 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
Objective
Two lines of research, on outcome moderators and on novel treatment targets, seek to improve the overall efficacy of child anxiety treatment, with mixed results. We propose that an integration of both lines of research can lead to improved treatment efficacy. In a first proof of concept of this approach, we studied whether the interaction between baseline levels and targeted changes in peripheral oxytocin (OT) can predict differential responses to two childhood anxiety treatments.
Method
A total of 124 mother-child dyads participated in the study. Children’s salivary OT levels were measured at baseline and again, immediately after an experimental dyadic interaction in the lab. Dyads were subsequently randomized to receive one of two treatments, differing in their targets: SPACE (Supportive Parenting for Anxious Childhood Emotions) and CBT (cognitive-behavioral therapy). Treatment outcomes were assessed using the Childhood Anxiety Related Emotional Disorders scale, reported by both mother and child.
Results
The findings suggest that in SPACE, where the mother is the main agent of change, higher baseline levels of child OT, coupled with increases in OT following a positive mother-child interaction, predicted greater treatment efficacy. By contrast, in CBT, where the child is the main agent of change, higher baseline levels of child OT, coupled with a decrease in OT following the interaction, predicted greater treatment efficacy.
Conclusions
The findings highlight the importance of the integration between moderators and targets of treatments for progress toward improving treatment efficacy through precision medicine.
Accumulating findings across meta-analyses show that treatments for childhood anxiety disorders are insufficiently effective in up to half of cases (Weisz et al., Citation2017). These findings are especially worrisome given the high prevalence of childhood anxiety disorders (Costello et al., Citation2005) and their adverse short and long-term consequences (Essau et al., Citation2000; Vigo et al., Citation2016). Over recent decades, much effort has been invested in identifying predictors indicating who may benefit from treatment, and moderators indicating the differential effects of treatments, with the aim of matching individuals with their most effective treatments (National Institute of Mental Health, Citation2015). Yet, few consistent findings emerged to date (Lebowitz et al., Citation2021).
It has been suggested that when identifying predictors and moderators of treatment efficacy, it is important to take into account both the baseline levels of a given construct and its responsivity to targeted manipulations (Zilcha-Mano, Citation2020). Interactions between baseline levels and targeted changes in a given construct may signal the importance of targeting that construct (Zilcha-Mano, Citation2017; Zilcha-Mano & Fisher, Citation2022). Findings support the importance of focusing on the interactions between baseline levels and targeted changes in a given construct for improving treatment efficacy. For example, the effect of state-like improvements in the client-therapist alliance on treatment outcome was dependent on the client’s trait-like ability to form a strong alliance (Zilcha-Mano, Citation2017; Zilcha-Mano & Fisher, Citation2022). Such interactions between baseline levels and treatment-related changes are of special interest when focusing on biological measures, which may directly tap into treatment mechanisms. For example, the effect of normalization of amygdala hyperactivation on treatment outcome was found to be moderated by the client’s baseline levels of amygdala hyperactivation. Normalization of the amygdala hyperactivation was associated with better treatment outcome only for clients with baseline hyperactivation of the amygdala (Zilcha-Mano et al., Citation2022).
In the context of psychosocial treatments for anxiety disorders in children, several biological measures have been suggested, including amygdala-based connectivity (White & Pine, Citation2017) and the neural reward circuitry (Sequeira et al., Citation2021). One biological system that has received attention is the oxytocinergic system. Oxytocin (OT), a nine-amino-acid cyclic neuropeptide produced in the paraventricular nucleus of the hypothalamus, is implicated in anxiety regulation and the modulation of close interpersonal and attachment behavior (Feldman, Citation2015). It has been argued that OT serves as a biological mechanism by which bonds are formed and strengthened across species (Algoe et al., Citation2017). OT is considered to play an important role in social interactions, intimate relationships, and the regulation of social behavior (e.g., Carter, Citation1998; Carter et al., Citation2008; Heinrichs & Domes, Citation2008), and to facilitate attachment security and parent-child bonding (Feldman, Gordon, & Zagoory-Sharon, Citation2010; Fries et al., Citation2005).
OT may facilitate bond formation and maintenance by increasing states of calmness and approaching behaviors, and reducing stress and negative mood (Gordon et al., Citation2008). OT has an anxiety-lowering effect, mediated by modulation of the amygdala, the hypothalamic (pituitary) adrenal axis, and the cardiovascular system. The anxiety-lowering effect of OT may trigger affiliative processes by being released when a safe situation involving another person is sensed, thereby motivating approach behaviors and reciprocity (Merolla et al., Citation2013), as well as empathy (Shamay-Tsoory, Citation2011; Shamay-Tsoory et al., Citation2013) and compassion (Palgi et al., Citation2016).
