ABSTRACT
Multicentric Castleman's disease (MCD) is a rare kind of lymphoproliferative disorder characterized by systemic problems such as frequent fever, fatigue and weight loss with angiofollicular lymph node hyperplasia. However, unlike unicentric Castleman's disease (UCD) with long-time survival by surgery and local radiotherapy, MCD remains poor prognosis due to no well-defined optimal treatment strategies and high risk of developing malignances especially lymphoma. We reported a case of MCD who received chemotherapy by ECHOP with unsatisfactory outcome and then oral administration with thalidomide combined with prednisone without disease progression after therapy. After 3 y, his MCD turned into multiple myeloma (MM) and accompanied by obvious response to combination of thalidomide with prednisone. Nowadays, there is no standard of therapy yet established for MCD. We successfully treated one such patient and found thalidomide based therapy may have a significant effect on MCD. We also proposed further researches with therapeutic potential about thalidomide for MCD.
Introduction
Castleman disease (CD) is a rare kind of lymphoproliferative disorder, which was first described by Castleman and Towne in 1954Citation1. Histologically, CD can be classified as the hyaline-vascular or plasma-cell group and occasional case demonstrating mixed varieties(2). According to the clinical manifestations, there are two disparate sub-classifications of CD: unicentric (UCD) and multicentric (MCD). Patients with UCD have localised disease and almost without systemic features, achieving long-term survival after mass resectionCitation3. While compared with UCD, MCD is a systemic disease which presents a variety of symptoms, such as fever, weight loss, peripheral lymphadenopathy and worse prognosis. Also, MCD was considered to be associated with human herpes virus (HHV-8) and human immunodeficiency virus (HIV) infections, but its pathogenesis remains unclear.
Although the CD primarily is a benign lymphoproliferative disorder, it has high risk of developing into certain malignancies such as lymphoma, kaposi's sarcoma or plasma cell dyscrasia. It most commonly turns into lymphoma but rarely transform into multiple myeloma (MM) as presented in our case. Here, we will report a 72 y old man who had MCD and then developed into MM, and successful treated with thalidomide.
Presentation of case
The history of present of illness
A 72-year-old man was presented with recurrent fever accompanied with weight loss for 6 months, and he was referred to our hospital for further examination and treatment in June 2010. He had no other constitutional symptoms such as cough, sputum, stomachache and diarrhea and past medical, personal and family history were also no special. On physical examination, he presented with left axillary and right inguinal lymph node of 0.5 cm in size and splenomegaly. Once he was hospitalized, we carried out the relevant laboratory tests, the results were as follows.
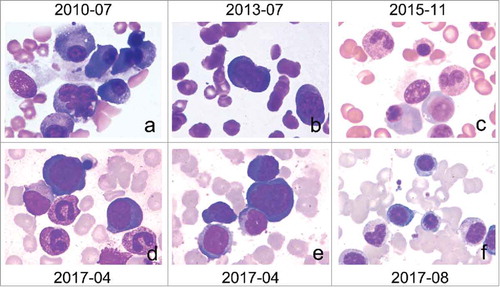
He had moderate anemia with hemoglobin count of 80 g/L, platelet count of 120*109/L, leukocyte count of 2.4*109/L. We also noticed signs of inflammatory with increased erythrocyte sedimentation rate (ESR) (65 mm), high C reaction protein (CRP) (71.80 mg/L) and high serum ferritin (>2000 ng/ml). And serum beta 2 microglobulin increased significantly to above 4.0 ug/ml. The function of renal and liver and the level of LDH were normal (178 U/L). The concentrations of most tumor markers, rheumatoid factor and autoimmune disease related antibody including antinuclear antibodies, anti Sm antibody and antistreptolysin O were normal. And the purified protein derivative (PPD) antibody tests, widal reaction, serological HIV, herpes simplex and EB virus antibody, cytomegalovirus antibody and blood culture were all negative. Chest and abdomen CT scan revealed many small pulmonary nodules and a small quantity of pleural effusion on both sides, retroperitoneal lymph nodes, prostatic hyperplasia with calcification. Abdominal Doppler ultrasound showed hydrops of gallbladder and splenomegaly (149 mm). And the appearances of bone marrow smear were bone marrow active hyperplasia, granulocyte cytoplasm particles increased and common bloodthirsty cells as showed in picture A of , which not suggested hematological malignancies.
