
Objective
To investigate the effect of hearing aid (HA) intervention on long-term health-related quality of life (HRQoL) changes in first-time and experienced HA users using the 15D questionnaire. Secondly, the study explored the relationship between clinical parameters and changes in 15D scores.
Design
A prospective observational study.
Study sample
The study population included 1562 patients (1113 first-time and 449 experienced HA users) referred for HA rehabilitation. All patients responded to the 15D at baseline, two months after HA fitting, and at long-term follow-up (698 ± 298 d).
Results
Among both first-time and experienced HA users, significant improvements in hearing-dimension (15D-3) score were observed at two-month follow-up which sustained at long-term follow-up. 15D total scores significantly decreased at long-term follow-up. Self-reported hearing abilities, word recognition scores, and HA use time were significantly and positively correlated to increased 15D.
Conclusions
Both groups of HA users reported improved hearing-related QoL after HA treatment which sustained at long-term follow-up but the improvement in total 15D total score did not sustain for either group. The results suggest that HA intervention positively affects hearing-related QoL among older adults with hearing loss, and the findings support the use of 15D as a tool for the evaluation of HA treatment effects.
Introduction
Outcome measures in hearing aid (HA) research are traditionally based on audiometric and perceived hearing outcomes. However, in the last decades, a focus on health-related quality of life (HRQoL) has been increasing to provide a more holistic measure of the benefit of HA rehabilitation. The HRQoL assessment “examines the degree to which people’s health status affect their self-perception of daily functioning and well-being” (Chisolm et al. Citation2007, 154). A driving force for the shift in focus has been facilitated by health economics to quantify treatment benefits in relation to its costs, using cost-utility analysis. Utility scores are used to estimate HRQoL and to define the net cost of treatments over the net effect in quality-adjusted life years (QALYs) over time. A widely distributed, and relatively low-cost, treatment such as HAs could effectively be evaluated through a process of cost-effectiveness. No instruments to evaluate benefits or utility treatment outcomes are used as a standard, neither in the Danish audiological health care system nor internationally. Studies that evaluate HA outcomes have done so with disease-specific measurements and have shown significant improvements of HA treatment on speech intelligibility, listening effort, and cognitive abilities (Cox et al. Citation2011). Some commonly used disease-specific instruments with a focus on hearing and communication include the International Outcome Inventory for Hearing Aids (IOI-HA, Cox et al Citation2000) and the Abbreviated Profile for Hearing-Aid Benefit (APHAB, Cox and Alexander Citation1995). Disease-specific measures are highly responsive to an intervention designed for a particular disease (Patrick and Deyo Citation1989) but lack the ability to establish the cost-utility of HA treatment, and hence the ability to compare the effects of HA treatment against treatments in other medical fields. The results of hearing-related studies using generic HRQoL measures vary (Tseng et al. Citation2018). This is perhaps because most generic HRQoL measures do not include questions related to hearing and oral communication (Abrams, Chisolm, and McArdle Citation2005). Some common generic HRQoL instruments used in hearing-related research include: The “36-item Short-Form health survey” (SF-36, Scoggins and Patrick Citation2009); the Health Utilities Index Mark 3 (HUI-3, Horsman et al. Citation2003); and the EuroQoL 5-dimensions (EQ-5D, EuroQoL Group Citation1990). The major shortcoming of SF-36 is the lack of finesse to evaluate the patient in hearing-related therapies (Crandell Citation1998). Additionally, SF-36 lacks a health utility score, which makes this instrument unsuitable for calculating QALYs. In relation to the EQ-5D, a systematic review assessing the responsiveness across various conditions reported that the instrument has poor to moderate responsiveness to clinical changes (Tordrup, Mossman, and Kanavos Citation2014). It is therefore less suitable for measuring the improvement of HRQoL over a brief period. The HUI-3 lacked a validated Danish version including health utility scores in a Danish context. In a recent systematic review including 14 studies on hearing impairment and quality of life among older adults, the majority of the studies (13 out of 14) identified hearing impairment to be associated with poorer quality of life, while one study observed the same trend, but the association did not reach the statistically significant level (Tay et al. Citation2007). Three of the 13 studies suggested that hearing impairment is only associated with certain dimensions of QoL, namely the vitality domain (Wong and Cheng Citation2012), social functioning domain (Fischer et al. Citation2009), physical and social domains (Zhang et al. Citation2016).
The 15D is a standardized, generic, self-administered measure of HRQoL (Sintonen and Richardson Citation1994). It can be used both as a profile and a single index score which enables the calculation of QALYs (Sintonen and Richardson Citation1994). Theoretical and empirical evidence suggests that 15D has good discriminatory power and responsiveness to change in health status (Michel, Augestad, and Rand Citation2018; Sintonen Citation2001). The questionnaire was originally developed in Finnish and validated in a Danish version according to the standards described in the validation system (15D-instrument.net). In conjunction with the validation, modelling of the Danish weights has been carried out to obtain the health utility scores in a Danish context (Wittrup-Jensen and Pedersen Citation2008). The 15 dimensions include mobility, vision, hearing, breathing, sleeping, eating, speech, excretion, usual activities, mental functioning, discomfort or pain, depression, distress, vitality, and sexual activity. Each dimension has one question with five response categories. The 15D score is generated based on a set of utility weights over all 15 dimensions. The maximum score is 1 (no problems) and the minimum score is 0 (being dead) (Sintonen Citation2001). To facilitate the clinical interpretation of the 15D scores, Alanne et al. (Citation2015) applied a subjective five-category global assessment scale (GAS) to estimate a minimum important change (MIC) in the 15D total score which they found to be ±0.015. The GAS categories included: (1) much better, (2) slightly better, (3) no change, (4) slightly worse, and (5) much worse.
