Abstract
Technology that can improve the ability to provide quick symptom control while decreasing the cost and burden of care could help hospice agencies deal with current hospice industry challenges. This paper describes how the use of a new rectal medication delivery technology at a large hospice in western New York has improved patient care and nursing efficiency while at the same time decreasing the cost of care.
Introduction
The ability to provide excellent end-of-life care in a cost-effective manner is the goal of every hospice agency. Unfortunately, the business of hospice is becoming more challenging each year. Hospices are questioning their long-term survival with the continued decreases in reimbursement and increased costs of care. The phaseout of the budget neutrality factor, sequestration, and the productivity adjustments by Medicare continue to decrease hospice reimbursement and are slated to continue through 2022 (Citation1).
In addition to decreased revenue, operational costs continue to rise. According to the most recent March 2018 MedPAC (Medicare Payment Advisory Commission) report, (Citation2) the 2015 average hospice cost of care was $150 per day, an increase of 0.5% from 2014. MedPAC reports an increased profit margin between 2014 and 2015 from 8.2% to 10% for all combined hospices but predicts the 2018 margins to be about 8.7%. MedPAC reports that the median length of hospice stay was 18 days for 2016, with more than 25% of patients enrolling within the last week of life, while acknowledging an increase in patient care needs and visit intensity during those last days of life. Lastly, the increased requirements for quality metrics and the rapidly changing regulatory landscape have put a large burden on hospices, which have had to add quality oversight staff to keep up with regulatory burdens.
Symptom management can be costly to agencies in clinician time and medication and other pharmacy-related costs. Although patients with difficult symptom management represent a minority of hospice cases in our experience, they can be very costly, raising the overall direct cost of care. Oral and sublingual routes of medication delivery facilitate effective symptom control in most hospice patients, but there is still a significant subset of patients for whom these routes either are not functional or fail to control symptoms. “Chasing” symptoms with sublingual medication by raising the dosage can lead to aspiration, stressed caregivers, patient suffering, and nonpeaceful deaths that lead to poor-quality outcomes and increase the cost of care. The sublingual route of delivery is in most cases not an effective route for patients with severe agitation, pain, seizures, nausea and vomiting, and other severe symptoms. These patients usually need an alternative route, which traditionally has been limited to intravenous (IV), subcutaneous (SQ), or rectal suppository. All these options mandate ordering, preparing, and delivering new forms of medication with additional cost and lag time to therapy implementation. Faced with these challenges, in 2015, Hospice Buffalo began using a specialized rectal administration catheter that solved these problems by enabling the use of oral medications that were already on hand at the bedside.
This rectal administration catheter (Macy catheter; Hospi Corporation, Eureka, CA) is Food and Drug Administration (FDA)-cleared to provide rectal access to deliver medications and fluids. The catheter comes in a kit that has a pill pulverizing system included. Use of the catheter and pulverizing system enables medications to be easily pulverized, suspended in a small amount of water, and given rectally. The catheter consists of a 14-Fr tube with a soft balloon on one end and a valved medication port and balloon inflation port on the other. It facilitates ongoing administration of medication or fluids for up to 28 days and can be reinserted during this time period if expelled with (or removed for) a bowel movement. The end of the catheter rests on the leg, allowing access to deliver medication or fluid without having to expose or move the patient. Medications in solid form are ground with the pill pulverizer, a small amount of water is added, and the resulting microenema suspension is injected into the distal one third of the rectum.
Hospice Buffalo provides hospice care in both private homes and long-term care facilities and provides inpatient care in a 22-bed hospice inpatient unit (HIU) in Erie County, New York. In 2016, the agency cared for approximately 4134 hospice beneficiaries, including 1609 home care patients, 1062 long-term care/assisted-living patients, 815 hospital patients, and 648 HIU patients.
Hospice Buffalo decided to implement use of the catheter as an additional symptom management tool with the goal of improving patient care and having an additional option to administer medications when the patient could not swallow, while hoping to simultaneously decrease the burden and cost of care. Use of the catheter was first piloted in the last quarter of 2015 in the 22-bed HIU, followed by a rollout to the home care teams in the first quarter of 2016. Pharmacy costs continued to rise through 2016, particularly parenteral medication costs in the HIU, despite the introduction of the catheter as a possible option for symptom management.
