Abstract
Objectives
In Denmark, the use of bicycles is widespread, and head injuries are often seen in cyclists involved in collisions. Despite the well-known effects of using a helmet to reduce head injuries, using helmets is not mandatory in Denmark. The primary objective of this study was to provide data regarding injury outcomes and helmet usage.
Methods
Participants were bicyclists who sustained head injuries in bicycle collisions and were assessed by the Copenhagen Emergency Medical Services between 1 January 2016; and 15 June 2019. Patients with suspected head injury were identified in an electronic prehospital patient record. Data were linked to the Danish National Patient Registry to retrieve the diagnosis and were categorized into head injury or no head injury based on the diagnosis. Adjusted logistic regression analyses were reported with odds ratios and corresponding confidence intervals to assess the risk of head injury while adjusting for risk factors like age, sex, alcohol consumption, occurrence during weekends and traumatic brain injury.
Results
A total of 407 patients were included in this study. Within this entity, 247 (61%) had sustained a head injury. The use of a helmet was reported in one-third of the included patients. Among the head-injured patients, 13% sustained moderate to severe head injuries. Patients with suspected alcohol involvement were significantly less likely to report the use of a helmet. Helmet use reduced the risk of head injury with an odds ratio of 0.52, (95% CI 0.31 − 0.86). In high-energy trauma, the use of a helmet showed a significant reduction in the risk of sustaining a head injury with an odds ratio of 0.28, (95% CI 0.12 − 0.80).
Conclusions
In this study, using a helmet was associated with a significantly decreased risk of head injury; this association was even more significant in high-energy trauma.
Background
Bicycling is a popular means of recreation and transportation globally. Denmark is a small and densely populated nation with a tradition for the use of bicycles. From 2016 to 2019; bicycling accounted for 14–16% of all commutes in Denmark (Christiansen Citation2019). Bicycling is most prevalent in large cities, and the estimated cycled distance per person per day is 50% higher in Copenhagen, the capital of Denmark, than in other large cities (Vejdirektoratet Citation2018a).
In 2018; deaths from bicycle collisions represented 27% of all deaths from traffic collisions in Denmark. The number of bicycle deaths and injuries in 2018 was the highest in 10 years (Vejdirektoratet Citation2018b). Head injuries are common among injured bicyclists, and traumatic brain injury (TBI) is a significant risk factor for mortality in bicycle collisions (de Guerre et al. Citation2020).
Several international studies have demonstrated the protective effect of using a helmet to reduce the incidence of head injury, including TBI and mortality in cyclists. However, the use of helmets in Denmark is not mandated by law, and information from studies on the Danish population is minimal (Høye Citation2018; Olivier and Creighton Citation2017).
When a person is in an accident on a bike and cannot get from the place of the accident by his means, then an ambulance is dispatched. In 2015, the Emergency Medical Service (EMS) in the Capital Region of Denmark introduced an electronic prehospital medical record, allowing for data collection from all bicycle collisions where an ambulance is dispatched, thus including more casualties than the police registry. Further, the prehospital medical records comprise data from patients closer to the actual collision than in-hospital medical records; this is especially relevant when obtaining information on difficult-to-assess features, such as altered state and loss of consciousness.
The majority of evidence within the field of traffic collisions involving cyclists is based on in-hospital data from admitted patients (Baschera et al. Citation2021; de Guerre et al. Citation2020; Reitano et al. Citation2022). It has been argued that this selection may underestimate the true incidence of casualties (Olivier and Creighton Citation2017). Based on data from the prehospital medical record, this study aimed to investigate the proportion of head injuries effect of wearing a helmet on the incidence of head injuries among cyclists in the Danish population.
Methods
Design
This observational cohort study included all cyclists who were involved in a traffic collision and were assessed by the Emergency Medical Services (EMS) of Copenhagen, the Capital Region of Denmark, between January 1, 2016; and June 15, 2019.
