Abstract
Objective
This study aimed to provide a conceptual model to understand what typifies the lived experience of hearing loss.
Design
A grounded theory informed study of adults with hearing loss (n = 46) who participated in individual interviews. The data were analysed in line with the constant comparative approach of grounded theory. A substantial patient and public engagement (PPIE) strategy underpinned decisions and processes throughout.
Study sample
Adults were recruited from age bands (16–29; 30–49;50–79 and 80 upwards) to provide different lived experience. We recruited individuals from across the UK including urban, sub-urban and rural communities and included a typical constituency of each location including black and minority ethnic participants. Our PPIE groups included adults often marginalised in research including South Asian community groups, adults in residential care and those with additional disabilities.
Results
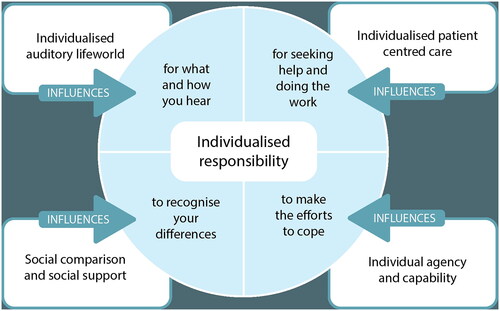
We identified the consistent features of the lived experience with hearing loss, as the individualised responsibility that hearing loss confers. These are an individual auditory lifeworld; social comparison and social support; individual and patient-centred care and individual agency and capability.
Conclusions
This work provides new insights for those practising audiology and highlights the importance of building social support systems through implementation of family and peer support approaches.
Background
One in two people over 70 experience hearing loss (World Health Organisation, Citation2018). The consequences of hearing loss extend beyond communication difficulties with far-reaching implications on various aspects of an individual’s life such as increasing social isolation, loneliness and increased rates of depression and falls (Arlinger, Citation2003; Scholes et al., Citation2018; Chen Citation1994). Hearing loss is both a core experience of ageing and has critical effects on social engagement (Chen, Citation1994; Shukla et al., Citation2020; Lawrence et al., Citation2020). Research has pointed towards an increased risk of dementia (Lin et al., Citation2011; Griffiths et al., Citation2020) and falls (Besser et al., Citation2018; Jiam et al., Citation2016) related to hearing loss.
Within the UK people with hearing loss are entitled to free provision of hearing aids on the National Health Service (NHS) and can also access Hearing Therapy interventions such as counselling, information provision and additional assistive listening devices, although access to these services varies by location (Hoare et al., 2015). To date complex patient lives and variations in hearing loss have been met by giving patients additional knowledge and skills training (Ferguson et al., Citation2016; Sweetow & Henderson-Sabes, Citation2004). Advances in evidence-based healthcare have emphasised the need to reduce burden on patients and to adapt services to meet individual needs rather than adapting individuals to meet the preferences of services, e.g., the ‘minimally disruptive medicine’ & ‘too much medicine’ movements (Glasziou et al., Citation2013; May et al., Citation2009; Leppin et al., Citation2015).
Patient centred audiological care has received increased attention over years (Gregory, Citation2012; Coleman et al., Citation2018; Erdman, Citation2014; Grenness et al., Citation2014). This drive is to include greater recognition of the role of the patient in achieving hearing care aims (e.g. hearing aid use) and positions patients as consumers of health services (Grenness et al., Citation2014). Patient centred care encompasses patient choice and promotes autonomy, but this may not be enough to integrate healthcare into an individual life. Some argue, the practice of patient-centred care in healthcare over emphasises illness and under emphasises the phenomenon of human agency and instead propose the notion of ‘lifeworld-led’ care. Lifeworld-led care aims for a deeper understanding of what health and wellbeing mean to the individual and how they relate to their health condition (Dahlberg et al., Citation2009). As a philosophical framework ‘Lifeworld’ is a term to describe a broader understanding than the classifications of function, disability and disease (ICF, WHO, Citation2018; Dahlberg et al., Citation2009) Lifeworld-led care recognises that an individual’s health and well-being are influenced by various factors, including their social, cultural, and environmental contexts. It acknowledges the interplay between a person’s condition and their life, understanding that addressing the challenges and promoting well-being requires considering the person holistically (Dahlberg et al., Citation2009). This provides a useful philosophy to base a biopsychosocial approach to healthcare in which social and psychological mechanisms are critical to understanding the experience of health conditions and their treatment. This is particularly important when exploring the unseen work of patients in managing their health conditions (May, 2009). As healthcare providers face an increasingly complex caseload with long term conditions, there has been a response to delegate the work of managing symptoms to patients and their support networks (May, 2009). Previous studies of audiology patients have highlighted the growing challenge of managing multiple health conditions and that the accumulation reduces capacity for coping (Laird et al., Citation2020). This is also true of audiological care in which patients are required to manage their symptoms through learning to use devices such as hearing aids, adjust communication and develop skills (Knudsen et al., Citation2013). Previous findings have highlighted the changes in response to health burdens over the life course (Namkung &Carr, 2020).
While there have been several investigations of lived experience in adults with acquired hearing loss, they tend to examine discrete populations, e.g. women participants in rehabilitation (Jonsson & Hedelin, Citation2018) or patients at specific centres (Khan et al., Citation2020; Pryce et al., 2016; Wänström at al., 2014). The research question of this study is: ‘What is the lived experience of adults with hearing loss, including those receiving audiology care?’
The Hearing Loss and Patient Reported Experience study (known as the HeLP study) is a National Institute of Health Research (NIHR) funded UK study (Health and social care Delivery Research study 131597). The HeLP study aims to develop a comprehensive model of lived experience of hearing loss and hearing care. The study consists of three connected studies of patient, carer and family experience of hearing loss and hearing care; the development of the first Patient Reported Experience Measure in audiology (known as a PREM) and the implementation of the PREM to clinical services in the UK. Further details are available in the protocol (Pryce et al., Citation2023a). This programme of work is key to acknowledging and understanding the unseen efforts made by patients to inform better services for managing hearing loss and increasing engagement with those services.
