 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Objective
The goal of this study was to determine open field stapedius reflex thresholds (oSRTs) in CI patients with fittings based on subjective loudness ratings. A further objective was to compare these oSRTs and those of eSRT-based fittings that are similar to the oSRTs of normal hearing.
Design
Impedance measurements of the ear drum were taken while subjects were wearing their audio processors. The stapedius reflex was elicited by electrical stimulation transmitted through the activated CI system in response to an acoustic stimulus presented in the free sound field.
Study sample
Subjects were 50 experienced CI users (n = 57 ears) with CI fittings based on subjective loudness scaling.
Results
A reference range for the oSRTs was defined that was identified in CI patients with eSRT-based fittings. Sound levels for stapedius reflex detection were inside the reference target range in 70% of the cases, below the reference range (i.e. down to 40 dB HL) in 20% of the cases, and above the reference range in 10% of the cases.
Conclusion
Stapedius reflex detection in a free sound field may help detect fittings with too high or too low stimulation levels that might reduce audiological performance.
Introduction
A main objective during the postoperative rehabilitation process of cochlear implant (CI) users following implant activation is to establish an appropriate set of electrical stimulation parameters. One method is to estimate the lower and upper limits of the electrical stimulation intensities by using subjective loudness scaling for each channel. This method based on subjective loudness scaling is common in many clinics despite it is known for many years, that loudness scaling as the primary estimator for upper stimulation levels might not be ideal. However, a necessary requirement for this procedure is that patients are able to assess and communicate the loudness of the electrical stimulation. For people who are unable or unwilling to provide such feedback (e.g. very young children, uncooperative recipients, or people with complex needs), this process is ineffective. Even with cooperative recipients, psychoacoustical methodology can lead to either overtly exaggerated or substantially lower stimulation levels. Higher stimulation levels (i.e. overstimulation) are associated with an increased spread of the electrical fields, which may blur the accuracy of transmitted acoustic information. In contrast, lower stimulation levels (i.e. understimulation) are associated with a reduced electrical dynamic range, which diminishes the accuracy of acoustic information. In both cases, speech understanding can be affected.
To overcome the difficulties entailed in fitting CIs based on recipients’ subjective feedback, objective methodologies are sorely needed. One objective method is to measure the electrical stapedius reflex threshold (eSRT) via single channel stimulation of the CI. A previous publication reported that the eSRT can be a valid estimator for upper stimulation levels in each implant channel. CI users with stimulation parameters that were adjusted using eSRT typically achieve good speech recognition scores. Koşaner et al. (Citation2009) investigated speech understanding in a large sample (n = 39) of experienced CI patients using eSRT-based fittings and found mean speech recognition scores of 80% monosyllabic words (Koşaner et al. Citation2009).
A direct comparison of “eSRT-based” and psychoacoustic fittings was reported by Spivak et al. (Citation1994) (Spivak et al. Citation1994) and Wolfe and Kasulis (Citation2008). Spivak et al. compared speech recognition using behaviourally determined fittings and eSRT-based fittings in a small group (n = 7) of subjects and found similar scores for both methods. The authors concluded that eSRTs are perhaps an appropriate substitute for psychoacoustically determined stimulus intensity levels when programming the CI in users who are unable to perform the subjective loudness scaling. Wolfe et al. created eSRT-based fittings in a small group (n = 11) and found them to provide better speech recognition than fittings using conventional behavioural measures of stimulation levels. The authors concluded that individuals can acquire a strong benefit from the eSRT-based fitting procedure.
The use of eSRT detection first appeared in the late 1980s. At that time research focused on the fundamental properties of the electrically evoked stapedius reflex rather than on determining a CI fitting procedure (Battmer, Laszig, and Lehnhardt Citation1990; Jerger et al. Citation1986; Stephan, Welzl-Müller, and Stiglbrunner Citation1988). Since then, various aspects of eSRT measurements have been investigated, such as the influence of stimulation parameters or probe tone frequency on detectability of the eSRT (Wolfe et al. Citation2017 and Citation2018, Hernandez et al. Citation2019; Scheperle and Hajicek Citation2020). Fundamental research has focused on the amplitude growth function of the impedance change within the eardrum (Brickley et al. Citation2005; Charroó et al. Citation2021; Jerger, Oliver, and Chmiel Citation1988; Stephan, Welzl-Müller, and Stiglbrunner Citation1990; Stephan and Welzl-Müller Citation1994). Furthermore, seminal investigations have shown positive correlations between the electrical stimulation levels, at the eSRT, and other objective measurements, such as electrically evoked compound action potentials and auditory brainstem responses (Brickley et al. Citation2005; Wolfe et al. 2008; Gordon, Papsin, and Harrison Citation2004; Kosaner et al. Citation2018).
The reported detectability of eSRTs elicited by electrical stimulation in CI patients ranges from 65% to 90% (Battmer, Laszig, and Lehnhardt Citation1990; Brickley et al. Citation2005; Cinar et al. Citation2011; Gordon, Papsin, and Harrison Citation2004; Hodges et al. Citation1997). This high variability could be due to various inclusion criteria employed for the study, e.g. regarding middle ear functionality. If patients with defective middle ears are excluded a priori, then the proportion of those in whom the reflex is detectable increases.