Findings suggest that anxiety disorders are linked to low levels of salivary OT in children (Lebowitz et al., Citation2016). Findings further suggest the importance of both baseline levels of OT and of changes in OT occurring during interpersonal interactions (Feldman, Gordon, & Zagoory-Sharon, Citation2010; Lebowitz et al., Citation2016, Citation2017), as indicators of the quality of interpersonal interactions and of subsequent treatment outcomes. Baseline OT, measured in both plasma and saliva, was found to be individually stable over a period of months and even years, representing a trait-like characteristic of the individual (Feldman et al., Citation2007, Citation2013; Priel et al., Citation2019; Schneiderman et al., Citation2012). Baseline OT has been considered a biomarker of social-affiliative functioning, such as affiliative tendency, empathy, social fitness, social engagement, and reciprocal relational style. State-like changes in OT have also been found to be important and serve as markers for affiliative experiences (Feldman, Gordon, Schneiderman, et al., Citation2010) and psychosocial stress (Elmadih et al., Citation2014; Seltzer et al., Citation2010). The release of OT is stimulated by interpersonal cues, such as the touch of a significant person, making its state-like changes a social biomarker (Insel, Citation2010). State-like changes in OT have been argued to be a potentially important mechanism of change in psychotherapy (Zilcha-Mano et al., Citation2020). Findings suggest that client-therapist synchrony mediates the effect of clients’ interpersonal abilities and treatment outcome (Zilcha-Mano et al., Citation2021). Furthermore, Jobst et al. (Citation2018) found that both trait-like levels of OT (higher oxytocin plasma levels at baseline) and state-like levels (faster recovery following a social exclusion manipulation) correlated with greater changes in self-reported depressive symptoms. No study to date has tested the interactive effect between baseline levels of OT and changes in these levels as a result of interpersonal interaction, as potential predictors or moderators of child anxiety treatment outcomes.
The current study investigated the ability of the interaction between baseline peripheral child-OT levels and targeted manipulation-related changes in the child-OT levels to serve as a predictor and a moderator of treatment outcome in childhood anxiety disorders. The targeted manipulation was an experimentally designed parent-child interaction. To minimize noise resulting from contextual effects of the interaction (Shamay-Tsoory & Abu-Akel, Citation2016), we instructed child-mother dyads to engage in a positive interaction in the lab (the Fun Day task) before the start of treatment. The Fun Day task was developed for evaluating parent-child reciprocity, maternal sensitivity, and child engagement (Feldman, Citation1998). It was found to be sensitive to both differences between parent-child dyads (Weisman et al., Citation2015) and changes within the dyad in reciprocity throughout development (Feldman, Citation2010). The Fun Day task has also been previously found to explore change in OT levels in anxious children (Lebowitz et al., Citation2016). We tested a potentially differential effect for two treatment conditions, one building on the mother as an agent of therapeutic change, targeting the parent-child interactions, the other in which the child is the change agent. Specifically, we hypothesized that in SPACE, where the mother is the main agent of change, higher baseline levels of child OT, coupled with increases in OT following a positive mother-child interaction, predict greater treatment efficacy. This hypothesis is based on the reasoning that an increase in the release of OT during a positive interaction with the parent may serve as a marker of the potential therapeutic effect of targeting the parent-child relationship through the therapeutic work with the parent. By contrast, in CBT, where the child is the main agent of change, we hypothesized that higher baseline levels, coupled with a decrease in OT following the interaction, predict greater treatment efficacy. This hypothesis is based on the reasoning that a decrease in OT during such an interaction that was designed to be positive may serve as a counter indication for the potential therapeutic merit of targeting the parent-child relationship, and the need for searching for alternative targets of treatments, such as those possible in individual treatment focused on the child. We used data from a recent randomized controlled trial comparing SPACE (Supportive Parenting for Anxious Childhood Emotions) and child-based cognitive-behavioral therapy (CBT).
Method
Participants
One hundred twenty-four mother-child dyads participated in the randomized controlled trial (RCT). The study was approved by the institutional review board. Children’s mean age was 9.6 (range 7–14, SD = 2.45), and 53% were female; they were predominantly white (83%). The primary anxiety diagnoses were generalized anxiety disorder (35.2%), social phobia (11.8%), separation anxiety disorder (18.2%), and specific phobia (11.8%). Details of the study including more complete sample characterization and description of procedures are provided elsewhere (Lebowitz et al., Citation2020).
Treatments
Study participants were randomly assigned to one of two manualized 12-session treatments: SPACE and CBT. In SPACE (N = 64), parents received parent-only sessions, targeting accommodation reduction (Lebowitz & Omer, Citation2013; Lebowitz et al., Citation2014) with no direct child-therapist contact. In CBT (N = 60), children received exposure-based CBT (Silverman et al., Citation2009), with no direct parent-treatment sessions. Therapists were crossed across treatment arms to reduce therapist variance. Primary and secondary outcomes of the trial have been previously reported (Lebowitz et al., Citation2019). Briefly, SPACE was found to be non-inferior to CBT across all outcome measures assessed, attrition did not differ significantly between groups, and treatment credibility was high for both treatments.