Methods
Design
Grounded theory is an approach to qualitative research that develops novel theories or models processes from data. This involves comparing summary themes to develop broader conceptual categories and then organising these categories in terms of explanation of variation. It differs from other forms of qualitative data synthesis (such as thematic analysis) by extending analysis beyond descriptive themes into a model (Strauss & Corbin, Citation1990). In this study we identified the categories that explained variance within the data set (in this case influenced the range of responses to changes in hearing). The final stage of grounded theory analysis (Strauss & Corbin, Citation1990) is to identify ‘negative cases’ - a form of deductive reasoning - to examine the model against new accounts that might challenge underlying assumptions. This version of grounded theory allows for (and recognises the likelihood of) researchers to bring previous knowledge and theory development to the process of refining theoretical concepts. This approach recognises the importance of prior expectation, knowledge etc. In this case the researchers include a Hearing Therapist (HP); a Clinical Scientist in Audiology (SH); Health Psychologists (SS and RS) and a sociologist with experience in hearing loss (GBOC). Thus, the team brought experience and knowledge about responses to illness and hearing loss. Our a priori assumptions included that acquired hearing loss is a complex experience that affects all communication, and that burden of care theory would apply to hearing loss (May, 2009; Pryce et al., Citation2023b).
Patient and Public Involvement and engagement (PPIE)
Our PPIE strategy prioritised the diverse and heterogeneous nature of the population affected by hearing loss in the UK. We developed our protocols in consultation with Patient and Public Involvement (PPIE) volunteers recruited through volunteer connections to Audiology services, and Aston University. Following their advice, we extended our PPIE groups, increasing the involvement from traditionally marginalised groups who are less likely to be involved with health research but more likely to be affected by hearing loss. We considered the populations in the UK more likely to be affected by hearing loss including people from South Asia (Indian, Pakistani and Bangladeshi communities) (WHO, Citation2018), older adults in residential care and adults with learning disabilities (WHO, Citation2018; Bent et al., Citation2015). By directly targeting these groups, we expanded the reach of our PPIE inclusion and range of views on the study. Our PPIE groups have provided insight into recruitment and sampling, it has informed our interview strategy, including topics, language and sensitivities around labelling individuals as having hearing ‘loss’ or ‘impairment’ (which were very unpopular terms with some groups). Furthermore, our PPIE leads have contributed to checking coding and analysis procedures and addressing uncertainties in interpretation of data. Our PPIE leads have contributed to all writing in the project to date.
Participants and setting
The study was conducted in the UK with participants (adults with hearing loss) recruited from three clinical sites in England (Bristol and Bath) and Scotland (Tayside) and non-clinical groups (e.g. lip reading classes).
The geographical spread of the different clinical sites (rural, urban and semi-urban) enabled us to achieve socioeconomic variation and find cases across a wide age range with contrasting features in terms of sex, income, housing and clinical needs. The participants were purposefully sampled to reflect different life stages. We grouped age bands as 16-29 years; 30-49 years- 50-79 years and 80+ years (see ). See supplementary files for Sampling taxonomy.
Table 1. Eligibility criteria for study participation.
Drawing on sampling principles of grounded theory, we used purposive sampling to provide maximum variation of cases to generate rich data from different backgrounds and perspectives thereby allowing us to target under-represented groups in the communities. Participants were invited to participate whether they used hearing aids (of any type) or not. Potentially eligible participants were made aware of the study through advertisements. Clinical sites in England and Scotland advertised the study to new and existing patients via word-of-mouth, invitation flyers and posters displayed in waiting/reception areas. Details of the study were circulated on social media (e.g. X/Twitter) and the study link hosted on Aston University website with the aim of recruiting participants with diverse experiences and backgrounds. In addition, our Personal and Public Involvement and Engagement (PPIEE) collaborator in South Asian community groups (e.g. exercise groups for older Asian women and mindfulness group for Asian women) prompted snowball sampling with word-of-mouth advertisement to encourage potential participants to contact the study team.
Interested participants made direct contact with the HeLP study team via email, phone or post. Potential participants were asked their age and invited to participate. The researchers provided potentially eligible participants with the participant information sheet and obtained informed consent from them at the start of an interview.
Data collection
Ethical approval was granted by the West of Scotland Research Ethics Service (22/WS/0057) and the Health Research Authority and Health and Care Research Wales Approval (IRAS project ID: 308816).
Potential participants volunteered to take part in the study. Individual interviews were carried out in person, at the participant’s home, on clinical sites or online in accordance with the participant preference. Participants were encouraged to describe their lifeworld with hearing loss. Four researchers conducted interviews in different locations in England and Scotland (HP,SH,GBOC,SS). All researchers followed the same interview schedule to ensure consistency of topic but were steered in each case by the responses of the participant. The interview schedule was devised following PPIE consultation with a wide range of people affected by hearing loss, both help-seekers and non-help-seekers from a range of ages and backgrounds. Feedback from the PPIE groups suggested that researchers should use terminology to describe hearing and hearing loss that was used by participants, be led by participants on communication needs and be sensitive to the impact of the questions they were asking. Participants were recruited through word of mouth at Birmingham City Council, lip-reading classes nationally, clinical services in Birmingham, Scotland, London, Bristol and Bath. Volunteers directly contacted the research team and were invited to participate based on age stratification.
Interviews were audio recorded and transcribed verbatim. Interviews followed a common schedule of topics, but questions varied depending on participant responses and interviews were as participant led as possible to facilitate the aim of inducting new insights and priorities from participant views. For full protocol please see Pryce et al. (Citation2023c).
Data analysis
Data analysis involved all researchers plus PPIE leads. It followed the interview schedule described in and the analysis process described in . Our sample are described in . No qualitative analysis software were used in this analysis process as the four researchers coded their own transcribed interviews and then blind coded a selection (approximately a third) of each other’s using MS word and Google jam board to group clusters of codes into themes. The blind coding was intended to check and cross check interpretations of meaning statements and salient content in the transcripts. There were no significant disagreements with interpretation but open discussions to confirm interpretation took place between the researchers and PPIE lead to allow an open and transparent process of researcher interpretation.