Setting
The Capital Region is the largest of the five healthcare regions in Denmark, with a population of 1.8 million in 2019; predominantly living in urban areas. The Danish healthcare system, including services provided by the EMS, is free of charge for all citizens. Citizens can call the 1-1-2 emergency phone (equivalent to 911) or the 1813-medical helpline in case of non-life-threatening situations. Both branches of the Emergency Medical Dispatch Center are operated by medical dispatchers with a background in healthcare and can dispatch an ambulance. Patients are screened by the medical dispatchers using the criteria-based Danish Index for Emergency Care. This decision tool supports the dispatch response based on the level of urgency A-E/F (Andersen et al. Citation2013). An A level dispatch is an ambulance with lights and sirens and a level B dispatch is to reach the injured before 30 min. The haste in which the ambulances are dispatched, is then diminished down through the levels C, D and E/F. All Danish citizens have a personal civil registration number registered for all contacts with the public healthcare system, allowing for the identification of patients across the Danish national registries (Schmidt et al. Citation2014). The Danish National Patient Registry (DNPR) is a population-based administrative registry; diagnoses and treatments associated with each hospital contact are registered in the DNPR (Lynge et al. Citation2011; Schmidt et al. Citation2014).
Data collection
The electronic prehospital medical records were searched for phrases where the EMS personnel had referred to “bicycle” to identify the medical records of bicyclists involved in collisions between January 1, 2016; and June 15, 2019. Cases of all ages were included if an ambulance with “lights and sirens” was dispatched.
The personal civil registration number was used along with the date of the incidence to link the included medical records with a diagnosis code of head injury or facial injury from the DNPR based on the tenth edition of the International Classification on Diseases (ICD-10) (World Health Organization Citation2016). Furthermore, in this study, records were linked with the diagnosis code “observation for a suspected concussion.” This code is given to patients whom healthcare professionals examine due to a potential concussion following a head injury. These diagnosis codes were chosen to identify all patients with a history of head injury who had not necessarily sustained a head injury. Head injury was defined as having a lesion of the scalp (open or superficial), a skull fracture (either in the base of the skull or the calvaria) or TBI, including concussion, contusions, diffuse traumatic brain lesion, intracerebral hemorrhage (ICH), epidural hemorrhage, subdural hemorrhage and traumatic subarachnoidal hemorrhage (SAH). No head injury was defined as the absence of the injuries mentioned above. All data on diagnoses were retrieved from the DNPR.
The case group comprised all the patients with head injuries, hereinafter mentioned as the injury group, and the control group included all those without head injuries, hereinafter mentioned as the non-injury group. The medical records were manually reviewed by two independent raters, and bicycle collisions were defined as injuries sustained by a rider or passenger of a bicycle. Pedestrians hit by a bicycle were excluded. Data was collected and reported according to the Strengthening of reporting observational studies in epidemiology checklist (von Elm et al. Citation2007).
Patient characteristics
Information on age, sex, day of the collision, time of day, diagnoses, and mortality were collected from the DNPR.
Characteristics of the event
Information on the mechanism of collision, type of injury, use of helmet, suspected alcohol involvement, triage level, Glasgow Coma Scale (GCS) score, loss of consciousness and neurological symptoms were obtained by reviewing the prehospital medical records. Suspected alcohol involvement was assessed by the EMS personnel, yet it was not based on any quantitative measure, such as serum ethanol. Triage level was determined by the EMS personnel based on a defined algorithm considering the patients’ vital parameters (evaluation of airways, peripheral oxygen saturation, respiratory rate, heart rate, blood pressure, last given GCS score, and temperature). There were four possible triage levels, where a triage level of one is the most urgent, and four is the least urgent. The mechanism of collision was categorized where possible into two categories: a bicycle collision involving a moving vehicle and a single bicycle collision characterized by impact against a stationary vehicle or object or a fall.
Stratification
According to the Head Injury Severity Scale (HISS), patients with injuries were stratified into four groups (Stein and Spettell Citation1995). Minimal: Glasgow Coma Score greater than 15 and no loss of consciousness. Mild: Glasgow Coma Score 14 or 15 and brief loss of consciousness (<5 min). Moderate: Glasgow Coma Score 9–13 or loss of consciousness ≥5 min or focal neurological deficits. Severe: Glasgow Coma Score 3–8. High-energy trauma was defined as collisions with moving motorized vehicles. In contrast, low-energy trauma was defined as a fall or collision with stationary vehicles or objects according to the Advanced Trauma Life Support definition. (Advanced trauma life support (ATLS®) Citation2013). The HISS was obtained by the medical records where available.