Measures
Childhood Anxiety Symptom Severity
Parallel parent and child versions of the Screen for Childhood Anxiety Related Emotional Disorders (SCARED-P and SCARED-C, respectively) 41-item rating scale of childhood anxiety symptoms were administered. Internal consistency was good (α = .89 and α = .91for the parent and the child versions, respectively). We chose the SCARED because it is a widely used instrument that evaluates the perspectives of both parent and child, and both versions received good to excellent scores on all psychometric criteria in recent evidence-based reviews of youth anxiety measures (Etkin et al., Citation2021a, Citation2021b).
Procedure
After describing the study to the parents and children, parents’ written informed consent and children’s written assent were obtained. Separately, children and mothers completed the SCARED at baseline, mid-treatment (following the sixth session) and post-treatment (following the 12th session). Although there is a debate regarding the reproducibility of OT assays and the association between plasma, salivary, urinary, and cerebrospinal fluid, OT levels, and the different forms of sample preparation (MacLean et al., Citation2019), there is some evidence suggesting that OT levels in plasma and saliva are interrelated (Feldman et al., Citation2011), therefore we used salivary OT measurements because they are minimally intrusive. At baseline, children provided a salivary sample for analysis, then children and mothers participated in a brief, seven-minute dyadic interaction during which they planned a “fun day” together (for details, see (Lebowitz et al., Citation2016). A second saliva sample was collected from the children after the dyadic interaction. Saliva samples were collected using salivettes (Sarstedt, Rommelsdorf, Germany), between 4 pm and 5 pm, after a 2-hr fast. The salivettes were stored at −20°C until they were centrifuged at 1,000 × g for 2 min for saliva release. Liquid samples were kept at−80°C, until lyophilized, and stored at−20°C (usually only for 2 hours) before they were tested. The lyophilizer worked at −89°C under vacuum (0.027 mbar). OT levels were analyzed using a commercially available enzyme linked immunosorbent assay (ELISA) kit from Enzo (NY, USA). Measurements were performed in duplicate. Further details about the design and procedures used are described elsewhere (Lebowitz et al., Citation2019). The data do not overlap with previous publications on OT during the Fun Day task (Lebowitz et al., Citation2016; Polack et al., Citation2021).
Overview of Statistical Analyses
To test moderation, we assessed the interactive effects of pre-randomization OT levels, both pre- and post-Fun Day task (Kraemer et al., Citation2002). To test the ability of the interaction between baseline child-OT and changes in child-OT to predict differential response to treatment (SPACE vs. CBT), as well as treatment outcome in general, we used linear regression analyses. Following De Los Reyes (Citation2017), we operationalized treatment outcome as the level of symptoms post-treatment, controlling for individual differences in the level of symptoms pre-treatment. To operationalize change in OT levels, we used residual scores of post-interaction predicted by baseline levels. We included the 3-way interaction between baseline OT, residual scores of OT, and treatment condition, and each of the lower-level interactions and main effects to predict treatment outcome. If a 3-way interaction was not significant, thus not supporting a differential effect for treatment, we tested the ability of the interaction between baseline OT and OT residual scores to predict outcome across treatments. Analyses were repeated twice, for each outcome variable (SCARED-P, SCARED-C). We used the MissForest package in R to impute missing observations in the independent variables. Specifically, 109 participants had OT baseline and 107 participants had OT post-interaction scores. Additionally, 104 participants had the SCARED-P outcome and 104 had the SCARED-C outcome. We used MissForest to impute OT observations only for individuals for whom OT observations but not outcome observations were missing. This procedure resulted in imputing 11 baseline OT observations and 12 post-interaction OT observations. For the outcome data, for individuals with mid-treatment but not post-treatment outcome, the mid-observation was carried forward and used in the analyses. Individuals with missing mid-treatment and post-treatment observations were removed from the analyses.
We used the following equations for the SCARED-P and the SCARED-C:
where SCRDp/c.post = post-treatment SCARED for parent report and child report (separate models); SCRDp/c.pre = pre-treatment SCARED for parent report and child report (separate models); OTc.post.residuals = OT at post-interaction, residualing out baseline scores; Condition = SPACE vs. CBT.
Results
Preliminary Analyses
Descriptive statistics for OT levels and outcome variables (SCARED-P, SCARED-C) at baseline and post-intervention appear in Table S1 in the online supplement. The correlations between age and OT at baseline and post-interaction were r = .08, p = .36 and r = .11, p = .23, respectively.
A significant 3-way interaction was found between baseline and changes in OT levels and treatment condition in predicting post-treatment SCARED-P (β = 0.02, S.E. = 0.01, t = 2.06, p = .042; see Table S2 in the online supplement). As shown in , in SPACE, we found a medium size trend level effect, according to which for individuals with higher levels of baseline OT, the association between an increase in OT and lower symptom levels was stronger. By contrast, in CBT, we found a medium size trend level effect, according to which for individuals with higher levels of baseline OT, association between a decrease in OT and lower symptom levels was stronger.