Correlations between the eSRT and the psychoacoustically determined electrical stimulus intensities have determined that the eSRT was a reasonable estimator of the upper limits of electrical stimulus intensities (Hodges et al. Citation1997; Shallop and Ash Citation1995; Stephan and Welzl-Muller Citation2000; Allum, Greisiger, and Probst Citation2002; Gordon, Papsin, and Harrison Citation2004; Koşaner et al. Citation2009; Wolfe et al. 2008, Walkowiak et al. Citation2011; Charroó et al. Citation2021; Brickley et al. Citation2005). In a recent study using a large sample (n = 205), eSRT tended to be higher than the behaviourally determined stimulation level (Pitt et al. Citation2021). Furthermore, this study found that eSRT remained stable over a three-year period. This was in accordance with earlier studies reporting consistency of eSRT measurements during the first six months of CI use (Allum, Greisiger, and Probst Citation2002; Van Den Abbeele et al. Citation2012).
A few studies have shown only a modest correlation between eSRT and pyschoacoustically determined stimulus levels, where eSRT measurements resulted in stimulation levels either above or below psychoacoustically determined stimulus levels (Bresnihan et al. Citation2001; Çiprut and Adıgül Citation2020; Spivak and Chute Citation1994). Deviations may be due to poor ratings of the subjective loudness impression in response to electrical stimulation with CI in some users. This can lead to either overstimulation (i.e. too high stimulation levels) or understimulation (i.e. too low stimulation levels). It remains unclear whether over- and understimulation occur when fitting is based solely on psychoacoustic methods such as loudness scaling.
In the present study we used an alternative type of stapedius reflex measurement with activated cochlear implant system in an open sound field to detect cochlear implant fittings suffering from possible over- or understimulation. Apart from the electrical stimulation on single channels of the CI, the stapedius reflex can also be elicited in a free sound field by means of acoustic stimuli while the user is wearing an activated CI audio processor. The successful application of such an open field stapedius reflex measurement (oSR) in CI patients using acoustic stimuli in a free sound field was shown in a very recent study by Franke-Trieger et al. (Citation2021).
In particular, open field stapedius reflex thresholds (oSRT) were determined for cochlear implant fittings based on the single channel eSRT method. The results obtained in CI users were compared to a normal hearing control group, where oSRT was measured in both groups. The main finding was that CI patients with eSRT-based fittings had oSRTs in a range similar to those seen in the normal hearing control group, but for CI patients a frequency dependence of oSRTs was found, whereas no frequency dependence of the oSRTs was seen in normal hearing listeners. For normal hearing listeners mean oSRTs were approx. 90 dB HL for all tested stimuli frequencies (500 Hz, 1000 Hz, 2000 Hz and 4000 Hz). For CI patients mean oSRT decreased for increasing stimulus frequencies with means of approx. 90 dB HL for 500 Hz and 1000 Hz, 85 dB HL for 2000 Hz and 80 dB HL for 4000 Hz. Considering the range of measured oSRTs no difference was found for the low frequencies (500 Hz, 1000 Hz) but a difference was found for the high frequencies (2000 Hz, 4000 Hz) with 10 dB lower oSRTs for CI patients using eSRT based fittings compared to the normal hearing control group. In CI patients oSRT were measured down to 70 dB and 65 dB for 2000 Hz and 4000 Hz. In the normal hearing control group oSRTs were measured down to 80 dB and 75 dB for these frequencies. Thus, oSRTs of CI patients using eSRT based fittings and oSRT of normal hearing subjects are in a similar range. However, it is possible to increase electrical stimulation in CI patients to such an extent that oSRTs are elicited already at sound levels of 40 dB HL, which is clearly below the range found for eSRT based fittings or for normal hearing subjects.
To date, oSRTs of subjective fittings and their relation to an eSRT-based objective fitting in the same CI patient have not been studied. Therefore, the primary goal of this study was to determine oSRTs in CI patients with fittings based on subjective loudness ratings. The second study goal was to compare the found oSRTs and those obtained in CI patients with objective eSRT-based fittings. A reference range for oSRTs was defined, which indicates whether electrical stimulation levels of the psychoacoustically determined fittings were similar to eSRT-based fittings or not. oSRTs clearly above or clearly below the reference range may be interpreted as under- or overstimulation. This might result in insufficient stimulation of the auditory nerve.
Materials and methods
Inclusion and exclusion criteria
To be included in the study, participants had to have a cochlear implant type MedEl Mi1200, Concerto, Sonata, Pulsar or Combi40+, at least ten months CI experience, an intact middle ear for detection of the stapedius reflex through impedance measurements, and be a native speaker of German. The inclusion criterion of at least ten months CI experience was chosen because stimulation levels typically stabilise after half a year during the rehabilitation process and hence a stable profile of comfort levels can be expected. The middle ear status and the detectability of the stapedius reflex in all patients who participated in the study were carefully determined prior to participation.
Potential participants were excluded if they showed abnormalities of the middle ear or if their stapedius reflex behaviour was unclear for other reasons. In total 37 patients were excluded for these reasons.
The inclusion criteria were met by 50 people (57 ears), all of whom were included in the study. A detailed outline of participant demographics and the details of their implant system are shown in . It must be noted that the subjects had different levels of contralateral hearing (normal hearing, mild, moderate, severe or profound hearing loss).
Table 1. Description of the study group.
