Abstract
Chronic Obstructive Pulmonary Disease (COPD) has a significant burden on patients and the healthcare system. There is a link between COPD and comorbidities such as congestive heart failure (CHF), fluid and electrolyte disorders, and renal failure. This adds to the complexity of healthcare in these patients. The objective of this study is to determine if certain comorbidities affect length of stay. A sample of 3,399 patients with COPD were assessed from the Premier© healthcare database. The cohort had a mean (standard deviation (SD)) age of 68.41 (10.85) years. The average number of comorbidities was 24.83 (10.46) with a mean length of stay (SD) of 11.64 (9.40) days. A negative binomial regression model was used to evaluate the impact that comorbidities have on the length of hospital stay. The authors found that the number of comorbidities was associated with an increased length of stay (r = .4596, p < .0001). Having at least one comorbidity was associated with a 13% greater length of stay (IRR = 1.13, 95% CI 1.11–1.15, p < 0.0001). CHF was associated with a 28% greater length of stay (IRR = 1.28, 95% CI 1.24–1.31, p < 0.0001). Fluid and electrolyte disorders were associated with a 2-fold greater length of stay (IRR = 2.57, 95% CI 2.52–2.62, p < 0.0001). Renal failure was associated with a 50% greater length of stay (IRR = 1.50, 95% CI 1.45–1.55, p < 0.0001). However, uncomplicated diabetes was associated with 13% shorter length of stay than not having uncomplicated diabetes (IRR = .87, 95% CI .82–.91, p < .0001). This study demonstrated that specific comorbidities have an impact on length of stay.
Introduction
Chronic Obstructive Pulmonary Disease (COPD) is a preventable and treatable disease with significant pulmonary effects that contribute to the impairment in patient functionality, thereby leading to morbidity and ultimately death (Citation1). COPD has been identified as a major health concern worldwide (Citation1). It is estimated that around 80 million people are affected by this disease (Citation1). In 2014, more than 12 million people have been diagnosed with COPD in the United States (Citation1). Hospital admissions for acute exacerbations have increased by nearly 60% over the last 10 years (Citation2). An exacerbation is defined as anything that requires intensifying management (Citation2). The direct and indirect costs of caring for patients with COPD in the United States are estimated to be around 50 billion (Citation1). These costs are suspected to be linked to increased length of stay.
There is a strong link between chronic comorbidity and exacerbation risks for patients with COPD (Citation3). Literature relates such diseases as cardiovascular disease, metabolic syndrome, skeletal muscle dysfunction, lung cancer, and depression to COPD (Citation3). This link is driven not only by these patients having an increased risk for other diseases due to their diminished lung function but this could also be directly related to such things as pharmacologic management. COPD patients who require continual regimens of high-dose inhaled corticosteroids have been shown to be at risk for the development of osteoporosis (Citation4). Researchers have identified that the systemic inflammation that occurs in COPD can be directly linked to an increase risk of developing several other disease processes (Citation5). It is important to identify if comorbidities are independent of COPD or if these comorbidities have common pathophysiologic pathways.
Hospitalizations for patients admitted for acute exacerbation of COPD count for nearly one-fourth of the overall direct costs of the disease (Citation6). However, there is limited literature internationally and within the United States that assesses the link between the number of comorbidities and length of stay. The lack of studies from the United States make it hard to infer the impact that comorbidities have on COPD patients in this country. The objective of this study is to assess if there is a direct link between comorbidities and length of stay in patients with COPD, this study can help to drive policy change related to the management of patients with COPD.
Methods
Study design
A longitudinal retrospective observational study was conducted. A sample of the Premier© healthcare database from January 1, 2016 to December 31, 2016 was used to determine if the number of comorbidities affects length of stay in patients with a primary diagnosis of COPD. The Premier© healthcare database is a large, United States hospital-based database that has information on inpatient discharges. Inpatient admissions include over 81 million visits which represents 20% of annual United States inpatient discharges (Citation7). Patients can be tracked in the same hospital across the inpatient and hospital-based outpatient settings and this allows for assessing hospital length of stay and readmissions to the same hospital (Citation7). Hospitals in the Premier© healthcare database represent the four geographic regions as defined by the United States Census (Citation7). Hospital level data includes admitting and attending physician specialities, point of origin, type of admission and discharge status. Patient demographics include age, sex, race, and ethnicity (Citation7). This study was exempt from IRB by the University of North Carolina-Charlotte Investigational Review Board.