Figure 1. (a) The moderating effect of changes in child OT on the association between baseline child OT and post-treatment SCARED-P, separately for SPACE and CBT; (b) the predicting effect of changes in OT on the association between baseline OT and post-treatment SCARED-C. The figures demonstrate the associations when baseline OT is high and when it is low, based on the 3-way interaction model. The shading represents the confidence intervals (95%).
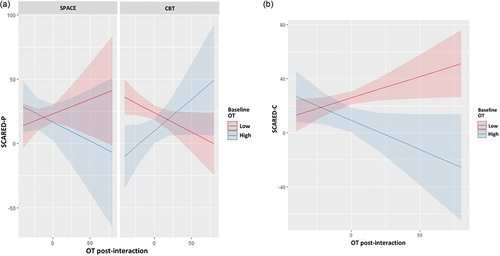
The 3-way interaction for SCRD-C was not significant (p = .35), but we found a significant 2-way interaction between baseline OT and changes in OT in predicting post-treatment child-SCRD (β=-0.011, S.E. = 0.005, t = −2.205, p = .02; ; see Table S3 in the online supplement). Findings suggest that for individuals with higher levels for baseline OT, the association between an increase in OT and lower symptom levels was stronger.
Sensitivity Analyses
Because previous studies used change scores, to remain consistent with previous studies, we used change scores instead of residual scores for OT to test whether findings replicated those reported above. Findings remained similar to those reported above. The 3-way interaction for parent-SCARD remained significant (β = 0.018, S.E. = 0.007, t = 2.521, p = .013), yielding the same pattern of differential effects for SPACE and CBT reported above. Likewise, the 2-way interaction for child-SCRD was significant (β=-0.009, S.E. = 0.004, t = −2.358, p = .02).
Discussion
Findings provide support for the ability of the interaction between baseline child peripheral OT levels and manipulation-related changes in child OT levels to predict and moderate childhood anxiety treatment outcomes from the child’s and the parent’s perspectives, respectively. First, findings based on parent-reported treatment outcomes may suggest that the interaction between baseline OT and changes in OT (operationalized as residual scores) can predict differential efficacy of SPACE vs. CBT. In SPACE, where the mother is the main agent of therapeutic change, higher baseline levels of OT, coupled with increases in OT following a positive mother-child interaction, showed a moderate effect size in predicting greater treatment efficacy. By contrast, in CBT, where the child is the main agent of therapeutic change, higher baseline levels of child OT, coupled with decrease in OT as a result of the interaction with the mother, showed a moderate effect size in predicting greater treatment efficacy. Second, findings based on child-reported treatment outcomes suggest that the interaction between baseline OT and changes in OT can predict treatment outcome, such that higher baseline levels of OT, coupled with increases in OT following the positive interaction with the mother, predicted greater treatment efficacy. Findings should be replicated in larger samples, before clinical implications can be confidently inferred.
It is intriguing to speculate on potential explanations of the pattern of findings obtained. The increase in OT when interacting with the mother may signal the ability of the mother to serve as an agent of positive change, either enhancing the release of OT, or the release of OT amplifying the positive interaction with the mother. In such cases, SPACE, where the parent is the main agent of change, may be recommended. By contrast, the reduction in child OT following such mother-child interaction may indicate that the parent may not be the optimal agent of therapeutic change (due perhaps to parental entanglement or a less positive mother-child relationship). In such cases, a child-based treatment such as CBT, in which the child is the agent of change and the parent is less involved, may be more efficacious. This explanation is supported by findings showing that maternal ratings of family accommodation are negatively associated with salivary OT levels in youths (Lebowitz et al., Citation2016). The findings should be interpreted with caution given that they were found for the parent but not the child perspective on outcome. These distinct patterns for different perspectives on outcome are consistent with the accumulating literature suggesting that parent and child rating of psychopathology and mental health represent complementary rather than identical aspects of the child’s functioning and wellbeing (De Los Reyes & Kazdin, Citation2005; Hawley & Weisz, Citation2003). If replicated in future research, the findings may offer new insights on a biomarker that has the potential to shed light on the question of when targeting the parent-child relationship may be more effective than working directly with the child. It is reasonable to assume that an accountable personalized assignment of individuals to their optimal treatment may depend on a collection of interacting markers that have increased predictive validity when combined (Lebowitz et al., Citation2021). While maladaptive interpersonal patterns characterizing the parent-child relationship, especially accommodating behavior, may indicate the promising potential of targeting the parent-child relationship, a positive initial effect of targeting the relationship may indicate the positive potential of the parent to serve as the agent of therapeutic change.
It is intriguing to speculate on the possible factors contributing to the distinct pattern of findings obtained for parent- and child-reported outcomes. Interpreting this difference requires caution, but one post hoc explanation may be that parent ratings are more impacted by the parent’s direct participation in treatment (as in SPACE) leading to results that are different for SPACE and for CBT. Child ratings may be less impacted by treatment modality as the child is going through treatment in both conditions (whether in person, as in CBT, or through the changes parents make to their behavior, as in CBT).