Statistics
Descriptive statistics are presented as absolute numbers with percentages or medians with interquartile ranges as appropriate. Comparative analyses were carried out using non-parametric testing to analyze subgroups. Gaussian continuous data were evaluated with Student’s t-test and categorical data with Fisher’s exact test. Multivariable logistic regression analyses were adjusted for age, sex, level of energy, if the insult was at the weekend, traumatic brain injury and suspected alcohol involvement. There was no adjustment for other types of injuries to the face or limbs as this was not considered to influence the outcome. The multivariable analysis was reported with adjusted odds ratios (aOR) and a corresponding 95% confidence interval (CI). There was no imputation of missing data. Statistical significance was considered at a p-value of <0.05, and all statistical tests were performed using R version 4.1.3 (2022-03-10).
Results
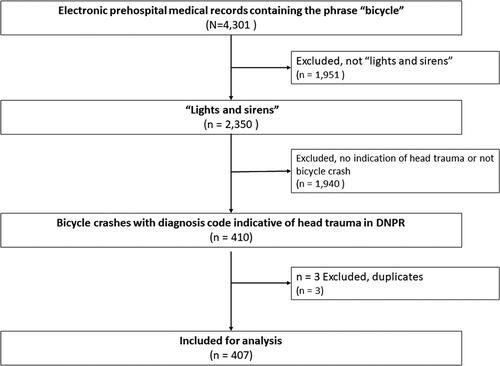
shows a revised STROBE chart of inclusion. A total of 4,301 electronic prehospital medical records containing the phrase “bicycle” were identified. Of these, 2,350 records were cross-referenced with DNPR based on fulfilling the “lights and sirens” criteria, and 410 were eligible for manual validation. The Copenhagen EMS assessed 407 patients involved in a bicycle collision severe enough to elicit an ambulance with “lights and sirens” with a diagnosis code indicative of head injury between January 1, 2016; and June 15, 2019. Of these patients, 247 (61%) had sustained a head injury and made up the injury group. The remaining 160 (39%) had facial injuries alone or had been observed for signs of a head injury after the collision and made up the non-injury group.
Figure 1. Revised STROBE chart of inclusion. STROBE: STrengthening the Reporting of OBservational studies in Epidemiology, DNPR
Patient characteristics
A comparison between patient demographics in patients with and without head injury is shown in . The median age was 41 years in both groups, and no significant difference was found between age groups within the injury group and the non-injury group. More males were in the injury than in the non-injury groups (63 vs. 52%, p = 0.03). In both the injury group and the non-injury group, more head injuries occurred during the day between 8.01 am to 5 pm (45 and 40%, p = 0.4) and the evening between 5.01 and 12 pm (37 and 42%, p = 0.3) compared to the night from 12.01 pm to 8 am (23 and 13%, p = 0.02%). No significant difference was found regarding suspected alcohol intake between the injury- and non-injury groups.
Table 1. Comparison of patients with head trauma according to status of head injury in patients assessed by the copenhagen emergency medical services.
Comparison of patients with reported helmet use
Baseline demographic characteristics between patients with reported helmet use and no reported helmet use are shown in . Patients in the non-helmet group were slightly younger, with a median age of 39 years, IQR (26–53) vs. 45 years, IQR (31–55), p = 0.049 in the helmet group. Fewer males were present in the non-helmet group (48.6%) vs. (61.1%) in the helmet group, p = 0.024. Suspected alcohol involvement was significantly more likely in the non-helmet group, 20.6 vs. 2.7% in the helmet group, p < 0.001. No significant differences were seen between the non-helmet and the helmet group concerning the triage level, with the majority triaged at the least urgent level in both groups. Regarding the mechanism of collision, no significant differences were seen between the groups.
Table 2. Reported helmet use in patients with suspected head trauma assessed by the copenhagen emergency medical services.
Reported helmet use in patients with suspected head injury is shown in . Helmet use was reported in n = 59 (52%) within the injury group vs. n = 54 (48%) within the non-injury group. Unknown helmet status was present in n = 119 (29%). The overall 30-survival rate was 99.6%. Among the deceased, one died in the non-helmet group, and one died with unknown helmet status. According to the HISS, n = 32 had severe or moderate head injury independent of helmet status. In the non-helmet group, 30% had mild head injury vs. 29% in the helmet group, p = 0.895. In the non-helmet group, 2.9% had a severe head injury vs. 0.9% within the helmet group, p = 0.409. Most patients suffered from concussions in both the non-helmet and helmet group. Only the primary diagnosis of open scalp lesion was significantly more frequent in the non-helmet group, 14% vs. 10% in the helmet group, p < 0.001. The incidence of the remaining diagnoses did not differ significantly between the two groups.
Table 3. Outcomes in patients with suspected head trauma according to the reported use of helmet.
