ABSTRACT
Nuclear protein in testis (NUT) midline carcinoma (NMC) is a rare malignant tumor defined by a unique chromosomal translocation of the NUT gene on chromosome 15q14. This very rare tumor is usually located in midline structures, especially in the head and neck region. However, there have been no previous reports of NMC arising from the eyes. Here, we first describe a case of NMC originating in the right orbit of a 60-year-old woman. A multimodality approach, including surgery, chemotherapy, radiotherapy, and target therapy, was adopted in clinical practice.
Background
Nuclear protein in testis (NUT) midline carcinoma (NMC) is a rare, aggressive, and fatal carcinoma characterized by chromosomal rearrangements of the NUT gene on 15q14.Citation1 NMC typically arises within the midline structures, which include the head, neck, and mediastinum. Tumors outside the midline have also been reported, such as the urinary bladder, iliac bone, pancreas, parotid gland, and lung.Citation2 Currently, NMC is diagnosed by FISH using NUT split-apart probes.Citation3 Another simple but highly sensitive and specific test for NMC is immunochemistry with NUT monoclonal antibody.Citation4 NMC is refractory to conventional chemotherapy and radiotherapy.Citation5 No consensus has been reached concerning the optimal treatment strategy.
This report describes the first case of NMC arising from the right orbit of an adult female and highlights new treatment options for this neoplasm.
Case report
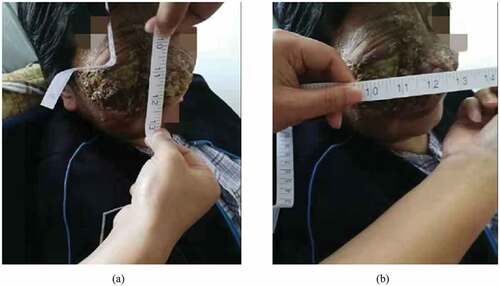
In April 2018, a 60-year-old female complaining about pain in her right eye was admitted in the hospital. A mass measuring about 8 cm×9 cm was noted wrapping around her right eye. The mass was ruptured in the surface and was accompanied with tenderness ().
Figure 1. A tough mass measuring about 8 cm×9 cm was seen in the right eye, accompanied with tenderness and surface rupture.

A detailed inquiry was made for her medical history. She firstly sought medical attention due to the foreign body sensation within the right eye in October 2017 in a tertiary hospital. Cranial magnetic resonance imaging (MRI) revealed a mass in the right orbit which was involved in the right maxillary sinus and the right ethmoid sinus. Positron emission tomography – computed tomography (CT) showed avid fluoroudeoxyglucose uptake in the region of the right orbit and right nasal cavity. She subsequently underwent a resection of the mass. FISH evaluation demonstrated NUT rearrangement. Immunohistochemical stain for NUT protein showed that the tumor cells were positive for NUT monoclonal antibodies. Based on the histopathological examination, the woman was definitively diagnosed with NMC. No additional treatment such as chemotherapy or radiotherapy was added immediately following the surgery except for traditional Chinese medicine. However, the tumor relapsed soon. In January 2018, she began to feel pain in the right eye. Two months later, a mass was found in her right neck, which was diagnosed as swollen subcutaneous lymph nodes by ultrasound. Punch biopsy confirmed metastatic malignant tumor. Since she could not bear the pain, she asked for medical help.
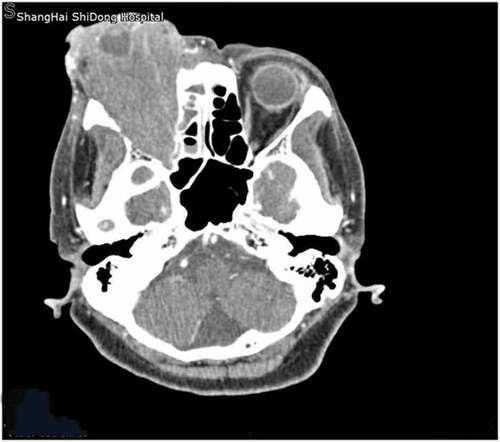
After admission in our hospital, a CT scan revealed a 7.5 cm- × 4.1-cm-sized mass located in the right orbit, which invaded the ocular muscle, ophthalmic nerve, the right maxillary sinus, ethmoid sinus, sphenoid sinus, and the soft tissue of the right cheek (). As the patient just pursued palliative pain relief at that time, she was administered with OxyContin, gabapentin along with acetaminophen. Then, she was discharged home.