The 15D includes a question related to hearing which distinguishes the 15D from other generic instruments used. It has previously been used within the audiological field, especially in the evaluation of potential changes in HRQoL following cochlear implantation (Carter and Hailey Citation1999). Additionally, the 15D was used in a Finnish study measuring the change in HRQoL from baseline to six months following HA fitting (Niemensivu et al. Citation2015). The study population (n = 949) was adults with symmetric hearing losses that had been unilaterally fitted with HAs, which at the time was a common procedure in the Finnish health care system. Mean positive changes in the hearing dimension of 15D (Δ15D-3 = 0.208, p < 0.001) and marginal mean improvement in the total 15D score (Δ15D = 0.006) was reported. Furthermore, a decrease in the dimension of mobility (15D-1 = −0.01, p = 0.028) and sexual activity (15D-15 = −0.025, p < 0.001) was observed. They concluded that significant changes were found only in the hearing and sexual activity dimension. The study demonstrated the applicability of the 15D instrument in HA research but stressed the necessity of more studies and a larger sample size to demonstrate the effects of HAs on generic HRQoL assessed with the 15D. An important limitation of the study was the 96% unilaterally fitted patients, which does not reflect the clinical practice of most countries worldwide providing bilateral HA fittings (Boymans et al. Citation2008).
The purpose of the current study was to evaluate the short and long-term effects of HA intervention on HRQoL measured with the 15D in a Danish cohort of adults fitted with HAs. In addition, the relationship between changes in HRQoL and clinical parameters such as the degree of hearing loss, word recognition score (WRS), self-reported hearing abilities, and average daily HA use time were investigated.
Materials and methods
Study design and participants
The study was part of the Danish national project “Better hEAring Rehabilitation” (BEAR, www.bear-hearing.com; Houmøller et al. Citation2022; Narayanan et al. Citation2023; Wolff Citation2019) and designed as a prospective observational study. Ethical approval for the project (S-20162000-64) was not warranted from The Regional Committees on Health Research Ethics for Southern Denmark.
A total of 2447 adults (≥18 yrs) referred for HA treatment were recruited at the Departments of Audiology at Odense University Hospital (OUH), Region of Southern Denmark and Aalborg University Hospital (AAUH), North Denmark Region, and the study population consisted of both first-time and experienced HA users referred for HA treatment. The experienced HA users had at least four years of HA experience. All patients were referred to one of the two Departments of Audiology by their Ear-Nose-Throat (ENT) specialist. At AAUH, the first-time HA users were sent an invitation to participate in the study two weeks before their scheduled visit at the clinic. At OUH, the patients were informed of the study and invited to participate directly by their ENT specialist. Acceptance to participate was received from 1961 patients and was noted in the referral letter to the department. All patients received information on study details, a consent form, and a letter on the patient’s rights related to study participation in their private digital mailbox (e-boks). Patients were excluded if they were offered alternative treatment (e.g. cochlear implants), or if they were not able to fill out the questionnaires. Four hundred eighty-six patients declined the initial HA treatment, was excluded, or discontinued treatment before the two-month follow-up, but the reasons for drop-out was not systematically recorded.
Questionnaires
A questionnaire survey was administered before the initial audiological assessment (baseline), two months following the HA fitting, and at long-term follow-up (more than one year after the HA fitting). The survey included the 15D, the abbreviated version of the Speech, Spatial, and Qualities of Hearing Scale (SSQ12) (Gatehouse and Noble Citation2004; Noble et al. Citation2013), and a non-standardised health-related questionnaire providing demographic details on age, sex, motivation, and HA experience that was only administered at baseline. Data were collected and managed using Research Electronic Data Capture (REDCap) tools hosted at Odense Patient Explorative Network (OPEN) in the Region of South Denmark (Harris et al. Citation2009, Citation2019). Responses were stored into the database through an online link generated by REDCap that was sent to their e-boks. A paper-and-pencil version was also available at the clinic if necessary. Responses from paper versions were manually entered into the database by research assistants.
Audiological assessment
The audiological assessment was carried out by the experienced staff at the two Audiological Departments. The procedure followed the standard protocol exerted by audiological clinics in Denmark when assessing hearing loss and subsequently fitting HAs. All patients underwent a standard pure tone- and speech audiometry conducted in a soundproof booth. Air- and bone conduction thresholds were measured according to ISO 8253-1:Citation2010 (International Organisation for Standardisation). Masking was used accordingly. TDH39 headphones or ER-3A insert earphones were used during the test. The WRS were assessed with the validated, phonetically balanced, monosyllabic word list in Danish, DANTALE I (Elberling et al. Citation1989). The measurement was conducted with headphones in the quiet and administrated sequentially to each ear separately with masking noise in the contralateral ear. The score is expressed in the percentage out of 25 correct repeated words. The initial audiological assessment also included a detailed medical and audiological case history.
Patients were fitted with HAs from one of the three manufacturers participating in the BEAR project. To avoid bias from a skewed HA representation, each patient was randomised to HAs from one of the three manufacturers using simple randomisation. If the given HA brand was not found suitable, an alternative HA model was found from the tender according to standard clinical practice in Denmark. The choice of the HA model was typically based on individual work-related and/or recreational listening needs as well as needs for manual adjustments (e.g. volume control, switch between programs for different sound environments, and telecoil). The distribution of HAs among the three manufacturers was: 30.5% Oticon; 29.1% GN Hearing; 27.5% Widex-Sivantos; and 12.9% from other brands.
