ABSTRACT
Background
Athletes display a high prevalence of undesired sleep characteristics that may affect both performance and wellbeing.
Objectives
This scoping review aimed to identify and map the existing evidence of behavioral sleep interventions and their effects on sleep outcomes in athletes, and retrospectively code the behavior change techniques (BCTs) implemented using the Behavior Change Technique Taxonomy (BCTTv1).
Methods
Conducted following the JBI methodology for scoping reviews, four online databases were used to identify prospective interventions with at least one behavioral component in competitive athletes, and reporting a sleep outcome pre- and post-intervention.
Results
Thirty-three studies met the inclusion criteria, encompassing 892 participants with a median age of 23. Five intervention categories were identified (education, mind-body practices, direct, multi-component, and other), with each demonstrating mixed efficacy but the potential to improve sleep outcomes. The BCTs varied in type and frequency between each category, with only 18 unique BCTs identified across all studies.
Conclusions
The varied efficacy of previous studies at improving sleep outcomes may be attributed to the lack of behavior change theory applied during intervention development. Designing interventions following a targeted specification of the behavioral problem, and the integration of corresponding BCTs should be considered in future research.
Introduction
Sleep has garnered significant interest within athlete populations due to the high prevalence of undesired sleep characteristics, such as nocturnal sleep durations under seven hours and sleep efficiencies below 85% (Gupta et al., Citation2017; Lastella et al., Citation2015). These findings can be attributed to sport-specific sleep risk factors, including those relating to training, travel, and competition, in addition to non-sporting factors (Gupta et al., Citation2017). The impact of poor sleep on sport performance outcomes is equivocal and dependent on the type of task; for example, while gross physical and motor performance appears to be relatively robust to acute sleep loss, cognitively demanding sporting tasks might experience impairment (Kirschen et al., Citation2020). Furthermore, the downstream effects of poor sleep over extended periods could result in undesired outcomes such as poorer physiological recovery and increased injury risk, which may have implications for sport performance (Milewski et al., Citation2014). Therefore, a need exists to develop targeted sleep health interventions for athletes to improve sleep and mitigate against any negative performance outcomes such as closed-skill accuracy and reaction time (Jarraya et al., Citation2014; Mah et al., Citation2011).
While sleep regulation is primarily grounded in biological processes, there is a complex interaction with the social-environmental context that influences observed sleep practices (Grandner, Citation2017). Little evidence exists to indicate a higher prevalence of sleep disorders in athletes compared to the general population (Tuomilehto et al., Citation2017). Therefore, much athlete research has viewed sleep through a behavioral lens. This has included interventions designed to catalyze a personal transformation in sleep practices by implementing changes at the individual (e.g., personal beliefs), social (e.g., the workplace), and societal levels (e.g., public policy), rather than direct manipulation of biological sleep control such as light therapies or pharmacological sleep aids (Grandner, Citation2017; Halson, Citation2019). Behavioral sleep interventions across the wider population have adopted diverse approaches to improve sleep outcomes, but have demonstrated mixed effectiveness (Baron et al., Citation2021). Past systematic reviews evaluating sleep interventions in athletes have incorporated both behavioral and non-behavioral interventions within their scope, and provide preliminary evidence to support the use of both intervention types on outcomes including sport performance, mood, and recovery (Bonnar et al., Citation2018; Gwyther et al., Citation2022; Silva et al., Citation2021). However, the extent of changes in sleep outcomes in behavioral interventions, and the behavioral components driving the observed sleep changes remain unclear.
The complexity of behavioral interventions and the diverse terminology used when reporting intervention content have posed challenges in separating and pinpointing the specific behavioral components that drive behavioral change. In response, there has been a push to categorize intervention content into standardized components termed behavior change techniques (BCTs; Abraham & Michie, Citation2008). A BCT is considered to be the “active ingredient” of an intervention, constituting an observable, replicable, and irreducible element that aims to modify or redirect the causal processes governing behavior (Michie & Johnston, Citation2013; Michie et al., Citation2011). Drawing upon previous behavior change taxonomies, the Behavior Change Technique Taxonomy (BCTTv1) was developed following Delphi-type exercises by field experts as a comprehensive, hierarchically-structured classification system(Michie et al., Citation2013). The BCTTv1 consists of 93 non-overlapping and clearly defined BCTs, further grouped into 16 clusters. For example, within the grouping “1. Goals and planning” sits the BCT “1.1 Goal setting (behavior)”, which is defined as “set or agree on a goal defined in terms of the behavior to be achieved”.
While the adoption of the BCTTv1 is now increasingly common, the majority of studies incorporating behavior change within interventions do not utilize the BCTTv1 or other standardized nomenclature when describing behavioral intervention content. Nevertheless, the BCTTv1 allows retrospective coding of previously published research, facilitating meaningful comparisons between intervention components (Michie et al., Citation2013). The absence of integrated behavior change theory in previous athlete sleep research has been identified as a limitation of current literature, with no research assessing the long-term efficacy of specific BCTs within interventions (Halson, Citation2019). Consequently, there exists a need to systemize previous interventions using a standardized framework such as the BCTTv1. This would allow for assessment of the specific BCTs and frequency of use, enable comparisons between studies, and ascertain the most effective BCTs at improving sleep in athletes that should be incorporated into future research.
In light of the inherent limitations of previous reviews, the objectives of this scoping review were: (1) to identify and map the existing evidence of behavioral sleep interventions and their impact on sleep outcomes in athletes, and (2) retrospectively classify the BCTs employed in the identified interventions using the BCTTv1. A scoping review was identified as the most suitable synthesis approach to address these objectives, given the relative novelty of the research area and variations in intervention design. These factors necessitate the identification of available evidence types and an examination of the research methodologies employed (Munn et al., Citation2018).
Methods
Overview
This review was conducted in accordance with the JBI methodology for scoping reviews (Peters et al., Citation2020), and followed the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Extension for Scoping Reviews(PRISMA-ScR; Tricco et al., Citation2018). The methodology outlined below was defined a priori and registered prospectively as a review protocol on the Open Science Framework on 24 March, 2023, and updated on 11 September, 2023 (DOI: 10.17605/OSF.IO/BFZWX).
Inclusion criteria
The review inclusion criteria were defined using the Population, Content, and Context framework (Peters et al., Citation2020), and are summarized in . A broad definition of sport was applied to encompass all physically demanding activities including non-traditional sports (e.g., mountaineering and dance). Inclusion based on performance level was defined using the framework outlined by McKay et al. (Citation2022), with athletes participating in a sport at Tier 2 (Trained/Developmental) or above, encompassing ∼12%–19% of the global population.
Table 1. Study inclusion criteria using the population, concept, context framework.