Table 2. Interview schedule.
Table 3. The process of data analysis.
Table 4. Participant details.
Findings
All 46 participants in this study had a diagnosed hearing loss, 34 participants used hearing aids (including 33 who used conventional hearing aids and 1 who used a Bone Anchored Hearing Aid (BAHA). The others chose not to use hearing devices including another participant who had been prescribed BAHA Twenty-six were recruited from non-clinical routes and community advertisement, 20 were recruited between the clinical sites in England and Scotland. Eleven individuals in our sample spoke both as individuals with hearing loss and as partners, parents or carers of others with hearing loss. We recruited from 7 regions of England (contrasting locations in England including Southwest and Midlands, northeast, South East and mid Scotland) including postcode districts with stable and affluent communities and communities with high levels of private renting and social housing and low-income districts. We include participants from a range of black and minority ethnic backgrounds.
The process of experiencing hearing loss – an individualised responsibility
Analysis of these data comprised comparison of meaning statements and collating common factors that influenced the process of living with hearing loss and influenced the experience of living with hearing loss. Initially codes summarising meaning statements were collated and compared within and between accounts. We then identified the relationship between groups of codes (or categories) and identified the categories that explained the variance within the data set. This resulted in the creation of a model, depicted in . The model comprises one core category, common to all data and providing explanation of variance within the data set as a whole. The core category is contingent on the four surrounding categories which describe the constituent commonalities in experience of hearing loss.
The data emphasised the individualised nature of the experience of hearing loss as the most consistent and explanatory factor, hence its place in the centre of the model. We examined contrasting cases (in the sense of grounded theory ‘negative cases’) including people who were required to take less responsibility for their hearing care alone (e.g. teenagers with parents who support and initiate their care). The four categories feeding into Individual responsibility represent constituents of hearing loss that are inextricably linked to an individual’s ability to take individual responsibility. For instance, the variation in individual responsibility profoundly changes the nature of the experience in that the symptoms and adaptations to the symptoms rely on social comparison and social support. The model links the individual auditory lifeworld and amount of functional hearing difficulty. The way hearing loss is experienced is contingent on social comparison and social support mechanisms and variance in individual agency and capability. Furthermore, participants describe individualised and patient centred care as contributing to the sense of individual responsibility. Below we describe the individual model components and provide example quotations to illustrate how these factors manifest in the lived experience.
Individualised responsibility
The core category in these data is that which explains variances within the data set and appears in every account: individualised responsibility. This term refers to experiencing personal responsibility for coping, care, management, adjustment to sound etc. This is reinforced via social and communicative isolation and individualised approaches to care. Both the sense that this is an individualised experience, e.g. no one can share full insight into how the affected individual perceives the world, and that the individual is held permanently responsible for coping with the experience, are the key factors that underpin all variations in how hearing loss is experienced.
An example of the individualised responsibility for communication repair is expressing feelings of guilt about not hearing and creating communicative breakdowns.
‘They’re [family] fed up by it all the time… [daughter] said “your hearing aid’s whistling again” and because I keep saying “speak up, I can’t hear you”, that gets irritating for them obviously.’ (Participant 39; age range 50-79)
Participants describe the tacit decision making about use of strategies in the light of the effort required of others.
‘At that moment in time there is no answer, you know, you can’t… there is a limit to the number of times you would say “oh sorry I missed what, can you say it again?” There is a limit to that.…, but if you desperately need, can move on and not bother with understanding what they were saying to you, well there are times when you just do that. And sometimes I will say to my wife after “what did they say?” and then get it repeated and get an edited version of it because I wasn’t with what they were saying. She feels irritated.’ (Participant 38; age range 80+)
The participants describe the effort of repairing conversation as reinforcing a separation from others.
‘And they’re all fed up with me going on about my hearing.’ (Participant 42; age range 80+)
‘That I was then like oh missed all that conversation. And then I didn’t want to have to tell people I’d try and like, just like, ohh what did you say? But you can only ask that so many times before someone’s like, what is wrong with you?’ (Participant 26; age range 16-29)
The narrative description of how hearing loss forms part of individual identity is mediated by social comparison within the individual lifeworld, e.g. hearing loss affects people like me, I am more affected in this way but less in that way in comparison to others. For example, these participants make sense of their own hearing loss through comparison with others.
‘He must have only been about 21 years old and he was the leading bass in the choir and he was deaf in one ear and I talked to him about it and he’d been deaf from birth and so he said he didn’t find it at all you know, a problem, and I just found that amazing…’ (Participant 31; age range 50-79)
‘My mother. I mean. hearing was probably the same as mine. Terrible. She never wore a hearing aid….And she never admit to having a hearing problem.’ (Participant 34; age range 50-79)
‘Our hearing loss sort of seems to be for different things. He [referring to husband] can hear the front doorbell, but I can’t, he said. Didn’t you hear that? And then I was things I can hear and he can’t.’ (Participant 30; age range 50-79)
‘And I think knowing that my dad for so long, he didn’t wear them (hearing aids). He put them in the drawer and now he does wear them in his 60s, but he’s just become a very quiet person because he was alone and quiet for so long. I mean, he’s an introvert and that’s fine, but I'm just aware that not having that help I think has shaped his character and has shaped our family dynamic because he’s not used to engaging in conversations around the table.’ (Participant 47; age range 30-49)
These data suggest that behaviours of disengagement with hearing aids are not the result of individual motivations alone but are the result of a system dependent on individual patient agency and capability to take responsibility for care.
‘I have now asked three times for you to find out how to switch on the induction loop. Why haven’t you done it?’ (Participant 31; age range 50-79)
‘The onus is on that one individual. In a social situations where I don’t know the other people, it is absolutely on me.’ (Participant 17; age range 30-49)
‘And I shouldn’t have to say all the time. I can’t hear you.’ (Participant 43; age range 30-49)
This respondent describes their process in accessing and using hearing aids.