This study was conducted in accordance with the Declaration of Helsinki (2013) on research involving human subjects and was approved by the local ethics committee (EK 368072019). All subjects provided verbal and written informed consent prior to testing.
Details of implant fitting
In the majority of the subjects, electrical stimulation pulses were biphasic except in one subject who was a bilateral CI user. This subject exhibited facial nerve co-stimulation and thus stimulation pulses were triphasic in both ears.
The lower limit of acoustic frequencies transmitted to the CI system ranged from 70 to 100 Hz. Seven subjects had functional residual hearing within these lower frequencies. In these cases the lowest acoustic frequency transmitted to the CI system was higher, i.e. 200 Hz to 1000 Hz. Four subjects used electro-acoustic stimulation with crossover frequencies of 175 Hz, 271 Hz, 600 Hz, and 1000 Hz according to their residual hearing. In all other subjects, no acoustic unit was used. The upper limit of transmitted acoustic frequencies was the default value of the particular CI system, namely 8500 Hz, in all but one subject, who was adjusted to 7500 Hz. The backend compression (MAPLAW) was set to the default value of 500 in the majority of the subjects (see ). In 11 subjects (i.e. ears) at least one stimulation electrode had to be deactivated because of unclear sound impressions, co-stimulation of the facial nerve, or migration of the electrode array resulting in electrodes located outside the cochlea. All subjects underwent a series of sessions in which the speech processor was fit using psychoacoustic methods. In particular, loudness scaling was performed to estimate the lower and upper limit of the electric stimulation levels for each channel, (i.e. the threshold level (THR) and the maximum comfort level (MCL) value). Regarding hearing thresholds, the subjects reached PTA4 values (i.e. mean of hearing threshold levels averaged across frequencies of 500, 1000, 2000 and 4000 Hz), with their CIs ranging from 20 to 54 dB HL, with a mean of 38 ± 6 dB HL.
Open field stapedius reflex measurement setup
The stapedius reflex was detected by measuring the change in acoustic impedance of the ear drum using an eTymp USB tympanometer and the eAudio software (Biomed Jena), as previously described (Franke-Trieger et al. Citation2021). The eTymp USB tympanometer was equipped to receive trigger signals from the CI interface box. Calibration of the tympanometer probe tone to 226 Hz was performed using a standardised 2ccm coupler, whereas the reference sound level was 85 dB SPL. The favoured placement of the probe was on the side of the implanted ear. In the case of any irregular impedance morphology or non-functioning middle ear, the tympanometer probe was placed in the ear canal of the non-implanted ear. The side with the implanted ear was preferred, because the majority of patients did not have acoustic hearing in that ear and thus the probe tone was not heard by the patients. The probe tone may become uncomfortable if heard during longer measurements.
Open field stapedius reflex measurement procedure
In order to measure the stapedius reflex in a free sound field, subjects were seated at a distance of one metre from the front of a loudspeaker while wearing their activated audio processor, using the daily use fittings. “Daily use fittings” are those that subjects use in their daily lives. All these “daily use fittings” had been obtained through subjective loudness rating in earlier fitting sessions.
Acoustic stimulation was performed using narrow band noise (NBN) bursts with centre frequencies (fc) at 500, 1000, 2000 and 4000 Hz . The stimuli are created by means of bandpass filtering of white noise with filters having an upper cut-off frequency (-3dB) of fc*20.2 and a lower cut-off frequency of fc/(20.2). Attenuation was -36dB per octave. The 500 ms stimuli had a rise and fall time of 40 ms, which is realised by means of a cosine window function (conforms to DIN EN 60645-5). Calibration is performed according to the reference values of the standard DIN EN 389-4 using a Class 1 sound level metre. The stimuli were presented at different sound levels ranging from 40 to 100 dB HL, except for the 500 Hz stimuli where the maximum presentation level was loudspeaker-dependent at 95 dB HL. Sound levels were increased in steps of 5 dB. Simultaneously, the acoustic impedance of the ear drum was recorded. To prevent the stapedius reflex from being evoked through the non-implanted ear with potential functional hearing, earplugs and/or earmuffs were used. This was necessary because some patients had normal hearing or mild hearing loss in the contralateral ear. Furthermore, an additional measurement with the contralateral ear plugged and/or covered, but without the patient wearing the CI processor, was performed to ensure that the stapedius reflex was not triggered by the contralateral ear at the particular presentation level. Once the probe is situated in the ear canal, the time needed to measure reflex thresholds in a free sound field is less than half a minute (for all frequencies). Franke-Trieger et al. (Citation2021) show an example of an impedance change originating from the” free field” stapedius reflex in one CI user (Franke-Trieger et al. Citation2021). In all free field measurements, pre-processing parameters of the audio processors were given the same settings in all study subjects. In particular, sensitivity was set to 75% and the compression ratio was set to 3:1.
Data analysis and statistics
All analysis and figure creation was completed using OriginLab (version 2019, OriginLab software, Northhampton, MA, USA). During analysis of the daily use fitting stimulation levels, we took into account the adjusted volume. The maximum effective stimulation levels after correcting for volume adjustment (MCLeffective) were calculated from the volume setting V, the maximum comfort levels of the electric stimulation MCL and the lower limit of the electric stimulation levels THR of the particular fitting, as follows:
The upper limit of stimulation levels of the daily use fitting refers to the effective stimulation level MCLeffective.