Hearing-Aid fitting
The HAs were fitted according to the proprietary fitting algorithm suggested by the specific HA manufacturer which is part of standard clinical practice in Denmark. Only a small percentage (3%) were fitted with generic fitting algorithms (e.g. NAL-NL1, NAL-NL2 (Keidser et al. Citation2011)). Acceptance of loud and high pitch noises was tested as part of standard practice (e.g. dropping a set of keys on a table or rattling a spoon in an empty glass). Fine-tuning of the HAs were conducted if the patient experienced intolerable loudness discomfort with the HAs or other issues related to the sound amplification. Validation via probe microphone measurements was not completed as it is not standard clinical practice in Denmark. However, information was given about self-adjustment of volume and program options, if applicable. The patients were informed of an expected HA acclimatisation period but were instructed to schedule an additional visit at the hearing clinic if the fitting prevented HA habituation. The HAs were fitted one-and-a-half months (mean, SD (days): 44 ± 23) after the initial audiological assessment. A subsequent follow-up visit was scheduled two months following the HA fitting in which the average daily HA use time was extracted from the data logging in the fitting software. Furthermore, the HA fitting was registered through real-ear measurements at three sound pressure levels and in later analyses compared to universal targets (incl. the NAL-NL2) as reported in Narayanan et al. (Citation2023).
Data analysis
The better hearing ear threshold and severity of hearing loss were calculated using the pure-tone average (PTA-4) across the frequencies 0.5, 1, 2, and 4 kHz. The hearing threshold severity categories were defined using the Global Burden of Disease (GBD) classification (Shield Citation2019; Stevens et al. Citation2013) and included the categories: normal (<20 dB hearing level [HL]); mild (20–34 dB HL); moderate (35–49 dB HL); moderate-severe (50–64 dB HL); severe (65–79 dB HL), and profound (>81 dB HL). Due to a low representation within the “severe” (35 patients) and “profound” (7 patients) HL groups, these two groups were merged into one group. The characteristics of the study population were examined using descriptive statistics including means, ranges, standard deviations, 95% confidence intervals, and percentages.
Significant differences in individual 15D dimension scores and 15D total score from baseline to two-month follow-up and from baseline to long-term follow-up in first-time and experienced HA users were assessed using mixed models. The numeric change in the 15D-3 and total 15D scores was interpreted using the GAS categories (Alanne et al. Citation2015). The GAS intervals for classifying the changes of 15D scores are: >0.035 (much better); 0.015 − 0.035 (slightly better): ±0.015 (no change); −0.035 to −0.015 (slightly worse); and < −0.035 much worse.
Two sets of mixed model analyses were applied to explore the correlates of the 15D total score and 15D-3 hearing dimension score in first-time and experienced HA users. 15D total score and 15D-3 hearing dimension score were analysed as outcome according to HA experience (first-time and experienced) in separate models. All models were additionally adjusted for age, sex, measurement time point, baseline SSQ12 total score, best ear WRS, best ear PTA-4 threshold, and daily HA use time. Patients’ identification number was included into the model as a random effect to account for multiple measurements for the same individual. All analyses were performed using STATA SE version 17.0 (Stata Corp., College Station, TX).
Results
The 15D epidemiology
In total, 1894 patients responded the 15D questionnaire at baseline including first-time (n = 1362) and experienced (n = 532) HA users. shows the study flow of the two groups of HA users responding to the 15D questionnaire at the three measurement time points (baseline, two-month follow-up, and long-term follow-up). In average, the two-month follow-up 15D responses were received 71 (±32) days after HA fitting and the long-term follow-up responses were received 698 (±298) days after HA fitting. describes the population characteristics among first-time (mean age: 65.9 ± 10.9 years) and experienced users (mean age: 67.7 ± 11.5 years). Experienced users had on average 9.6 years of HA experience. The mean PTA-4 thresholds in the better ear were 32.1 ± 10.9 dB HL and 43.6 ± 14 dB HL in first-time and experienced users, respectively. According to the GBD categories, mild hearing loss was the most frequent type of hearing loss among the first-time users whereas moderate hearing loss was the predominant type of hearing loss among the experienced users.
Figure 1. Study flow diagram according to hearing aid (HA) experience and measurement point (baseline, two-month follow-up, and long-term (>1Y) follow-up).
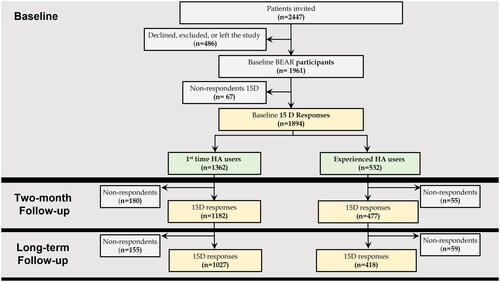
Table 1. Patient characteristics according to hearing aid (HA) experience at baseline.
Comparison of the 15D dimension scores and total score before and after HA intervention in first-time and experienced HA users
summarises 15D-3 scores and total scores for first-time and experienced HA users at baseline, two-month, and long-term follow-up. Compared to baseline, the hearing dimension score (15D-3) increased significantly for both first-time and experienced HA users at two-month follow-up and at a lower level at long-term follow-up (β [95%CI] at 2-month/long-term for first-time HA users: 0.10 [0.09, 0.11]/0.09 [0.08, 0.10]; for experienced HA users: 0.08 [0.06, 0.10]/0.06 [0.04, 0.08]). The 15D total score increased significantly at the two-month follow-up but decreased again significantly to below baseline level at the long-term follow-up, a trend that was observed in both groups of HA users (β [95% CI] at 2-month/long-term follow-up for first-time HA users: 0.006 [0.003, 0.009]/−0.004 [−0.007, −0.001]; for experienced HA users: 0.08 [0.06, 0.10]/0.06 [0.04, 0.08]).
Table 2. Mean 15D dimension scores and total score at baseline, two-month follow-up, and long-term follow-up according to hearing aid (HA) experience.
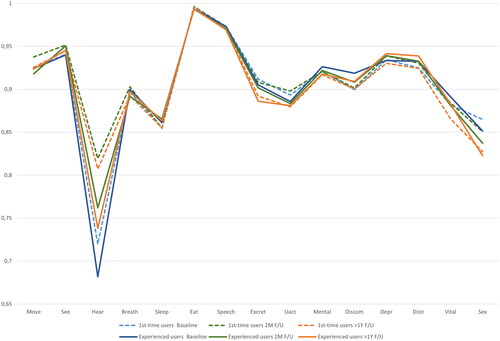
shows the change in the 15D dimension scores including the hearing dimension (15D-3) from baseline to two-month follow-up and from baseline to long-term follow-up. Besides the hearing dimension, first-time HA users also exhibited significant improvement in the mobility and sexual activity dimension score at two-months follow-up and a decline in the depression dimension score. For both groups of HA users, a significant decline in excretion, usual activities, vitality, and sexual activity was observed at long-term follow-up.