Figure 2. Orbit computed tomography (CT) with intravenous contrast showed a 7.5-cm- × 4.1-cm-sized mass arising from the right orbit. The mass extended toward the right-sided maxillary sinus, ethmoid sinus, and frontal sinus.
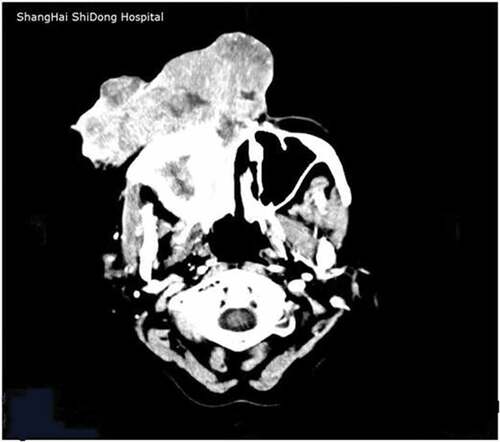
In June 2018, the tumor became larger and infiltrated the right nasal cavity ( and ), so she had visual disorder, greater pain, and difficulty breathing. In addition, a lymph node of 3 cm was palpated in her right neck. Contrast-enhanced cranial CT scan revealed that the right orbital tumor had invaded bilateral maxillary sinus, ethmoid sinus, and frontal sinus (). Chemotherapy was initiated with docetaxel 60 mg/m2 on day 1, cisplatin 60 mg/m2 on days 1 to 3, and avastin 375 mg on day 1 at 3-week intervals. However, the tumor still rapidly progressed. After discussions with the radiation oncologist, a total dose of 60 Gy in 30 fractions of radiotherapy was administrated to the primary site. At the end of radiotherapy, the primary cancer tended to shrink ( and ).
Figure 3. The tumor measuring 14 cm (a) × 15 cm (b) extended onto the right nasal cavity, which led to the shortness of breath.

Figure 4. Contrast-enhanced CT imaging of the head revealed the tumor occupied the right orbit and was involved in the nasal cavity.
Considered the very aggressive feature of NMCs, we discussed the following therapeutic regimen. As unpublished data of clinical experiments in anlotinib hydrochloride, a novel small molecule multitarget tyrosine kinase inhibitor, showed great efficiency for a wide spread of cancers, the same strategy was adopted in the current case. Before target therapy, MRI was applied (). The patient was prescribed with anlotinib hydrochloride with a dose of 12 mg for 14 days, every 3 weeks. Three months later, the tumor was remarkably decreased in size (). Notably, MRI demonstrated a reduction in radiodensity of the primary lesion (). She is still alive 15 months after the original diagnosis.
Figure 6. MRI image of the tumor prior to anlotinib hydrochloride. The tumor was located in the right orbit, with massive extension into the right maxillary sinus, ethmoid sinus, frontal sinus, sphenoid.
Discussion
NMC is a rare aggressive cancer which is typified by a reciprocal translocation between chromosomes 15 and 191 . Though initially described in adolescents and young adults, this tumor can actually occur at any age.Citation6 The median age of onset reported in the literature is 21.9 years (range: 0.1–81.7 years).Citation7 NMC most often affects midline structures, particularly in the head and neck or lung and mediastinum.Citation8,Citation9 Tumors outside the midline have also been described: pancreas,Citation10 bladder,Citation3 or iliac bone.Citation11 However, there have been no previous reports of NMC developing from the eye. Here, we describe the first case of NMC arising from the right orbit in a 60-year-old woman, further suggesting that this tumor is possible to occur at any sites.