Association of helmet use
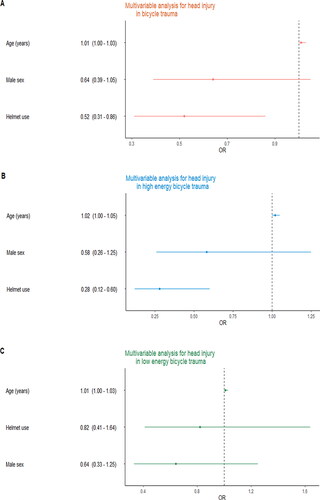
shows that helmet use was associated with a decreased risk of head injury in bicycle collisions with an aOR of 0.52 95% CI (0.31–0.96). evaluates the risk of head injury in high-energy trauma; this model indicates that helmet use was associated with a significantly decreased risk of head injury, OR 0.28, 95% CI (0.12 − 0.80). Finally, shows no significant effect of helmet use when evaluating the risk of head injury among patients who sustained a low-energy bicycle trauma, aOR 0.82 (0.41 − 1.64). Age and male sex did not contribute significantly to any of the models in .
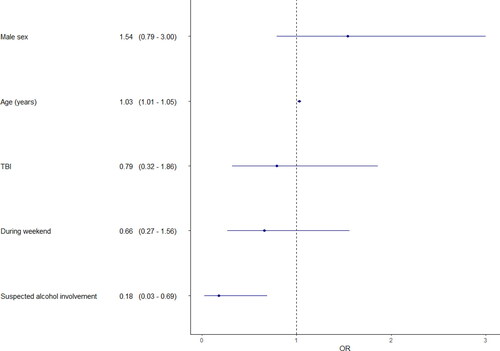
The adjusted multivariable analysis for reported helmet use in patients with a sustained head injury is shown in . A trend toward an association between the use of helmets and increasing age was found, aOR 1.05, 95% CI (1.01–1.05), however it was not statistically significant. Suspected alcohol involvement was significantly less likely in patients with reported helmet use, aOR 0.18, 95% CI (0.03–0.69). An insignificant trend toward a decreased risk of TBI was observed for patients with reported helmet use, aOR 0.79, 95% CI (0.32–1.86).
Discussion
Prior studies have evaluated the role of helmet use in head injury. Still, data from settings with high proportions of the population using bicycles and highly developed roadway infrastructure, including the priority of bicycle lanes, remain scarce. Given the increasing number of cyclists in many regions, both for leisure and transport, an evaluation of head injury in this subgroup of injury is paramount. This study on bicycle-related head injuries provides novel information on the characteristics of cyclists with head injuries following traffic collisions in Copenhagen, Denmark.
Previous meta-analyses have described the positive effects of helmets and have found helmets to reduce the risk of head injuries by 50% (Høye Citation2018; Olivier and Radun Citation2017). Further, severe head injury was decreased by 60% and TBI by 53% (Høye Citation2018). Høye reported a 20% reduction in head injuries by mandating helmets (Hoye Citation2018). Findings from this study indicate that the prevalence of wearing a helmet for cyclists remains relatively low in Copenhagen, Denmark. Results on helmet use from previous trials from the Netherlands, Norway, Italy, and the US are conflicting, with reported rates between 7.5 and 91% (de Guerre et al. Citation2020; Næss et al. Citation2020; Reitano et al. Citation2022; Sethi et al. Citation2015). These differences might be explained by different bicycle cultures and helmet legislation across regions. Reitano et al. evaluated prognostic factors for survival in patients sustaining bicycle collisions and showed that among the 446 included patients, only 9% did not wear a helmet, even though it is not mandated by law. The authors found no independent association between helmet use and increased survival. Yet, they proved a significant reduction in the incidence of head injuries related to using helmets (Reitano et al. Citation2022). This present study showed a 48% reduction in the risk of head injury when wearing a helmet, in line with previous findings (Høye Citation2018; Olivier and Creighton Citation2017). When adjusting for the level of energy, using a helmet was associated with a significantly reduced risk of head injury in high-energy trauma. Evidence regarding the protective effect of helmets when evaluating the mechanism of collision is limited with different used nomenclature and unequivocal results (Høye Citation2018). In this study, 55% of the included patients with a head injury sustained a single bicycle collision, defined as a fall or a collision with a stationary vehicle or object. Olivier et al. reported no difference when introducing the proportion of bicycle collisions in motor vehicle collisions in a meta-regression analysis, thus concluding that there was no change in the protective effect of the use of helmets between different mechanisms of collision (Olivier and Creighton Citation2017). Another meta-analysis by Høye found a likely larger protective effect in single bicycle crashes vs. motor vehicle collisions. However, the analysis for motor vehicle collisions in head injury failed to reach the level of significance (Høye Citation2018).