Normality was tested using the Kolmogorov-Smirnov test. Pairwise comparisons of oSRT data were performed using T tests for data normality and using the Mann-Whitney test when normality was violated. In particular, T tests were performed for the stimulus frequencies 1000, 2000 and 4000 Hz to compare oSRT data on daily use fittings and oSRT data on eSRT-based fittings. To compare the oSRT data at 500 Hz stimulus the non-parametric test was used.
Results
Open field stapedius reflex thresholds of the daily use fitting
The measured oSRTs were found in ranges of 40 dB HL and 100 dB HL for 1000, 2000 and 4000 Hz and between 65 dB HL and 95 dB HL for 500 Hz. To compare these measured oSRTs and the oSRTs of eSRT-based fittings serving as reference range the data were clustered into three categories: oSRTs above, within and below this reference range. The reference range refers to oSRTs of CI patients with eSRT-based fittings as reported in our previous work (Franke-Trieger et al. Citation2021). In this earlier study oSRTs of the particular patients using eSRT-based fittings were found between 75 dB Hl and 95 dB HL for the 500 Hz stimulus, between 80 dB HL and 100 dB HL for the 1000 Hz stimulus, between 70 dB HL and 100 dB HL for the 2000 Hz stimulus and between 55 dB HL and 100 dB HL for the 4000 Hz stimulus. These ranges for each stimulus frequency provided the basis for defining the categories, as described below.
Grading of fittings of cochlear implants according to the open field stapedius reflex
Category 1: Open field stapedius reflex thresholds above the reference range:
A CI fitting was assigned to Category 1 if oSRTs were detectable only after increasing stimulation levels when presenting the maximum stimulus. In “daily use condition” oSRTs for such a CI fitting were not detectable up to 95 dB HL for the 500 Hz stimulus and up to 100 dB HL for the other stimuli (with a centre frequency of 1000, 2000 and 4000 Hz).
Category 2: Open field stapedius reflex thresholds within the reference range:
A CI fitting was assigned to Category 2 if oSRTs were detectable in “daily use condition” and the oSRTs were found within the reference range for at least two of the four stimulus types and for not more than one of the four stimulus types below the reference range.
Category 3: Open field stapedius reflex thresholds below the reference range:
A CI fitting was assigned to Category 3 if oSRTs were present at stimulus levels below the frequency-dependent reference range for at least two of the four stimulus types.
shows measured oSRTs in Categories 2 and 3 and the reference range for eSRT-based fittings (oSRTs are absent in Category 1).
Figure 1. Open field stapedius reflex thresholds (oSRT) with daily use fitting activated. The red lines indicate the reference range for oSRTs in eSRT-based fittings measured by Franke-Trieger et al. (Citation2021). (a) Open field stapedius reflex thresholds for n = 40 ears with reflex thresholds within the reference range for at least two of the four stimulus types and for no more than one of the four stimulus types below the reference range (Category 2). (b) Open field stapedius reflex thresholds for n = 11 ears with reflex thresholds below the reference range for at least two of the four tested narrow band noise signals (Category 3). In n = 6 ears no open field stapedius reflexes were registered when using the daily use fitting (Category 3). Since no reflex threshold could be determined for this group by definition, these ears are not shown in this figure.
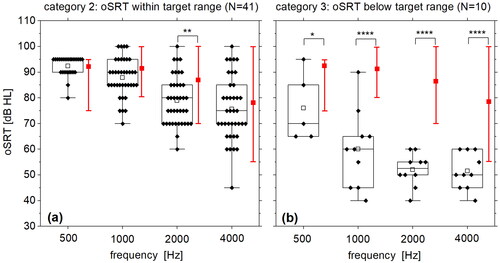
In 70% of the ears (n = 41), the measured oSRTs were within the reference range as defined above, thus meeting the definition for Category 2 as shown in . For not more than one of the four presented narrow band noise stimuli oSRT were below the reference range and at least two of the oSRTs were within the reference range. The thresholds in this group ranged between 80 and 95 dB HL for 500 Hz, 70 and 100 dB HL for 1000 Hz, 60 and 100 dB HL for 2000 Hz, and between 45 and 100 dB HL for 4000 Hz (). The mean thresholds in this group were 92, 88, 79, and 76 dB HL. The mean oSRTs of CI fittings based on eSRT (Franke-Trieger et al. Citation2021) were 92, 91, 87 and 79 dB HL. No significant differences were found between the oSRTs of daily use fittings and the oSRTs of eSRT-based fittings for the 500 Hz, 1000 Hz and 4000 Hz stimulus (T test for 1000 Hz and 4000 Hz, Mann-Whitney test for 500 Hz). For the 2000 Hz stimulus the mean oSRT of the daily use fittings is smaller than the mean oSRT of the eSRT-based fittings (T test, p < 0.001).
In 20% of the ears (n = 10), the measured oSRTs were below the reference range as defined above, thus meeting the definition for Category 3 as shown in . For at least two of the four presented narrow band noise stimuli oSRTs were below the reference range. Stapedius reflex thresholds ranged between 65 and 95 dB HL for 500 Hz, 40 and 90 dB HL for 1000 Hz, and between 40 and 75 dB HL for 2000 Hz and 40 and 60 dB HL for 4000 Hz. The means were 76, 60, 53 and 52 dB HL. Comparison of these oSRTs with oSRTs of eSRT-based fittings (Franke-Trieger et al. Citation2021) with means of 92, 91, 87 and 79 dB HL resulted in significantly lower oSRTs for the oSRTs of daily use fittings for all stimulus types (p < 0.00001 for 1000 Hz, 2000 Hz and 4000 Hz by means of T test; p < 0.05 for 500 Hz by means of Mann-Whitney test).