Due to challenges in accurately classifying performance levels from study manuscripts, studies were categorized into professional, student-athlete, or amateur groups. The exclusion of athletes aged <18 years and para-athletes was imposed due to the impact of age and certain disabilities on sleep regulation (Grade et al., Citation2023; Hagenauer et al., Citation2009). A broad definition of behavior was applied, constituting “anything a person does in response to internal or external events, that may be overt and directly measurable or covert and indirectly measurable, and are physical events that occur in the body and controlled by the brain” (Davis et al., Citation2015). Direct interventions where sleep schedules or targets are specified were included alongside indirect interventions (e.g., education), reflecting the approach used in a previous review by Baron et al. (Citation2021). Studies solely published in English were included, as the translation from other languages into English could result in the inadvertent exclusion or misinterpretation of BCTs. No restrictions were placed on the publication date of studies to ensure the identification of a wide range of evidence.
Search strategy
A systematic search strategy was employed to identify research articles, conference papers, and abstracts for inclusion. An initial limited search of MEDLINE (PubMed) was undertaken to identify relevant studies on the subject. Article text words and index terms from this preliminary search were used to develop a simple search strategy using Title/Abstract keywords: [(sleep*) AND (athlete* OR sport* OR athletic* OR player) AND (intervention OR hygiene OR education* OR behavior* OR behaviour* OR extension OR counseling OR optimization OR optimization OR workshop)] and restricted to the English language. MEDLINE (PubMed), EMBASE (Ovid), APA PsycInfo, and SCOPUS databases were searched, with the full search term for each database available in the appendix (Table S1). The initial literature search was run on March 21, 2023, and then rerun on September 6, 2023. Additionally, backward citation searching of the included studies was performed to identify any further relevant studies.
Study selection
Following the search, all identified studies were collated and imported to Rayyan online review software (Rayyan Systems Inc, Cambridge, MA, USA; Ouzzani et al., Citation2016). Duplicate studies were manually removed, and a pilot calibration exercise was performed with a random selection of 25 full-text studies screened by two reviewers in accordance with the JBI pilot framework to increase inter-reviewer consistency (Peters et al., Citation2020). The level of agreement between reviewers was almost perfect (agreement = 96.0%, Cohen’s κ = 0.83; Landis & Koch, Citation1977). Adjustments to the inclusion criteria relating to performance level classification and studies including para-athletes were made at this stage (). Both reviewers then independently evaluated the titles, abstracts, and then the full texts of each study. Agreement between reviewers was substantial (agreement = 98.3%, Cohen’s κ = 0.61; Landis & Koch, Citation1977). Disparities or disagreements were resolved through reviewer discussion.
Data extraction
Data from the included studies were extracted by the lead reviewer and verified by a second reviewer. The extracted data encompassed study aims, study format (e.g., journal article or abstract), study design, participant characteristics (country, sport, performance level, sample size, age, and gender), intervention components (e.g., any inclusion criteria, direct or indirect intervention, and any control groups), study duration, sleep outcomes, and key findings, and was documented in a data-charting form based on recommendations from the JBI scoping review methodology (Peters et al., Citation2020; Appendix Table S2). Authors of papers were contacted once to request any missing or supplementary data where required.
For the coding of behavioral intervention content, two reviewers who had completed prior online training (www.bct-taxonomy.com) independently performed the coding for the included studies. All 93 BCTs outlined in the BCTTv1 were considered for each study, with both reviewers explaining their rationale for assigning the BCT in each instance. Fourteen discrepancies (i.e., the BCT was only coded by one reviewer) were resolved through discussion; if a consensus could not be reached, the proposed BCT was not included.
Quality appraisal
Quality appraisal was conducted to support the study objective of mapping the available evidence by providing an assessment of the methodological quality and possibility of bias in each study to enable an understanding of the current strengths and limitations in this research area. Quality appraisals were conducted using the nine-question quasi-experimental, and thirteen-question randomised controlled trial JBI critical appraisal checklists corresponding to the study design employed (Tufanaru et al., Citation2020). No inclusion criteria were applied in relation to quality appraisal scores. Quality appraisal was not performed on conference abstracts. The level of agreement between the two independent reviewers was substantial (agreement = 83.5%, Cohen’s κ = 0.64; Landis & Koch, Citation1977), with discrepancies resolved through discussion. Following quality appraisal, the overall score for each study was incorporated into data synthesis alongside the data extraction form and coded BCTs.
Results
The PRISMA flowchart highlighting the study selection process is presented in . A total of 33 studies were identified, and are summarized in .
Figure 1. Search results and study selection and inclusion process (Page et al., Citation2021).
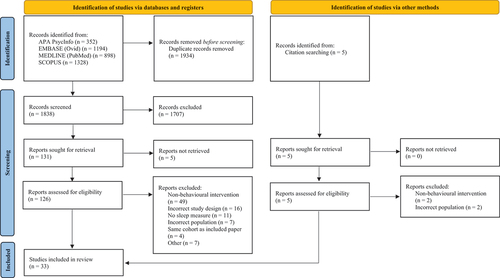
Table 2. Characteristics of included studies.
Study characteristics
The predominant study locations by region were Oceania (n = 11), Europe (n = 9), and North America (n = 9). Professional athletes were used in 17 studies, with 10 using student-athletes and six using amateur athletes (one unknown). Five studies encompassed participants from multiple sports, with rugby union (n = 5) and football (n = 3) the most prevalent sports in single-sport studies. Amongst the included studies, 19 used all-male participants, with five all-female and eight using mixed-gender samples. The collective participant count across studies was 892, with a median sample size of 21 (IQR: 15), and a median age of 23 (IQR: 4) where reported.
Study design
Studies were categorized into five groups for narrative synthesis based on similarities in extracted intervention characteristics before the coding of BCTs: education (n = 11), mind-body practices (n = 5), direct (n = 7), multi-component (n = 7), and other (n = 3). Pre-post study designs were utilized in 23 studies (single-group: n = 21, non-randomized parallel groups: n = 2), while ten studies utilized randomized designs (RCT: n = 5; randomized cross-over, n = 4; quasi-randomized trial, n = 1). Intervention durations spanned from acute one-day studies to multiple weeks. Assessment of sleep outcomes was typically performed during or immediately post-intervention, with only ten studies conducting a follow-up ≥ 7-d post-intervention. Sleep outcomes were evaluated using actigraphy (n = 21), questionnaires (n = 15), and sleep diaries (n = 7), with 11 studies utilizing two or more assessment methods.