According to the HISS, most patients in this study sustained a mild and minimal head injury, yet two in five included patients presented with TBI. Further, the definition of the severity of head injury is not well-defined within the available studies; some studies have reported the severity of head injury according to Glagow Coma Score, and others have reported abbreviated injury scores. These inconsistencies challenge the reproducibility and comparability of results within the existing evidence. Open scalp lesions and skull fractures were significantly less common in patients with reported use of helmets in line with previous findings (Baschera et al. Citation2021). Among patients with TBI, the most common type of injury was concussion, then followed by traumatic SAH and traumatic ICH; this does not corresponds to the findings within the existing literature where concussion is not included as a part of TBI (Baschera et al. Citation2021; de Guerre et al. Citation2020; Dodds et al. Citation2019).
It has been reported that helmet use is associated with safer riding practices which add to the protective effect of helmet use (Webman et al. Citation2013). This study showed that suspected alcohol intake was significantly more frequent among patients with no helmet. Even though alcohol consumption has been proven to increase the risk of injury, it has not been shown to confound the positive effect of using a helmet (Crocker et al. Citation2012).
The role of sex and the use of helmets has been debated (Feler et al. Citation2021; Vyas et al. Citation2021). Explanations for these sex-based differences have ranged from anatomical toward on-road behavioral differences (Feler et al. Citation2021). Males were overrepresented within the helmet group and were less likely to sustain a head injury in this study, but no significant associations were found in the multivariable analysis. These findings advocate for the role of sex as a possible confounder and stress the need for further evaluation to target campaigns.
Data from this study did not find any significant difference regarding survival; established evidence has reported a reduction in fatal head injury of 65–71% in patients using a helmet (Høye Citation2018; Olivier and Creighton Citation2017). Only two fatal cases were present in this study, and it was not possible to draw any conclusions on survival.
The adjusted analyses demonstrated a positive effect of helmet use in all bicycle collisions as well as in high-energy bicycle trauma. Unadjusted analyses, however, showed no statistically significant differences between those wearing a helmet and those not regarding injury severity and primary diagnosis. This difference may be explained by confounding, both regarding age and sex, and, as the adjusted analysis of low-energy trauma reveals, the amount of energy involved.
Strengths and limitations
One strength of this study is how patients were included in the control group. To allow for a better comparison between cases and controls, the control group consisted of patients observed for a concussion or diagnosed with facial injury likely to have sustained head injury in the collision. Using this approach, this study evaluated whether helmets were effective in situations where they were intended to protect against injuries in the first place. Most of the available evidence includes patients admitted to the hospital, which might lead to a bias toward the true incidence with an underlying risk of underestimation. Further, it has been argued that this selection underestimates the number of patients using helmets, thereby questioning the validity of such evaluations (Olivier and Creighton Citation2017).
The applied approach does also present a limitation to this study. The small sample size is an important limitation, especially when considering subgroups. It is beyond the scope of this study to evaluate whether the estimated protective effect of helmets in collisions with motor vehicles is either larger or smaller than the protective effect in single bicycle collisions. When analyzing the effectiveness of different types of collisions, the sample sizes of the subgroups were too small to introduce them into a logistic regression analysis. Further, several confounders were present in this study, including sex, observation of occurrence, comorbidity, and socioeconomic status. Where age might as well constitute a mediator, future studies should include adjusted analyses to overcome the role of confounding bias. Selection bias should also be addressed. Since this study was based on patients assessed by the Danish EMS, patients involved in bicycle collisions with minor injuries whom the Danish EMS did not assess were likely underrepresented.
While bicycling is common in Denmark, this might not apply to other regions and countries. This consideration is relevant regarding helmets, bicycle infrastructure and legislation, yet the Danish setting is comparable to other countries in Northern Europe. Another applicable limitation is that suspected alcohol involvement was based on a subjective assessment, not ethanol concentration measurements from blood samples or the expiratory breath.
The DNPR is a valuable source of information and is generally approved of, yet misclassification bias should be considered. Nonetheless, there is no reason to believe that any potential misdiagnosis of head injuries should be especially pronounced in either of the subgroups.