Methods
In February 2017, Hospice Buffalo initiated a set of guidelines to curb pharmacy expenses by further encouraging and directing the use of the rectal catheter in both home care and the HIU. The guidelines included instructing clinicians to try the rectal administration catheter as the first-line alternative when a patient was unable to swallow and sublingual was ineffective. The agency continued to ask patient families to bring the patient’s oral medications to the HIU to reduce waste and costs, as had been done all along.
A more detailed post hoc analysis of cost and clinical outcomes was conducted following the guideline implementation when pharmacy invoices were noted to be significantly lower. Actual cost savings and modeled cost savings were calculated from the monthly pharmacy billing invoices and census data. The clinicians (physicians, nurse practitioners, and registered nurses) were informally surveyed regarding the catheter’s effectiveness, benefits, and challenges.
Results
In 2016, Hospice Buffalo utilized 160 catheters in the HIU (approximately 25% of patients) and 139 catheters in home care (approximately 9% of patients). This did not include the routine home hospice patients in skilled nursing facilities, as the agency had not yet trained facilities in use of the catheter. The direct supply cost of the catheter in 2016 was $0.15 per patient day ($25,415 in total cost for the catheters divided by 168,054 total days of care).
HIU costs
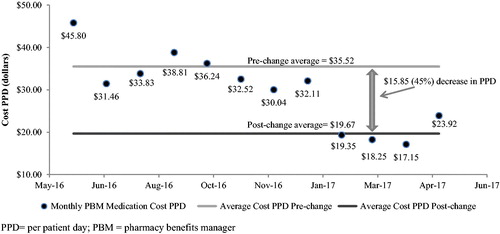
The first month the guidelines were in effect, medication costs in the HIU dropped $12.76 per patient day (PPD), or 40% from $32.11 PPD to $19.35 PPD. The average pharmacy benefit manager (PBM) costs from June 2016 through January 2017 before the change were $35.52 PPD, dropping to $19.67 PPD from February to May after the change, representing a 45% decrease in medication costs.1 The annualized medication cost in the HIU prior to the change was $254,439, dropping to $142,587 after the policy change for an annualized gross savings of $111,852 in the HIU. We calculated net annualized savings by subtracting the 2017 projected annualized catheter cost in the HIU from the annualized gross savings. After the new guidelines went into effect in the HIU, there was a 43% increase in catheter utilization in the HIU. Based on the new utilization rate, the HIU is projected to use 230 catheters in 2017 at a cost of $19,550. Subtracting this from the gross savings projects a net savings in the HIU of $92,302 for 2017. shows the monthly medication cost in PPD and the average cost before and after guideline changes throughout the time period in the HIU.
The medications that had the biggest cost reduction impact were the decreased use of parenteral methadone and parenteral haloperidol. Both medications are utilized extensively by Hospice Buffalo in the oral form and frequently changed to parenteral when the patient is no longer able to swallow well. Clinicians on the unit report that effective symptom relief has been maintained for most patients when the medications are changed to the rectal route. No clinician reported the catheter as inferior to the usual parenteral therapy for the majority of patients. The few exceptions are discussed subsequent in the discussion.
Infusion costs
Infusions are billed through an infusion pharmacy at a per diem rate that is separate from PBM costs incurred when using bolus injected medication. Medication infusions and hydration incur a per diem infusion fee that costs an average of $40 per day plus the cost of the medication and an additional infusion nurse visit charge if needed.
