Abstract
Objective
Improvements in road infrastructure and vehicle safety have been achieved in many countries during the last decades. As the number of fatalities have dropped, the consequences of non-fatal injuries have been brought into focus. Therefore, the objective was to investigate self-reported health status and health-related quality of life several years after the crash for road-users that sustained injuries resulting in permanent medical impairment (PMI).
Methods
A self-administered questionnaire using instruments to measure if health, health-related quality of life and physical activity had been affected by the crash, were used. The injured road-users were identified from insurance policy holders of the Folksam Insurance Group. The response rate was 29%, a total of 2078 responses were received from the 7174 road-users with PMI that received the questionnaire.
Results
In total 85% were still suffering from the injuries several years after the crash (8-18 year after the crash). Furthermore, road-users with injuries to the spine were having highest pain intensity. Older road-users had poorer self-reported health status than younger road-users. Although, younger road-users had the greatest change in physical activity when comparing before and after the crash. Before the crash in total 63% were physically active while only 34% after the crash. The higher the PMI the higher it affected health several years after the crash.
Conclusions
The Swedish definition of serious injury, an injury leading to PMI, was found to correlate with self-reported health loss; 85% of the injured road-users reported that they still had remaining symptoms several years after the accident. The injured body region leading to PMI after an accident can vary from the body regions reported to cause long-term health loss. It was found that the higher the degree of PMI the higher the health loss. Sustaining a PMI regardless severity and injured body region has the same effects on general health for men and women. Sustaining a PMI will both lower the health-related quality of life and physical activity after the crash compared to before.
Introduction
Road traffic injuries constitute a major public health problem. Improvements in road infrastructure and vehicle safety have had a positive effect on casualties in many countries during the last decades (Strandroth Citation2015). As the number of fatalities have dropped, the consequences of non-fatal injuries have been brought into focus. For example, in 2008 the Swedish Transport Administration extended the definition of serious injuries to include injuries leading to permanent medical impairment (PMI). This definition is based on insurance data to classify if an injured road user still had residual symptoms three years after a crash. Focusing on non-fatal injuries leading to PMI, the vast majority are AIS 1 injuries (Gustafsson et al. Citation2015, Stigson et al. Citation2015). Therefore, using long-term outcomes provides a different picture of road traffic injuries compared to using initial injury diagnoses (Tingvall et al. Citation2013) . By studying injury outcomes among various types of road users different patterns will also be possible to identify. However, a study only showed small variations regarding the consequences following a crash among different road user types (Mayou and Bryant Citation2003). A systematic literature review showed that regardless which instrument was used the quality of life decreased significantly among individuals injured in a crash compared to individuals not injured (Rissanen et al. Citation2017). Older persons, women, individuals with low socioeconomic status, individuals diagnosed with a post-traumatic stress disorder and individuals with severe injuries or injuries to the lower extremity were more prone to have a reduced quality of life after a traffic accident, compared to other groups.
Injuries to the cervical spine as well as brain injuries have been found to affect the future situation in terms of sickness absents for the injured individual to a higher extent (Elrud et al. Citation2017). However, most of the injuries resulting in PMI are injuries to the upper and lower extremities or whiplash associated disorders (Malm et al. Citation2008, Stigson et al. Citation2015). For example, for bicyclists 50% of all injuries resulting in PMI are to the upper extremities (Rizzi et al. Citation2013) and for car occupants 50% of the injuries resulting in PMI are whiplash associated disorders (Stigson et al. Citation2015). To understand to what extent injuries leading to long-term consequences is affecting the health of the injured road users, it is important to gain knowledge of different aspects of health loss. Permanent medical impairment has been established in consensus between physicians, claims adjustment specialists and lawyers who specialize in insurance matters and is used by all insurance companies in Sweden. It does not reflect the self-perceived health status or quality of life (Malm et al. Citation2008). The objective of the present study was to investigate self-reported health status and quality of life several years after the crash for road users with injuries that resulted in PMI.