Figure 2. 15D Individual dimension scores at baseline, two-month, and long-term (>1Y) follow-up (F/U). Move: mobility; See: vision; Hear: hearing; Breath: breathing; Sleep: sleeping; Eat: eating; Excret: excretion; Uact: usual activities; Mental: mental function; Discom: discomfort; Depr: depression; Distr: distress; Vital: vitality; Sex: sexual activity.
presents the changes in the 15D total score from baseline to two-month follow-up and from baseline to long-term follow-up classified into the GAS categories and the distribution of patients into these categories. According to this classification, the results show that up to 20% of the first-time users and 16% of the experienced users reported much better QoL following HA treatment at both two-month and long-term follow-up. Approximately 40% of the first-time users and 36% of the experienced users reported no change in QoL two months following HA fitting. At long-term follow-up, this number dropped to 34% of first-time and experienced users. Approximately 25%–35% of the first-time users and 35%–38% of the experienced users reported slightly worse to much worse QoL at two-month and long-term follow-up, respectively.
Table 3. Classification of the change in 15D total scores from baseline to two-month and long-term follow-up into global assessment scale (GAS) categories according to hearing aid experience.
Change in 15D total score and 15D-3 hearing dimension score
Results from mixed models () showed that the 15D total score increased significantly by 0.006 (95% CI: [0.003; 0.009], p = 0.01) scale points at the two-month follow-up among first-time HA users only, whereas at the long-term follow-up, the 15D total scores significantly decreased for both groups of HA users by −0.004 (95%CI: [−0.007; −0.001], p < 0.001) scale points and −0.01 (95% CI: [−0.012; −0.002], p < 0.001) respectively, compared to baseline 15D total scores. On the other hand, the hearing dimension (15D-3) scores increased at the two-month follow-up for both groups of HA users by 0.102 (95% CI: [0.09; 0.11], p < 0.001) scale points and 0.085 (95% CI: [0.07; 0.10], p < 0.001) scale points, respectively. At the long-term follow-up, the 15D-3 scores increased by 0.090 (95% CI: [0.08; 1.02], p < 0.001) scale points among first-time users and 0.059 (95% CI: [0.04; 0.08], p < 0.001) among the experienced users.
Table 4. Correlates of 15D total score and 15D-3 hearing dimension score in first-time and experienced hearing aid (HA) users.
With regards to the clinical parameters, as seen in , an increase of one scale point of the SSQ12 baseline total score increased the 15D total scores by 0.014 (95% CI: [0.01;0.02]) for first-time users and 0.01 (95% CI: [0.008–0.016]) for experienced users. This means that a higher SSQ12 score at baseline correlates with a higher 15D scores. Likewise, an increase in WRS along with an increase in the data logged HA use time were also significantly correlated with increased 15D total scores in both groups of HA users. The hearing dimension (15D-3 scores) were significantly correlated and positively influenced by an increase in SSQ12 total scores at baseline, higher WRS at baseline, lower PTA-4 thresholds at baseline and increased HA use time in first-time users. Among the experienced users, only an increase in baseline SSQ12 total scores and lower PTA-4 thresholds were significantly related to an increase in 15D-3 scores.
Discussion
Effects of hearing aid treatment on 15D-3 hearing dimension score and 15D total score
This study quantifies hearing-related improvements in HRQoL following HA intervention in first-time and experienced HA users measured by 15D. Hearing loss in old age has been associated with depression, withdrawal from activities, and social interaction (Crews and Campbell Citation2004; Mener et al. Citation2013; Mikkola, Portegijs, et al. Citation2015) which can lead to mobility decline (Mikkola, Polku, et al. Citation2015; Polku et al. Citation2015). In the current study, a significant improvement in the hearing dimension score (15D-3) was observed in both groups of HA users at a two-month follow-up, and the improvement sustained in long-term follow-up when compared to baseline scores. It might seem surprising that the experienced users already using HAs reported an improvement, but this could be due to an experienced user experiences the subtle differences in technology between a previous older model and a newer model built on more advanced technology. The results show a positive treatment effect of hearing rehabilitation on HRQoL related to the hearing dimension, which is sustained during an average of almost two years follow-up period. Our findings correspond with a recent systematic review including 29 studies, which concluded that hearing rehabilitation has a positive impact on the quality of life after hearing loss (Brodie, Smith, and Ray Citation2018).
We observed a slight decrease in hearing dimension score (15D-3) from two-month to long-term follow-up in both groups of HA users that might be related to two different aspects. This could be due to the “honey-moon” effect which is a well-known phenomenon within HA rehabilitation related to arousal when realising the improvement in the first months after HA fitting (Ivory et al. Citation2009; Malinoff and Weinstein Citation1989).