Accumulating evidence suggests that given the biological complexity of OT, varying approaches to sample preparation and measurement of OT may yield different and in some cases even conflicting findings owing to differential sensitivity to diverse conformational states of the OT molecule (Lefevre et al., Citation2017; Leng & Sabatier, Citation2016; MacLean et al., Citation2019). Although there are documented advantages of saliva over blood OT, the current findings should be evaluated taking into account the general debate regarding OT measurement (MacLean et al., Citation2019). Another notable limitation of the study is that the children’s baseline OT levels were quantified based on a single sample. Although previous studies of peripheral oxytocin have similarly relied on a single assessment, baseline measures of OT are more robust when they are repeated several times at the same visit, and then the area under the curve (AUC; Pruessner et al., Citation2003) can be used to estimate the baseline level. Future studies should also measure changes in OT across a variety of experimental manipulations, varying in the instructions provided to the child-mother dyads, and monitoring their behaviors during the interactions. Moreover, although a correct temporal relationship has been established between the two OT measurements collected pre-treatment and subsequent treatment outcome, causality cannot be assumed, and intranasal OT vs. placebo could be administered to enable causal inferences (Josef et al., Citation2019). Additionally, this study focused on mother-child interactions and fathers were not directly involved in the study procedures, but could attend parent-based treatment sessions. Future studies should explore whether findings can be generalized to child-father dyads as well, and use child-stranger and child-peer dyads for comparison. Future studies should also seek to replicate the different patterns of results for mother- and child-reported outcomes. Finally, the sample in this RCT was medium in size and predominantly white, limiting its generalizability.
Notwithstanding the study’s limitations and the need for future research, the present study provides initial positive support for OT as a potential agent indicating change in treatments for childhood anxiety. The findings suggest that coupling of higher baseline OT with experimentally induced increase in OT as a result of positive interaction with the mother predicts greater treatment efficacy, especially for SPACE, where the parent is the main agent of therapeutic change.
Supplemental Material
Download MS Word (22.2 KB)Disclosure Statement
No potential conflict of interest was reported by the author(s).
Supplementary Data
Supplemental material for this article can be accessed online at https://doi.org/10.1080/15374416.2023.2188557
Additional information
Funding
References
- Algoe, S. B., Kurtz, L. E., & Grewen, K. (2017). Oxytocin and social bonds: The role of oxytocin in perceptions of romantic partners’ bonding behavior. Psychological Science, 28(12), 1763–1772. https://doi.org/10.1177/0956797617716922
- Carter, C. S. (1998). Neuroendocrine perspectives on social attachment and love. Psychoneuroendocrinology, 23(8), 779–818. https://doi.org/10.1016/S0306-4530(98)00055-9
- Carter, C. S., Grippo, A. J., Pournajafi-Nazarloo, H., Ruscio, M. G., & Porges, S. W. (2008). Oxytocin, vasopressin and sociality. Progress in Brain Research, 170, 331–336.
- Costello, E. J., Egger, H. L., & Angold, A. (2005). The developmental epidemiology of anxiety disorders: Phenomenology, prevalence, and comorbidity. Child and Adolescent Psychiatric Clinics of North America, 14(4), 631–648. https://doi.org/10.1016/j.chc.2005.06.003
- De Los Reyes, A. (2017). Inaugural editorial: Making the journal of clinical child & adolescent psychology your “home journal”. Journal of Clinical Child & Adolescent Psychology, 46(1), 1–10. https://doi.org/10.1080/15374416.2016.1266649
- De Los Reyes, A., & Kazdin, A. E. (2005). Informant discrepancies in the assessment of childhood psychopathology: A critical review, theoretical framework, and recommendations for further study. Psychological Bulletin, 131(4), 483–509. https://doi.org/10.1037/0033-2909.131.4.483
- Elmadih, A., Wan, M. W., Numan, M., Elliott, R., Downey, D., & Abel, K. M. (2014). Does oxytocin modulate variation in maternal caregiving in healthy new mothers? Brain Research, 1580, 143–150. https://doi.org/10.1016/j.brainres.2014.01.020
- Essau, C. A., Conradt, J., & Petermann, F. (2000). Frequency, comorbidity, and psychosocial impairment of anxiety disorders in German adolescents. Journal of Anxiety Disorders, 14(3), 263–279. https://doi.org/10.1016/S0887-6185(99)00039-0
- Etkin, R. G., Lebowitz, E. R., & Silverman, W. K. (2021b). Using evaluative criteria to review youth anxiety measures, part II: Parent-report. Journal of Clinical Child & Adolescent Psychology, 50(2), 155–176. https://doi.org/10.1080/15374416.2021.1878898
- Etkin, R. G., Shimshoni, Y., Lebowitz, E. R., & Silverman, W. K. (2021a). Using evaluative criteria to review youth anxiety measures, part I: Self-report. Journal of Clinical Child & Adolescent Psychology, 50(1), 58–76. https://doi.org/10.1080/15374416.2020.1802736
- Feldman, R. (1998). Coding interactive behavior manual [ Unpublished manual]. Bar-Ilan University.