Behavior change techniques
Across the 33 studies, a total of 18 distinct BCTs were identified, occurring in 79 separate instances. The most frequently employed BCTs were ” 4.1 Instruction on how to perform a behavior” (20), “9.1 Credible source” (12), and “1.1 Goal setting (behavior)” (9). When categorized into the 16 BCT groupings, 12 groupings were identified on at least one instance (). Four BCT groupings were not found in any study: “6. Comparison of behavior”, “14. Scheduled consequences”, “15. Self-belief”, and “16. Covert learning”. A comprehensive breakdown of the coded BCTs for each intervention and their definitions can be found in Appendix Tables S3 and S4.
Narrative synthesis
Educational
Twelve studies were categorized as educational studies and were primarily focused on the change in sleep behaviors through the dissemination of sleep-related knowledge. Except for Harada et al. (Citation2016), where educational information was conveyed through a text-based information leaflet, all other studies delivered education via one or more group sessions, ranging in duration from 30 to 150 minutes. In four studies, this was complemented by the delivery of an individual session and/or feedback (Driller et al., Citation2019; Dunican et al., Citation2021; Jenkins et al., Citation2021; Van Ryswyk et al., Citation2017). Eight educational studies demonstrated at least one favorable change in sleep outcomes, while three revealed no significant findings (Dunican et al., Citation2021; Jenkins et al., Citation2021; Kaier et al., Citation2016), and one solely demonstrated a phase delay in sleep timing (Dunican et al., Citation2023). Notable outcomes included significant improvements in actigraphy-derived total sleep time ranging between 20–36 minutes(Caia et al., Citation2018; O’Donnell & Driller, Citation2017; Sargent et al., Citation2021) and improvements in subjective measures of sleep quality (Driller et al., Citation2019; Harada et al., Citation2016; Vitale et al., Citation2019). The only unfavorable outcome observed was a lower sleep efficiency at the one-month follow-up in the study by Caia et al. (Citation2018).
Educational studies exhibited the highest frequency of BCT usage (mean: 3 ± 1), and also displayed the greatest heterogeneity in content, encompassing nine BCT groupings across the studies. The BCT “4.1 Instruction on how to perform a behavior” was present in all studies due to the nature of education delivery. Additionally, the utilization of sleep experts and healthcare professionals to deliver education sessions resulted in the inclusion of the BCT “9.1 Credible source” in eight educational studies.
Mind-body practices
Five studies were categorized as mind-body practices, where a holistic approach was taken to improve health outcomes through relaxation and mental awareness. These interventions encompass practices including yoga, progressive muscle relaxation, mindfulness, and breathing techniques. Amongst the five studies, three incorporated multiple mind-body practices within the delivered intervention, with two of them demonstrating some favorable changes in sleep outcomes (Chen et al., Citation2018; Jones et al., Citation2020) and one showing no change (Rijken et al., Citation2016). While a comparison between different mind-body practices was not feasible, a comparative study suggested that yoga may yield more favorable changes to sleep outcomes than progressive muscle relaxation (Datta et al., Citation2022).
The mean number of BCTs used in mind-body practice studies was 3 ± 2. The BCTs “12.6 Body changes” and “8.1 Repetition and Substitution” were each identified in four of the five studies, reflecting the impact of mind-body practices on body awareness and the repeated performance of the practice. Additionally, the BCT “4.1 Instruction on how to perform a behavior” was present in three mind-body practice studies.
Direct
The seven direct studies sought to increase sleep duration above baseline values by establishing a goal to increase sleep by a specific amount or toward a predefined target. This typically occurred as part of an intervention where the change in sleep duration served as an independent variable to assess the effect on a non-sleep dependent variable (e.g., sport performance). In all studies, either actigraphy-derived total sleep time or self-reported sleep duration was increased. However, in each study, the increase fell short of the predetermined goal. An unintended outcome of increased sleep duration can be a corresponding reduction in sleep efficiency, as was observed by Roberts et al. (Citation2019). Only one study augmented a direct intervention with a non-direct behavioral intervention component, where the addition of sleep hygiene education demonstrated improvements in self-reported sleep quality and an increase in actigraphy-derived total sleep time (Swinbourne et al., Citation2018).
Direct studies exhibited the lowest frequency of BCT usage (mean: 1 ± 0). Furthermore, the BCTs used were the most homogenous; “1.1 Goal setting (behavior)” was present in all the direct studies due to the inherent goal-setting aspect, while “4.1 Instruction on how to perform a behavior” was the only other BCT identified, appearing in two instances.
Multi-component
Seven studies integrated two or more distinct components within the delivered intervention. In five studies, behavioral components such as education or sleep hygiene strategies were integrated to support the utilization of non-behavioral components including light therapies, cold water immersion, and environmental modifications (Charest et al., Citation2017; de Mello et al., Citation2020; Duffield et al., Citation2014; Fullagar et al., Citation2016; Vachon et al., Citation2022). The remaining two studies included the amalgamation of education and mind-body practices (Vachon et al., Citation2023), and a cluster of behavioral components including education, tracking, and social support (Grandner et al., Citation2017). All studies exhibited a significant change in one or more assessed sleep outcome with the exception of Duffield et al. (Citation2014), where large effect sizes were demonstrated within a limited sample size.
The mean number of BCTs utilized per study was 2 ± 2, yet a distinct division was apparent. Three studies featured four or five BCTs present, spanning a diverse range of nine BCT groupings (Grandner et al., Citation2017; Vachon et al., Citation2022, Citation2023). Conversely, the remaining four studies either employed “8.1 Behavioral practice/substitution” as the sole BCT, or in the case of Charest et al. (Citation2017), no BCTs were identified.
Other
Three studies did not align with the previously discussed categories. In Bender et al. (Citation2018) and Tuomilehto et al. (Citation2017), the intervention components delivered were contingent on a sleep assessment performed at baseline and thus varied in content and duration between participants. Both studies featured 2 BCTs, though the use of the BCTTv1 framework was limited to the intervention components delivered to all participants. Jakowski and Stork (Citation2022) employed a combination of app feedback and smart alarms using the BCT “2.2 Feedback on behavior”, yet no significant changes in sleep outcomes were observed.
Quality appraisal
Twenty studies underwent appraisal using the nine-item assessment tool for quasi-experimental studies, yielding a mean study score of 6 ± 1. The poorest scored items pertained to the inclusion of a control group (Q4, 1/20 studies) and appropriate statistical analysis (Q9, 8/20 studies). Nine studies were assessed using the 13-item appraisal tool for randomized controlled trials, producing a mean study score of 8 ± 2. The poorest scored items concerned insufficient blinding of participants (Q4) and researchers (Q5) to treatment allocation (both 1/9 studies). A comprehensive breakdown of the quality appraisal scores for each study is presented in Appendix Tables S5 and S6.