Patients
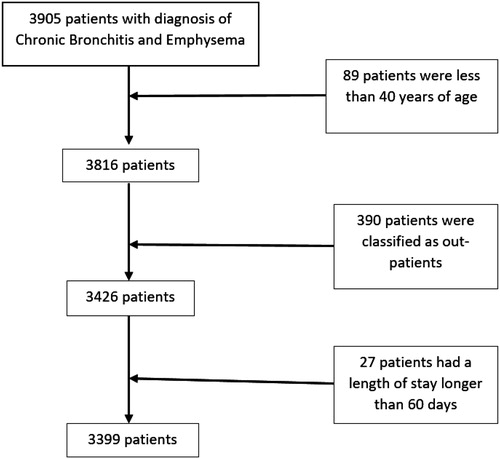
From the sample population, 3,905 patients with a primary diagnosis of chronic bronchitis and emphysema were identified. Patients younger than 40 years of age were then excluded, as patients with COPD are often diagnosed at a later age (Citation8–10). Patients classified as out-patients were excluded as well as patients with a length of stay of greater than 60 days. It was determined that patients with a length of stay greater than 60 days was greater than the reported average length of stay and should be excluded from the cohort (Citation11). One hypothesis is that longer length of stay could be due to iatrogenic complications related to the overall care of the patients.
We identified 3,399 patients (). Inclusion criteria was patients with at least 1 claim of COPD. COPD was classified into chronic bronchitis (ICD-10: J41), Unspecified chronic bronchitis (ICD-10: J42), and Emphysema (ICD-10: J43). Patients also had to be enrolled in the database in 2016. Patients were excluded if they had a secondary diagnosis of respiratory cancer (ICD-10: D02.4), cystic fibrosis (ICD-10: E84.9), or pulmonary tuberculosis (ICD-10:A15.0). Patients with any claim for Acute or Chronic Bronchitis (ICD-10: J40), other Chronic Bronchitis (ICD-10: J44), Asthma (ICD-10: J45), or Bronchiectasis (ICD-10: J47) were also excluded.
Statistical analysis
Descriptive statistics were used to report the cohort demographic data. Spearman’s rank correlation coefficient was used to determine the correlation between number of comorbidities and length of stay. The Elixhauser Comorbidity Index was used to identify common comorbidities (Citation12). Negative binomial regression (NBR) was used to evaluate the association between each comorbidity and overall length of stay. Incidence rate ratios (IRRs) indicated the increase in overall length of stay by co-morbid condition. All the statistical analysis were carried out using SAS 9.4 (SAS Institute, Inc., Cary, NC, USA).
Results
The eligible cohort comprised 3,399 patients with a primary diagnosis of COPD (). The cohort had a mean (SD) age of 68.41 (10.85) years. The cohort comprised 61% males and 83% were white. Patients in the cohort were admitted through the emergency department 56% of the time while 30% were considered elective. Of the patients in this cohort, 30% were discharged to home, 20% were discharged to a skilled nursing facility and 14% expired. 71% of the patients were Medicare patients ().
Table 1. Patient demographics.