Figure 1. Bone marrow cytomorphologic examination: a. Bone marrow primarily showed active hyperplasia, granulocyte cytoplasm particles increased and common bloodthirsty cells in the July 2010. b. Reexamination of bone marrow due to negative outcome of chemotherapy for MCD showed the same with the last which not suggested hematological malignancies in July 2013. c. In November 2015 the bone marrow showed Active bone marrow hyperplasia, mature plasma cells increased, accounting for 7.0%. d and e. In April 2017, the patient came to hospital due to fever with pancytopenia and bone marrow showed plasma cells obviously increased with 29.5%, and proplasmacyte seen, which can be diagnosed MM accompanied with other examination. f. After therapy, Reexamination of bone marrow was positive with the plasma cells decrease to 3.5% in August 2017.
The diagnosis and treatments of MCD
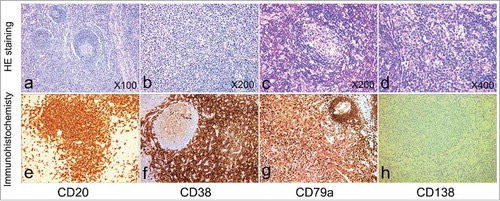
Given the superficial lymph nodes were too small to be biopsied and the cause of fever cannot be definite, the treatment approach was only against infection with amoxicillin and levofloxacin. But the patient's temperature had been dropped after one week and then been discharged. But after 10 d, he came to hospital again due to fever. The clinical symptoms were more serious than the last time, such as severe anemia, aggravated thrombocytopenia (hemoglobin count of 48 g/L, platelet count of 44*109/L) and the left cervical lymph nodes of 1.0 cm in size noticed. And the lymph node biopsy showed lymphoid hyperplasia with numerous plasma cells in interfollicular region in July 2010 as showed in Immunohistochemistry revealed in cluster of differentiation 38 (+++), MUM-1 (+++), cluster of differentiation 21 (+ in follicular dendritic cells), cluster of differentiation 35 (+ in follicular dendritic and plasma cells), cluster of differentiation 20 (+ in B cells), cluster of differentiation 79 a (+ in B cells), cluster of differentiation 138 (-), cluster of differentiation 3 (-), cluster of differentiation 45RO (-), Ki-67 (60%). The overall features were consistent with plasma-cell multicentric Castleman disease. And then chemotherapy of cyclophosphamide, vincristine, doxorubicin and prednisone with VP16 (ECHOP) regimen were initiated in July 2010. And the temperature and hemoglobin, the platelet count gradually recovered normal during treatment (7/2010–11/2010). But from February 2013, he had recurrent fever again and not responded to antibiotic. Given that, we thought MCD was advanced and the chemotherapy of ECHOP was used but the effect was not as expected. And after three courses of ECHOP therapy, the patient received chemotherapy of oral thalidomide combined with prednisone (oral 200 mg thalidomide per night and prednisone 60 mg per day for 7 d every month) in July 2013. After that, patient exhibited evident clinical improvement in health status with obvious reduction in frequency of fever. When the patient felt good, we adjusted the dose of the drugs (oral 200 mg thalidomide per night every two weeks and prednisone 45 mg per day for 7 d every month) in November 2015. During the therapy, the patient had occasional fever and we thought it should be attributed to infection rather than MCD, because of using steroid in long term.