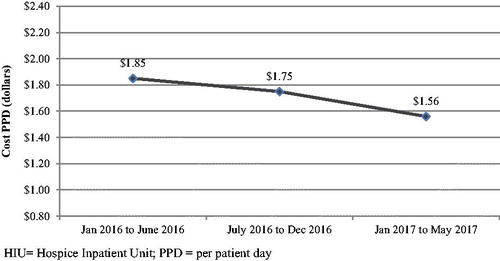
There is large monthly infusion cost fluctuations related to intermittent utilization of expensive infusions such as total parenteral nutrition, antibiotics, or other medications. When analyzing these expenditures in 6-month increments, there is a steady decrease in these costs over the three consecutive 6-month periods since the rectal catheter was introduced. shows the decreased trend in infusion expenditures in the HIU. From January to June 2016, costs averaged $1.85 PPD, dropping 6% to $1.74 from July to December. After initiating the new guidelines, infusion costs dropped another 10% to $1.56 PPD from January 2017 to May 2017. It is concluded that the 16% decrease in cost is partially related to the rectal catheter replacing infusions because no other variables have changed in the infusion practices in the HIU. This calculates as a projected $1,703 in annualized savings in 2017 over the 2016 average infusion cost in the HIU. These savings are not included in the reported net savings, as the fluctuations in cost from month to month were high and other variables may be affecting the data.
HIU nursing time
The HIU manager and clinical staff report that the catheter has improved nursing efficiency compared with the use of SQ ports. They report that SQ ports take more nursing time to place and maintain. This time increase is related to SQ port placement, labeling, site assessment, and documentation of, at times, numerous ports per patient. They report that the rectal administration catheter placement takes about 5 minutes and there is no associated maintenance or complications unless the catheter is expelled by the patient. Reinsertion of the catheter takes an additional 5 minutes. They also report a smaller amount of time spent counting and disposing of controlled substances, which requires two charge nurses each shift. Per the nursing staff, medications in tablet form are easier to count than parenteral medications, which are more tedious to measure and dispose. Additionally, fewer formulations of the same medication are present requiring counting (i.e., oral lorazepam and parenteral lorazepam) when only the oral formulation is needed. If an enema is needed prior to insertion due to excessive stool in the rectum, nurses report a small increase in time spent prior to the catheter being inserted that consists of enema administration and staff (typically home health aide) time providing personal cleansing if the patient is unable to do so themselves. Actual dollar savings related to HIU nursing efficiency (shift time overages related to counting, etc.) was not calculated for this study because it was not readily available and not felt necessary given the large cost savings attributable to medication use.
Home care costs
A quantified aggregate savings with direct correlation to catheter use was unable to be quantified with the available accounting data due to a large number of confounding variables. The agency was able to perform qualitative cost and efficiency modeling between the catheter and the other alternatives used. Potential savings identified using the rectal catheter in the home care setting are in the categories of medication delivery charges when new formulation are required, parenteral and suppository medication costs and associated fees, infusion supply costs, and decreased nursing time.
Parenteral versus oral medication via the catheter model
The ability to use medication in oral form already in the home is likely the biggest cost savings associated with the catheter in the home setting (as it is in the HIU). Most parenteral medications given in home care patients at Hospice Buffalo are given via bolus injection through SQ ports as in the HIU. It has been demonstrated in the HIU analysis that decreasing these parenteral medication costs and utilizing oral medications is cost-effective. This model also applies to home care but with the addition of the cost of the medication and supply delivery.
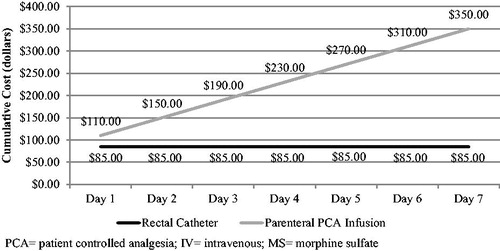
Another less utilized parenteral option at home is infusion via a PCA (patient-controlled analgesia) pump. Infusion costs include a $40/day per diem charge in addition to the cost for the medication, a delivery charge, and an additional infusion nurse visit cost if needed. models the comparative cost for a morphine infusion, a relatively inexpensive parenteral drug, over a 7-day period compared with the cost of oral morphine given via the rectal catheter. The model assumes a $40/day charge for the pump, a one-time $50 delivery charge, and a $20 charge for two morphine PCA cassettes that need to be changed every 4 days. The model does not include any cost for the parenteral venous access, any supplies needed for parenteral delivery, or infusion nurse visits for troubleshooting. The graph shows the parenteral infusion to be more expensive than the catheter on the first day, with the rectal catheter option becoming even more cost-effective every day thereafter.