‘So, I’ve had to be quite clear about what I need, but I did have to go through a long process and quite a few tears in order to get to the point where I could do that because at one point I was very low and I honestly just saw it as a reflection on me and I do go back to that position sometimes if I’m stressed or tired, which is another reason why I need to keep building myself up, and that’s OK because it’s, yeah, I needed to find strategies to cope with work.’ (Participant 4; age range 50-79)
Again, it is striking how this is considered by participants to be an individual responsibility. Note the use of ‘I’ throughout.
Similarly, participants describe a sense of being responsible to access care. Therefore, provision and use of services depend on the individual assuming the responsibility required to use services.
‘It’s on you to sort of keep at the, you know, the maintenance and contact with the hearing doctors or audiology doctors.’ (Participant 21; age range 30-49)
The individual responsibility is clear throughout these quotations, and this is informed by the categories described in the next section.
Individual auditory lifeworld
Hearing loss has at the core of the experience an altered acoustic perception of sound. This is different from other people’s perceptions and from the way things used to be for the individual who acquires their hearing loss, an immediately individualised experience. The changes to hearing fundamentally alter the way individuals experience the world around them. Depending on the type and severity of hearing loss, certain frequencies or ranges of sound may become distorted or entirely inaccessible. This altered perception can lead to challenges in understanding speech, discerning environmental sounds, and experiencing music or other forms of auditory pleasure.
‘I woke up one day and, very early, and suddenly the dawn chorus started and I thought, that’s strange you know, I’m used to living kind of in the countryside but I’ve never known the dawn chorus to start, all the birds to sing simultaneously, I thought that is extraordinary, and I, then suddenly it occurred to me I’d turned over in bed and it stopped and I then realised that I’d heard, when I’d woken up and I’d turned on to my back, I turned over, and I’d released, I wasn’t hearing in one ear and that’s why you know, everything was peaceful and as soon as I turned over then the sound came into the other ear obviously altogether.’ (Participant 39; age range 50-79)
The auditory lifeworld encompasses the unique subjective experiences and perspectives of individuals living with this condition. This describes the profound impact of hearing loss on the perception of sound, the process of adjusting to a new auditory reality. What follows is an adjustment to the emotional significance of sound, changes in identity and self-concept, and the subsequent reconstruction of the auditory lifeworld.
‘I woke up one morning when I was 39 and my hearing had gone. So I've been living with this for a little over 20 years. I've got used to it now. But there’s a whole bunch of things that I've had to get used to.’ (Participant 31; age range 50-79).
In every case this variation leads to a sense of being separate from the other people and features of the environment. Hearing aids and distinct amplified sounds enhance this difference from the way others hear.
‘They’re too crackly, they’re too noisy, and whether that’s normal for most people to hear those things but to me it’s I can’t live with it. They’re too crackly. It’s like cutlery and packet of crisps being opened all the time. Yeah, it’s too noisy for me.’ (Participant 30; age range 50-79)
‘I got this hearing aid and I put it in and I walked down the road and a lorry nearly blew my head off. It’s the noise. It was just awful, so I took that out. So it was a long time again before I kind of thought I need to do something.’ (Participant 32; age range 50-79)
‘So when it comes to conversation. You’re piecing the words together and there were certain syllables that you don’t hear as well.’ (Participant11; age range 30-49)
Individuals with acquired or progressive hearing loss often describe a period of adjustment as they adapt to a new auditory reality. This adjustment encompasses both the physical aspects, such as learning to use hearing aids or cochlear implants effectively, and the psychological, including coming to terms with the limitations imposed by hearing loss and finding new ways to engage with the world.
‘My main thing is I always hated when anything changed. I always hated going from one hearing aid to a different hearing aid and things sounding different.’ (Participant 12; age range 16-29)
The loss or alteration of certain sounds can lead to a range of emotional responses, including grief, frustration, and a sense of disconnection. Conversely, certain sounds, such as those associated with communication or nature, may acquire heightened emotional significance for individuals with hearing loss. The experience is typified by separation from others and a loss of shared understanding of the problems an individual with hearing loss faces.
‘You know, missing things when it’s like people talking in a group and things like that. I guess I don’t feel like 100% fit in.’ (Participant 12; age range 16-29)
‘There’s this frustration when you’re hearing the certain volume of noise coming from them but you’re not, you’re losing the ability to translate that volume of noise into meaningful thoughts, you know, because you can genuinely say to them “yes I hear you, I don’t understand you”. I‘m not able to follow the thread, particularly if someone has switched subject’. (Participant 38; age range 80+)
The specific auditory encounters contribute to a growing sense of difference from others and thus the ‘individualised’ nature of the hearing loss. The expectation that the individual will self-manage this as illustrated above contributes to the sense of responsibility.
Social comparison and social support
Social comparison is a coping process through which individuals compare their situation and apparent hearing function with others they know (Carson, Citation2005). This influences symptom detection, coping behaviours and internal interpretation. We noticed examples of social comparison throughout the data set. Social comparison contributed to the core category by determining, in part, when and how an individual decided to act.
‘You’re in much worse situation than I am in terms of hearing things.’ (Participant 1; age range 30-49)
‘I had a partner a few years ago who was playing with me a game of doubles and she was standing near the net and I was serving, and I was shouting at her, you know, to do something, and she couldn’t hear me, you know, and in the end I was shouting really, really loud, and she couldn’t hear me, you know, so I mean my hearing loss has never been anything like that, you know? You know, well I presume she wasn’t wearing hearing aids, but even so…’ (Participant 24; age range 80+)
Participants describe how hearing loss can profoundly impact a sense of identity. This can involve grappling with feelings of diminished self-worth, questioning one’s capabilities, and negotiating a new sense of identity that incorporates hearing loss as a part of one’s lived experience. This leads to a sense of responsibility for difference.
