Abstract
Acute exacerbations of chronic obstructive pulmonary disease (COPD) are associated with significant mortality, morbidity and increased risk for further exacerbations. Therefore, appropriate measures for prevention of further exacerbations should be initiated before discharge. Unfortunately, this opportunity for treatment review and change in disease course is often missed. We designed a decision support tool to automatically generate discharge recommendations for COPD patients based on the Global Initiative for Chronic Obstructive Lung Disease (GOLD) report. A pre- and post-intervention study was conducted including data from 24 months before and 18 months after the implementation of the tool. The rate of adherence of the discharge recommendations to the report was measured. Overall, 536 patients were included in the pre-intervention cohort and 367 in the intervention cohort. Demographic and clinical features were similar between the two groups. After introduction of the tool, the percentage of patients discharged with long-acting medications increased from 42% to 84%, recommendations for smoking cessation increased from 32% to 91%, for vaccination from 13% to 92%, and for follow-up visit in a pulmonology clinic from 72% to 98%. Of the patients given prescriptions for long-acting bronchodilators, 54% purchased these after discharge versus 20% of the patients without such prescriptions. Decision-support tools can significantly improve adherence to guidelines among patients discharged after hospitalization due to Acute Exacerbation of Chronic Obstructive Pulmonary Disease (AECOPD) and potentially improve their clinical course.
Introduction
Chronic obstructive pulmonary disease (COPD) is estimated to affect 1 in 10 persons worldwide and it is the third leading cause of death in the United States (Citation1). Acute exacerbations of COPD (AECOPD) accounts for 3.5% of hospital admissions and nearly 10% of unplanned hospitalizations (Citation2, Citation3). Acute exacerbations are key events in COPD. They are not only associated with significant mortality rates, but also accelerate the decline in lung function, reduce quality of life and activity tolerance, and increase the risk of further exacerbations (Citation4, Citation5). Therefore, after a hospitalization due to AECOPD, appropriate measures for prevention of further exacerbations should be initiated. Interventions shown to have significant effect on exacerbations frequency include proper usage of long-acting bronchodilators and inhaled corticosteroids (ICS), smoking cessation, early pulmonologist follow-up, and influenza and pneumococcal vaccinations (Citation6). All these issues need to be addressed before discharge in order to improve patients’ care and reducing readmission rates (Citation7, Citation8).
Numerous studies have shown a significant gap between up-to-date clinical evidence for best practices, as reflected by the clinical guidelines, and actual practice patterns (Citation9–11). In various studies, only 50% of patients discharged after AECOPD were prescribed maintenance bronchodilators or provided with smoking cessation counseling. Pneumococcal and Influenza vaccination rates were also low, ranging from 17% to 67% (Citation7, Citation12). Only 9–56% of patients had follow-up arrangements completed before discharge (Citation12–14). These low rates of adherence are likely the result of multiple factors, including: lack of familiarity with recent recommendations, inadequate training, tendency to address only urgent matters during hospitalizations and lack of time for discharge planning (Citation15). However, implementation of the evidence based guidelines can lead to substantial clinical benefit; thus, these barriers must be addressed (Citation16).
In other fields of medicine, strong evidence supports the use of clinical decision support (CDS) tools to achieve improvements in care delivery (Citation17). Examples include the use of CDS for screening of patients at risk for developing disease, medication management and quality improvement in conditions such as diabetes, venous thromboembolism, mental health and asthma (Citation14, Citation17–20). However, scant evidence exists on CDS use for hospitalized patients with COPD (Citation21). In a small study which included only 44 patients, Parikh et al. (Citation5) demonstrated that incorporation of automated CDS tool into hospital’s medical record system, significantly improved the care for COPD exacerbations.
Relying on the success of integrating CDS systems into the patient care workflow in other domains, we designed a CDS tool which provides physicians with point-of-care recommendations when discharging patients with AECOPD. The tool was based on the Global Initiative for Chronic Obstructive Lung Disease (GOLD) report and integrated into the hospital’s Electronic Health Record (EHR) system. We conducted a pragmatic study to evaluate the effect of this tool on rates of adherence to published guidelines among patients discharged after hospitalization due to AECOPD.
Methods
Study design and settings
The study was conducted in the Rambam Health Care Campus (RHCC) in Haifa, Israel. RHCC is a 1000-bed academic hospital serving over 2 million residents in northern Israel with 80,000–90,000 hospitalizations annually. RHCC is supported by a comprehensive integrated EHR system called Prometheus, that was developed in-house.