- Feldman, R. (2010). The relational basis of adolescent adjustment: Trajectories of mother–child interactive behaviors from infancy to adolescence shape adolescents’ adaptation. Attachment & Human Development, 12(1–2), 173–192. https://doi.org/10.1080/14616730903282472
- Feldman, R. (2015). The adaptive human parental brain: Implications for children’s social development. Trends in Neurosciences, 38(6), 387–399. https://doi.org/10.1016/j.tins.2015.04.004
- Feldman, R., Gordon, I., Influs, M., Gutbir, T., & Ebstein, R. P. (2013). Parental oxytocin and early caregiving jointly shape children’s oxytocin response and social reciprocity. Neuropsychopharmacology, 38(7), 1154–1162. https://doi.org/10.1038/npp.2013.22
- Feldman, R., Gordon, I., Schneiderman, I., Weisman, O., & Zagoory-Sharon, O. (2010). Natural variations in maternal and paternal care are associated with systematic changes in oxytocin following parent–infant contact. Psychoneuroendocrinology, 35(8), 1133–1141. https://doi.org/10.1016/j.psyneuen.2010.01.013
- Feldman, R., Gordon, I., & Zagoory‐Sharon, O. (2011). Maternal and paternal plasma, salivary, and urinary oxytocin and parent–infant synchrony: Considering stress and affiliation components of human bonding. Developmental Science, 14(4), 752–761. https://doi.org/10.1111/j.1467-7687.2010.01021.x
- Feldman, R., Gordon, I., & Zagoory-Sharon, O. (2010). The cross-generation transmission of oxytocin in humans. Hormones and Behavior, 58(4), 669–676. https://doi.org/10.1016/j.yhbeh.2010.06.005
- Feldman, R., Weller, A., Zagoory-Sharon, O., & Levine, A. (2007). Evidence for a neuroendocrinological foundation of human affiliation: Plasma oxytocin levels across pregnancy and the postpartum period predict mother-infant bonding. Psychological Science, 18(11), 965–970. https://doi.org/10.1111/j.1467-9280.2007.02010.x
- Fries, A. B. W., Ziegler, T. E., Kurian, J. R., Jacoris, S., & Pollak, S. D. (2005). Early experience in humans is associated with changes in neuropeptides critical for regulating social behavior. Proceedings of the National Academy of Sciences, 102(47), 17237–17240. https://doi.org/10.1073/pnas.0504767102
- Gadassi Polack, R., Joormann, J., Orbach, M., Silverman, W. K., & Lebowitz, E. R. (2021). Maternal Depression and Mother-Child Oxytocin Synchrony in Youth with Anxiety Disorders. Research on Child and Adolescent Psychopathology, 49, 381–392.
- Gordon, I., Zagoory‐Sharon, O., Schneiderman, I., Leckman, J. F., Weller, A., & Feldman, R. (2008). Oxytocin and cortisol in romantically unattached young adults: Associations with bonding and psychological distress. Psychophysiology, 45(3), 349–352. https://doi.org/10.1111/j.1469-8986.2008.00649.x
- Hawley, K. M., & Weisz, J. R. (2003). Child, parent and therapist (dis) agreement on target problems in outpatient therapy: The therapist’s dilemma and its implications. Journal of Consulting and Clinical Psychology, 71(1), 62–70. https://doi.org/10.1037/0022-006X.71.1.62
- Heinrichs, M., & Domes, G. (2008). Neuropeptides and social behaviour: Effects of oxytocin and vasopressin in humans. Progress in Brain Research, 170, 337–350.