‘I didn’t want to wear the hearing aids because I felt like I was different to everybody else.’ (Participant 12; age range 16-29)
This concern about difference is described in other accounts as a cognitive activity and a form of sense making about how the hearing loss alters them as an individual.
‘My identity in terms of my hearing loss was completely……I I was just lost in that sense…. I was figuring out coping skills myself. …. I’m not part of the deaf hearing, but I’m also not part of the hearing community either.’ (Participant 17; age range 30-49)
This sense making was described as intertwined with the requirement to work on finding out about support options as described here.
‘I still find it a very separate part of me. Sometimes it is hard to know what’s out there and what’s available.’ (Participant 21; age range 30-49)
Participants described these on-going efforts as linked to a sense of frustration at being held individually responsible for restoring communication.
‘I've I'm more resigned obviously to being deaf. Because I've had it for so long. But what angers me is the lack of consideration for those of us who do have problems.’ (Participant 15; age range 50-79)
The category of social comparison included reports of not hearing, missing out and becoming separated to those around them. As an example, one participant referred to losing a job. Here the social comparison clearly leads to a sense of individual responsibility.
‘I thought that I was such a failure, because I've managed every other job with my hearing loss, but then obviously it’s got worse as the years have gone on.’ (Participant 45; age range 30-49)
Participants describe their variation in experiences based on the level of social support they report.
‘I don’t get embarrassed until I get home and then, you know, my wife said, “didn’t you hear this and didn’t you hear that? You were quiet, you didn’t say much.” And it’s because I can’t join in the conversations with everybody when you’re talking across the table and there’s four or five people all talking at the same time.’ (Participant 23; age range 80+)
The mechanisms by which social isolation occurs are based on the separation from others that occurs through not hearing well.
‘I feel very cut off.’ (Participant 35; age range 80+)
What was described as helping this sense of isolation were displays of support from others and a sense of social connection.
‘Yeah, we’re a very open family, we have conversations like that about lots of different things. But yeah, I've sat and talked to them both. [Dad and sister who both have hearing loss]’ (Participant 9; age range 50-79)
What is striking is that across the life course the experience of living with hearing loss is described as acutely personal, challenging the sense of self and perceived - by clinicians, family and friends and affected individuals - as the responsibility of the person with hearing loss. Family and friends can be helpful in relieving the miss-hearing occurrences or providing practical help with hearing aids or help-seeking but not hearing remains an individual’s responsibility.
Individual agency and capability
The system depends on individuals accepting their responsibility for managing their hearing and seeking help. This relies on individual resources.
‘It’s down to you to learn to deal with things and it’s your problem, not anybody else’s if that makes sense?’ (Participant 43; age range 30-49)
The buffer of social support was particularly evident with individuals in their late teens whose parents directed their audiological care and managed their use of devices. For example, note the passive voice when describing this coping strategy:
‘I'm still included cause I'm always put to the front of the class cause of my hearing, so I'm always right by the teacher.’ (Participant 28; age range 16-29)
‘I think you know, because it was all me doing all of the chasing and the following up and thinking.’ (Participant 9; age range 50-79)
Individualised and patient centred care
One of the paradoxes of audiology care in the UK is that, with a heavy focus on individual prescription of hearing aids, the sense of individual responsibility for management is reinforced and the potential for social support and social connectedness is diminished or untapped entirely. For example group support, assistive listening devices, lip-reading classes are not routinely included in NHS audiology provision.
The individual is responsible for adapting to the auditory changes, without additional support. Such changes can be difficult.
‘The service is quite one-size-fits-all and all that it fits is very old people or you know not very old people, but people who are older than me. And they didn’t seem to be much flex in the system for the fact that I was entering it. And I really felt like quite desperate, like sitting in front of this woman and saying you don’t understand I need to go to work. I need to go to social events.’ (Participant 46; age range 30-49)
Good quality audiological care, such as changing or upgrading hearing aids, result in extra work for the patient in adapting to the new sounds. The responsibility for coping with this work is perceived as theirs alone.
‘Look I can hear but at the same time I can’t hear because there’s noise going on around me so, you know, I struggle to hear. ’ (Participant 43, age range 30-49)
Despite the challenges posed by hearing loss, individuals often find ways to reconstruct their auditory lifeworld. This may involve developing new communication strategies, utilising assistive technologies, seeking support from peers, professionals, and advocacy organisations. Through these efforts, individuals with hearing loss describe how they can actively participate in and contribute to various domains of life, including education, work, relationships, and social activities.
‘To be honest I’m not sure actually how much actually we’re learning to lip read, but it’s more to be part of the hearing community so I mean it is helpful and they’ve actually, they’ll teach us little tricks and things like that to recognise lip shapes and it’s more to hear that you’re not alone in the difficulties you experience and that I find, we both find very, very valuable.’ (Participant 16; age range 50-79)
These data illustrate that person-centred care reinforces the individualised nature of the health experience by placing the individual at the centre of their care. This preserves autonomy but comes at a cost in terms of reinforcing the individual responsibilities that each person has and delegating the work of coping with hearing loss exclusively to the individual.
Discussion
This qualitative study presents a novel theoretical model, grounded in data. Researchers cross checked their interpretation of data by blind coding a selection of each others’ transcripts. This work presents data on analysed accounts from 46 participants and was also informed by a strong PPIE component in which our analysis processes were examined. We included both clinical help-seekers and non-help-seekers in our sample and there was little variation in reported lived experience. We sampled a diverse set of participants across life course bands, expecting substantial variation in the experience of people in their 20s and people in their 90s. Whilst hearing aids were considered to provide some important benefit, there were substantial difficulties that remained with hearing loss and hearing aid use was effortful. The preservation of individual dignity was challenged by instances of not hearing and the use of hearing aids. Indeed, these findings map onto the concept of dignity in health literature.