Discussion
The objectives of this scoping review were to identify and map the existing body of evidence on behavioral sleep interventions in athletes and their effect on sleep outcomes, and retrospectively code the BCTs employed in identified interventions using the BCTTv1 framework. This review identified a total of 33 studies, all published within the last decade, reflecting the burgeoning interest in athlete sleep. Diverse behavioral strategies were employed within the included interventions, coalescing into five categories: educational, mind-body practices, direct, multi-component, and other. These categories exhibited distinctions concerning the individual BCTs used and the frequency of usage. However, only 18 of the 93 BCTs specified in the BCTTv1 were identified across the 33 studies. This finding indicates there are alternative behavioral strategies that remain currently unexplored within athletes that could potentially prove effective in instigating favorable changes in sleep outcomes.
The sleep outcomes extracted from the included studies indicate that each category of behavioral intervention can be effective at improving sleep outcomes. This reaffirms the viability of behavioral interventions to improve athlete sleep indicated in previous reviews (Bonnar et al., Citation2018; Gwyther et al., Citation2022; Silva et al., Citation2021). However, there are important considerations beyond changes in sleep outcomes for each intervention category that should be noted. Direct interventions exhibited the most notable changes in sleep outcomes, with multiple studies achieving an increase in total sleep time exceeding an hour. Yet, the application of a direct intervention outside a controlled intervention poses challenges when the wider impact of the social-environmental context on sleep is considered (Grandner, Citation2017). For instance, sport-related factors impinge the ability to increase sleep opportunity, such as that noted by Mah et al. (Citation2011) where travel schedules impaired the ability to maintain a consistent sleep-wake pattern. Educational interventions emerged as the most prevalent intervention type. A recent consensus statement advocates the use of sleep education multiple times a year as a first-line tool to improve sleep in athletes, irrespective of baseline sleep characteristics (Walsh et al., Citation2020). However, concerns over the long-term efficacy of sleep education as a standalone tool have been raised (Halson, Citation2019), and were exemplified in the study by Caia et al. (Citation2018) where improvements in sleep outcomes were not maintained post-intervention. This observation aligns with the core components of the COM-B behavior change model (Michie et al., Citation2011), as while education can bolster psychological capability, it is unable to overcome deficits in opportunity or automatic motivation that may prevent sleep behavior change. Therefore, the inclusion of education as part of a multi-component intervention may be more prudent. Mind-body practices and multi-component interventions demonstrated efficacy at changing sleep outcomes, however quantifying the contribution of behavioral driven changes poses certain challenges for both categories. In mind-body practices, behavioral changes are inherently intertwined with bodily changes. Furthermore, the purpose of these interventions is not solely to change sleep behavior, but to enhance holistic health. This is highlighted by the inclusion of sleep as one of multiple health outcomes assessed in several studies (Chen et al., Citation2018; Jones et al., Citation2020; Rijken et al., Citation2016). Similarly, in multi-component interventions, dissecting the effect of each component is complex in the absence of a comparison condition, where a single component is delivered in isolation. Lastly, while studies involving individually tailored studies are highly applicable to real-world practice (Bender et al., Citation2018; Tuomilehto et al., Citation2017), the level of detail provided in a journal article format restricts the evaluation of behavioral components only delivered to select participants.
While the biological regulation of sleep introduces a layer of complexity to the implementation of behavior change theory within sleep health interventions when compared to more traditional health intervention targets like physical activity, many facets of sleep remain under behavioral control (Mead & Irish, Citation2020). This study aligns with previous reviews that view sleep through a behavioral lens and have applied the BCTTv1 framework to specify the BCTs employed within sleep interventions across diverse populations.The average use of BCTs within the journal articles included in this review (mean: 2.7) is notably higher than a previous review on sleep extension interventions for ages ≥ 12 (mean: 1.8; Baron et al., Citation2021), yet falls short of those found in a review focused on interventions in emergent adults aged 18–29 (mean: 4.25; Pegado et al., Citation2023). The diversity of BCT groupings used in this review (12 out of 16 BCT groupings) sits above the eight BCT groupings identified by Baron et al. (Citation2021) and the 11 groupings identified by Pegado et al. (Citation2023), however, the latter was observed across only eight studies. This suggests there is scope to incorporate more BCTs within future behavioral sleep interventions tailored toward athletes, with specific literature gaps evident. For instance, the group sessions performed in all but one educational intervention could provide a “blank canvas” to incorporate multiple BCTs beyond the scope of education delivery. This was demonstrated in two studies that incorporated five and six unique BCTs into a multifaceted workshop format (Kaier et al., Citation2016; Sargent et al., Citation2021). The incorporation of multiple BCTs has been shown to improve the extent of increases in total sleep times, but conversely, interventions with a large number of curriculum components showed smaller increases in TST compared to those with fewer curriculum components (Baron et al., Citation2021). Hence, ensuring workshops are designed to be concise but targeted and impactful regarding BCT implementation is an important consideration, and provides an avenue to enhance the efficacy of future interventions. highlights examples of such BCTs that were not identified in any studies within this review, but could be incorporated into a workshop format.
Table 3. Example BCTs for integration into group sessions.
While the rationale behind the inclusion of specific BCTs within studies cannot be determined through retrospective coding, the justification for intervention design lacks clarity, and in certain instances, empirical substantiation. The mixed efficacy of sleep health interventions has been in part attributed to the absence of behavior theory as a foundation for intervention design (Mead & Irish, Citation2020), while health interventions that embed behavior change theory within development tend to demonstrate more consistently positive outcomes (Glanz & Bishop, Citation2010). As an illustration, the integration of the BCT “4.1 Instruction on how to perform a behavior” within an educational sleep intervention would be strengthened by prior evidence demonstrating that the targeted athletes possess insufficient knowledge regarding sleep behaviors. Various behavioral theories can be applied to sleep health research (Mead & Irish, Citation2020). The use of the BCTTv1 taxonomy in conjunction with the COM-B behavioral model provides a potential avenue to bridge the existing gap between a behavioral diagnosis and intervention development (Michie et al., Citation2011). The COM-B can be used to identify which of the core components of capability, opportunity, and motivation are underpinning the undesired behavior, and can then be mapped onto the BCTTv1 such that only relevant BCTs are incorporated within a precisely targeted intervention (Michie et al., Citation2013). There exists a plausible rationale for any combination of the COM-B components to underpin desired and undesired sleep behaviors in athletes, and likely differ contingent on the unique attributes of the athlete group being addressed, such as age, sex, and performance level amongst other variables. This underscores the need to specify the problem in behavioral terms before attempting to resolve it.