Method
A self-administered questionnaire in paper form was sent out by mail to individuals injured in a road traffic accident between 2001 and 2013 and where the injury resulted in a PMI. A reminder was sent out one month after the initial survey date. The selection was made from Folksam Insurance Group (Folksam). Folksam is one of the largest Swedish insurance companies, with a market share of car insurances of approximately 20% (4.4 million registered vehicles) and 50% of household insurances. All road users struck by or injured due to a vehicle will be adjusted by the mandatory third-party liability insurance of the vehicle. Vulnerable road users that sustained an injury not involving a motor vehicle will be handled by a specific non-mandatory accident insurance. The policy holders of Folksam can be considered representative of the general population (Elrud et al. Citation2019). In total 7922 individuals were identified. Of these individuals, 640 people had died, 59 were foreign residents, 37 had incomplete questionnaires and 12 had protected personal data. Thus, a total of 748 individuals were excluded. The questionnaire was therefore sent out to 7174 individuals who were over 17 years when they received it. Of these, 4386 were car drivers, 1271 car occupants, 94 motorcyclists, 31 moped, 243 bicyclists injured in collision with motor vehicles, 61 pedestrians and 212 unknown type of road user. In addition, 863 cyclists or pedestrians who were injured in accidents where no motor vehicles were involved (identified via an insurance for personal accidents) were included in the sample.
Initial injury diagnosis coding and permanent medical impairment assessment
All persons included had an injury or injuries that had resulted in PMI. The procedure for all insurance companies in Sweden is that if an injured road user has not recovered within three years, the medical records from before and after the crash will be assessed by medical specialists to see if the injury and the symptoms can be traced to the crash. The assessment will be done according to the guidelines Grading of Medical Impairment Degree. The principles of grading medical impairment were developed in the beginning of the 20th century and established in consensus with physicians. The injury is given a degree of PMI between 1 and 99 percent. Before a PMI is established, a preliminary forecast can be given because the long-term consequences of the injury can be difficult to estimate. Most PMI degrees are decided within five years after the time of the accident, but in some cases even later. In order to consolidate the reliability of the judgment, all impairment degrees that receive a PMI of 10% or more are handled by a national medical committee. The PMI for each injured person is defined as physical and/or mental functional reduction, independent of cause and without regard to the occupation, hobbies or other special circumstances of the injured person. In all the analyses conducted the injury outcome was based on the initial injury in terms of AIS-grade and body region of the injuries that resulted in PMI, except those who had PMI due to Post-traumatic stress disorder (n = 12). These were only included in a part of the analysis.
The questionnaire
The questionnaire consisted of 18 questions with a total of 50 items. It was stated in the beginning of the questionnaire that the participants should answer the questions in relation to the injury that resulted in PMI. This was applied to all questions in the survey. Early in the survey, it was asked whether the individual had remaining symptoms from the injury that resulted in PMI (Question 2). The individuals who answered No to this question completed the questionnaire here after two questions. The others continued to answer the entire questionnaire. The respondents could answer either by post or on the web through an included link. Estimated time to answer the questionnaire was 10-15 minutes, based on a test among a group of colleagues. This information was included in the questionnaire.
Each road user responded to specific questions about several health aspects to obtain additional information regarding how the health and the health-related quality of life had been affected by the crash. One question concerned self-reported general health using a slightly modified version from SF-12, a well-known and validated health questionnaire (Hurst et al. Citation1998). To indicate residual pain following the injuries that resulted in PMI the respondents marked the body regions that were affected on a picture of a human (Bergman et al. Citation2002). The Swedish version of the instrument Patient-Reported Outcomes Measurement Information System (PROMIS-29 V 2.1) (Chaplin et al. Citation2018, Craig et al. Citation2014) was used to measure different dimensions of health. Several applicable aspects of health (physical function, depression, sleep problems, influence of pain on activities, and pain intensity) were selected from the instrument forming an index of health-related quality of life. Pain intensity, included in PROMIS, was measured using a single 0–10 numeric rating scale item with 10 corresponding worst pain. A four-level questionnaire was used to assess leisure time physical activity (Grimby et al. Citation2015). Information including sex, age, type of road user and degree of PMI were collected from Folksam. The initial injury data were obtained from medical records.
The response rate was 29% (34% among women and 24% among men), a total of 2079 responses were received from the 7174 road users with PMI that received the questionnaire. The response rate was lower among young individuals. The higher the PMI the higher response rate (among the ones that responded the average PMI was 4.2 compared to 3.7% among those that did not respond). The injury distribution was similar between among those that respond and those that did not respond.