Figure 2. Histological findings: The left cervical lymph node biopsy in patient. a-d: The hematoxylin and eosin stained section showed lymphoid hyperplasia with numerous plasma cells in interfollicular region and no hyaline vascular in July 2010. Immunohistochemistry features: e. cluster of differentiation 38 antibody confirming the presence of numerous plasma cells f. cluster of differentiation 20 (+) g. cluster of differentiation 79a (+) h. cluster of differentiation 138 (-).
MCD transformed into MM
In April 2017, the patient came to hospital due to fever with pancytopenia. Then we took further examination and found the transform from MCD into MM in bone marrow in which plasma cells obviously increased with 29.5%, and proplasmacyte seen as showed in and . And the blood cell count showed the hemoglobin count of 77 g/L, platelet count of 39*109/L, leukocyte count of 3.8*109/L, abnormal lymphocytes count for 3% and 9% abnormal cells. The karyotype analysis was normal but the result of Ig gene rearrangement was positive. Blood biochemical index demonstrated: total protein (59.4 g/L), albumin (28.60 g/L), globulin (30.80 g/L) and the ratio of albumin to globulin (0.93), the function of renal and liver was normal but the level of LDH were increased to 417 U/L and serum beta 2 microglobulin was 3.235 ug/ml. The level of CRP was increased to 214 mg/L. ESR was 120 mm60 min, urine protein and Bence Jones protein was positive but blood calcium was normal. The immunoglobulin showed IgA 1.11 g/L, IgG 25.60 g/L, IgM 0.37 g/L. Given those results, the patient was diagnosed as IgG type MM.
The subsequent treatments and outcome
According to the treatments for MM, the patient received monthly cycles of bortezomib 3 mg intravenously on d 1,8 and dexamethasone 20 mg on d 1,2,8,9 for three cycles. But due to economic pinch, the patient had to discontinue medication of bortezomib and only take oral thalidomide combined with prednisone. In the process of therapy, the therapy of oral thalidomide combined with prednisone was not stopped and continued up till now.
During therapy, complete blood count was examined at each weekly visit and renal function, liver function test and serum protein electrophoresis was tested every month. And after treatments, the patients presented marked improvement in the form of increased hemoglobin count and platelet count as showed in , no recurrent fever, disappearance of urine protein, normal level of LDH, decreased IgG and CRP. And the bone marrow plasma cells were 3.5%. Presently, he is in very good partial remission without fever.
Figure 3. The variations of laboratory parameters. The picture of A and B represent respectively Hemoglobin and Platelet counts of the patient and these parameters was tested before transfusions with blood cells or platelet. (C) C-reactive protein (CRP): the level of CRP has not been decline when used ECHOP regimens but there had been obvious respond to thalidomide. And when the patient was diagnosed MM, the CRP had been increased dramatically. a: the patient was diagnosed plasma-cell MCD. a-b: the patient received chemotherapy of cyclophosphamide, vincristine, doxorubicin and prednisone with VP16 (ECHOP) regimen. c: the patient started oral thalidomide combined with prednisone because the MCD was advanced and the effect of chemotherapy was not as expected. d: the MCD turned to MM and the laboratory parameters was both worsen, but then have been better gradually after therapy.
Discussion
According to pathological presence of lymphadenopathy, CD is principally divided into UCD and MCD. MCD was firstly reported in 1978 by Gaba, who described a patient with retroperitoneal and axillary lymphadenopathy characterized histologically by the hyaline vascular type of giant lymph node hyperplasia with plasma cell infiltrate in each region.Citation4 And due to rarity and clinical heterogeneity of CD, there are no diagnostic codes for CD, UCD or MCD in national databases, which contributed to difficult expression for accurate epidemiology of CD. But recently, Nikhil et al. used a claims database to characterize and estimate the incidence rate for CD, and they found the incidence was 21–25 cases per million person-y, with 23% of those cases potentially suffering from MCD.Citation5 Furthermore, UCD has a good prognosis with 10-year overall survival of 95% by surgery and local radiotherapy.Citation3 Conversely, prognosis for patients with MCD remains poor and no well-defined optimal treatment strategy.