- Insel, T. R. (2010). The challenge of translation in social neuroscience: A review of oxytocin, vasopressin, and affiliative behavior. Neuron, 65(6), 768–779. https://doi.org/10.1016/j.neuron.2010.03.005
- Jobst, A., Sabass, L., Hall, D., Brücklmeier, B., Buchheim, A., Hall, J., Sarubin, N., Zill, P., Falkai, P., Brakemeier, E.-L., & Padberg, F. (2018). Oxytocin plasma levels predict the outcome of psychotherapy: A pilot study in chronic depression. Journal of Affective Disorders, 227, 206–213. https://doi.org/10.1016/j.jad.2017.10.037
- Josef, L., Goldstein, P., Mayseless, N., Ayalon, L., & Shamay-Tsoory, S. G. (2019). The oxytocinergic system mediates synchronized interpersonal movement during dance. Scientific Reports, 9(1), 1894. https://doi.org/10.1038/s41598-018-37141-1
- Kraemer, H. C., Wilson, G. T., Fairburn, C. G., & Agras, W. S. (2002). Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry, 59(10), 877–883. https://doi.org/10.1001/archpsyc.59.10.877
- Lebowitz, E. R., Leckman, J. F., Feldman, R., Zagoory-Sharon, O., McDonald, N., & Silverman, W. K. (2016). Salivary oxytocin in clinically anxious youth: Associations with separation anxiety and family accommodation. Psychoneuroendocrinology, 65, 35–43. https://doi.org/10.1016/j.psyneuen.2015.12.007
- Lebowitz, E. R., Marin, C., Martino, A., Shimshoni, Y., & Silverman, W. K. (2019). Parent-based treatment as efficacious as cognitive behavioral therapy for childhood anxiety: A randomized noninferiority study of supportive parenting for anxious childhood emotions. Journal of the American Academy of Child & Adolescent Psychiatry, 59(3), 362–372. https://doi.org/10.1016/j.jaac.2019.02.014
- Lebowitz, E. R., Marin, C., Martino, A., Shimshoni, Y., & Silverman, W. K. (2020). Parent-based treatment as efficacious as cognitive-behavioral therapy for childhood anxiety: A randomized noninferiority study of supportive parenting for anxious childhood emotions. Journal of the American Academy of Child & Adolescent Psychiatry, 59(3), 362–372.
- Lebowitz, E. R., & Omer, H. (2013). Treating Childhood and Adolescent Anxiety. John Wiley & Sons, Inc. https://doi.org/10.1002/9781118589366
- Lebowitz, E. R., Omer, H., Hermes, H., & Scahill, L. (2014). Parent training for childhood anxiety disorders: The SPACE program. Cognitive and Behavioral Practice, 21(4), 456–469. https://doi.org/10.1016/j.cbpra.2013.10.004
- Lebowitz, E. R., Silverman, W. K., Martino, A. M., Zagoory‐Sharon, O., Feldman, R., & Leckman, J. F. (2017). Oxytocin response to youth–mother interactions in clinically anxious youth is associated with separation anxiety and dyadic behavior. Depression and Anxiety, 34(2), 127–136. https://doi.org/10.1002/da.22585
- Lebowitz, E. R., Zilcha-Mano, S., Orbach, M., Shimshoni, Y., & Silverman, W. K. (2021). Moderators of response to child-based and parent-based child anxiety treatment: A machine learning based analysis. Journal of Child Psychology and Psychiatry, 62(10), 1175–1182. https://doi.org/10.1111/jcpp.13386
- Lefevre, A., Mottolese, R., Dirheimer, M., Mottolese, C., Duhamel, J. R., & Sirigu, A. (2017). A comparison of methods to measure central and peripheral oxytocin concentrations in human and non-human primates. Scientific Reports, 7(1), 1–10. https://doi.org/10.1038/s41598-017-17674-7
- Leng, G., & Sabatier, N. (2016). Measuring oxytocin and vasopressin: Bioassays, immunoassays and random numbers. Journal of Neuroendocrinology, 28(10). https://doi.org/10.1111/jne.12413
- MacLean, E. L., Wilson, S. R., Martin, W. L., Davis, J. M., Nazarloo, H. P., & Carter, C. S. (2019). Challenges for measuring oxytocin: The blind men and the elephant? Psychoneuroendocrinology, 107, 225–231. https://doi.org/10.1016/j.psyneuen.2019.05.018
- Merolla, J. L., Burnett, G., Pyle, K. V., Ahmadi, S., & Zak, P. J. (2013). Oxytocin and the biological basis for interpersonal and political trust. Political Behavior, 35(4), 753–776. https://doi.org/10.1007/s11109-012-9219-8
- National Institute of Mental Health. (2015). National Institute of Mental Health strategic plan for research. DHHS Publication No. 15–6368.