The Universal Declaration on Human Rights stresses the role of dignity as a core right (Mann, Citation1998). This is described as comprising two dimensions; internal (how I see myself) and external (how others see me) (Mann, Citation1998). The descriptions of managing dignity resonate with categories in this model of lived experience of hearing loss. The auditory lifeworld concept touches on internal dignity – I have responsibility for what and how I hear. Likewise social comparison and agency and choice on managing behaviour changes to adapt to hearing loss do so to preserve external dignity (how other see me) (Mann, Citation1998). This suggests a degree of fittingness in our model (Polit & Beck, Citation2010). Preserving dignity should be a key aim of healthcare. Descriptive taxonomies of behaviours that support and violate dignity provide guidance on how people with hearing loss could be supported (Jacobson, Citation2009).
The chronicity, the ongoing challenge to every auditory aspect of life is a profound experience which challenges dignity. Our study describes how individuals who do not hear well often experience challenges and violations to dignity such as dismissal, condescension, diminishment of their experience or are disregarded (Jacobson, Citation2009) This is often forgotten in prioritising autonomy and reliance on technological hearing aid developments. Whilst use of hearing aids was reported as helpful, they incurred additional efforts on the part of the individual.
Our a priori assumptions had been that life course stage would significantly impact the experience of living with hearing loss. We were surprised that this was not the case. There was little variation in terms of the core elements of the experience. Participants aged 16- 80+ years describe efforts to manage hearing loss around others and to work at reducing communication breakdown. The levels of social comparison and social support vary individually, but patterns were not evident by age band. There was no increase in social support for sharing of hearing loss and wider communication problems by any group within our sample, or in the experience of any of our PPIE contributors. Whilst life worlds vary the experience of hearing loss as an individualised responsibility remains. The other a priori assumption was that illness and treatment burden would be evident in our participants in line with burden of care theory (May, 2009). These data provide evidence of the illness and treatment burden of hearing loss and the individualised responsibility that characterises it. Earlier qualitative studies also highlight the work of hearing loss (Knudsen et al., Citation2013). We have expanded on these descriptions and proposed an analysis of how this occurs and is maintained. The most important contribution of this model is identifying the workload and responsibility that is devolved to the individual when hearing loss is present. Any additional individualised intervention risks enhancing rather than reducing this burden and challenging internal and external dimensions of dignity.
Audiological care relies on the unseen labour of individual patients, who manage communication, work at using devices and adapt behaviour. Audiological researchers and clinicians should be wary of increasing tasks, technology, and responsibility to the individual as this diminishes dignity (Jacobson, Citation2009). Conversely activities which support and build resource in health literacy are likely to increase positive social comparison and agency of the individual by preserving dignity (Jacobson, Citation2009).
The participants in this study describe resources that help with managing the work of hearing loss. Family, or peer support and social contact are the characteristics that make it more likely an individual will manage hearing aids. This suggests that there is the potential of clinical providers to engage in resource building interventions through supportive relationships.
Models of family centred care broaden the individual approach and demonstrate a shared responsibility for communication (Ekberg et al., Citation2015; Meyer et al., Citation2019). Such approaches deserve greater exploration in UK provision. In other chronic health conditions such as asthma, epilepsy and diabetes there has been some evidence of benefit from social support interventions (Gallant, Citation2003). Groups and social support targets have been demonstrated to improve family and friends support (Hogan et al., Citation2002). Furthermore, trends in NHS primary care practice towards ‘social prescribing’ where individuals are referred to non-clinical social activities and groups could be an opportunity to build social support for those with hearing loss (Kings Fund, Citation2023). With related difficulties, such as tinnitus, peer support improves coping and adaptation (Pryce & Shaw, Citation2019). Evidence from complex health conditions proposes that efforts to routinise management tasks (e.g. setting consistent times of week to change batteries), increasing social support, clinicians providing emotional support and well-coordinated care that is easy to access can help reduce treatment burdens (Ridgeway et al., Citation2014).
Conclusions
Audiology provision would benefit from a recognition of the efforts made by individuals with hearing loss to manage their day-to-day function and consideration of ways to preserve dignity in healthcare (Jacobson, Citation2009; Mann, Citation1998).
Family centred approaches, support groups and therapeutic support in managing the burden of treatment could provide valuable care for individuals beyond the fitting of devices. Drives to improve health literacy and support informed shared decision making in audiology are low-cost changes that could lead to improved patient outcomes (Lesage et al., Citation2021). Simple interventions such as ‘offer conversation not information’ would assist clinicians in tailoring interventions to reduce burdens on patients (Hargraves et al., Citation2016).
Greater exploration of the burden of treatment in audiology is warranted and fits with the growing recognition that multimorbidity and cumulative efforts impact access and use of healthcare (Leppin et al., Citation2015). Audiological care should include a recognition of the individualised experience of hearing loss and explicit provision to building support.
Supplemental Material
Download MS Word (13.6 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Arlinger, S. 2003. “Negative Consequences of Uncorrected Hearing Loss-A Review.” International Journal of Audiology 42 (sup2):17–20. 1; https://www.researchgate.net/profile/Stig-Arlinger/publication/10612964_Negative_consequences_of_uncorrected_hearing_loss_-_A_review/links/0912f502caf00a31ce000000/Negative-consequences-of-uncorrected-hearing-loss-A-review.pdf. https://doi.org/10.3109/14992020309074639.
- Bent, S., L. McShea, and S. Brennan. 2015. “The Importance of Hearing: A Review of the Literature on Hearing Loss for Older People with Learning Disabilities.” British Journal of Learning Disabilities 43 (4):277–284. https://doi.org/10.1111/bld.12148.
- Besser, J., M. Stropahl, E. Urry, and S. Launer. 2018. “Comorbidities of Hearing Loss and The Implications of Multimorbidity for Audiological Care.” Hearing Research 369:3–14. https://doi.org/10.1016/j.heares.2018.06.008.