The quality appraisal conducted on the included studies showed that study quality was generally satisfactory, but highlighted some limitations within the current literature. The inclusion of control conditions within quasi-experimental study designs is undoubtedly challenging, with methodological constraints including participant availability and the cost and availability of measurement tools. Nevertheless, with various sport-related and non-sport-related factors acting as extraneous variables that can influence observed sleep outcomes (e.g., Astridge et al., Citation2021), control conditions should be implemented where possible to ensure changes can be attributed to the intervention and enhance the robustness of findings. Furthermore, the lack of blinding of both participants and researchers surfaced as a limitation in randomized controlled trials. This is a common issue within applied behavioral research, however, recommendations such as the use of an additional unblinded research coordinator can minimize bias (Friedberg et al., Citation2010).
A component of quality appraisal not evaluated by the JBI assessment tools is the pre-registration of studies. No studies referenced pre-registration within the manuscript, and a search of Open Science Framework and PubPsych online repositories returned only a handful of studies included in this review (Jakowski & Stork, Citation2022; Jones et al., Citation2020; Rijken et al., Citation2016; Schwartz & Simon, Citation2015). Furthermore, some studies omitted the a priori outcomes and/or definitions of extracted sleep outcomes within the methods section. In the future, behavioral sleep interventions in athletes should preregister studies in a public repository to increase transparency and confidence in findings (Hardwicke & Wagenmakers, Citation2023).
Limitations
An important limitation of this scoping review is that, whilst the coding of BCTs was facilitated by the BCTTv1, there remains a subjective element contingent upon the philosophical standpoint of the coders. The coders in this review adopted a more liberal approach to BCT coding, and as such identified a slightly greater number of BCTs in several studies that were also included in a previous review (Baron et al., Citation2021). This process is further complicated by the restrictive word count imposed upon most journal articles, which often prevents the inclusion of comprehensive methodological details, and in turn, creates ambiguity regarding the application of specific BCTs. Two key strategies can be incorporated into future research to overcome this limitation: (1) the publication of study intervention manuals as an appendix or in an open repository, and (2) the employment of standardized terminologies, such as those defined within the BCTTv1 when describing behavioral components within an intervention.
There also exist limitations related to the search parameters employed in this review, most notably related to age. Although this restriction was applied in response to the differences in biological sleep regulation during childhood and adolescence (Hagenauer et al., Citation2009), it is noteworthy that recent research has employed behavioral sleep interventions within athletes in this age group, and contain BCTs that could apply to adult athletes and warrant further exploration (e.g., Aben et al., Citation2023; Edinborough et al., Citation2023; Lever et al., Citation2021). Finally, there are inherent methodological limitations concerning the search strategy employed. These include the non-consideration of gray literature and unpublished studies, the reliance on only five databases for literature searching, and the inclusion of English-only studies. While these choices were pragmatic, they may have resulted in the inadvertent exclusion of relevant studies.
Conclusion and future directions
To summarize, this scoping review sheds light on the wide range of behavioral sleep interventions that have been performed in athlete populations within the last decade. The identified intervention categories – educational, mind-body practices, direct, multi-component, and other – differed concerning the prevalence and diversity of BCTs implemented. While each category contained studies demonstrating some favorable changes to sleep outcomes, there was no clear study type or BCT that showed consistent changes. Furthermore, the limited range of BCTs used would indicate that there are alternative behavioral components that have yet to be examined in athletes. The included studies appear to exhibit an insufficient integration of behavior change theory during intervention development, which could partially explain the mixed effectiveness observed concerning sleep outcomes. Moving forward, future studies should prioritize the completion of a behavioral diagnosis before intervention development that is specific to the athlete cohort the intervention is targeting. Furthermore, any behavioral components incorporated into interventions should be specified using standardized terminology, such as those outlined in the BCTTv1. This would facilitate more effective cross-study comparisons, and pave the way for a future meta-analysis that could identify the most potent BCTs for driving sleep behavior change in athlete populations.
Author contributions
SMBW acted as the reviewer at each stage and wrote the review. KVS acted as a reviewer for screening and study selection. JKP acted as a reviewer for quality appraisal and data extraction. AC acted as a reviewer for the coding of behavior change techniques. SBD, MIJ, and JKP were involved in the direction and revision of the manuscript. All authors read and approved the final manuscript.
BSM_Appendix_Revision clean.docx
Download MS Word (39 KB)BSM PRISMA ScR Checklist.docx
Download MS Word (84.1 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data supporting the findings of this study are available within the article and its supplementary materials.
Supplemental data
Supplemental data for this article can be accessed online at https://doi.org/10.1080/15402002.2024.2374257.
Additional information
Funding
References
- Aben, H. G. J., Hills, S. P., Higgins, D., Cooke, C. B., Davis, D., Jones, B., & Russell, M. (2023). The efficacy of a multimodal recovery strategy implemented after a high-intensity rugby league training session. Journal of Strength and Conditioning Research, 37(8), 1634–1642. https://doi.org/10.1519/JSC.0000000000004450