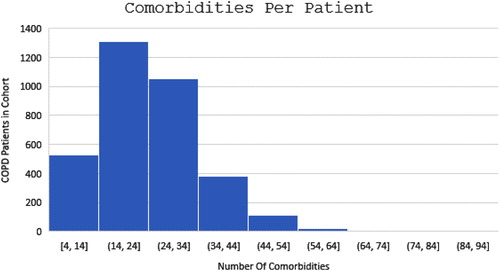
The average number of comorbidities was 24.83 with a standard deviation of 10.46 with an average length of stay of 11.64 days and standard deviation of 9.40 days. The authors looked at a distribution of number of comorbidities per patient. The largest number of patients in the cohort had between 14 and 24 co-morbid conditions with the next highest group having between 24 and 34. (). Spearman’s rank correlation coefficient showed r = .4596 (p < .0001). The authors determined that the number of comorbidities was associated with an increase in length of stay. When specific comorbidities are evaluated using negative binomial regression we see specific patterns related to certain comorbidities, such as CHF and complicated hypertension leading to an increase in length of stay (). We observed that patients with at least one comorbidity was associated with a 13% greater length of stay than not having a comorbidity (IRR = 1.13, 95% CI 1.11–1.15, p < 0.0001). Congestive heart failure (CHF) was associated with a 28% greater length of stay than not having CHF (IRR = 1.28, 95% CI 1.24–1.31, p < 0.0001). Fluid and electrolyte disorders were associated with a 157% greater length of stay than not having fluid and electrolyte disorders (IRR = 2.57, 95% CI 2.52–2.62, p < 0.0001). Cardiac arrhythmias were associated with a 40% greater length of stay than not having a cardiac arrhythmia (IRR = 1.40, 95% CI 1.37–1.44, p < 0.0001). Renal failure was associated with a 50% greater length of stay than not having renal failure (IRR = 1.50, 95% CI 1.45–1.55, p < 0.0001). Weight loss was associated with an 80% greater length of stay than not having weight loss (IRR = 1.80, 95% CI 1.76–1.85, p < 0.0001). Conversely, obesity was associated with a 39% greater length of stay than not being obese (IRR = 1.39, 95% CI 1.36–1.43, p < .0001). Additionally, depression was associated with a 21% greater length of stay than not having depression (IRR = 1.21, 95% CI 1.18–1.25, p < .0001). Not all comorbidities were found to cause an increase in length of stay. Uncomplicated diabetes was associated with a 13% lesser length of stay than not having uncomplicated diabetes (IRR=.87, 95% CI .82–.91, p<.0001). Also complicated diabetes was shown to not have a significant effect on length of stay. We hypothesize that the patients in our study may have been misclassified related to a diabetes diagnosis. lists additional comorbidities related to this cohort of COPD patients.
Table 2. Analysis of maximum likelihood parameter estimates.
Discussion
This retrospective database analysis sought to describe a cohort of patients with COPD, and to determine if the number of comorbidities affects overall length of stay. Additionally to determine if certain comorbidities lead to an increase in length of stay. The study showed that the number of comorbidities was associated with an increased length of stay. The results were consistent with studies related to the affects certain comorbidities in COPD patients have on length of stay (Citation2, Citation13, Citation14).
The findings of this study correspond with research that found CHF to be independently related with prolonged length of stay (Citation15). Diez et al. discussed common risk factors that are commonly seen in patients with COPD and CHF (Citation16). It has been reported that up to one third of COPD patients have been affected by CHF (Citation17). Tobacco use appears to be the common thread that links these two conditions (Citation16). Disorders of fluid, electrolyte, and acid–base balance were shown to be among the top ten reasons for readmissions in COPD patients (Citation18). Sievi et al. found that one third of COPD patients have altered cardiac repolarization which potential causes an increased risk of malignant ventricular arrhythmias (Citation19). A commonly seen cardiac arrhythmia in COPD patients is atrial fibrillation. Terzano et al. performed a retrospective cohort study on COPD patients in Italy (Citation20). They found that cardiovascular comorbidities and diabetes mellitus had the greatest impact on effecting length of stay (Citation20). A study in Poland assessed several factors to determine the relationship between certain comorbidities of COPD patients and duration of hospital stay (Citation21). These authors found that certain co-morbid conditions were great predictors of prolonged hospitalization (Citation21). One final study from Finland investigated the impact of comorbidities on the duration of stay for COPD patients (Citation22). The authors found that by identifying patients with multiple co-morbid conditions, a treatment regimen could be targeted at reducing days of care (Citation22). There is very limited research related to the incidence of renal failure in patients with COPD. Incalzi et al. found a prevalence of concealed chronic renal failure of 20.8% and overt chronic renal failure of 22.2% (Citation23). Other studies also found significantly worse renal function in patients with COPD (Citation24–26). Weight loss has been noted in between 25 and 40% of patients diagnosed with COPD (Citation27). Loss of fat-free mass also known as cachexia and skeletal muscle dysfunction (myopathy) have been reported as common comorbidities in COPD patients (Citation3). In a study that assessed the association between body mass index (BMI) and in-hospital outcomes, higher BMI was associated with increased risk of mortality and longer hospital stay (Citation28). Studies have found significantly higher depression symptoms in the patients with COPD (Citation29, Citation30). Our study did not show an association between diabetes and COPD related to length of stay. This is contradictory to several studies (Citation10, Citation31). One study showed a significant increase in type 2 diabetes mellitus in patients with moderate-to-severe COPD (Citation32). Cazzola et al. also described a link between COPD and type 2 diabetes mellitus (Citation33). Diabetes has also been associated with stage 3 and 4 COPD patients (Citation34).