In total 60 cases had to be excluded from the analyses since the respondent gave responses regarding another accident that the respondent was involved in. To be able to exclude individuals who had a long-term impairment, illness or other long-term health problem before the traffic accident occurred, a question regarding this was included. The participants who answered that they had any of these problems before the traffic accident were given a follow-up question. In 87 cases the respondent indicated that they suffered from other injuries before the crash that highly affected the daily life. These were excluded in the analyses. This question has been used in this way in previous studies (Monarrez-Espino et al. Citation2018). In total 147 cases were excluded resulting in a total of 1932 cases that were used in the analysis. In total 81% of the respondents were car occupants, 10% cyclist injured in a single bicycle crash, 5% cyclist injured in a collision with motor vehicle, 3% were motorcyclist or moped riders and 1% were pedestrians injured in a collision with motor vehicle.
Associations between the self-reported health-related parameters and various categories were evaluated. These categories included individual’s socio-demographic data (sex, age and level of education), crash type, type of injury, injured body region, and PROMIS scores. Chi‐squared test was used to analyze whether there was a difference in proportions between the categories. In all analyses 95 percent confidence intervals (CIs) were used, and p-values from chi‐squared tests were calculated using SPSS (version 25). Additional references can be found in the Appendix.
Results
In total 85% of the respondents were still suffering from the injuries several years after the crash (8-18 year after the crash, on average 13 years). Table A1 provided in Appendix. A high proportion of the respondents had remaining symptoms from a minor injury (66% with MAIS1) and a trend was found that the younger respondents the higher proportion with remaining symptoms (up to 95% among respondents younger than 35 years of age compared to less than 74% among the age group 55 years or older). However, the rate of response was lower among younger respondents.
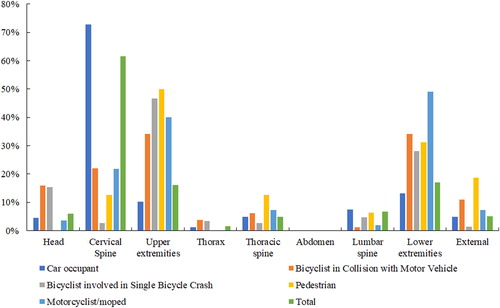
In total 73% of the car occupants that reported remaining symptoms were individuals who sustained a PMI from an initial injury in the cervical spine, . Among bicyclists and pedestrians, the most common body region was upper extremities (47% and 50% respectively) followed by lower extremities. Injuries to lower extremities were most common for motorcyclists/mopeds. Most of the injuries were fractures (53%) for all road users accept for car occupants.
Figure 1. Distribution of body regions for injuries resulting in PMI among different type of road users reporting remaining symptoms.
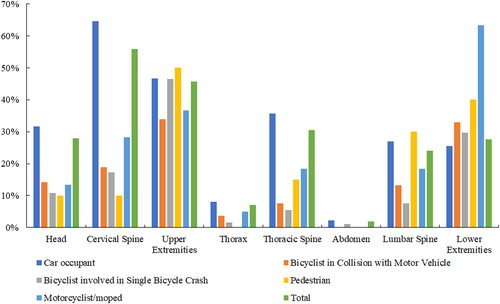
The proportions differ between the body regions that were initial injured and resulted in PMI, and in those the respondents indicate they had residual pain following the injuries that resulted in PMI, and . Only 10% of the car occupants had an injury to the upper extremities, while 47% indicated that they had pain in this body region. A similar result was found for the head (4% had an injury, while 32% indicated pain), thoracic spine (5% had an injury, while 36% indicated pain) and lumbar spine (7% had an injury, while 27% indicated pain). In general, a higher proportion of pain in the lumbar spine was reported for all road users probably indicating an increase in sedentary behavior post-crash. In total 64% of the car occupants reported pain in the cervical spine, while only 10% of the pedestrians. Pain related to the upper extremities was reported by 46% of the road users, and pain in the head, lower extremities and thoracic spine was each reported by approximately 30% of the road users, .
Bicyclist reported better health status than car occupants, . Furthermore, the bicyclist health status was significantly less affected when comparing the health status prior the crash, . Before the crash there was no difference in physical activity but several years after the crash bicyclists were significantly more physically active than car occupants, although the proportion of individuals 45 years or older was significantly higher among bicyclist compared to car occupants (66% respectively 41% p < 0.001), and . In general, road users 45 years or older had significantly poorer self-reported health status than younger road users, although younger road users had the greatest change in physical activity when comparing before and after the crash. Before the crash 63% were in total regularly physically active. The corresponding figure was 34% after the crash. For road users younger than 45 years of age 66% were regularly physically active before the crash and only 34% after the crash. In the age group ≥45 years of age or older 60% were regularly physically active before the crash and 34% after the crash. Respondents with a higher PMI did to a higher extent report a worsened self-reported health status.