- Abraham, C., & Michie, S. (2008). A taxonomy of behaviour change techniques used in interventions. Health Psychology, 27(3), 379–387. https://doi.org/10.1037/0278-6133.27.3.379
- Alfonso-Miller, P., Athey, A., & Grandner, M. A. (2017). Evaluation of a sleep health intervention in student-athletes: Insights for intervention development. Sleep, 40(Suppl. 1), A450–A450. https://doi.org/10.1093/sleepj/zsx050.1205
- Astridge, D., Sommerville, A., Verheul, M., & Turner, A. P. (2021). Training and academic demands are associated with sleep quality in high-performance “dual career” student swimmers. European Journal of Sport Science, 21(12), 1675–1683. https://doi.org/10.1080/17461391.2020.1857442
- Athey, A., Alfonso-Miller, P., Killgore, W. D., & Grandner, M. A. (2017). Preliminary results of a sleep health intervention in student athletes: Perceived changes to sleep, performance, and mental and physical well-being. Sleep, 40(Suppl. 1), A450–A450. https://doi.org/10.1093/sleepj/zsx050.1206
- Baron, K. G., Duffecy, J., Reutrakul, S., Levenson, J. C., McFarland, M. M., Lee, S., & Qeadan, F. (2021). Behavioral interventions to extend sleep duration: A systematic review and meta-analysis. Sleep Medicine Reviews, 60, 101532. https://doi.org/10.1016/j.smrv.2021.101532
- Bender, A. M., Lawson, D., Werthner, P., & Samuels, C. H. (2018). The clinical validation of the Athlete sleep screening questionnaire: An instrument to identify athletes that need further sleep assessment. Sports Medicine – Open, 4(1), 23. https://doi.org/10.1186/s40798-018-0140-5
- Bonnar, D., Bartel, K., Kakoschke, N., & Lang, C. (2018). Sleep interventions designed to improve athletic performance and recovery: A systematic review of current approaches. Sports Medicine, 48(3), 683–703. https://doi.org/10.1007/s40279-017-0832-x
- Caia, J., Scott, T. J., Halson, S. L., & Kelly, V. G. (2018). The influence of sleep hygiene education on sleep in professional rugby league athletes. Sleep Health, 4(4), 364–368. https://doi.org/10.1016/j.sleh.2018.05.002
- Charest, J., Bender, A., Bastien, C., & Samuels, C. (2017). Sleep interventions improve subjective sleep, mood, and race performance in Canadian national team speed skaters. Sleep Medicine, 40, e51–e52. https://doi.org/10.1016/j.sleep.2017.11.144
- Chen, J. H., Tsai, P. H., Lin, Y. C., Chen, C. K., & Chen, C. Y. (2018). Mindfulness training enhances flow state and mental health among baseball players in Taiwan. Psychology Research and Behavior Management, 12, 15–21. https://doi.org/10.2147/prbm.s188734
- Datta, K., Yadav, N., Narawade, Y., Mahajan, U., Joseph, T., & Kumar, A. (2022). Sleep strategies for sportsmen; what can they be? A randomised controlled trial. Sleep and Vigilance, 6(1), 165–171. https://doi.org/10.1007/s41782-021-00188-8
- Davis, R., Campbell, R., Hildon, Z., Hobbs, L., & Michie, S. (2015). Theories of behaviour and behaviour change across the social and behavioural sciences: A scoping review. Health Psychology Review, 9(3), 323–344. https://doi.org/10.1080/17437199.2014.941722
- de Mello, M. T., Simim, M. A. M., Narciso, F. V., Rosa, J. P. P., Rodrigues, D. F., Freitas, L. S. N., Bichara, J. J., Pereira, S. R. D., da Silva, S. C., Tufik, S., & Silva, A. (2020). Duration and quality of sleep in sprint and recovery performances among elite swimmers. Revista Brasileira de Medicina do Esporte, 26(2), 126–129. https://doi.org/10.1590/1517-869220202602220003
- Driller, M. W., Lastella, M., & Sharp, A. P. (2019). Individualized sleep education improves subjective and objective sleep indices in elite cricket athletes: A pilot study. Journal of Sports Sciences, 37(17), 2121–2125. https://doi.org/10.1080/02640414.2019.1616900
- Duffield, R., Murphy, A., Kellett, A., & Reid, M. (2014). Recovery from repeated on-court tennis sessions: Combining cold-water immersion, compression, and sleep interventions. International Journal of Sports Physiology and Performance, 9(2), 273–282. https://doi.org/10.1123/ijspp.2012-0359
- Dunican, I. C., Caldwell, J. A., Morgan, D., Stewart, A., & Eastwood, P. R. (2021). An education intervention in a professional female basketball team and coaching staff improves sleep and alertness. Translational Sports Medicine, 4(3), 419–427. https://doi.org/10.1002/tsm2.218
- Dunican, I. C., Perry, E., Maisey, G., Nesci, E., & Roberts, S. (2023). Sleep hygiene education for improving sleep in ultra-marathon swimmers: Guidance for coaches and swimmers. International Journal of Sports Science and Coaching, 1–7. https://doi.org/10.1177/17479541231152196
- Edinborough, L., Hill, J., Jarvis, M., Bruce-Low, S., & Pedlar, C. R. (2023). A bespoke sleep monitoring and sleep hygiene intervention improves sleep in an U18 professional football player: A case study. Journal of Sports Sciences, 41(4), 350–357. https://doi.org/10.1080/02640414.2023.2213032
- Famodu, O. A., Montgomery-Downs, H., Thomas, J. M., Gilleland, D. L., Bryner, R. W., & Olfert, M. D. (2017). Impact of a single week of sleep extension on performance, mood, and nutrition among female college track athletes. Sleep, 40(Suppl. 1), A32. https://doi.org/10.1093/sleepj/zsx050.082
- Famodu, O., Bryner, R., Montgomery-Downs, H., & Olfert, M. (2014). Effects of extended sleep on female athlete’s performance and nutrition. FASEB Journal, 28(Suppl. 1), 633.632. https://doi.org/10.1096/fasebj.28.1_supplement.633.2
- Friedberg, J. P., Lipsitz, S. R., & Natarajan, S. (2010). Challenges and recommendations for blinding in behavioral interventions illustrated using a case study of a behavioral intervention to lower blood pressure. Patient Education and Counseling, 78(1), 5–11. https://doi.org/10.1016/j.pec.2009.04.009
- Fullagar, H., Skorski, S., Duffield, R., & Meyer, T. (2016). The effect of an acute sleep hygiene strategy following a late-night soccer match on recovery of players. Chronobiology International, 33(5), 490–505. https://doi.org/10.3109/07420528.2016.1149190
- Glanz, K., & Bishop, D. B. (2010). The role of behavioral science theory in development and implementation of public health interventions. Annual Review of Public Health, 31(1), 399–418. https://doi.org/10.1146/annurev.publhealth.012809.103604
- Grade, I., Andrade, H., Guerreiro, R., Stieler, E., Da Silva, F. R., Da Silva, H. G. V., Vital, R., Resende, R. A., Gonçalves, D. A. P., Andrade, A. G., De Mello, M. T., & Silva, A. (2023). The sleep parameters of Paralympic athletes: Characteristics and assessment instruments. Journal of Sport Rehabilitation, 32(2), 203–214. https://doi.org/10.1123/jsr.2021-0407