In 10% of the ears (n = 6), we found that no oSRTs were registered in the free sound field when using the daily use fitting, but the reflex was indeed registered after increasing stimulus intensities (i.e. with a modified fitting of the cochlear implant). They were assigned to Category1.
Stimulation levels of the “daily use fitting”
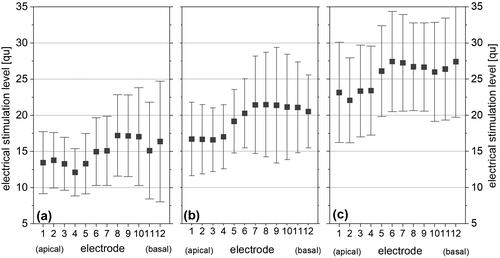
The upper stimulation levels (MCLeffective) of the daily use fittings of all ears (n = 57) are presented in . The left, middle, and right panels show the daily use fittings with oSRTs that are above (Category 1; ), within (Category 2; ), or below (Category 3; ) the reference range (Categories 1, 2, and 3). Mean upper limit of stimulation levels for fittings with reflex thresholds oSRT above the reference range (Category 1) varied from 12 to 13 charge units for the apical electrodes to 15 to 17 charge units for the medial and basal electrodes. Standard deviation was 4–8 charge units in this group (). One charge unit corresponds to approximately 1 e-6 coulomb. Mean upper limits of stimulation levels for ears with oSRT within the reference range (Category 2) varied from 17 charge units for the apical electrodes to 22 charge units for the medial and basal electrodes (). Standard deviation was 5–7 charge units in this group. Mean upper limits of stimulation levels for ears with oSRT below the reference range (Category 3; ) varied from 22 charge units for the apical electrodes to 25 charge units for the medial and basal electrodes. Standard deviation was 3–5 charge units in this group. Overall, the mean stimulation intensity of ears with oSRT above the reference range (Category 1; ) was on average approximately 5 charge units lower than that of ears with oSRT within the reference range (Category 2; ). Mean stimulation intensity of ears with oSRT below the reference range (Category 3; ) was on average 5 charge units higher than that of fittings with oSRT within the reference range.
Figure 2. Mean and standard deviation of the upper limits of stimulation levels MCLeffective of daily use fittings with open field stapedius reflex thresholds above the reference range (Category 1; a), within the reference range (Category 2; b) and above below the reference range (Category 3; c). The upper limits of stimulation are the lowest for individuals included in 2a. These individuals are underfit (eSRT above reference range - Category 1). The upper limits of stimulation are the highest for individuals included in 2c. These individuals are overfit (eSRT below reference range - Category 3).
Discussion
The main objective of the study was to establish a systematic classification of open sound field stapedius reflex thresholds (oSRT) found in patients with CI fittings created by psychoacoustic means. A reference range for oSRTs was defined, which may indicate that electrical stimulation parameters are adjusted such that the stapedius reflex behaviour is close to that of normal hearing listeners. The oSRT reference range was derived from measurements in patients, whose CI fittings were created by objective single channel electrical stapedius reflex (eSRT) measurements performed in our previous works.
The methodology for grading fittings of CIs according to oSRT was conceived in an earlier investigation by Franke-Trieger et al. (Citation2021), who published the method for measuring stapedius reflexes in an open sound field while wearing the implant system’s audio processor. In this study oSRTs in CI patients with eSRT-based fittings were measured and compared to those of a normal hearing control group. The oSRTs of patients with eSRT-based fittings showed a range similar to that of the normal hearing control group. Hence, oSRTs in CI patients with eSRT-based fittings may be a potential reference for the oSRTs in CI patients with subjective CI fittings. The primary objective of the current investigation aimed to identify and rate oSRTs with regard to intensity of electrical stimulation levels in experienced CI users, whose fittings were based on subjective loudness scaling. For this purpose, oSRTs of the particular CI users were graded as being above (Category 1), within (Category 2), or below (Category 3) the defined reference range that had been found for eSRT-based fittings (Franke-Trieger et al. Citation2021). In the earlier and the current investigation we measured the oSRT using four narrow band noise stimuli with different centre frequencies in order to cover possible frequency dependencies. Hence, the rating of a CI fitting was based on four oSRT values. When defining the categories “below, within or above the reference range” the frequency dependence of oSRTs found for eSRT-based fittings should be considered. Categories should be defined in such a way that each patient meets one of the definitions in a unique manner. This was challenging because if we had chosen a too strong definition, such as “all four oSRT values are below reference range,” only two patients (N = 3%) would have met this criterion. On the other hand, “one oSRT value below reference range” might be too weak if the other three oSRT values are within the reference range. Since patients show some variability in the oSRTs for the different frequencies, a trade-off in the definition of the reference range was necessary, which may limit the study in some way. However, the proposed definition is applicable to typical CI fittings based on psychoacoustic methods that are widely used in clinics, and a large number of CI fittings (n = 57) were included in the present study. This is an advantage of the current study as compared to other works on stapedius reflexes in CI users, where sample sizes were smaller and the study results were thus less reliable. Previously, smaller sample sizes prevented investigations from using specific category groups when assessing postoperative stapedius reflexes and their relation to psychoacoustically determined stimulation levels (Bresnihan et al. Citation2001; Spivak and Chute Citation1994; Stephan, Welzl-Müller, and Stiglbrunner Citation1988; Citation1990; Stephan and Welzl-Muller Citation2000; van den Borne et al. Citation1996; Walkowiak et al. Citation2011).