Table 1. Self-reported health status in general after the crash.
Table 2. Self-reported health status in relation to prior to the crash.
Table 3. Self-reported physical activity after the crash.
Table 4. Self-reported physical activity in relation to prior to the crash.
When using the instrument PROMIS to measure health-related quality of life some differences could be found. Table A2 provided in Appendix. Post-traumatic stress disorder was also associated with higher loss of health-related quality of life although the number of individuals were very low (n = 12). There were no differences between gender or age regarding the PROMIS value. As expected, the ones that reported poor health status had higher PROMIS value than the respondents with very good or good self-reported health status. Car occupants and pedestrians had to some extent higher PROMIS value. Injuries to the nerves and post-traumatic stress disorders did more often lead to health loss compared with fractures, Table A2. Furthermore, road users with injuries classified as MAIS 3 or higher were more affected than road users with injuries classified MAIS 1 or 2.
Road users with injures to the spine were having the highest pain intensity with the highest pain intensity among road users with cervical spine injuries (mean value of 5.4 on the numeric rating scale of 0 to 10), followed by thoracic spine and lumber spine (mean value of 5.2 respectively 5.0). Road users with cervical spine injuries had significantly higher proportion of pain intensity above 5. The lowest pain intensity was found among road users with injuries to the upper extremities (mean value 4.1). A dislocation was in general causing more problem than a fracture to the extremities. There was no difference between gender but the proportion of road users with pain above 5 was significantly higher in the age group 35-44 compared with all other age groups. Furthermore, road users under 25 years of age had significantly lower pain intensity.
Discussion
This is the first study showing self-reported health status among road users with injuries resulting in PMI. The findings of this retrospective study with follow-up by self-administered questionnaire show that PMI was associated with large average decrements in health on several measures. In total 85% were still suffering from the injuries several years after the crash (in average 13 years). In line with previous studies it is clear that some injuries affect the quality of life to higher extent than others. Furthermore, the higher the PMI the lower self-reported health status was found to be. Other perspective of health loss after a crash such as sickness absence/disability pension have been found to correlate with PMI. Individuals with a higher PMI had a higher proportion of disability pension (Elrud et al. Citation2019), showing that injuries often effected a wider spectrum of health.
Long-term effects of road traffic injuries in terms of temporary and permanent impairment are less known than the impact on health in terms of deaths and initial consequences. Studying the long-term consequences of non-fatal injuries is difficult because few have the possibility to follow an initial injury over time. For instance, police and hospital data often used in the traffic safety field only reflect the direct and short-term health consequences of an injury. However, insurance data can here be used to follow the injured road user over time and therefore establish the proportion of injuries leading to a PMI as an outcome of the injury. Another strength of using insurance data is that all injury severity levels are included. Several studies have been using the risk of PMI presented in Malm et al. (Citation2008) to analyzed injury outcomes and to predict long-term consequences (see for example (Rizzi et al. Citation2013, Tingvall et al. Citation2013) ). By using PMI instead of severe injuries reported by the police or categories of injuries classified as AIS 3 or higher other spectrums could be found (Tingvall et al. Citation2013) . Some injuries with high AIS scores (AIS 3+) have low risk for long-term consequences; for example, lung contusions (Haxhija et al. Citation2004). In contrast, some injuries with low AIS levels (AIS 1–2) often lead to long-term consequences; for example, AIS 1 cervical spine injuries (Malm et al. Citation2008). Several studies have shown that not only the more severe injuries have a negative effect on the health of the affected (Rissanen et al. Citation2017). However, the instrument PROMIS used in the present study indicated that the health was more affected among road users with a PMI form a MAIS3+ injury. The high proportions of individuals still suffering from an injury resulting in PMI indicating that the risk of PMI could be used as a measurement to capture long-term consequences from several health-related aspects.