Suppositories versus rectal catheter cost model
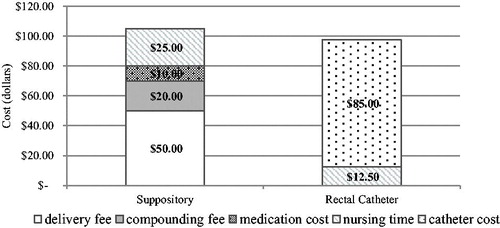
Analysis found medication administered via catheter to be potentially less expensive and clinically preferred than the use of compounded suppositories. For suppository preparation, there is a compounding fee of $20 plus the cost of the medication plus a delivery charge. Contracted regular business hours courier delivery charges run from $30 to $75 depending on distance. After-hours deliveries are contracted between $40 and $100 and weekend/holiday rates are double the base rate. To calculate a modest estimate of the cost of a single medication suppository intervention in the home, it was assumed an average delivery fee on a regular day to cost $50 plus a $20 compounding charge plus a $10 medication cost for a relatively inexpensive medication to total about $80. After-hours delivery or more expensive medications incur a higher charge. There is an associated increase in nursing time to follow up on the status of the patient, since there is a lag time for medication delivery and an associated delay in the intervention and symptom control. If the caregiver needs instruction or is uncomfortable inserting a suppository, another nursing visit would be necessary. For modeling purposes, it is assumed a nurse’s salary is $50 per hour, an additional 30 minutes of nursing time calling the prescriber, the pharmacy, checking on the patient status, and assuring the patient is comfortable after administration would cost an additional $25 minimum. Mileage reimbursement and nurse salary would be additional costs for any additional nurse visits related to the symptom. details the expense breakdown of a suppository versus the rectal catheter. Although there is not a striking direct cost differential in this single suppository medication model, the associated clinical challenges with suppositories (discussed later), the likely need for several different medications in suppository form, the reusability of the catheter after expulsion, delivery charges, and decreased nursing time and follow-up make up the additional cost savings.
Discussion
The staff report that the largest clinical benefit of using the rectal catheter is the ability to quickly administer oral formulary medications that are already on hand in both the HIU and in home care. Importantly, they also report that administering the medications rectally is efficacious. In home care, the nurses are able to gain faster symptom control by avoiding the lag time of having to order and deliver alternate forms of medication. Alternative forms, such as compounded suppositories, have several disadvantages: family/caregiver reluctant to use suppositories; repositioning of the patient and exposing private areas with each dose; discomfort with each insertion; and questionable or variable absorption in dehydrated patients. Each of the home care nurses carries a catheter kit in his/her car, allowing immediate catheter placement when symptoms demand. Once the nurse is in the home, a quick phone call to the prescriber is all that is required to give the oral medications already present via the rectal route.
The staff report that utilization of the rectal administration catheter helps some patients fulfill their desire to remain at home through the end of life. The ease of use by the caregivers allows them to maintain good symptom management in the home and prevent caregiver breakdown. Notable symptoms that create rapid caregiver breakdown or emergent transfer to a higher level of care include extreme pain, agitated delirium, nausea/vomiting, and seizures. Sublingual medications frequently do not work well in these instances, and preemptively switching to the catheter prevents symptom escalation.
In the HIU, the catheter provides a more home-like atmosphere compared with parenteral medication delivery, as it is not visible and requires no pumps, needles, or IV lines. Unlike needles, which can be uncomfortable, the rectal catheter is reported both anecdotally and in the literature to be comfortable for the patient and does not run the risks associated with parenteral access such as infection or infiltration (Citation3). It provides a good discharge option from the HIU to home, as it is easy and safe for non–medically trained caregivers to use compared with parenteral medications.
The HIU staff identified medication pass efficiency gains because the oral medications are all placed into the same grinder, suspended with water, and administered together as a single bolus. Parenteral medications have to be drawn up individually with sterile technique and administered individually, often via slow push (medications are not mixed in this HIU). Rectal administration is also noted to be faster in those patients who have some dysphagia and require oral medications crushed, placed in soft foods, and administered slowly by the spoonful. lists the benefits identified through the study analysis.
Table 1. Clinical benefits of the rectal catheter.