In total, 70% of the patients had oSRTs within the reference range. Therefore, in most CI users psychoacoustic fitting methods yield oSRTs similar to those in patients whose CI fittings were created with eSRT measurements on each implant channel. Furthermore, the oSRTs of these CI patients are similar to those of normal hearing listeners, which might indicate that stimulation of the hearing nerve is neither too low nor too high. Frequency dependence of the oSRT was seen in all patients for psychoacoustic CI fittings as well as for objective CI fittings with eSRT. In particular, the mean oSRTs for eSRT based fittings was observed at 90 dB HL for the narrow band noise stimuli of 500 Hz and 1000 Hz, whereas for narrow band noise stimuli of 2000 Hz and 4000 Hz the oSRT was about 85 and 80 dB HL respectively. When comparing the oSRTs of the patients in the present study group – having oSRTs within the reference range – and the oSRTs of patients with eSRT-based fittings - that served as reference range - thresholds were found that were similar to those expected. No difference in mean oSRTs was found for three (500, 1000, 4000 Hz) of four stimulus types. For 2000 Hz a small difference of approx. 5 dB was found between the mean oSRT of CI users with behavioural fittings and the mean oSRT for eSRT-based fittings.
In 20% of the patients using psychoacoustic CI fittings corresponding oSRTs were below the reference range. In this group, oSRTs were found down to a sound level of 40 dB HL for the tested narrow band signals. This behaviour was particularly pronounced at the high frequencies above 500 Hz. The difference between oSRTs in this group - with oSRTs below the reference range - and oSRTs of eSRT-based fittings - that served as the reference range – was found to be statistically significant for all four stimulus types. The mean difference was approx. 10 dB for 500 Hz and 30 dB for 1000 Hz, 2000 Hz and 4000 Hz. Obviously, oSRTs were far below the reference range in these subjects, when comparing them with oSRTs of eSRT-based fittings and far below the range of oSRTs in normal hearing listeners as found by Franke-Trieger et al. (Citation2021). As a result, the stapedius reflex can be elicited in an open sound field in these CI users at typical speech sound levels. The effect of such excessive activation of the stapedius reflex is unknown, but it might indicate that stimulation levels are too high. Furthermore, it might have a negative impact on overall listening effort. In these patients, comfort levels were reduced using the objective eSRT method on single channels, which resulted in oSRTs in the reference range. All patients accepted the modification of comfort levels and used the new eSRT-based fitting in daily life.
Moreover, in a small group of 10% of the study patients no oSRTs were registered at the maximum possible sound presentation levels of the narrow band noises. Interestingly, in each of these subjects, the reflex was able to be registered after increasing the stimulus intensity, whereby a new fitting with increased maximum comfort levels on all implant channels was created. Thus, the lack of stapedius reflexes in CI users might be an indicator for stimulation levels that are too low. However, caution must be exercised when interpreting this particular result because not every CI fitting lacking oSRTs is caused by too low stimulation levels. Indeed, in some CI users oSRTs cannot be elicited regardless of the CI fitting, namely because of insufficient function of the middle ear. On the other hand, if the middle ear status of the implanted ear is normal, too low stimulation levels based on psychoacoustic methods can potentially be corrected. Ultimately, a CI fitting may be created for such users, thus resulting in oSRTs in a range similar to that of their normal hearing counterparts. In the patients participating in the present study the fittings were modified by increasing the MCL based on eSRT, resulting in oSRTs within the reference range. Unfortunately, only two of the six patients accepted the increase in the comfort levels achieved with the eSRT procedure and consequently used this eSRT-based fitting in daily life.
Apart from open field stapedius reflex properties in CI users, absolute stimulation levels of their CI fittings have been analysed. The question remains: can CI fittings that show a trend to too low or too high stimulation levels be detected a priori based on the adjusted electrical stimulation levels? This is of particular interest for patients with insufficient function of the middle ear, since reflex measurement is not possible in these patients. In this study, average electrical stimulation levels of a CI fitting with oSRTs within the reference range were about 20 charge units (which corresponds to approximately 20 µC). This is very similar to the comfort levels of eSRT-based fittings found in the previous study by Franke-Trieger et al. (Citation2021).
Indeed, stimulation intensities were lower in CI fittings with oSRT above the reference range (i.e. 15 charge units on average) and higher in those CI fittings with oSRT below the reference range (i.e. 25 charge units on average). However, the variability within the stimulation levels across the study group was large (8–10 charge units), which limits their informative value. In fact, CI fittings with similar stimulation intensities can result in oSRTs above, within or below the reference range. Stimulation intensities alone are therefore not a unique indicator for detecting CI fittings that would result in oSRTs above or below the reference range.