Conclusion
Bicyclists are involved in different collisions, including falling and colliding with stationary objects or moving vehicles. Severe and moderate head injuries were rare. Several factors determine the risk of head injury in these collisions. This study indicates that bicyclists with head injury can considerably reduce the risk of head injury by wearing a helmet; this effect was significantly increased in the case of high-energy trauma.
Ethical approval
According to Danish law, registry-based studies do not require ethical approval or patient consent. The Danish legislation was followed according to the general data protection agency.
Author contributions
EMB: Contributed to literature search, data curation, figures, methodology, data interpretation, formal analyses, software, data interpretation, figures, project administration (lead), validation, writing the original draft and editing final paper (lead). Have accessed and verified underlying data. SAW: Contributed to data curation, data collection, methodology, software, figures, and validation; reviewed and edited the original draft and final paper. Have accessed and verified underlying data. NB: Contributed to data collection and reviewed and edited the original draft and final paper. Have accessed and verified underlying data. SNB: Contributed to data curation, data collection and methodology. Have accessed and verified underlying data. FL: Contributed to editing and reviewing the final paper. VE: Contributed to methodology and data interpretation and edited and reviewed the final paper. HCC: Contributed with conceptualization (lead), data curation, validation, methodology, data interpretation, project administration, supervision, editing and reviewed the original draft and final paper. Have accessed and verified underlying data. All authors have read and approved the final version of the manuscript.
| Abbreviations | ||
| HISS | = | Head injury severity scale |
| GCS | = | Glasgow coma scale |
| EMS | = | Emergency medical service |
| TBI | = | Traumatic brain injury |
| SAH | = | Subarachnoidal hemorrhage |
| ICH | = | Intracranial hemorrhage |
| EDH | = | Epidural hemorrhage |
| SDH | = | Subdural hemorrhage |
| DNPR | = | The Danish national patient registry |
| CPR | = | Personal civil identification number |
| aOR | = | Adjusted odds ratio |
| CI | = | Confidence interval |
| IQR | = | Interquartile range |
| ICD-10 | = | International classification of disease, tenth edition. |
Acknowledgements
The authors thank the Copenhagen Emergency Medical Service, especially the EMS personnel, for consistently and thoroughly registering when treating patients in bicycle collisions.
Disclosure statement
No conflict of interest was reported by the author(s).
Data availability statement
The data supporting this study’s findings are available from the Danish Patient Safety Authority. Still, restrictions apply to the availability of these data, which were used under license for the current research and are not publicly available. Data are, however, available from the authors upon reasonable request and with permission of the Danish Patient Safety Authority.
Additional information
Funding
References
- Advanced Trauma Life Support (ATLS®). 2013. Advanced trauma life support (ATLS®). J Trauma Acute Care Surg. 74(5):1363–1366. doi:10.1097/TA.0b013e31828b82f5.
- Andersen MS, Johnsen SP, Sørensen JN, Jepsen SB, Hansen JB, Christensen EF. 2013. Implementing a nationwide criteria-based emergency medical dispatch system: a register-based follow-up study. Scand J Trauma Resusc Emerg Med. 21(1):53. https://sjtrem.biomedcentral.com/articles/10.1186/1757-7241-21-53. doi:10.1186/1757-7241-21-53.
- Baschera D, Lawless A, Roeters R, Frysch CWS, Zellweger R. 2021. Severity and predictors of head injury due to bicycle accidents in Western Australia. Acta Neurochir. 163(1):49–56. doi:10.1007/s00701-020-04626-w.
- Christiansen B. 2019. The Danish National Travel Survey - Annual Statistical Report 2019 [accessed 2023 June 10]. https://backend.orbit.dtu.dk/ws/portalfiles/portal/284291337/TU_Denmark_2019_n_TU0621v1.pdf.
- Crocker P, King B, Cooper H, Milling TJ. 2012. Self-reported alcohol use is an independent risk factor for head and brain injury among cyclists but does not confound helmets’ protective effect. J Emerg Med. 43(2):244–250. doi:10.1016/j.jemermed.2011.05.029.
- de Guerre LEVM, Sadiqi S, Leenen LPH, Oner CF, van Gaalen SM. 2020. Injuries related to bicycle accidents: an epidemiological study in The Netherlands. Eur J Trauma Emerg Surg. 46(2):413–418. doi:10.1007/s00068-018-1033-5.