- Braun, V., and V. Clarke. 2021. “To Saturate or Not to Saturate? Questioning data saturation as a Useful Concept for Thematic Analysis and Sample-Size Rationales.” Qualitative Research in Sport, Exercise and Health 13 (2):201–216. https://doi.org/10.1080/2159676X.2019.1704846.
- Carson, A. J. 2005. “What Brings You Here Today?” The Role of Self-Assessment in Help-Seeking for Age Related Hearing Loss.” Journal of Aging Studies 19 (2):185–200. https://doi.org/10.1016/j.jaging.2004.07.001.
- Chen, H. L. 1994. “Hearing in the Elderly: Relation of Hearing Loss, Loneliness, and Self-Esteem.” Journal of Gerontological Nursing 20 (6):22–28. 3 https://doi.org/10.3928/0098-9134-19940601-07.
- Coleman, C. K., K. Muñoz, C. W. Ong, G. M. Butcher, L. Nelson, and M. Twohig. 2018. “Opportunities for Audiologists to Use Patient-Centred Communication During Hearing Device Monitoring Encounters.” Seminars in Hearing 39 (1):32–43. https://digitalcommons.usu.edu/cgi/viewcontent.cgi?article=2642&context=psych_facpub. https://doi.org/10.1055/s-0037-1613703.
- Dahlberg, K., L. Todres, and K. Galvin. 2009. “Lifeworld-Led Healthcare is More Than Patient-Led Care: An Existential View of Well-Being.” Medicine, Health Care, and Philosophy 12 (3):265–271. https://doi.org/10.1007/s11019-008-9174-7.
- Ekberg, K., C. Meyer, N. Scarinci, C. Grenness, and L. Hickson. 2015. “Family Member Involvement in Audiology Appointments with Older People with Hearing Impairment.” International Journal of Audiology 54 (2):70–76. https://doi.org/10.3109/14992027.2014.948218.
- Erdman, S. A. 2014. “The Biopsychosocial Approach in Patient- and Relationship-Centred Care: Implications for Audiologic Counselling.” In Adult audiologic rehabilitation, edited by J. J. Montano & J. B. Spitzer ,159–206. San Diego,CA: Plural Publishing Inc. ISBN 9781635501438
- Ferguson, M., M. Brandreth, W. Brassington, P. Leighton, and H. Wharrad. 2016. “A Randomized Controlled Trial to Evaluate the Benefits of a Multimedia Educational Program for First-Time Hearing Aid Users.” Ear and Hearing 37 (2):123–136. https://doi.org/10.1097/AUD.0000000000000237.
- Gallant, M. P. 2003. “The Influence of Social Support on Chronic Illness Self-Management: A Review and Directions for Research.” Health Education & Behavior: The Official Publication of the Society for Public Health Education 30 (2):170–195. https://doi.org/10.1177/1090198102251030.
- Glasziou, P., R. Moynihan, T. Richards, and F. Godlee. 2013. “Too Much Medicine; Too Little Care.” BMJ (Clinical Research ed.) 347 (2):f4247–f4247. https://doi.org/10.1136/bmj.f4247.
- Gregory, M. 2012. “A Possible Patient Journey: A Tool to Facilitate Patient-Centred Care.” Seminars in Hearing 33 (01):009–015. https://doi.org/10.1055/s-0032-1304723.
- Grenness, C., L. Hickson, A. Laplante-Lévesque, and B. Davidson. 2014. “Patient-Centred Care: A Review for Rehabilitative Audiologists.” International Journal of Audiology 53 (Supp 1):S60–S67. https://doi.org/10.3109/14992027.2013.847286.
- Griffiths, T. D., M. Lad, S. Kumar, E. Holmes, B. McMurray, E. A. Maguire, A. J. Billig, and W. Sedley. 2020. “How Can Hearing Loss Cause Dementia?” Neuron 108 (3):401–412. https://doi.org/10.1016/j.neuron.2020.08.003.
- Hargraves, I., A. LeBlanc, N. D. Shah, and V. M. Montori. 2016. “Shared Decision Making: The Need for Patient-Clinician Conversation, Not Just Information.” Health Affairs (Project Hope)35 (4):627–629. https://doi.org/10.1377/hlthaff.2015.1354.
- Hogan, B. E., W. Linden, and B. Najarian. 2002. “Social Support Interventions: Do They Work?” Clinical Psychology Review 22 (3):383–442. https://doi.org/10.1016/S0272-7358(01)00102-7.
- Jacobson, N. 2009. “A Taxonomy of Dignity: A Grounded Theory Study.” BMC International Health and Human Rights 9 (1):3. https://doi.org/10.1186/1472-698X-9-3.
- Jiam, N. T. L., C. Li, and Y. Agrawal. 2016. “Hearing Loss and Falls: A Systematic Review and Meta‐Analysis.” The Laryngoscope 126 (11):2587–2596. https://doi.org/10.1002/lary.25927.
- Jonsson, I., and B. Hedelin. 2018. “Women’s Lived Experiences of Disabling Hearing Loss in Daily Life.” Scandinavian Journal of Disability Research 20 (1):111–119. https://doi.org/10.16993/sjdr.39.
- Khan, A., N. Mubdi, A. Budnick, D. R. Feldman, S. W. Williams, S. Patel, and E. S. Tonorezos. 2020. “The Experience of Hearing Loss in Adult Survivors of Childhood and Young Adult Cancer: A Qualitative Study.” Cancer 126 (8):1776–1783. https://doi.org/10.1002/cncr.32698.
- Kings Fund 2023. What is Social Prescribing? https://www.kingsfund.org.uk/publications/social-prescribing. Accessed 12/9/2023
- Knudsen, L. V., C. Nielsen, S. E. Kramer, L. Jones, and A. Laplante-Lévesque. 2013. “Client Labor: Adults with Hearing Impairment Describing Their Participation in their Hearing Help-Seeking And Rehabilitation.” Journal of the American Academy of Audiology 24 (3):192–204. https://doi.org/10.3766/jaaa.24.3.5.