Previous studies have shown that both the physical and the psychological health will be affected for those involved in traffic crashes (Rissanen et al. Citation2017). Also that bicyclists reported better health status than car occupants has been shown (Ohlin et al. Citation2017). One reason for this might be that they were found to be more physical active after the crash than car occupants in the present study. Lack of physical activity is a well-known risk factor and is estimated to high health care cost. A previous study has shown that individuals with injuries compared to non-injured had significantly poorer self-assessed general health and higher self-reported depression up to ten years after the injury (Toft et al. Citation2010). Just as in the present study, they found that individuals with back, head and neck injuries reported poor general health and they did not find any differences in gender regarding self-assessed health. Furthermore, individuals with a fracture, one of the most common injury types in both these studies, seemed to have a lower impact on the self-reported health than other injury types. In the present study only road users with documented long-term consequences in terms of PMI were included. It is therefore more likely that the ones included in the present study would have an affected health. However, PMI have to our knowledge never been validated regarding self-reported health status before. This study clearly shows that an injury leading to PMI will affect the individual future health. Self-reported outcome measures are important to validate measures like PMI to see if it captures the full spectrum of long-term consequences.
A trend was found that young respondents were suffering to a higher extent and that their physical activity was more affected than older respondents. Young individuals will most likely live longer with the remaining symptoms of the injury and thereby the burden of the injury in terms of both economical and health aspect will be greater. Therefore, there is a need to prevent injuries among this age group since road traffic injuries are the leading cause of death and one of the main causes for children and young adults aged 5-29 years to be treated at hospital. When using a measurement like PMI it might be relevant to also highlight the age. Other measurements like Disability-Adjusted LifeYears (DALY) include the injured individual’s age to better capture the effect of lifelong duration (see for example (Nilsson et al. Citation2017)).
The questionnaire was sent out to injured individuals selected from a large insurance company in Sweden with a market share of approximately 20 percent of 4.4 million vehicles used in traffic and almost insure every second person in Sweden. The result might not be applicable for low- or middle-income countries. The low response rate should be considered when assessing the validity of the results. The fact that the injury distribution was similar among those that respond and those that did not respond although indicate that it did not influence the results. However, only a few respondents were injured as pedestrians (n = 20) and thereby it is uncertain how an injured pedestrian’s health will be affected after the accident. Regarding diagnoses such as post-traumatic stress disorder too few (n = 12) were included to draw any conclusions but these needs to further be study since the result indicated that post-traumatic stress disorder was associated with higher health loss. As in previous studies the response rate was lower among young individuals (Monarrez-Espino et al. Citation2018) which might have affected the result among this age group. Little is known about how patterns of non-response effects on estimates of self-reported health status and should be further studied.
The consequences of non-fatal injuries will be even more relevant in the future and should been brought into focus for policy making and interventions. The Vision Zero defines serious injury as one resulting in unacceptable health loss, in Sweden defined as risk of PMI ≥1%. The present study clearly shows that individuals with injuries resulting in PMI will still suffer several years after the crash. Therefore, the deteriorated self-reported health, quality of life as well as the severe reduction of physical activity following a crash need to be addressed to create a sustainable road transport system.
In conclusion, the Swedish definition of serious injury, an injury leading to permanent medical impairment, was found to correlate with self-reported health loss; 85% of the injured road users reported that they still had remaining symptoms several years after the accident occurred. The quality of life and the physical activity among road users sustaining PMI was lower after the crash compared to prior. How the health is affected will differ between different type of road users. Bicyclists reported better health status and were more physically active than car occupants although the mean age was higher among bicyclists. The higher the degree of PMI the higher health loss. The injured body region leading to permanent medical impairment after an accident can vary from the body regions reported to cause long-term health loss. Sustaining a PMI regardless severity and injured body region has the same effects on general health and quality of life for men and women.
The present study shows that the serious injured road users were still suffering up to 18 years after the accident and several dimensions of health were affected many years after a road traffic accident. Even if a high proportion of the injuries were initial classified as minor injuries. Therefore, the consequences of non-fatal injuries of all severity should be brought into focus to further prevent these.
Supplemental Material
Download ()Additional information
Funding
References
- Bergman S , Herrstrom P , Jacobsson LT , Petersson IF. 2002. Chronic widespread pain: a three year followup of pain distribution and risk factors. J Rheumatol. 29(4):818–825.
- Chaplin J , Nilsson E , Ström E , Holmström L , Wicksell R. 2018. The Swedish Linguistic Team-based PROMIS® Item Quality Review Process. Paper presented at: the 4th Annual PROMIS® Health Organization Conference: Global Advances in Methodology and Clinical Science 28-29 October; Dublin, Ireland.