Certain pathophysiologic links between COPD and comorbidities could help to also explain the results of the study. One such link could be the influence of chronic systemic inflammation and its relationship to COPD and cardiovascular disease (Citation5). Oxidative stress protease/antiprotease imbalance has been linked to systemic inflammation which could manifest comorbidities in patients with COPD (Citation14). COPD patients are thought to be in a constant prothrombotic state (Citation29). This makes these patients more susceptible to comorbidities such as venothromboembolic disease and acute coronary syndromes (Citation14). Airway and systemic inflammation along with lung hyperinflation with endothelial dysfunction and oxidative stress can lead to ischemic heart disease, stroke, heart failure, hypertension, diabetes, muscle weakness and osteoporotic fractures, and depression (Citation14). COPD patients often have chronic hypoxemia and hypercapnia (Citation1). Renal function can be directly affected by these conditions (Citation35). There is a well-established link between COPD and certain co-morbid conditions. This aids researchers in gaining a better understanding into why certain comorbidities are more prevalent in COPD patients. Identifying this link can help explain certain patterns in length of stay seen in this study.
The prevalence of COPD has been widely documented in the literature (Citation1, Citation2, Citation36). Patients with lower socioeconomic status have been identified as having a higher prevalence (Citation36). There are several factors that make this patient population more susceptible, such as increased tobacco use, increased exposure to pollutants, and decreased accessibility to healthcare (Citation36). Additionally, poorer medication adherence is positively correlated with increased readmission rates (Citation37). These factors are further complicated by a relatively high presence of comorbidities among COPD patients.
Conclusion
This study showed that the number of comorbidities had a positive correlation to length of stay and specifically that having certain comorbidities leads to an increase in length of stay. This information is important to gaining a further understanding of factors that cause patients with COPD to stay in the hospital longer. Further research should look at how the number of comorbidities affects the overall cost. Mannino et al. used a similar healthcare database to assess the overall economic burden of COPD patients when certain comorbidities were identified (Citation9). As healthcare continues to change it is important to find ways to lower the cost of care in patients diagnosed with COPD.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.
Statement of IRB approval
This study was reviewed by the University of North Carolina at Charlotte Institutional Review Board and deemed as exempt from regulation.
Additional information
Notes on contributors
Lanny S. Inabnit
LI was the primary author and conducted statistical analysis and interpretation. CB and CR provided assistance with statistical analysis, interpretation and proofreading of the manuscript.
Christopher Blanchette
LI was the primary author and conducted statistical analysis and interpretation. CB and CR provided assistance with statistical analysis, interpretation and proofreading of the manuscript.
Cynthiya Ruban
LI was the primary author and conducted statistical analysis and interpretation. CB and CR provided assistance with statistical analysis, interpretation and proofreading of the manuscript.
References
- Hess DR, MacIntyre NR, Galvin WF, Mishoe SC. Respiratory care: principles and practices. 3rd ed. Burlington (MA): Jones and Bartlett Publishing; 2016.
- Dalal AA. Direct costs of chronic obstructive pulmonary disease among managed care patients. Int J Chron Obstr Pulm Dis. 2010;5:341–349. doi:10.2147/COPD.513771.
- Hillas G, Perlikos F, Tsiligianni I, Tzanakis N. Managing comorbidities in COPD. Int J Chron Pulmon Dis. 2015;10:95–109. doi:10.2147/COPD.s54473.
- Jorgensen NR, Schwarz P, Holme I, Henriksen BM, Petersen LJ, Backer V. The prevalence of osteoporosis in patients with chronic obstructive pulmonary disease: a cross sectional study. Respir Med. 2007;101:177–185. doi:10.1016/j.med.2006.03.029.
- Fabbri LM, Rabe KF. From COPD to chronic systemic inflammatory syndrome? Lancet 2007;370(9589):797–799. doi:10.1016/S0140-6776(07)61383-X.
- Westerik JAM, Metting EI, van Boven JFM, Tiersma W, Kocks JWH, Schermer TR. Association between chronic comorbidity and exacerbation risk in primary care patients with COPD. Respir Res. 2017;18(31):1–17. doi:10.1186/s12931-017-0412-2.