- Laird, E. C., R. J. Bennett, C. M. Barr, and C. A. Bryant. 2020. “Experiences of Hearing Loss and Audiological Rehabilitation for Older Adults with Comorbid Psychological Symptoms: A Qualitative Study.” American Journal of Audiology 29 (4):809–824. https://doi.org/10.1044/2020_AJA-19-00123.
- Lawrence, B. J., D. M. P. Jayakody, R. J. Bennett, R. H. Eikelboom, N. Gasson, and P. L. Friedland. 2020. “Hearing Loss and Depression in Older Adults: A Systematic Review and Meta-analysis.” The Gerontologist 60 (3):e137–e54. https://doi.org/10.1093/geront/gnz009.
- Lesage, A., B. Leclère, L. Moret, and C. Le Glatin. 2021. “Decreasing patient-reported burden of treatment: a systematic review of quantitative interventional studies.” PLOS One 16 (1):e0245112. https://doi.org/10.1371/journal.pone.0245112.
- Leppin, A. L., V. M. Montori, and M. R. Gionfriddo. 2015. “Minimally Disruptive Medicine: A Pragmatically Comprehensive Model for Delivering Care to Patients With Multiple Chronic Conditions.” Healthcare 3 (1):50–63. https://doi.org/10.3390/healthcare3010050.
- Lin, F. R., E. J. Metter, R. J. O'Brien, S. M. Resnick, A. B. Zonderman, and L. Ferrucci. 2011. “Hearing Loss and Incident Dementia.” Archives of Neurology 68 (2):214–220. https://doi.org/10.1001/archneurol.2010.362.
- May, C., V. M. Montori, and F. S. Mair. 2009. “We need minimally disruptive medicine.” BMJ (Clinical Research ed.)339 (2):b2803–b2803. https://doi.org/10.1136/bmj.b2803.
- Mann, J. 1998. “Dignity and health: The UDHR's revolutionary first article.” Health and Human Rights 3 (2):30. https://www.jstor.org/stable/4065297. https://doi.org/10.2307/4065297.
- Meyer, C., N. Scarinci, and L. Hickson. 2019. Patient and family-centred speech-language pathology and audiology. New York, NY, United States: Georg Thieme Verlag. https://doi.org/10.1055/b-006-161149.
- Polit, D. F., and C. T. Beck. 2010. “Generalization in Quantitative and Qualitative research: Myths and Strategies.” International Journal of Nursing Studies 47 (11):1451–1458. https://doi.org/10.1016/j.ijnurstu.2010.06.004.
- Pryce, H., and R. Shaw. 2019. “Lifeworld Interpretation of Tinnitus.” Medical Humanities 45 (4):428–433. https://doi.org/10.1136/medhum-2019-011665.
- Pryce, H., T. Moutela, C. Bunker, and R. Shaw. 2019. “Tinnitus Groups: A Model of Social Support and Social Connectedness from Peer Interaction.” British Journal of Health Psychology 24 (4):913–930. https://doi.org/10.1111/bjhp.12386.
- Pryce, H., S. K. Smith, G. Burns-O'Connell, R. Shaw, S. Hussain, J. Banks, A. Hall, R. Knibb, R. Greenwood, and J. Straus. 2023a. “Protocol for a Qualitative Study Exploring the Lived Experience of Hearing Loss and Patient Reported Experience in the UK: The HeLP Study.” BMJ Open 13 (6):e069363. https://doi.org/10.1136/bmjopen-2022-069363.
- Pryce, H., N. Dauman, and G. Burns O’Connell. 2023b. “What is the Burden of Tinnitus?” Frontiers in Psychology 13:981776. https://doi.org/10.3389/fpsyg.2022.981776.
- Pryce, H., S. K. Smith, G. Burns-O'Connell, R. Knibb, R. Greenwood, R. Shaw, S. Hussain, J. Banks, A. Hall, J. Straus, et al. 2023c. “Protocol for the Development and Validation of a Patient-Reported Experience Measure (PREM) for People with Hearing Loss: the PREM-HeLP.” BMJ Open 13 (11):e075229. https://doi.org/10.1136/bmjopen-2023-075229.
- Ridgeway, J. L., J. S. Egginton, K. Tiedje, M. Linzer, D. Boehm, S. Poplau, D. R. De Oliveira, L. Odell, V. M. Montori, and D. T. Eton. 2014. “Factors That lessen the Burden of Treatment in Complex Patients with Chronic Conditions: A Qualitative Study.” Patient Preference and Adherence 8:339–351. https://doi.org/10.2147/PPA.S58014.
- Scholes, S., J. Biddulph, A. Davis, and J. S. Mindell. 2018. “Socioeconomic Differences in Hearing Among Middleaged and Older Adults: Cross-Sectional Analyses Using the Health Survey for England.” BMJ Open 8 (2):e019615. 4. https://bmjopen.bmj.com/content/8/2/e019615. https://doi.org/10.1136/bmjopen-2017-019615.
- Shukla, A., M. Harper, E. Pedersen, A. Goman, J. J. Suen, C. Price, J. Applebaum, M. Hoyer, F. R. Lin, and N. S. Reed. 2020. “Hearing Loss, Loneliness, and Social Isolation: A Systematic Review.” Otolaryngology-Head and Neck Surgery: official Journal of American Academy of Otolaryngology-Head and Neck Surgery 162 (5):622–633. https://doi.org/10.1177/0194599820910377.
- Strauss, A., and J. Corbin. 1990. Basics of qualitative research. Thousand Oaks: Sage publications. ISBN 0-8039-5939-7
- Sweetow, R. W., and J. Henderson-Sabes. 2004. “The case for LACE: Listening and auditory communication enhancement training.” The Hearing Journal 1 (3):32–35. 57https://citeseerx.ist.psu.edu/document?repid=rep1&type=pdf&doi=e43bf5a78b0a8fa7f47f0c9c28de2ad5cf113a99.
- World Health Organisation (WHO). 2018. Addressing the prevalence of hearing loss. https://iris.who.int/bitstream/handle/10665