- Dodds N, Johnson R, Walton B, Bouamra O, Yates D, Lecky FE, Thompson J. 2019. Evaluating the impact of cycle helmet use on severe traumatic brain injury and death in a national cohort of over 11000 pedal cyclists: a retrospective study from the NHS England Trauma Audit and Research Network dataset. BMJ Open. 9(9):e027845. doi:10.1136/bmjopen-2018-027845.
- Feler J, Maung AA, O'Connor R, Davis KA, Gerrard J. 2021. Sex-based differences in helmet performance in bicycle trauma. J Epidemiol Community Health. 75(10):994–1000. doi:10.1136/jech-2020-215544.
- Høye A. 2018. Bicycle helmets – To wear or not to wear? A meta-analyses of the effects of bicycle helmets on injuries. Accident Anal Prevent. 117:85–97. doi:10.1016/j.aap.2018.03.026.
- Hoye A. 2018. Recommend or mandate? A systematic review and meta-analysis of the effects of mandatory bicycle helmet legislation. Accid Anal Prev. 120:239–249.
- Lynge E, Sandegaard JL, Rebolj M. 2011. The Danish National Patient Register. Scand J Public Health. 39(7 Suppl):30–33. doi:10.1177/1403494811401482.
- Næss I, Galteland P, Skaga NO, Eken T, Helseth E, Ramm-Pettersen J. 2020. The number of patients hospitalized with bicycle injuries is increasing – a cry for better road safety. Accid Anal Prev. 148:105836. doi:10.1016/j.aap.2020.105836.
- Olivier J, Creighton P. 2017. Bicycle injuries and helmet use: a systematic review and meta-analysis. Int J Epidemiol. 46(1):372. doi:10.1093/ije/dyw360.
- Olivier J, Radun I. 2017. Bicycle helmet effectiveness is not overstated. Traffic Inj Prev. 18(7):755–760. doi:10.1080/15389588.2017.1298748.
- Reitano E, Cioffi SPB, Virdis F, Altomare M, Spota A, Chiara O, Cimbanassi S. 2022. Predictors of mortality in bicycle-related trauma: an eight-year experience in a level one trauma center. J Pers Med. 12(11):1936.
- Schmidt M, Pedersen L, Sørensen HT. 2014. The Danish civil registration system as a tool in epidemiology. Eur J Epidemiol. 29(8):541–549. http://link.springer.com. doi:10.1007/s10654-014-9930-3.
- Sethi M, Heidenberg J, Wall SP, Ayoung-Chee P, Slaughter D, Levine DA, Jacko S, Wilson C, Marshall G, Pachter HL, et al. 2015. Bicycle helmets are highly protective against traumatic brain injury within a dense urban setting. Injury. 46(12):2483–2490. doi:10.1016/j.injury.2015.07.030.
- Stein SC, Spettell C. 1995. The Head Injury Severity Scale (HISS): a practical classification of closed-head injury. Brain Inj. 9(5):437–444.
- Vejdirektoratet. 2018a. Bicycles on the roads [Cykler på vejene] [accessed 2021a May 19]. https://vejdirektoratet.dk/tema/cykler-paa-vejene.
- Vejdirektoratet. 2018b. Traffic accidents in 2018 [Trafikulykker for året 2018]. [Accessed 2021b May 19]. https://www.vejdirektoratet.dk/api/drupal/sites/default/files/2019-10/Trafikulykker. for året 2018 – web_wcag.
- von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, STROBE Initiative. 2007. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Ann Intern Med. 147(8):573–577. doi:10.7326/0003-4819-147-8-200710160-00010.
- Vyas A, Grigorian A, Kuza CM, Dolich M, Joe V, Chin T, Nahmias J. 2021. Adult bicycle collisions: impact of helmet use on head and cervical spine injury. J Surg Res. 258:307–313. doi:10.1016/j.jss.2020.08.042.
- Webman R, Dultz LA, Simon RJ, Todd SR, Slaughter D, Jacko S, Bholat O, Wall S, Wilson C, Levine DA, et al. 2013. Helmet use is associated with safer bicycling behaviors and reduced hospital resource use following injury. J Trauma Acute Care Surg. 75(5):877–881. doi:10.1097/TA.0b013e3182a85f97.
- World Health Organization. 2016. International statistical classification of diseases and related health problems 10th revision. Available at: https://icd.who.int/browse10/2016/en.