Since lack of distinct clinical presentation and histologic features, NMC was probably misdiagnosed before.Citation1 However, monoclonal NUT-specific antibody (C52) has been developed to detect the NUT protein with a sensitivity of 87% and a specificity of 100%.Citation4 For a confirmative diagnosis, karyotyping, FISH, or NUT mRNA by reverse transcription polymerase chain reaction can be used to detect the NUT gene rearrangement.Citation6
NMC is considered a very aggressive malignancy with unfavorable outcomes. Over 80% patients will die within one year since the diagnosis.Citation1 Therefore, effective treatment is warranted. There has been no established therapy for NMC yet. In a retrospective analysis of 40 patients with head and neck NMCs, Chau et al. found that surgical resection, especially the extent of surgical resection, was significantly associated with improved Overall survival (OS) and progression-free survival (PFS).Citation7 However, because of the nonspecific initial clinical presentation, NMC is often widely metastatic and unresectable at diagnosis. Thus, most patients have received radiation and/or combined multidrug chemotherapy. In a retrospective analysis, early radiation therapy was a predictor of improved survival.Citation3 After receiving radiation therapy, our patient also had an objective clinical response. In contrast to the demonstrated benefit of surgical resection and radiotherapy, no available chemotherapy regimens have been associated with improved outcome in NMCs.Citation1 In a retrospective multicenter study, chemotherapeutic agents including alkylating agents, platinum compounds, and anthracyclines were used alone or in combination. However, only a very transient response rate of 36% was observed, followed by tumor progression regardless of the drug regimens used.Citation12
Recent studies have shed light on the role of new targeted treatment regimens. Bromodomain inhibitorsCitation13 have been shown to have promising efficacy in this cancer. Histone deacetylase inhibitor, which restores chromatin acetylation, is another potential therapy for NMCs.Citation14 However, they are both in clinical trial and have not been available yet. Therefore, alternative treatment option is imperative for our patient. Anlotinib hydrochloride is a novel small molecule multitarget tyrosine kinase inhibitor, which can effectively inhibit kinases such as vascular endothelial growth factor receptor (VEGFR), platelet-derived growth factor receptor (PDGFR), fibroblast growth factor receptor (FGFR), and c-Kit. It is proved to have pleiotropic anticancer properties, especially antitumor angiogenesis and tumor growth inhibition. Unpublished data of clinical trials showed evidently improved PFS and OS in various cancers, such as non-small cell lung cancer, soft tissue sarcoma, gastric cancer, and colorectal cancer. Given that there is no effective treatment for NMCs currently,Citation1,Citation7,Citation12 we considered anlotinib hydrochloride as a combined therapy. Surprisingly, the primary tumor was found to have a continuum decrease in size. Moreover, the MRI indicated decreased radiodensity of the original lesion, suggesting that this patient had an encouraging response to anlotinib hydrochloride.
In this report, we firstly presented a case of NMC which developed in the right orbit of an adult woman. The combination of multimodality therapies indicates the extremely aggressive feature of this tumor. The successfully tentative use of anlotinib hydrochloride provides a candidate for inclusion in future combination approaches for NMCs.
Disclosure of interest
No potential conflicts of interest were disclosed.
References
- Bauer DE, Mitchell CM, Strait KM, Lathan CS, Stelow EB, Luer SC, Muhammed S, Evans AG, Sholl LM, Rosai J, et al. Clinicopathologic features and long-term outcomes of NUT midline carcinoma. Clin Cancer Res. 2012;18(20):5773–5779. doi:10.1158/1078-0432.
- Polsani A, Braithwaite KA, Alazraki AL, Abramowsky C, Shehata BM. 2012. NUT midline carcinoma: an imaging case series and review of literature. Pediatr Radiol. 42(2):205–210. doi:10.1007/s00247-011-2272-3.