Though significant discovers about CD over the past 20 y, the etiology and pathogenesis of CD still remains undefined. MCD is considered to be associated with HHV-8 and HIV infections, and there is also a part of HHV-8-negative and HIV-negative patients called as idiopathic MCD (iMCD).Citation6 And our case may be classified into iMCD due to the negative HIV and human herpes simplex and EB virus antibody. In addition, the pathogenic contribution of IL-6, a potent stimulant for B lymphocyte and plasma cell growth, has been shown in the CD. And Brandt et al had found IL-6 could aggravate some symptoms such as lymphadenopathy, anemia and hypoalbuminemia in mice.Citation7 Given these results, many experiments have been ongoing to study anti-IL-6 monoclonal antibody therapy for MCD, which may be a novel therapeutic target in the future.Citation8 In our case, we didn't detect the level of IL-6, but some studies have showed the IL-6 can stimulate the production of CRP and anti-IL-6 therapy can abolish CRP production, which is considered a convenient marker of IL-6 level.Citation9 Form the , the patient CRP level had been charged according to the state of the illness and when the CD turned to MM, the CRP had been increased dramatically, which may associate with the expression level of IL-6.
Although CD is a rare benign lymphoproliferative disorder, it has a high risk of developing into malignances especially lymphoma. And some researchers have shown that HIV-negative patients presenting the transformation and non-Hodgkin's lymphoma (NHL) is more often associated with MCD.Citation10 But the turn form CD to MM has been reported very rarely as in our case. Afaq et al in 2012 described a 51-year-old man who had MCD accompanying MM associated with cutaneous vasculitis achievedgood partial remission by using bortezomib.Citation11 The mechanism about MCD associated with MM has not been well understood. Maybe the transformation to MM is attributed to the high expression level of IL-6 in these two diseases, which need further research.
The MCD shows a more aggressive deterioration with poor prognosis, and optimal therapies have not been well defined. A number of therapies have been utilized, such as cytotoxic chemotherapy, immunomodulators, bortezomib, antibodies against CD20 or IL-6 and its receptor.Citation12 Despite administration with these treatments, the median survival of MCD reportedly ranges from 14 to 30 months.Citation13 Therefore, the normative and effective management for MCD is needed. In the present case, the patient received chemotherapy by ECHOP without good outcome and then took oral thalidomide combined with prednisone. He had been in good situation for 3 y without disease progression after the therapy. But after 3 y, his disease had turned into MM. He had been received bortezomib for MM at first while he asked to stop use bortezomib due to the high expense after three cycles. The patients have been insisting on oral thalidomide combined with prednisone from the beginning. Given the outcome, we think the thalidomide may play an important role in our case. And it is also consistent with several previous results.Citation14
Thalidomide is a kind of immunomodulatory drug used commonly in the treatment of hematological tumor such as MM and myelodysplastic syndrome (MDS), which may be associated with the capacity of blocking production of IL-6. The effect of thalidomide on MCD has not been established yet. Lee et al in 2003 reported the first case report of MCD who showed a dramatical response to single agent thalidomide for one year.Citation14 In this case, we took longer time to treat and observe the state of the patient with thalidomide and prednisone. The outcomes suggest thalidomide may not only improve the symptoms but lengthen survival for MCD patients, which need large sample analysis to verify and evaluate. Given this, we think the combination of thalidomide with prednisone have a significant therapeutic role in MCD and turned MM form MCD, which may provide a promising and therapeutic treatment for MCD patients in the future.
Consent
Witten informed consent was obtained from the patient for publication of this case report and any accompanying images.
Disclosure of potential conflicts of interest
No potential conflicts of interest were reported.
Acknowledgments
This work was supported by the Municipal Science and Technology Bureau of Nanjing under Grant (YKK13116). Special thanks to the Youcai Zhao and Shibin Cao for supplying photomicrographs.