- Grandner, M. A. (2017). Sleep, health, and society. Sleep Medicine Clinics, 12(1), 1–22. https://doi.org/10.1016/j.jsmc.2016.10.012
- Grandner, M. A., Athey, A., Killgore, W. D., & Alfonso-Miller, P. (2017). Preliminary results of a sleep health intervention in student athletes: Changes in sleep, energy level, and mental well-being, and body weight. Sleep, 40(Suppl. 1), A294. https://doi.org/10.1093/sleepj/zsx050.792
- Gupta, L., Morgan, K., & Gilchrist, S. (2017). Does elite sport degrade sleep quality? A systematic review. Sports Medicine, 47(7), 1317–1333. https://doi.org/10.1007/s40279-016-0650-6
- Gwyther, K., Rice, S., Purcell, R., Pilkington, V., Santesteban-Echarri, O., Bailey, A., & Walton, C. C. (2022). Sleep interventions for performance, mood and sleep outcomes in athletes: A systematic review and meta-analysis. Psychology of Sport and Exercise, 58, 102094. https://doi.org/10.1016/j.psychsport.2021.102094
- Hagenauer, M. H., Perryman, J. I., Lee, T. M., & Carskadon, M. A. (2009). Adolescent changes in the homeostatic and circadian regulation of sleep. Developmental Neuroscience, 31(4), 276–284. https://doi.org/10.1159/000216538
- Halson, S. L. (2019). Sleep monitoring in athletes: Motivation, methods, miscalculations and why it matters. Sports Medicine, 49(10), 1487–1497. https://doi.org/10.1007/s40279-019-01119-4
- Harada, T., Wada, K., Tsuji, F., Krejci, M., Kawada, T., Noji, T., Nakade, M., & Takeuchi, H. (2016). Intervention study using a leaflet entitled ‘three benefits of “go to bed early! get up early! and intake nutritionally rich breakfast!” a message for athletes’ to improve the soccer performance of university soccer team. Sleep and Biological Rhythms, 14(Suppl. 1), 65–74. https://doi.org/10.1007/s41105-015-0035-5
- Hardwicke, T. E., & Wagenmakers, E.-J. (2023). Reducing bias, increasing transparency and calibrating confidence with preregistration. Nature Human Behaviour, 7(1), 15–26. https://doi.org/10.1038/s41562-022-01497-2
- Jakowski, S., & Stork, M. (2022). Effects of sleep self-monitoring via app on subjective sleep markers in student athletes. Somnologie, 26(4), 244–251. https://doi.org/10.1007/s11818-022-00395-z
- Jarraya, S., Jarraya, M., Chtourou, H., & Souissi, N. (2014). Effect of time of day and partial sleep deprivation on the reaction time and the attentional capacities of the handball goalkeeper. Biological Rhythm Research, 45(2), 183–191. https://doi.org/10.1080/09291016.2013.787685
- Jenkins, C. D. R., Moody, J. A., Byrne, P. J., & Esformes, J. I. (2021). Acute effects of in-season sleep hygiene education on elite rugby union athletes. ARC Journal of Research in Sports Medicine, 5(1), 28–34. https://www.arcjournals.org/journal-of-research-in-sports-medicine/volume-5-issue-1/
- Jones, B. J., Kaur, S., Miller, M., & Spencer, R. M. C. (2020). Mindfulness-based stress reduction benefits psychological well-being, sleep quality, and athletic performance in female collegiate rowers. Frontiers in Psychology, 11, 572980. https://doi.org/10.3389/fpsyg.2020.572980
- Kaier, E., Zanotti, D., Davis, J. L., Strunk, K., & Cromer, L. D. (2016). Addressing the problem of student-athlete sleepiness: Feasibility of implementing an interactive sleep workshop at a division I school. Journal of Clinical Sport Psychology, 10(3), 237–247. https://doi.org/10.1123/jcsp.2015-0023
- Kirschen, G. W., Jones, J. J., & Hale, L. (2020). The impact of sleep duration on performance among competitive athletes: A systematic literature review. Clinical Journal of Sport Medicine, 30(5), 503–512. https://doi.org/10.1097/JSM.0000000000000622
- Landis, J. R., & Koch, G. G. (1977). The measurement of observer agreement for categorical data. Biometrics Bulletin, 33(1), 159–174. https://doi.org/10.2307/2529310
- Lastella, M., Roach, G. D., Halson, S. L., & Sargent, C. (2015). Sleep/wake behaviours of elite athletes from individual and team sports. European Journal of Sport Science, 15(2), 94–100. https://doi.org/10.1080/17461391.2014.932016
- Leduc, C., Weaving, D., Owen, C., Ramirez-Lopez, C., Chantler, S., Aloulou, A., Tee, J., Jones, B., & Ruddock, A. (2022). The effect of acute sleep extension vs active recovery on post exercise recovery kinetics in rugby union players. PLoS One, 17(8), e0273026. https://doi.org/10.1371/journal.pone.0273026
- Lever, J. R., Murphy, A. P., Duffield, R., & Fullagar, H. H. K. (2021). A combined sleep hygiene and mindfulness intervention to improve sleep and well-being during high-performance youth tennis tournaments. International Journal of Sports Physiology & Performance, 16(2), 250–258. https://doi.org/10.1123/ijspp.2019-1008
- Mah, C. D., Anguera, J. A., Gazzaley, A., & Luke, A. (2017). Sleep loading improves visual search response time and reduces fatigue in professional baseball players. Sleep, 40(Suppl. 1), A278. https://doi.org/10.1093/sleepj/zsx050.748
- Mah, C. D., Mah, K. E., Kezirian, E. J., & Dement, W. C. (2011). The effects of sleep extension on the athletic performance of collegiate basketball players. Sleep, 34(7), 943–950. https://doi.org/10.5665/SLEEP.1132
- McCloughan, L., Hanrahan, S., Anderson, R., & Halson, S. (2014). Progressive muscle relaxation (PMR), sleep, and recovery in elite performers. Journal of Science and Medicine in Sport, 18(Suppl. 1), e113. https://doi.org/10.1016/j.jsams.2014.11.071
- McCloughan, L. J., Hanrahan, S. J., Anderson, R., & Halson, S. R. (2016). Psychological recovery: Progressive muscle relaxation (PMR), anxiety, and sleep in dancers. Performance Enhancement and Health, 4(1–2), 12–17. https://doi.org/10.1016/j.peh.2015.11.002
- McKay, A. K. A., Stellingwerff, T., Smith, E. S., Martin, D. T., Mujika, I., Goosey-Tolfrey, V. L., Sheppard, J., & Burke, L. M. (2022). Defining training and performance caliber: A participant classification framework. International Journal of Sports Physiology and Performance, 17(2), 317–331. https://doi.org/10.1123/ijspp.2021-0451
- Mead, M. P., & Irish, L. A. (2020). Application of health behaviour theory to sleep health improvement. Journal of Sleep Research, 29(5). https://doi.org/10.1111/jsr.12950
- Michie, S., & Johnston, M. (2013). Behavior change techniques. In M. D. Gellman & J. R. Turner (Eds.), Encyclopedia of behavioral medicine (1st ed. pp. 182–187). Springer.