Use of the catheter presents some challenges and limitations. highlights the contraindications to the use of the rectal catheter and the identified clinical challenges. The catheter cannot be used on patients who have tumors and lesions in the rectum, active rectal bleeding, bowel surgery within the last 6 weeks, or diarrhea. Anecdotal evidence from our agency suggests that a large amount of soft stool in the rectum or frequent stooling may inhibit the full absorption of microenema medication. Clinicians have noted medication failure when a large amount of soft stool was noted in the rectum and stooling occurred after dosing. For that reason, patients in the HIU will receive an enema prior to catheter insertion when a large amount of soft stool is noted in the rectal vault. This extra step is somewhat time-consuming and can delay medication therapy.
Table 2. Contraindications and challenges to rectal catheter use.
Another challenge in adopting a new medication administration technology is education and comfort in practice around the pharmacokinetics of rectal drugs. The rectal pharmacokinetics and oral-to-rectal dose conversions for some medications are not known or not quickly available in handheld drug references, and clinicians are more familiar with parenteral dosing. Most of the drugs given for end-of-life symptom management have at least one pharmacokinetic study in the literature. The catheter manufacturer provides a list of medications for which rectal pharmacokinetic studies have been completed, with dose conversions for commonly used symptom management medications. However, rectal dosing literature often cites suppository preparations or commercially available solutions, which may contain ingredients that could enhance or even hinder absorption (Citation4). These studies therefore may not be applicable to oral medications pulverized and administered via microenema. In general, the literature tends to support improved absorption kinetics for microenema formulations versus suppository formulations for most end-of-life medications (Citation3–7). The absorption rate, and therefore time to effect, can differ significantly between microenema and suppository formulations primarily due to a lack of water in the rectum to dissolve the medication into an absorbable form. This is relevant at end of life when patients are dehydrated and many patients are on anticholinergic or opioid medications, which dry the mucus membranes. An example of the difference in microenema versus suppository pharmacokinetics is demonstrated in a study done by Lam et al. The results demonstrated both improved speed (Tmax) and overall absorption (Cmax) and decreased variability between healthy subjects for microenema administered phenobarbital versus suppository (Citation3).
There is little evidence base in the literature on the pharmacokinetics of subcutaneously administered palliative drugs such as opioids, benzodiazepines, and haloperidol when utilized at the end of life (Citation8). One population pharmacokinetic study done by Franken et al. looked at both oral and subcutaneously administered haloperidol in 28 patients. The authors identified the half-life of the drug to be about 30 hours but were unable to identify an effective plasma concentration, and they were unable to explain the large variability in plasma concentrations between subjects with the covariate model (Citation9). One possible reason for the reported variability in absorption could be that blood flow to the subcutaneous tissue can decrease significantly as a patient nears death, decreasing the ability of medication to enter the general circulation from the subcutaneous tissue. If this were the case, it could mean a dosage failure for the patient at a critical time. Thus, there is a great need for more study of the pharmacokinetics and efficacy of both subcutaneously and rectally administered medications, especially at the end of life.
Another challenge noted with adoption of the catheter is related to education of the patient, caregiver, and the clinician in the nonpharmacological issues related to rectal delivery via a new device. Patients, caregivers, and even clinicians sometimes have an initial hesitance to using the rectal route of delivery. The rectal route can be considered “invasive” or an invasion of privacy. Some clinicians and caregivers think that rectal medication is not “aggressive” symptom management, as they are accustomed to parenteral medication use during hospitalization and emergency care. Most of the time, these concerns are handled with education and explanation.
The initial clinician preference for parenteral medications in the HIU setting was the result of familiarity, justification for inpatient level status, and noted failure of oral medication management in the home care setting. As clinicians have become more comfortable with the use and efficacy of the catheter and recognize the catheter as a justifiable intervention in the inpatient setting, the catheter is frequently utilized before prescribing parenteral therapy. Some prescribers report that they are more likely to utilize parenteral medications if the prognosis is only a few days, when the patient is likely to improve and go back on oral medications, and for the rapid and predictable effects of short-acting opioids for managing a pain crisis. In some instances, the cost of utilizing the catheter in the HIU can be greater than the cost of parenteral medications if treatment is only for 1–2 days, and if inexpensive parenteral medications such as lorazepam, hydromorphone, or morphine are utilized, but nursing time and complication costs are not considered in this estimate. With the recent shortage in parenteral morphine, lorazepam, and hydromorphone in 2017, the catheter is increasingly being used out of necessity to manage patients without a functional oral route, and with good results.