Additional information
Funding
References
- Castleman B, Towne VW. Case records of the Massachusetts General Hospital: Case No. 40231. N Eng J Med. 1954;250(23):1001–5. doi:10.1056/nejm195406102502308. PMID:13165944.
- Wang HW, Pittaluga S, Jaffe ES. Multicentric Castleman disease: Where are we now? Semin Diagn Pathol. 2016;33(5):294–306. doi:10.1053/j.semdp.2016.05.006. PMID:27296355.
- Talat N, Belgaumkar AP, Schulte KM. Surgery in Castleman's disease: a systematic review of 404 published cases. Ann Surg. 2012;255(4):677–84. doi:10.1097/SLA.0b013e318249dcdc. PMID:22367441.
- Gaba AR, Stein RS, Sweet DL, Variakojis D. Multicentric giant lymph node hyperplasia. Am J Clin Pathol. 1978;69(1):86–90. doi:10.1093/ajcp/69.1.86. PMID:619617.
- Munshi N, Mehra M, van de Velde H, Desai A, Potluri R, Vermeulen J. Use of a claims database to characterize and estimate the incidence rate for Castleman disease. Leukemia & lymphoma. 2015;56(5):1252–60. doi:10.3109/10428194.2014.953145.
- Fajgenbaum DC, van Rhee F, Nabel CS. HHV-8-negative, idiopathic multicentric Castleman disease: novel insights into biology, pathogenesis, and therapy. Blood. 2014;123(19):2924–33. doi:10.1182/blood-2013-12-545087. PMID:24622327.
- Brandt SJ, Bodine DM, Dunbar CE, Nienhuis AW. Dysregulated interleukin 6 expression produces a syndrome resembling Castleman's disease in mice. J Clin Invest. 1990;86(2):592–9. doi:10.1172/JCI114749. PMID:2384605.
- Suthaus J, Stuhlmann-Laeisz C, Tompkins VS, Rosean TR, Klapper W, Tosato G, Janz S, Scheller J, Rose-John S. HHV-8-encoded viral IL-6 collaborates with mouse IL-6 in the development of multicentric Castleman disease in mice. Blood. 2012;119(22):5173–81. doi:10.1182/blood-2011-09-377705. PMID:22490805.
- Rossi JF, Lu ZY, Jourdan M, Klein B. Interleukin-6 as a therapeutic target. Clin Cancer Res: an official journal of the American Association for Cancer Research. 2015;21(6):1248–57. doi:10.1158/1078-0432.CCR-14-2291. PMID:25589616.
- Larroche C, Cacoub P, Soulier J, Oksenhendler E, Clauvel JP, Piette JC, Raphael M. Castleman's disease and lymphoma: report of eight cases in HIV-negative patients and literature review. Am J Hematol. 2002;69(2):119–26. doi:10.1002/ajh.10022. PMID:11835348.
- Khan AA, Siraj F, Bhargava M, Aggarwal S. Successful treatment of multicentric Castleman's disease accompanying myeloma with bortezomib. Bmj Case Rep. 2012;2012. pii: bcr2012007646. doi:10.1136/bcr-2012-007646. PMID:23264156.
- Chan KL, Lade S, Prince HM, Harrison SJ. Update and new approaches in the treatment of Castleman disease. J Blood Med. 2016;7:145–58. doi:10.2147/JBM.S60514. PMID:27536166.
- Madan R, Chen JH, Trotman-Dickenson B, Jacobson F, Hunsaker A. The spectrum of Castleman's disease: mimics, radiologic pathologic correlation and role of imaging in patient management. Eur J Radiol. 2012;81(1):123–31. doi:10.1016/j.ejrad.2010.06.018. PMID:20643523.
- Lee FC, Merchant SH. Alleviation of systemic manifestations of multicentric Castleman's disease by thalidomide. Am J Hematol. 2003;73(1):48–53. doi:10.1002/ajh.10310. PMID:12701121.