When comparing the changes in 15D-3 scores between the two groups of HA users, it is evident that the experienced users reported less improvement in hearing-related QoL from baseline to two-month follow-up compared to the first-time users. This could be due to the HA habituation effect is less evident in experienced users due to previous HA use. The long-term effect of HA treatment on QoL is also less evident among the experienced users. On the other hand, the overall 15D total score, which summarises 15 dimensions with different weightings, showed an improvement in HRQoL after HA fitting (at the two-month follow-up) in first-time HA users but declined significantly at long-term follow-up for both groups of HA users. However, the magnitude of improvement seen in the 15D total score at the two-month follow-up was below the clinically significant threshold (±0.015) proposed by Alanne et al. (Citation2015). The decline in 15D total score at long-term follow-up was evident along with a significant decline in excretion, usual activities, vitality, and sexual activity at long-term follow-up for both groups of HA users. These findings are consistent with previous studies that showed QoL decline notably after age 75 years in the general population, especially in older adults with hearing disabilities (Ciorba et al. Citation2012; Hogan et al. Citation2009). Our results could indicate that the improvement in the hearing dimension may not be enough to overcome the impact of other health issues on other dimensions, which may play an important role in overall HRQoL among older adults. In a Finnish study, musculoskeletal disorders followed by psychiatric conditions were associated with the largest decline in HRQoL (Saarni et al. Citation2006). Thus, we speculate that other important dimensions are driving the decline in HRQoL. It is important to note that outside the scope of the 15D questionnaire, HRQoL in older adults have been found to be associated with a wide range of demographic and psychosocial factors (Etxeberria, Urdaneta, and Galdona Citation2019) including older age, female sex (Gallicchio, Hoffman, and Helzlsouer Citation2007; Tajvar, Arab, and Montazeri Citation2008), low socio-economic status (Tajvar, Arab, and Montazeri Citation2008), the presence of depressive symptoms (Gouveia et al. Citation2017; Sivertsen et al. Citation2015), and living alone (Gouveia et al. Citation2017; Hawton et al. Citation2011). Therefore, future studies are warranted to investigate the relationship between hearing loss and HRQoL by taking a wider range of covariates into consideration.
The effect of clinical parameters on changes in 15D-3 and 15D total score
The fact that self-reported baseline hearing disabilities were significantly associated with QoL changes (in 15D-3 and 15D total score) in both groups of HA users is consistent with the results from Niemensivu et al. (Citation2015). In contrast, the PTA-4 levels were not significantly related to the overall QoL which is in line with previous research that found the perceived hearing disabilities are a stronger predictor of changes in HRQoL in older adults (assessed using SF-36) compared to the degree of hearing loss (Gopinath et al. Citation2012). Thus, perceived hearing disabilities is shown to be of greater importance for successful hearing rehabilitation than the magnitude of the hearing loss assessed with pure-tone audiometry (Vestergaard Knudsen et al. Citation2010). However, PTA-4 was negatively associated with hearing-related QoL (15D-3) which seems reasonable, as a more severe hearing loss is suspected to negatively affect the QoL to a greater extent than a mild hearing loss. The ability to discriminate words in quiet was positively related to QoL in both groups of HA users, whereas the hearing-related QoL was only positive associated with WRS among the first-time users. It is possible that better speech intelligibility improves the QoL as this is related to the ability to communicate. Using the HAs more hours per day also showed to increase the overall QoL in both groups. Overall, these results indicate that the above-mentioned clinical parameters can also modestly affect QoL changes in older adults with hearing loss.
Clinical utility and weighting of the 15D questionnaire
Using the GAS classification as a clinical interpretation of the changes in the 15D total score revealed that 35% (one-third) of the first-time users and 29% (less than one-third) of the experienced users perceived improved QoL after HA treatment, and the improvement was maintained at long-term follow-up. These findings support the clinical procedures of HA intervention for older adults with hearing loss, and the results suggest that the provision of HAs positively affects their overall HRQoL. However, 25% (one-fourth) of the first-time users and 35% of the experienced users reported worse QoL at the two-month follow-up which increased to 34% and 38% of the first-time and experienced users, respectively at the long-term follow-up. These findings could indicate that the patients experience increasing health issues as part of the ageing process which impacts their HRQoL.
It is worth noting that the 15 dimensions have a weighted score attached to each of the single dimensions according to the impact on the overall QoL, which is called a utility weight. In the Danish weighting of the 15 dimensions, the hearing dimension is placed as number eleventh, only weighted higher than excretion, distress, vision, and sexual activity (Wittrup-Jensen and Pedersen Citation2008). In the Norwegian and Finnish weightings, the hearing dimension is placed fourteenth (Michel, Augestad, and Rand Citation2018), having a larger impact on the total 15D score than sexual activity (in the Norwegian version) or vision (in the Finnish version). The mental dimension of 15D is weighted highest in both the Danish, Finnish, and Norwegian utility system. Thus, the score in the 15D-3 needs to change relatively more than, e.g. the mental dimension, to have an impact on the total HRQoL. Regardless of this, the 15D instrument might still be the most sensitive and comprehensive HRQoL measure presently available for use in hearing research because it combines the advantages of a profile measure and a single (total) index score measure (Michel, Augestad, and Rand Citation2018). It also provides a new valid set of health state valuations for further QALY measurements in cost-utility analysis. Future studies should investigate the cost-benefit of improvements in QoL following HA rehabilitation.
Strengths and limitations
The large study population and comprehensive amounts of data collected for each patient were the main advantages to this study. However, some limitations still apply. Using real-ear measurement to verify the HA fitting is not part of current clinical practice in Denmark which can be considered a limitation to the study as it might have affected the changes in HRQoL measured with the 15D. Real-ear measurements were however obtained at the two-month follow-up to compare the fitting to NAL-NL2. Narayanan et al. (Citation2023) showed that deviation from the target had no influence on reported outcome in first-time users and only a small effect in experienced users analysing the IOI-HA Factor 1 scores. Also, due to the recruitment strategy, the experienced users were all in need of re-fitting, hence they were not random experienced users and this might be considered as a strength of the study.
Patients most affected by their hearing loss might have turned down the invitation due to lack of mental excess to participate and those less satisfied with their HAs might be less likely to accept the invitation and complete the questionnaires. This could cause an error in the estimation of the positive impact of HA treatment on HRQoL. Furthermore, the study does not include an untreated control group with and without hearing loss. Therefore, we can only speculate that the reason for the long-term decline in dimensions such as excretion, usual activities, vitality, and sexual activity as well as hearing may be due to ageing in the study population.