- PremierConnect Research [Internet]. 2018. [cited 2018 May 10]. Available from: https://www.premierinc.com/transforming-healthcare/healthcareperformance improvement/premier-applied-sciences/premierconnect-research/.
- Collison KA, Patel P, Preece AF, Stanford RH, Sharma RK, Feldman G. A randomized clinical trial comparing the ELLIPTA and handihaler dry powder inhalers in patients with COPD: inhaler-specific attributes and overall patient preference. COPD 2018;15(1):46–50. doi:10.1080/15412555.2017.1400000.
- Mannino DM, Higuchi K, Yu TC, Zhou H, Li Y, Tian H, Suh K. Economic burden of COPD in the presence of comorbidities. Chest 2015;148(1):138–150. doi:10.1378/chest.14-2434.
- Schnell K, Weiss CO, Lee T, Krishnan JA, Leff B, Wolff JL, Boyd C. The prevalence of conditions in patients with physician-diagnosed COPD: a cross-sectional study using data from NHANES 1999-2008. BMC Pulm Med. 2012;12(26):1–9. Available from: http://www.biomedcentral.com/1471-2466/12/26.
- Madani Y, Saigal A, Sunny J, Morris L, Johns RH. Characterization of chronic obstructive pulmonary disease patients with a long length of stay: a retrospective observational cohort study. Turk Thorac J. 2017;18:119–124. doi:10.5152/Turk.
- Elixhauser A, Steiner C, Harris RD, Coffey CM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. Available from: https://insights.ovid.com/pubmed?pmid = 9431328.
- Kinnunen T, Saynajakangas O, Tuuponen T, Keistinen T. Impact of comorbidities on the duration of COPD patients’ hospital episodes. Respir Med. 2003;97:143–146. Available from: http://www.sciencedirect.com.
- Aryal S, Diaz-Guzman E, Mannino DM. Epidemiology of comorbidities in chronic obstructive pulmonary disease: clusters, phenotypes and outcomes. Ital J Med. 2012;6:276–284. doi:10.1016/j.itjm.2012.02.006.
- Wang Y, Stavem K, Dahl FA, Humerfelt S, Haugen T. Factors associated with a prolonged length of stay after acute exacerbation of chronic obstructive pulmonary disease (AECOPD). Int J Chron Obstruct Pulmon Dis. 2014;9:99–105. doi:10.2147/COPD.S51467.
- Diez JDM, Morgan JC, Garcia RJ. The association between COPD and heart failure: a review. Int J Chron Obstruct Pulmon Dis. 2013;8:305–312. doi:10.2147/COPD.S31236.
- Sanders-van Wijk S, van Empel V, Knackstedt C, LaRocca HPB. Heart failure and COPD: time to shift? Int J Cardiol. 2014;172(2):293–294. doi:10.1016/jijcard.2013.12.285.
- Vorhies JS, Wang Y, Herndon JH, Maloney WJ, Huddleston JI. Decreased length of stay after TKA is not associated with increased readmission rates in a national medicare sample. Clin Orthop Relat Res. 2012;470:166–171. doi:10.1007/s11999-011-1957-0.
- Sievi NA, Clarenbach CF, Camen G, Rossi VA, van Gestel AJR, Kohler M. High prevalence of altered cardiac repolarization in patients with COPD. BMC Pulm Med. 2014;14(55):1–8. doi:10.1186/1471-2466-14-55.
- Terzano C, Colamesta V, Unim B, Romani S, Meneghini A, Volpe G, La Torre G. Chronic obstructive pulmonary disease (COPD) exacerbation: impact of comorbidities on length and costs during hospitalization. Eur. Rev. Med Pharmaco Sci. 2017;21:3680–3689. Accessed from: https://www.europeanreview.org/article/13285.
- Nowinski A, Kaminski D, Korzybski D, Stoktosa A, Gorecka D. The impact of comorbidities on the length of hospital treatment in patients with chronic obstructive pulmonary disease. Pneumonol Alergol Pol. 2011;79(6):388–396. Available from: https://journals.viamedica.pl/advances_in_respiratory_medicine/article/view/27622.