Although training staff in how to use the catheter is easy, changing an established culture of using parenteral medication as a first-line alternative, or the dependence on sublingual medication beyond what is actually effective, is more challenging. Before nurses and physicians can properly train and convince caregivers to feel comfortable with the rectal route, it is necessary for the practitioner to be properly educated and comfortable with this mode of delivery also. At Hospice Buffalo, we found that the culture change took place through education, followed by early adopter clinicians using of the catheter and subsequently sharing the positive outcomes with the rest of the team.
The post hoc analysis of the effects on costs and the informality with which the clinicians were surveyed are acknowledged limitations of this study. Related direct and indirect costs associated with using the rectal catheter were unable to be quantified with the available accounting information but are necessary for a thorough analysis. We identified those cost areas that may also be significantly impacted, such as nursing wages and mileage reimbursement. A prospective pharmacoeconomic study is needed to detail cost-effectiveness of the catheter intervention in both the home setting and the HIU setting.
Conclusion
The rectal administration catheter has improved the ability of Hospice Buffalo to facilitate quick and effective symptom management while simultaneously decreasing costs and improving nursing efficiency. More savings and positive outcomes can potentially be achieved with increased utilization. Further research into the rectal pharmacokinetics of common palliative medications and disease maintenance medications is warranted, as well as more formal studies comparing clinical efficacy of rectally administered medications versus oral and subcutaneously administered medications.
Declaration of interest
The authors report no conflict of interest. The authors alone are responsible for the content and writing of the article.
Notes
1 Due to a change in pharmacy vendor and discontinuation of an automated dispensing unit, we did not do a 12-month analysis of 2016, as it would have made the results from the first half of 2016 incomparable to the second half of 2016 and post guideline implementation in 2017.
References
- Hospice Action Network. Current State of the Hospice Community. 2013. http://hospiceactionnetwork.org/linked_documents/get_informed/policy_resources/CurrentStateofHospice_Nov2013.pdf. Accessed May 11, 2017.
- Medicare Payment and Advisory Commission (MEDPAC) Hospice services: Report to the Congress: Medicare Payment Policy. March 2018. http://www.medpac.gov/docs/default-source/reports/mar18_medpac_ch12_sec.pdf?sfvrsn=0. Accessed June 5, 2018.
- Lam YW, Lam A, Macy B. Pharmacokinetics of Phenobarbital in Microenema Via Macy Catheter Versus Suppository. J Pain Symptom Manage. 2016;51(6):994–1001.
- Davis MP, Walsh D, LeGrand SB, Naughton M. Symptom control in cancer patients: the clinical pharmacology and therapeutic role of suppositories and rectal suspensions. Support Care Cancer. 2002;10(2):117–138. doi:10.1007/s00520-001-0311-6.
- de Boer AG, Moolenaar F, de Leede LG, Breimer DD. Rectal drug administration: clinical pharmacokinetic considerations. Clin Pharmacokinet. 1982;7(4):285–311. doi:10.2165/00003088-198207040-00002.
- van Hoogdalem E, de Boer AG, Breimer DD. Pharmacokinetics of rectal drug administration, Part I. General considerations and clinical applications of centrally acting drugs. Clin Pharmacokinet. 1991;21(1):11–26. doi:10.2165/00003088-199121010-00002.
- Warren DE. Practical use of rectal medications in palliative care. J Pain Symptom Manage. 1996;11(6):378–387.
- Franken LG, de Winter BC, van Esch HJ, et al. Pharmacokinetic considerations and recommendations in palliative care, with focus on morphine, midazolam and haloperidol. Expert Opin Drug Metab Toxicol. 2016;12(6):669–680. doi:10.1080/17425255.2016.1179281.
- Franken LG, Mathot RAA, Masman AD, et al. Population pharmacokinetics of haloperidol in terminally ill adult patients. Eur J Clin Pharmacol. 2017;73(10):1271–1277.