Conclusion
The current study showed an improvement in the hearing-related QoL following HA intervention in first-time and experienced users, and the improvement was maintained at long-term follow-up. The overall HRQoL improved among first-time HA users at two-month follow-up only and declined significantly at long-term follow-up for both groups of HA users. It was evident that there is an important difference of using the single dimension score versus the overall 15D score. Using long-term changes in the 15D as an index score (15D total) may reflect the ageing process whereas using the profile score (15 dimensions) more clearly reveals aspects of hearing rehabilitation. The results from our study support the prescription of HAs as a clinical intervention for older adults with hearing loss. In addition, our finding supports the use of 15D to evaluate the treatment effect of hearing rehabilitation.
Acknowledgements
Collaboration and support by Innovation Fund Denmark (Grand Solutions 5164-00011B), Oticon, GN Hearing, Widex-Sivantos Audiology, and other partners (Aalborg University Hospital, Odense University Hospital, University of Southern Denmark, Aalborg University, Technical University of Denmark, FORCE Technology, and Copenhagen University Hospital) are sincerely acknowledged. The authors would like to give special thanks to the study participants and the staff at the Departments of Audiology at AAUH and OUH. Also, thanks to Harri Sintonen for his support in using the 15D questionnaire.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Abrams, H. B., T. H. Chisolm, and R. McArdle. 2005. “Health-Related Quality of Life and Hearing Aids: A Tutorial.” Trends in Amplification 9 (3): 99–109. doi:10.1177/108471380500900302.
- Alanne, S., R. P. Roine, P. Räsänen, T. Vainiola, and H. Sintonen. 2015. “Estimating the Minimum Important Change in the 15D Scores.” Quality of Life Research 24 (3):599–606. doi:10.1007/s11136-014-0787-4.
- Boymans, M., S. Theo Goverts, S. E. Kramer, J. M. Festen, and W. A. Dreschler. 2008. “A Prospective Multi-Centre Study of the Benefits of Bilateral Hearing Aids.” Ear and Hearing 29 (6):930–941. doi:10.1097/AUD.0b013e31818713a8.
- Brodie, A., B. Smith, and J. Ray. 2018. “The Impact of Rehabilitation on Quality of Life After Hearing Loss: A Systematic Review.” European Archives of Oto-Rhino-Laryngology 275 (10):2435–2440. doi:10.1007/s00405-018-5100-7.
- Carter, R., and D. Hailey. 1999. “Economic Evaluation of the Cochlear Implant.” International Journal of Technology Assessment in Health Care 15 (3):520–530. doi:10.1017/S0266462399015378.
- Chisolm, T. H., C. E. Johnson, J. L. Danhauer, L. J. P. Portz, H. B. Abrams, S. Lesner, P. A. McCarthy, and C. W. Newman. 2007. “A Systematic Review of Health-Related Quality of Life Hearing Aids: Final Report of the American Academy of Audiology Task Force on the Health-Related Quality of Life Benefits of Amplication in Adults.” Journal of the American Academy of Audiology 18 (2):151–183. doi:10.3766/jaaa.18.2.7.
- Ciorba, A., C. Bianchini, S. Pelucchi, and A. Pastore. 2012. “The Impact of Hearing Loss on the Quality of Life of Elderly Adults.” Clinical Interventions in Aging 7:159–163. doi:10.2147/CIA.S26059.
- Cox, R., M. Hyde, S. Gatehouse, W. Noble, H. Dillon, R. Bentler, D. Stephens et al. 2000. “Optimal Outcome Measures, Research Priorities, and International Cooperation.” Ear and Hearing 21: 106S–115S. doi:10.1097/00003446-200008001-00014.
- Cox, R. M., and G. C. Alexander. 1995. “The Abbreviated Profile of Hearing Aid Benefit.” Ear and Hearing 16 (2):176–186. doi:10.1097/00003446-199504000-00005.
- Cox, R. M., K. S. Schwartz, C. M. Noe, and G. C. Alexander. 2011. “Preference for One or Two Hearing Aids Among Adult Patients.” Ear and Hearing 32 (2):181–197. doi:10.1097/AUD.0b013e3181f8bf6c.
- Crandell, C. 1998. “Hearing Aids: Their Effects on Functional Health Status.” The Hearing Journal 51 (2):22. doi:10.1097/00025572-199802000-00002.
- Crews, J. E., and V. A. Campbell. 2004. “Vision Impairment and Hearing Loss among Community-Dwelling Older Americans: Implications for Health and Functioning.” American Journal of Public Health 94 (5):823–829. doi:10.2105/AJPH.94.5.823.
- Elberling, C., C. Ludvigsen, and P. E. Lyregaard. 1989. “Dantale: A New Danish Speech Material.” Scandinavian Audiology 18 (3):169–175. doi:10.3109/01050398909070742.
- Etxeberria, I., E. Urdaneta, and N. Galdona. 2019. “Factors Associated with Health-Related Quality of Life (HRQoL): Differential Patterns Depending on Age.” Quality of Life Research 28 (8):2221–2231. doi:10.1007/s11136-019-02182-0.
- EuroQoL Group. 1990. “EuroQol – A New Facility for the Measurement of Health-Related Quality of Life.” Health Policy 16 (3):199–208. doi:10.1016/0168-8510(90)90421-9.
- Fischer, M. E., K. J. Cruickshanks, B. E. Klein, R. Klein, C. R. Schubert, and T. L. Wiley. 2009. “Multiple Sensory Impairment and Quality of Life.” Ophthalmic Epidemiology 16 (6):346–353. doi:10.3109/09286580903312236.
- Gallicchio, L., S. C. Hoffman, and K. J. Helzlsouer. 2007. “The Relationship Between Gender, Social Support, and Health-Related Quality of Life in a Community-Based Study in Washington County, Maryland.” Quality of Life Research 16 (5):777–786. doi:10.1007/s11136-006-9162-4.