- Michie, S., Richardson, M., Johnston, M., Abraham, C., Francis, J., Hardeman, W., Eccles, M. P., Cane, J., & Wood, C. E. (2013). The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Annals of Behavioral Medicine, 46(1), 81–95. https://doi.org/10.1007/s12160-013-9486-6
- Michie, S., Van Stralen, M. M., & West, R. (2011). The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implementation Science, 6(1), 42. https://doi.org/10.1186/1748-5908-6-42
- Milewski, M. D., Skaggs, D. L., Bishop, G. A., Pace, J. L., Ibrahim, D. A., Wren, T. A., & Barzdukas, A. (2014). Chronic lack of sleep is associated with increased sports injuries in adolescent athletes. Journal of Pediatric Orthopaedics, 34(2), 129–133. https://doi.org/10.1097/BPO.0000000000000151
- Munn, Z., Peters, M. D. J., Stern, C., Tufanaru, C., McArthur, A., & Aromataris, E. (2018). Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Medical Research Methodology, 18(1). https://doi.org/10.1186/s12874-018-0611-x
- O’Donnell, S., & Driller, M. W. (2017). Sleep-hygiene education improves sleep indices in elite female athletes. International Journal of Exercise Science, 10(4), 522–530. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5466408/
- Ouzzani, M., Hammady, H., Fedorowicz, Z., & Elmagarmid, A. (2016). Rayyan – a web and mobile app for systematic reviews. Systematic Reviews, 5(1), 210. https://doi.org/10.1186/s13643-016-0384-4
- Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S. & Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, n71. https://doi.org/10.1136/bmj.n71
- Pegado, A., Alvarez, M. J., & Roberto, M. S. (2023). The role of behaviour-change theory in sleep interventions with emerging adults (aged 18–29 years): A systematic review and meta-analysis. Journal of Sleep Research, 32(5), e13877. https://doi.org/10.1111/jsr.13877
- Peters, M. D. J., Marnie, C., Tricco, A. C., Pollock, D., Munn, Z., Alexander, L., McInerney, P., Godfrey, C. M., & Khalil, H. (2020). Updated methodological guidance for the conduct of scoping reviews. JBI Evidence Synthesis, 18(10), 2119–2126. https://doi.org/10.11124/JBIES-20-00167
- Rijken, N. H., Soer, R., de Maar, E., Prins, H., Teeuw, W. B., Peuscher, J., & Oosterveld, F. G. (2016). Increasing performance of professional soccer players and elite track and field athletes with peak performance training and biofeedback: A pilot study. Applied Psychophysiology and Biofeedback, 41(4), 421–430. https://doi.org/10.1007/s10484-016-9344-y
- Roberts, S. S. H., Aisbett, B., Teo, W. P., & Warmington, S. (2022). Monitoring effects of sleep extension and restriction on endurance performance using heart rate indices. The Journal of Strength & Conditioning Research, 36(12), 3381–3389. https://doi.org/10.1519/jsc.0000000000004157
- Roberts, S. S. H., Teo, W. P., Aisbett, B., & Warmington, S. A. (2019). Extended sleep maintains endurance performance better than normal or restricted sleep. Medicine and Science in Sports and Exercise, 51(12), 2516–2523. https://doi.org/10.1249/mss.0000000000002071
- Sargent, C., Lastella, M., Schwerdt, S., & Roach, G. D. (2021). An individualized intervention increases sleep duration in professional athletes. Journal of Strength and Conditioning Research, 35(12), 3407–3413. https://doi.org/10.1519/JSC.0000000000004138
- Schwartz, J., & Simon, R. D., Jr. (2015). Sleep extension improves serving accuracy: A study with college varsity tennis players. Physiology and Behavior, 151, 541–544. https://doi.org/10.1016/j.physbeh.2015.08.035
- Silva, A. C., Silva, A., Edwards, B. J., Tod, D., de Souza Amaral, A., de Alcântara Borba, D., Grade, I., & de Mello, M. T. (2021). Sleep extension in athletes: What we know so far – a systematic review. Sleep Medicine, 77, 128–135. https://doi.org/10.1016/j.sleep.2020.11.028
- Swinbourne, R., Miller, J., Smart, D., Dulson, D. K., & Gill, N. (2018). The effects of sleep extension on sleep, performance, immunity and physical stress in rugby players. Sports, 6(2), 42. https://doi.org/10.3390/sports6020042
- Tricco, A. C., Lillie, E., Zarin, W., O’Brien, K. K., Colquhoun, H., Levac, D., Moher, D., Peters, M. D. J., Horsley, T., Weeks, L., Hempel, S., Akl, E. A., Chang, C., McGowan, J., Stewart, L., Hartling, L., Aldcroft, A., Wilson, M. G., Garritty, C. & Straus, S. E. (2018). PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Annals of Internal Medicine, 169(7), 467–473. https://doi.org/10.7326/M18-0850
- Tufanaru, C., Munn, Z., Aromataris, E., Campbell, J., & Hopp, L. (2020). Chapter 3: Systematic reviews of effectiveness. In E. Aromataris & Z. Munn (Eds.), JBI manual for evidence synthesis. JBI. https://doi.org/10.46658/JBIMES-20-04
- Tuomilehto, H., Vuorinen, V. P., Penttila, E., Kivimaki, M., Vuorenmaa, M., Venojarvi, M., Airaksinen, O., & Pihlajamaki, J. (2017). Sleep of professional athletes: Underexploited potential to improve health and performance. Journal of Sports Sciences, 35(7), 704–710. https://doi.org/10.1080/02640414.2016.1184300
- Vachon, A., Berryman, N., Mujika, I., Paquet, J.-B., Sauvet, F., & Bosquet, L. (2022). Impact of tapering and proactive recovery on young elite rugby union players’ repeated high intensity effort ability. Biology of Sport, 39(3), 735–743. https://doi.org/10.5114/biolsport.2022.109453
- Vachon, A., Sauvet, F., Pasquier, F., Paquet, J. B., & Bosquet, L. (2023). Effects of a sleep hygiene strategy on parameters of sleep quality and quantity in youth elite rugby union players. International Journal of Sports Physiology and Performance, 1–8. https://doi.org/10.1123/ijspp.2023-0069
- Van Ryswyk, E., Weeks, R., Bandick, L., O’Keefe, M., Vakulin, A., Catcheside, P., Barger, L., Potter, A., Poulos, N., Wallace, J., & Antic, N. A. (2017). A novel sleep optimisation programme to improve athletes’ well-being and performance. European Journal of Sport Science, 17(2), 144–151. https://doi.org/10.1080/17461391.2016.1221470
- Vitale, J. A., La Torre, A., Banfi, G., & Bonato, M. (2019). Acute sleep hygiene strategy improves objective sleep latency following a late-evening soccer-specific training session: A randomized controlled trial. Journal of Sports Sciences, 37(23), 2711–2719. https://doi.org/10.1080/02640414.2019.1661938
- Walsh, N. P., Halson, S. L., Sargent, C., Roach, G. D., Nedelec, M., Gupta, L., Leeder, J., Fullagar, H. H., Coutts, A. J., Edwards, B. J., Pullinger, S. A., Robertson, C. M., Burniston, J. G., Lastella, M., Le Meur, Y., Hausswirth, C., Bender, A. M., Grandner, M. A., & Samuels, C. H. (2020). Sleep and the athlete: Narrative review and 2021 expert consensus recommendations. British Journal of Sports Medicine, 55(7), 356–368. https://doi.org/10.1136/bjsports-2020-102025