Investigations regarding speech understanding were not part of the present study. Hence, the question remains whether patients with oSRTs below or above the reference range have lower speech recognition scores than patients with oSRTs in the reference range. Furthermore, the question remains whether oSRTs of CI patients with eSRT based fittings or of normal hearing listeners should serve as “target range”. Using oSRTs of normal hearing listeners as target range does not consider that pre-emphasis filters are used in the CI technique. Pre-emphasis filters are designed to reduce the low-frequency energy prior to encoding the acoustic signal, which might explain the increasing trend in stapedius reflex thresholds with stimulus frequency. However, for patients with oSRTs far below or far above the target range it would be of interest to know whether speech understanding can be improved by adjusting stimulation levels to move the corresponding oSRTs into the target range. Speech recognition scores may give insight into whether understimulation or overstimulation effectively results in poor speech performance by CI patients.
Conclusion
The objective method of open field stapedius reflex thresholds (oSRT) was used to analyse fittings, based on subjective loudness rating as the primary source for setting the upper limit of stimulation levels. In the majority of patients oSRTs were close to those of normal hearing listeners. However, in some patients oSRTs were far below or far above this normal range, which was associated with higher or lower stimulation levels compared to the group of patients with oSRTs in the normal range. Too high or too low stimulation levels might be accompanied by poor overall audiological performance. Thus, the method of open field stapedius reflex thresholds may be used to identify over- or understimulation, which could be the root cause of poor audiological performance.
Acknowledgments
The authors thank MED-EL for its support for this study and are indebted to the subjects of this study. Furthermore the authors thank Mary Heaney Margreiter for language editing.
Disclosure statement
The authors have no conflicts of interest to declare.
Additional information
Funding
References
- Allum, J. H., R. Greisiger, and R. Probst. 2002. “Relationship of intraoperative electrically evoked stapedius reflex thresholds to maximum comfortable loudness levels of children with cochlear implants.” International Journal of Audiology 41 (2):93–99. https://doi.org/10.3109/14992020209090399
- Battmer, R. D., R. Laszig, and E. Lehnhardt. 1990. “Electrically elicited stapedius reflex in cochlear implant patients.” Ear and Hearing 11 (5):370–374. https://doi.org/10.1097/00003446-199010000-00008
- Bresnihan, M., G. Norman, F. Scott, and L. Viani. 2001. “Measurement of comfort levels by means of electrical stapedial reflex in children.” Archives of Otolaryngology-Head & Neck Surgery 127 (8):963–966. https://doi.org/10.1001/archotol.127.8.963
- Brickley, G., P. Boyd, F. Wyllie, M. O'Driscoll, D. Webster, and P. Nopp. 2005. “Investigations into electrically evoked stapedius reflex measures and subjective loudness percepts in the MED-EL COMBI 40+ cochlear implant.” Cochlear Implants International 6 (1):31–42. https://doi.org/10.1002/cii.18
- Charroó, L. E., S. Bermejo, A. S. Paz Cordovez, C. Rodríguez, C. C. Finley, and A. A. Saoji. 2021. “Effect of Number of Electrodes Used to Elicit Electrical Stapedius Reflex Thresholds in Cochlear Implants.” Audiology & Neuro-Otology 26 (3):164–172. https://doi.org/10.1159/000510467
- Cinar, B. C., A. Atas, G. Sennaroglu, and L. Sennaroglu. 2011. “Evaluation of objective test techniques in cochlear implant users with inner ear malformations.” Otology & Neurotology 32 (7):1065–1074. https://doi.org/10.1097/MAO.0b013e318229d4af
- Çiprut, A., and Ç. Adıgül. 2020. “The Relationship between Electrical Stapedius Reflex Thresholds and Behaviorally Most Comfortable Levels in Experienced Cochlear Implant Users.” The Journal of International Advanced Otology 16 (1):8–12. https://doi.org/10.5152/iao.2019.6589
- Franke-Trieger, A., W. Mattheus, J. Seebacher, T. Zahnert, and M. Neudert. 2021. “Stapedius reflex evoked in free sound field in cochlear implant users compared to normal-hearing listeners.” International Journal of Audiology 60 (9):695–703. https://doi.org/10.1080/14992027.2020.1866780
- Gordon, K. A., B. C. Papsin, and R. V. Harrison. 2004. “Toward a battery of behavioral and objective measures to achieve optimal cochlear implant stimulation levels in children.” Ear and Hearing 25 (5):447–463. https://doi.org/10.1097/01.aud.0000146178.84065.b3
- Hernandez, L. C., L. C. Sánchez, M. C. Olivares, C. Rodríguez, C. C. Finley, and A. A. Saoji. 2019. “Effect of Probe-Tone Frequency on Ipsilateral and Contralateral Electrical Stapedius Reflex Measurement in Children With Cochlear Implants.” Ear & Hearing 40 (3):732–740. https://doi.org/10.1097/AUD.0000000000000656.
- Hodges, A. V., T. J. Balkany, R. A. Ruth, P. R. Lambert, S. Dolan-Ash, and J. J. Schloffman. 1997. “Electrical middle ear muscle reflex: use in cochlear implant programming.” Otolaryngology-Head and Neck Surgery 117 (3 Pt 1):255–261. https://doi.org/10.1016/s0194-5998(97)70183-9
- Jerger, J., H. Jenkins, R. Fifer, and D. Mecklenburg. 1986. “Stapedius reflex to electrical stimulation in a patient with a cochlear implant.” The Annals of Otology, Rhinology, and Laryngology 95 (2 Pt 1):151–157. https://doi.org/10.1177/000348948609500208
- Jerger, J., T. A. Oliver, and R. A. Chmiel. 1988. “Prediction of dynamic range from stapedius reflex in cochlear implant patients.” Ear and Hearing 9 (1):4–8. https://doi.org/10.1097/00003446-198802000-00010
- Koşaner, J., I. Anderson, Z. Turan, and M. Deibl. 2009. "The Use of ESRT in Fitting Children with Cochlear Implants."