- Gatehouse, S., and I. Noble. 2004. “The Speech, Spatial and Qualities of Hearing Scale (SSQ).” International Journal of Audiology 43 (2):85–99. doi:10.1080/14992020400050014.
- Gopinath, B., J. Schneider, L. Hickson, C. M. McMahon, G. Burlutsky, S. R. Leeder, and P. Mitchell. 2012. “Hearing Handicap, Rather Than Measured Hearing Impairment, Predicts Poorer Quality of Life Over 10 Years in Older Adults.” Maturitas 72 (2):146–151. doi:10.1016/j.maturitas.2012.03.010.
- Gouveia, É. R. Q., B. R. Gouveia, A. Ihle, M. Kliegel, J. A. Maia, S. B. I Badia, and D. L. Freitas. 2017. “Correlates of Health-Related Quality of Life in Young-Old and Old–Old Community-Dwelling Older Adults.” Quality of Life Research 26 (6):1561–1569. doi:10.1007/s11136-017-1502-z.
- Harris, P. A., R. Taylor, B. L. Minor, V. Elliott, M. Fernandez, L. O'Neal, L. McLeod, et al. 2019. “The REDCap Consortium: Building an International Community of Software Platform Partners.” In Journal of Biomedical Informatics 95:103208. doi:10.1016/j.jbi.2019.103208.
- Harris, P. A., R. Taylor, R. Thielke, J. Payne, N. Gonzalez, and J. G. Conde. 2009. “Research Electronic Data Capture (REDCap)-A Metadata-Driven Methodology and Workflow Process For Providing Translational Research Informatics Support.” Journal of Biomedical Informatics 42 (2):377–381. doi:10.1016/j.jbi.2008.08.010.
- Hawton, A., C. Green, A. P. Dickens, S. H. Richards, R. S. Taylor, R. Edwards, C. J. Greaves, and J. L. Campbell. 2011. “The Impact of Social Isolation on the Health Status and Health-Related Quality of Life of Older People.” Quality of Life Research 20 (1):57–67. doi:10.1007/s11136-010-9717-2.
- Hogan, A., K. O'Loughlin, P. Miller, and H. Kendig. 2009. “The Health Impact of a Hearing Disability on Older People in Australia.” Journal of Aging and Health 21 (8):1098–1111. doi:10.1177/0898264309347821.
- Horsman, J., W. Furlong, D. Feeny, and G. Torrance. 2003. “The Health Utilities Index (HUI®): Concepts, Measurement Properties and Applications.” Health and Quality of Life Outcomes 1 (1):54. doi:10.1186/1477-7525-1-54.
- Houmøller, S. S., A. Wolff, S. Möller, V. K. Narne, S. K. Narayanan, C. Godballe, D. D. Hougaard, et al. 2022. “Prediction of Successful Hearing Aid Treatment in First-Time and Experienced Hearing Aid Users: Using the International Outcome Inventory for Hearing Aids.” International Journal of Audiology 61 (2):119–129. doi:10.1080/14992027.2021.1916632.
- ISO 8253-1. 2010. Acoustics – Audiometric Test Methods – Part 1: Basic Pure-Tone Air And Bone Conduction Threshold Audiometry. Geneva: International Organisation for Standardisation.
- Ivory, P. J., B. L. Hendricks, D. Van Vliet, C. M. Beyer, and H. B. Abrams. 2009. “Short-Term Hearing Aid Benefit in a Large Group.” Trends in Amplification 13 (4):260–280. doi:10.1177/1084713809354902.
- Keidser, G., H. Dillon, M. Flax, T. Ching, and S. Brewer. 2011. “The NAL-NL2 Prescription Procedure.” Audiology Research 1 (1):e24. doi:10.4081/audiores.2011.e24.
- Malinoff, R. L., and B. E. Weinstein. 1989. “Changes in Self-Assessment of Hearing Handicap Over the First Year of Hearing Aid Use by Older Adults.” Journal of the Academy of Rehabilitative Audiology 22: 54–60. https://psycnet.apa.org/record/1990-23487-001
- Mener, D. J., J. Betz, D. J. Genther, D. Chen, and F. R. Lin. 2013. “Hearing loss and depression in older adults.” Journal of the American Geriatrics Society 61 (9):1627–1629. doi:10.1111/jgs.12429.
- Michel, Y. A., L. A. Augestad, and K. Rand. 2018. “Comparing 15D Valuation Studies in Norway and Finland—Challenges When Combining Information from Several Valuation Tasks.” Value in Health 21 (4):462–470. doi:10.1016/j.jval.2017.09.018.
- Mikkola, T. M., H. Polku, E. Portegijs, M. Rantakokko, T. Rantanen, and A. Viljanen. 2015. “Self-Reported Hearing Status is Associated with Lower Limb Physical Performance, Perceived Mobility, and Activities of Daily Living in Older Community-Dwelling Men and Women.” Journal of the American Geriatrics Society 63 (6):1164–1169. doi:10.1111/jgs.13381.
- Mikkola, T. M., E. Portegijs, M. Rantakokko, J.-P. Gagné, T. Rantanen, and A. Viljanen. 2015. “Association of Self-Reported Hearing Difficulty to Objective and Perceived Participation Outside the Home in Older Community-Dwelling Adults.” Journal of Aging and Health 27 (1):103–122. doi:10.1177/0898264314538662.
- Narayanan, S. K., P. Rye, T. Piechowiak, G. Ravn, A. Wolff, S. S. Houmøller, J. H. Schmidt, and D. Hammershøi. 2023. “Can Real-Ear Insertion Gain Deviations from Generic Fitting Prescriptions Predict Self-Reported Outcomes?” International Journal of Audiology 62 (5):433–441. doi:10.1080/14992027.2022.2053594.
- Niemensivu, R., V. Manchaiah, R. P. Roine, E. Kentala, and H. Sintonen. 2015. “Health-Related Quality of Life in Adults with Hearing Impairment Before and After Hearing-Aid Rehabilitation in Finland.” International Journal of Audiology 54 (12):967–975. doi:10.3109/14992027.2015.1077400.