- Craig BM , Reeve BB , Brown PM , Cella D , Hays RD , Lipscomb J , Simon Pickard A , Revicki DA. 2014. US valuation of health outcomes measured using the PROMIS-29. Value Health. 17(8):846–853. doi:10.1016/j.jval.2014.09.005
- Elrud R , Friberg E , Alexanderson K , Stigson H. 2019. Sickness absence, disability pension and permanent medical impairment among 64 000 injured car occupants of working ages: A two-year prospective cohort study. Accid Anal Prev. 127:35–41. doi:10.1016/j.aap.2019.02.019
- Elrud R , Stigson H , Ohlin M , Alexanderson K , Friberg E. 2017. Sickness Absence among Passenger Car Occupants following a Crash. Paper presented at: Int. IRCOBI Conf. on the Biomechanics of Injury; 13-15 September, Antwerpen, Belgium.
- Grimby G , Borjesson M , Jonsdottir IH , Schnohr P , Thelle DS , Saltin B. 2015. The "Saltin-Grimby Physical Activity Level Scale" and its application to health research. Scand J Med Sci Sports. 25:119–125. doi:10.1111/sms.12611
- Gustafsson M , Stigson H , Krafft M , Kullgren A. 2015. Risk of Permanent Medical Impairment (RPMI) in Car Crashes Correlated to Age and Gender. Traffic Inj Prev. 16(4):353–361. doi:10.1080/15389588.2014.940459
- Haxhija EQ , Nores H , Schober P , Hollwarth ME. 2004. Lung contusion-lacerations after blunt thoracic trauma in children. Pediatr Surg Int. 20(6):412–414.
- Hurst NP , Ruta DA , Kind P. 1998. Comparison of the MOS short form-12 (SF12) health status questionnaire with the SF36 in patients with rheumatoid arthritis. Br J Rheumatol. 37(8):862–869. doi:10.1093/rheumatology/37.8.862
- Malm S , Krafft M , Kullgren A , Ydenius A , Tingvall C. 2008. Risk of permanent medical impairment (RPMI) in road traffic accidents. Annu Proc Assoc Adv Automot Med 52:93–100.
- Mayou R , Bryant B. 2003. Consequences of road traffic accidents for different types of road user. Injury. 34(3):197–202. doi:10.1016/S0020-1383(02)00285-1
- Monarrez-Espino J , Laflamme L , Berg HY. 2018. Measuring and assessing risk of quality of life loss following a road traffic injury: A proposed methodology for use of a composite score. Accid Anal Prev. 115:151–159. doi:10.1016/j.aap.2018.02.009
- Nilsson P , Stigson H , Ohlin M , Strandroth J. 2017. Modelling the effect on injuries and fatalities when changing mode of transport from car to bicycle. Accid Anal Prev. 100:30–36. doi:10.1016/j.aap.2016.12.020
- Ohlin M , Berg HY , Lie A , Algurén B. 2017. Long-term problems influencing health-related quality of life after road traffic injury – Differences between bicyclists and car occupants. J Transport Health. 4:180–190. doi:10.1016/j.jth.2016.08.007
- Rissanen R , Berg H-Y , Hasselberg M. 2017. Quality of life following road traffic injury: A systematic literature review. Accid Anal Prev. 108:308–320. doi:10.1016/j.aap.2017.09.013
- Rizzi M , Stigson H , Krafft M. 2013. Cyclist injuries leading to permanent medical impairment in Sweden and the effect of bicycle helmets. Paper presented at: IRCOBI Conference2013; Gothenburg, Sweden.
- Stigson H , Gustafsson M , Sunnevang C , Krafft M , Kullgren A. 2015. Differences in long-term medical consequences depending on impact direction involving passenger cars. Traffic Inj Prev. 16 Suppl 1:S133–S139. doi:10.1080/15389588.2015.1014999
- Strandroth J. 2015. Validation of a method to evaluate future impact of road safety interventions, a comparison between fatal passenger car crashes in Sweden 2000 and 2010. Accid Anal Prev. 76:133–140. doi:10.1016/j.aap.2015.01.001
- Tingvall C , Ifver J , Krafft M , Kullgren A , Lie A , Rizzi M , Sternlund S , Stigson H , Strandroth J. 2013. The Consequences of Adopting a MAIS 3 Injury Target for Road Safety in the EU, a Comparison with Targets Based on Fatalities and Long-term Consequences. Paper presented at: Int. IRCOBI Conf. on the Biomechanics of Injury Gothenburg, Sweden.
- Toft AM , Moller H , Laursen B. 2010. The years after an injury: long-term consequences of injury on self-rated health. J Trauma. 69(1):26–30. doi:10.1097/TA.0b013e3181d3cbf2