- Rycroft CE, Heyes A, Lanza L, Becker K. Epidemiology of chronic obstructive pulmonary disease: a literature review. Int J Chron Pulmon Dis. 2012;7:457–494. doi:10.2147/COPD.S32330.
- Incalzi RA, Corsonello A, Pedone C, Battaglia S, Paglino G, Belli V. Chronic renal failure: a neglected comorbidity of COPD. Chest 2010;137(4):831–837. doi:10.1378/chest.09-1710.
- AbdelHalim HA, AbEINaga HH. Is renal impairment an anticipated COPD morbidity. Respir Care 2016;61(9):1201–1206. doi:10.4187/respcare.04516.
- Yoshizawa T, Okada K, Furuichi S, Ishiguro T, Yoshizawa A, Akahoshi T, Gon Y, Akashiba T, Hosokawa Y, Hashimoto S. Prevalence of chronic kidney diseases in patients with chronic obstructive pulmonary disease: assessment based on glomerular filtration rate estimated from creatinine and cystatin C levels. Int J Chron Obstruct Pulmon Dis. 2015;10:1283–1289. doi: 10.2147/COPD.580673.
- Barakat MF, McDonald HI, Collier TJ, Smeeth L, Nitsch D, Quint JK. Acute kidney disease in stable COPD and at exacerbation. Int J Chron Obstruct Pulmon Dis. 2015;10:2067–2077. doi:10.2147/COPD.588759.
- Itoh M, Tsuji T, Nemoto K, Nakamura H, Aoshiba K. Undernutrition in patients with COPD and its treatment. Nutrients 2013;5:1316–1335. doi:10.3390/nu5041316.
- Akinyemiju T, Meng Q, Vin-Raviv N. Association between body mass index and in-hospital outcomes: analysis of the nationwide inpatient database. Medicine 2016;95(28):1–8. doi:10.1097/MD.0000000000004189.
- Zhang MWB, Roger CM, Cheung MWL, Fu E, Mak A. Prevalence of depressive symptoms in patients with chronic obstructive pulmonary disease: a systematic review, meta-analysis and meta-regression. Gen Hosp Psychiatry 2011;33(3):217–223. doi: 10.1016/j.genhosppsych.2011.03.009.
- Norwood R. Prevalence and impact of depression in chronic obstructive pulmonary disease patients. Curr Opin Pulm Med. 2006;12(2):113–117. doi:10.1097/01.mcp.00002086.50231.c6.
- Martinez CH, Mannino DM, Curtis JL, Han MK, Diaz AA. Socioeconomic characteristics are major contributors to ethnic differences in health status in obstructive lung disease: an analysis of the national health and nutrition examination survey 2007-2010. Chest 2015;148(1):151–158. doi:10.1378/chest.14-1814.
- Rogliani P, Calzetta L, Segreti A, Barrile A, Cazzola M. Diabetes mellitus among outpatients with COPD attending a university hospital. Acta Diabetol. 2014;51(6):933. doi:10.1007/s00592-014-0584-0.
- Cazzola M, Rogliani P, Calzetta L, Lauro D, Page C, Matera MG. Targeting mechanisms linking COPD to type 2 diabetes mellitus. Trends Pharmacol Sci. 2017;38(10):940–951. doi:10.1016/j.tips.2017.07.003.
- Mannino DM, Thorn D, Swenson A, Holguin F. Prevalence and outcomes of diabetes, hypertension and cardiovascular disease in COPD. Eur Respir J. 2008;32:962–969. doi:10.1183/09031936.00012408.
- Mapel D. Renal and hepatobiliary dysfunction in chronic obstructive pulmonary disease. Curr Opin Pulm Med. 2014;20(2):186–193. doi:10.1097/MCP.0000000000000024.
- Eisner MD, Blanc PD, Omachi TA, Yelin EH, Sidney S, Katz PP, Ackerson LM, Sanchez G, Tolstykh I, Iribarren C. Socioeconomic status. race, and COPD health outcomes. J Epidemiol Community Health 2011;65(1):26–34. doi:10.1136/jech.2009.089722.
- McCullough AR, Ryan C, Macindoe C, Yii N, Bradley JM, O’Neill B, Elborn JS, Hughes CM. Behavior change theory, content and delivery of interventions to enhance adherence in chronic respiratory disease: a systematic review. Respir Med. 2016;116:78–84. doi:10.1016/j.rmed.0016.05.021.