- Noble, W., N. S. S. Jensen, G. Naylor, N. Bhullar, and M. A. Akeroyd. 2013. “A Short form of the Speech, Spatial and Qualities of Hearing Scale Suitable for Clinical Use: The SSQ12.” International Journal of Audiology 52 (62012):409–412. doi:10.3109/14992027.2013.781278.
- Patrick, D. L., and R. A. Deyo. 1989. “Generic and Disease-Specific Measures in Assessing Health Status and Quality of Life.” Medical Care 27:S217–S232. doi:10.1097/00005650-198903001-00018.
- Polku, H., T. M. Mikkola, M. Rantakokko, E. Portegijs, T. Törmäkangas, T. Rantanen, and A. Viljanen. 2015. “Self-Reported Hearing Difficulties and Changes in Life-Space Mobility Among Community-Dwelling Older Adults: A Two-Year Follow-Up Study.” BMC Geriatrics 15 (1):1–7. doi:10.1186/s12877-015-0119-8.
- Saarni, S. I., T. Härkänen, H. Sintonen, J. Suvisaari, S. Koskinen, A. Aromaa, and J. Lönnqvist. 2006. “The Impact of 29 Chronic Conditions on Health-Related Quality of Life: A General Population Survey in Finland Using 15D and EQ-5D.” Quality of Life Research 15 (8):1403–1414. doi:10.1007/s11136-006-0020-1.
- Scoggins, J. F., and D. L. Patrick. 2009. “The Use of Patient-Reported Outcomes Instruments in Registered Clinical Trials: Evidence from ClinicalTrials.gov.” Contemporary Clinical Trials 30 (4):289–292. doi:10.1016/j.cct.2009.02.005.
- Shield, B. 2019. Evaluation of the Social and Economic Costs of Hearing Impairment. London: Brunel University.
- Sintonen, H., and J. Richardson. 1994. The 15-D Measure of Health Related Quality of Life: Reliability, Validity and Sensitivity of its Health State Descriptive System. Working Paper 41. Melbourne: National Centre for Health Program Evaluation.
- Sintonen, H. 2001. “The 15D Instrument of Health-Related Quality of Life: Properties and Applications.” Annals of Medicine 33 (5):328–336. doi:10.3109/07853890109002086.
- Sivertsen, H., G. H. Bjørkløf, K. Engedal, G. Selbæk, and A.-S. Helvik. 2015. “Depression and Quality of Life in Older Persons: A Review.” Dementia and Geriatric Cognitive Disorders 40 (5–6):311–339. doi:10.1159/000437299.
- Stevens, G., S. Flaxman, E. Brunskill, M. Mascarenhas, C. D. Mathers, and M. Finucane. 2013. “Global and Regional Hearing Impairment Prevalence: An Analysis of 42 Studies in 29 Countries.” European Journal of Public Health 23 (1):146–152. doi:10.1093/eurpub/ckr176.
- Tajvar, M., M. Arab, and A. Montazeri. 2008. “Determinants of Health-Related Quality of Life in Elderly in Tehran, Iran.” BMC Public Health 8:323. doi:10.1186/1471-2458-8-323.
- Tay, T., J. J. Wang, R. Lindley, E. M. Chia, P. Landau, N. Ingham, A. Kifley, and P. Mitchell. 2007. “Sensory Impairment, Use of Community Support Services, and Quality of Life in Aged Care Clients.” Journal of Aging and Health 19 (2):229–241. doi:10.1177/0898264307299243.
- Tordrup, D., J. Mossman, and P. Kanavos. 2014. “Responsiveness of the EQ-5D to Clinical Change: Is the Patient Experience Adequately Represented?” International Journal of Technology Assessment in Health Care 30 (1):10–19. doi:10.1017/S0266462313000640.
- Tseng, Y. C., S. H. Y. Liu, M. F. Lou, and G. S. Huang. 2018. “Quality of Life in Older Adults With Sensory Impairments: A Systematic Review.” Quality of Life Research 27 (8):1957–1971. doi:10.1007/s11136-018-1799-2.
- Vestergaard Knudsen, L., M. Öberg, C. Nielsen, G. Naylor, and S. E. Kramer. 2010. “Factors Influencing Help Seeking, Hearing Aid Uptake, Hearing Aid Use and Satisfaction With Hearing Aids: A Review of the Literature.” Trends in Amplification 14 (3):127–154. doi:10.1177/1084713810385712.
- Wittrup-Jensen, K., and K. Pedersen. 2008. “Modelling Danish Weights for the 15D Quality of Life Questionnaire by Applying Multi-Attribute Utility Theory (MAUT).” Health EconomicsPapers 7. University of Southern Denmark:1–35. http://static.sdu.dk/mediafiles/Files/Om_SDU/Centre/c_ist_sundoke/Forskningsdokumenter/publications/Workingpapers/20087.pdf%0Ahttp://findresearcher.sdu.dk/portal/da/publications/modelling-danish-weights-for-the-15d-quality-of-life-questionnaire-by-a-appl.
- Wolff, A. 2019. “Health-Related Quality of Life Following Hearing Aid Treatment a large Cohort study.” PhD diss., Aalborg Universitetsforlag.
- Wong, L. L., and L. K. Cheng. 2012. “Quality of Life in Older Chinese-Speaking Adults With Hearing Impairment.” Disability and Rehabilitation 34 (8):655–664. doi:10.3109/09638288.2011.619614.
- Zhang, S., S. Moyes, C. McLean, G. Searchfield, D. Welch, R. Jacobs, and N. Kerse. 2016. “Self-Reported Hearing, Vision and Quality of Life: Older People in New Zealand.” Australasian Journal on Ageing 35 (2):98–105. doi:10.1111/j.1741-6612.2012.00627.x.