- Kosaner, J., P. Spitzer, S. Bayguzina, M. Gultekin, and L. A. Behar. 2018. “Comparing eSRT and eCAP measurements in pediatric MED-EL cochlear implant users.” Cochlear Implants International 19 (3):153–161. https://doi.org/10.1080/14670100.2017.1416759
- Pitt, C., K. Muñoz, S. Schwartz, and J. M. Kunz. 2021. “The Long-Term Stability of the Electrical Stapedial Reflex Threshold.” Otology & Neurotology 42 (1):188–196. https://doi.org/10.1097/mao.0000000000002964
- Scheperle, R. A, and J. J. Hajicek. 2020. “Wideband Acoustic Immittance in Cochlear Implant Recipients: Reflectance and Stapedial Reflexes.” Ear & Hearing 41 (4):883–895. https://doi.org/10.1097/AUD.0000000000000810.
- Shallop, J. K., and K. R. Ash. 1995. “Relationships among comfort levels determined by cochlear implant patient’s self-programming, audiologist’s programming, and electrical stapedius reflex thresholds.” Ann Otol Rhinol Laryngol Suppl 166:175–176.
- Spivak, L. G., and P. M. Chute. 1994. “The Relationship Between Electrical Acoustic Reflex Thresholds and Behavioral Comfort Levels in Children and Adult Cochlear Implant Patients.” Ear and Hearing 15 (2):184–192. https://doi.org/10.1097/00003446-199404000-00008
- Spivak, L. G., P. M. Chute, A. L. Popp, and S. C. Parisier. 1994. “Programming the cochlear implant based on electrical acoustic reflex thresholds: patient performance.” The Laryngoscope 104 (10):1225–1230. https://doi.org/10.1288/00005537-199410000-00007
- Stephan, K., and K. Welzl-Müller. 1994. “Effect of Stimulus Duration on Stapedius Reflex Threshold in Electrical Stimulation via Cochlear Implant.” Audiology 33 (3):143–151. https://doi.org/10.3109/00206099409071875
- Stephan, K., and K. Welzl-Muller. 2000. “Post-operative Stapedius Reflex Tests with Simultaneous Loudness Scaling in Patients Supplied with Cochlear Implants.” Audiology 39 (1):13–18. https://doi.org/10.3109/00206090009073049
- Stephan, K., K. Welzl-Müller, and H. Stiglbrunner. 1988. “Stapedius Reflex Threshold in Cochlear Implant Patients.” Audiology : official Organ of the International Society of Audiology 27 (4):227–233. https://doi.org/10.3109/00206098809081593
- Stephan, K., K. Welzl-Müller, and H. Stiglbrunner. 1990. “Dynamic Range of the Contralateral Stapedius Reflex in Cochlear Implant Patients.” Scandinavian Audiology 19 (2):111–115. https://doi.org/10.3109/01050399009070761
- Van Den Abbeele, T., N. Noël-Petroff, I. Akin, G. Caner, L. Olgun, J. Guiraud, E. Truy, J. Attias, E. Raveh, E. Belgin, et al. 2012. “Multicentre investigation on electrically evoked compound action potential and stapedius reflex: how do these objective measures relate to implant programming parameters?” Cochlear Implants International 13 (1):26–34. https://doi.org/10.1179/1754762810Y.0000000001
- van den Borne, B., A. F. Snik, L. H. Mens, J. P. Brokx, and P. van den Broek. 1996. “Stapedius reflex measurements during surgery for cochlear implantation in children.” Am J Otol 17 (4):554–558.
- Walkowiak, A., A. Lorens, M. Polak, B. Kostek, H. Skarzynski, A. Szkielkowska, and P. H. Skarzynski. 2011. “Evoked stapedius reflex and compound action potential thresholds versus most comfortable loudness level: assessment of their relation for charge-based fitting strategies in implant users.” ORL; Journal for Oto-Rhino-Laryngology and Its Related Specialties 73 (4):189–195. https://doi.org/10.1159/000326892
- Wolfe, J., and H. Kasulis. 2008. “Relationships among objective measures and speech perception in adult users of the HiResolution Bionic Ear.” Cochlear Implants International 9 (2):70–81. https://doi.org/10.1179/cim.2008.9.2.70.
- Wolfe, J., M. Gilbert, E. Schafer, L. M. Litvak, A. J. Spahr, A. Saoji, and C. Finley. 2017. „“Optimizations for the electrically-evoked stapedial reflex threshold measurement in cochlear implant recipients.” Ear and Hearing 38 (2):255–261. https://doi.org/10.1097/AUD.0000000000000390
- Wolfe, J., R. Gifford, and E. Schafer. 2018. “Measurement of the electrically evoked stapedial reflex response with wideband acoustic reflectance measurement.” Journal of the American Academy of Audiology 29 (4):337–347. https://doi.org/10.3766/jaaa.16176