- French CA, Kutok JL, Faquin WC, Toretsky JA, Antonescu CR, Griffin CA, Nose V, Vargas SO, Moschovi M, Tzortzatou-Stathopoulou F, et al. Midline carcinoma of children and young adults with NUT rearrangement. J Clin Oncol. 2004;22(20):4135–4139. doi:10.1200/JCO.2004.02.107.
- Haack H, Johnson LA, Fry CJ, Crosby K, Polakiewicz RD, Stelow EB, Hong SM, Schwartz BE, Cameron MJ, Rubin MA, et al. Diagnosis of NUT midline carcinoma using a NUT-specific monoclonal antibody. Am J Surg Pathol. 2009;33(7):984–991. doi:10.1097/PAS.0b013e318198d666.
- Bishop JA, French CA, Ali SZ. 2016. Cytopathologic features of NUT midline carcinoma: A series of 26 specimens from 13 patients. Cancer Cytopathol. 124(12):901–908. doi:10.1002/cncy.21761.
- French CA. Pathogenesis of NUT midline carcinoma. Annu Rev Pathol. 2012;7:247–265. doi:10.1146/annurev-pathol-011811-132438.
- Chau NG, Hurwitz S, Mitchell CM, Aserlind A, Grunfeld N, Kaplan L, Hsi P, Bauer DE, Lathan CS, Rodriguez-Galindo C, et al. Intensive treatment and survival outcomes in NUT midline carcinoma of the head and neck. Cancer. 2016;122(23):3632–3640. doi:10.1146/annurev-pathol-011811-132438.
- Den Bakker MA, Beverloo BH, van Den Heuvel-Eibrink MM, Meeuwis CA, Tan LM, Johnson LA, French CA, van Leenders GJ. 2009. NUT midline carcinoma of the parotid gland with mesenchymal differentiation. Am J Surg Pathol. 33(8):1253–1258. doi:10.1146/annurev-pathol-011811-132438.
- Ziai J, French CA, Zambrano E. 2010. NUT gene rearrangement in a poorly-differentiated carcinoma of the submandibular gland. Head Neck Pathol. 4(2):163–168. doi:10.1146/annurev-pathol-011811-132438.
- Shehata BM, Steelman CK, Abramowsky CR, Olson TA, French CA, Saxe DF, Ricketts RR, Katzenstein HM. 2010. NUT midline carcinoma in a newborn with multiorgan disseminated tumor and a 2-year-old with a pancreatic/hepatic primary. Pediatr Dev Pathol. 13(6):481–485. doi:10.2350/09-10-0727-CR.1.
- Mertens F, Wiebe T, Adlercreutz C, Mandahl N, French CA. 2007. Successful treatment of a child with t(15;19)-positive tumor. Pediatr Blood Cancer. 49(7):1015–1017. doi:10.1002/pbc.20755.
- Lemelle L, Pierron G, Freneaux P, Huybrechts S, Spiegel A, Plantaz D, Julieron M, Dumoucel S, Italiano A, Millot F, et al. NUT carcinoma in children and adults: A multicenter retrospective study. Pediatr Blood Cancer. 2017;64:12. doi:10.1002/pbc.26693.
- Mirguet O, Gosmini R, Toum J, Clement Ca, Barnathan M, Brusq Jm, Mordaunt Je, Grimes Rm, Crowe M, Pineau O et al. Discovery of epigenetic regulator I-BET762: Lead optimization to afford a clinical candidate inhibitor of the BET bromodomains. J Med Chem. 2013;56(19):7501–7515. doi:10.1021/jm401088k.
- Schwartz BE, Hofer MD, Lemieux ME, Bauer DE, Cameron MJ, West NH, Agoston ES, Reynoird N, Khochbin S, Ince TA, et al. Differentiation of NUT midline carcinoma by epigenomic reprogramming. Cancer Res. 2011;71(7):2686–2696. doi:10.1158/0008-5472.CAN-10-3513.