- Palgi, S., Klein, E., & Shamay-Tsoory, S. G. (2016). Oxytocin improves compassion toward women among patients with PTSD. Psychoneuroendocrinology, 64, 143–149. https://doi.org/10.1016/j.psyneuen.2015.11.008
- Priel, A., Djalovski, A., Zagoory‐Sharon, O., & Feldman, R. (2019). Maternal depression impacts child psychopathology across the first decade of life: Oxytocin and synchrony as markers of resilience. Journal of Child Psychology and Psychiatry, 60(1), 30–42. https://doi.org/10.1111/jcpp.12880
- Pruessner, J. C., Kirschbaum, C., Meinlschmid, G., & Hellhammer, D. H. (2003). Two formulas for computation of the area under the curve represent measures of total hormone concentration versus time-dependent change. Psychoneuroendocrinology, 28(7), 916–931. https://doi.org/10.1016/S0306-4530(02)00108-7
- Schneiderman, I., Zagoory-Sharon, O., Leckman, J. F., & Feldman, R. (2012). Oxytocin during the initial stages of romantic attachment: Relations to couples’ interactive reciprocity. Psychoneuroendocrinology, 37(8), 1277–1285. https://doi.org/10.1016/j.psyneuen.2011.12.021
- Seltzer, L. J., Ziegler, T. E., & Pollak, S. D. (2010). Social vocalizations can release oxytocin in humans. Proceedings of the Royal Society B: Biological Sciences, 277(1694), 2661–2666. https://doi.org/10.1098/rspb.2010.0567
- Sequeira, S. L., Silk, J. S., Ladouceur, C. D., Hanson, J. L., Ryan, N. D., Morgan, J. K., McMakin, D. L., Kendall, P. C., Dahl, R. E., & Forbes, E. E. (2021). Association of neural reward circuitry function with response to psychotherapy in youths with anxiety disorders. The American Journal of Psychiatry, 178(4), 343–351. https://doi.org/10.1176/appi.ajp.2020.20010094
- Shamay-Tsoory, S. G. (2011). The neural bases for empathy. The Neuroscientist, 17(1), 18–24. https://doi.org/10.1177/1073858410379268
- Shamay-Tsoory, S. G., & Abu-Akel, A. (2016). The social salience hypothesis of oxytocin. Biological Psychiatry, 79(3), 194–202. https://doi.org/10.1016/j.biopsych.2015.07.020
- Shamay-Tsoory, S. G., Abu-Akel, A., Palgi, S., Sulieman, R., Fischer-Shofty, M., Levkovitz, Y., & Decety, J. (2013). Giving peace a chance: Oxytocin increases empathy to pain in the context of the Israeli–Palestinian conflict. Psychoneuroendocrinology, 38(12), 3139–3144. https://doi.org/10.1016/j.psyneuen.2013.09.015
- Silverman, W. K., Kurtines, W. M., Jaccard, J., & Pina, A. A. (2009). Directionality of change in youth anxiety treatment involving parents: An initial examination. Journal of Consulting and Clinical Psychology, 77(3), 474–485. https://doi.org/10.1037/a0015761
- Vigo, D., Thornicroft, G., & Atun, R. (2016). Estimating the true global burden of mental illness. The Lancet Psychiatry, 3(2), 171–178. https://doi.org/10.1016/S2215-0366(15)00505-2
- Weisman, O., Feldman, R., Burg-Malki, M., Keren, M., Geva, R., Diesendruck, G., & Gothelf, D. (2015). Mother–child interaction as a window to a unique social phenotype in 22q11. 2 deletion syndrome and in Williams syndrome. Journal of Autism and Developmental Disorders, 45(8), 2567–2577. https://doi.org/10.1007/s10803-015-2425-6
- Weisz, J. R., Kuppens, S., Ng, M. Y., Eckshtain, D., Ugueto, A. M., Vaughn-Coaxum, R., Jensen Doss, A., Hawley, K. M., Krumholz Marchette, L. S., & Chu, B. C. (2017). What five decades of research tells us about the effects of youth psychological therapy: A multilevel meta-analysis and implications for science and practice. The American Psychologist, 72(2), 79. https://doi.org/10.1037/a0040360
- White, L., & Pine, D. (2017). 781. Amygdala-based connectivity on the dot-probe task: Associations with pediatric anxiety and treatment response. Biological Psychiatry, 81(10), S317. https://doi.org/10.1016/j.biopsych.2017.02.848
- Zilcha-Mano, S. (2017). Is the alliance really therapeutic? Revisiting this question in light of recent methodological advances. The American Psychologist, 72(4), 311. https://doi.org/10.1037/a0040435
- Zilcha-Mano, S. (2020). Toward personalized psychotherapy: The importance of the trait-like/state-like distinction for understanding therapeutic change. The American Psychologist, 76(3), 516–528. https://doi.org/10.1037/amp0000629
- Zilcha-Mano, S., & Fisher, H. (2022). Distinct roles of state-like and trait-like patient–therapist alliance in psychotherapy. Nature Reviews in Psychology, 1(4), 194–210. https://doi.org/10.1038/s44159-022-00029-z
- Zilcha-Mano, S., Goldstein, P., Dolev-Amit, T., Ben David-Sela, T., & Barber, J. P. (2021). A randomized controlled trial for identifying the most suitable treatment for depression based on patients’ attachment orientation. Journal of Consulting and Clinical Psychology, 89(12), 985. https://doi.org/10.1037/ccp0000696
- Zilcha-Mano, S., Shamay-Tsoory, S., Dolev-Amit, T., Zagoory-Sharon, O., & Feldman, R. (2020). Oxytocin as a biomarker of the formation of therapeutic alliance in psychotherapy and counseling psychology. Journal of Counseling Psychology, 67(4), 523.. https://doi.org/10.1037/cou0000386
- Zilcha-Mano, S., Solomonov, N., Posner, J. E., Roose, S. P., & Rutherford, B. R. (2022). Proof of concept of the contribution of the interaction between trait-like and state-like effects in identifying individual-specific mechanisms of action in biological psychiatry. Journal of Personalized Medicine, 12(8), 1197. https://doi.org/10.3390/jpm12081197