A CDS system based on the GOLD 2016 report was designed to improve the adherence of clinicians discharging patients (Citation22). In concordance with this report, we decided to address the following issues, proved to reduce the frequency of exacerbations:
Recommendation (and prescription) for long-term usage of long-acting bronchodilators—long-acting beta agonists (LABAs), and/or long-acting muscarinic receptor antagonists (LAMAs), with or without ICS.
Recommendation for follow-up visit with a pulmonologist within 30 days of discharge.
Smoking cessation.
Annual influenza and pneumococcal vaccination.
Pulmonary rehabilitation was not addressed by our CDS tool as such recommendations can only be given by the patient’s pulmonologist physician in our care-system.
During the study period, 2017 and 2018 GOLD reports were published. In this report, there were no significant changes that necessitated a change in these parameters (Citation8).
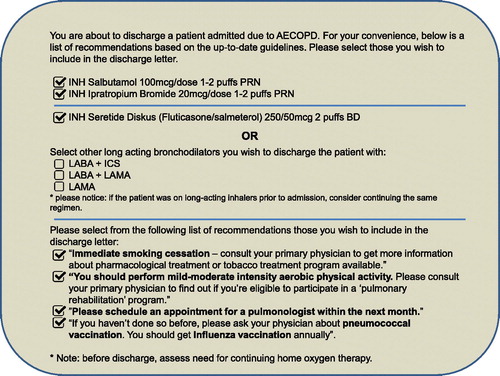
The CDS tool implemented within the EHR was placed in the patient care workflow after confirmation of the AECOPD diagnosis and before completion of discharge medications and recommendations. The tool was launched automatically in the navigator menu of the EHR. The landing window listed all commercially available long-acting inhalers (ICS, LABA and LAMA) alongside their available dosages, as well as built-in recommendations for smoking cessation, influenza and pneumococcal vaccinations and for a pulmonologist follow up (). Patient care decisions were made at the discretion of the treating physicians who could opt-out from any or all of the recommendations given by the tool, as well as modify the recommendations before signing the discharge note. All discharge letters were discussed with the patient and his caregivers before discharge and were electronically transferred to the patients’ primary care physicians.
Figure 1. The above EHR-based CDS tool was placed in the patient care workflow after confirmation of the AECOPD diagnosis and before completion of discharge medications and recommendations. The tool is launched automatically in the navigator menu. Once the physician selects one of the long-acting bronchodilators shown above then a menu with all of the relevant inhalers for that specific category is shown (e.g. “INH. Tiotropium bromide 2.5 mcg/puff 2-puffs OD”). The recommendations selected by the physician will automatically convert into prescriptions and written recommendations that will appear in the discharge letter.
A pre- and post-intervention study was conducted, including data from before and after the implementation of the CDS tool. The pre-intervention time period included 24 months between 1 Jan 2015 and 31 Dec 2016, and the post-intervention time period included 18 months between 10 Jan 2017 and 4 Jul 2018. The rate of adherence to the discharge recommendations given to patients with AECOPD was measured.
Study population
The study population included patients 18 years or older with a primary discharge diagnosis of AECOPD (ICD-9 491.21) or COPD (ICD-9 496) as recorded in the EHR. Excluded from the study were patients that left against medical advice or patients that died during their hospitalizations. Patients with tracheostomy were also excluded as this prevents them from using majority of long-acting inhalers. Patients with significant cognitive impairment preventing them from using inhalers or continuing ambulatory follow-up were also excluded as well as those suffering from advanced-stage oncologic disease and receiving merely palliative care. These parameters were based on the clinical notes of the discharging physician. For patients with multiple encounters for AECOPD during the study time period, only their first encounter was included in the analysis.
Data collection
The electronic charts of all hospitalizations for AECOPD were retrieved from the hospital’s EHR system. These were manually reviewed by the researchers to ensure the adequacy of the diagnosis, for the existence of any exclusion criteria, and to extract the following demographic and clinical features: age (in years), sex (male or female), pCO2 level (mmHg) at admission and before discharge, and all drugs taken at home prior to admission. Charlson index was used to assess co-morbidity burden.
Medical charts from the pre-intervention phase were reviewed retrospectively and charts from the intervention phase were reviewed prospectively. During the intervention phase, in addition to the information collected from the hospital EHR system, we also obtained information from the patient’s Health Maintenance Organization (HMO) database. This included outpatient information such as the fulfillment of prescribed medications in HMO pharmacies. The HMO database was queried 60 days after discharge and thus included information available within this period.
Statistical analysis
Baseline characteristics were summarized using descriptive statistics. The Kolmogorov–Smirnov test was used to examine significant deviations from the normal distribution for continuous variables. Student’s t test for independent samples was used to compare means of variables with normal distribution, and Mann–Whitney U test was used for variables that deviated from the normal distribution. Chi-squared test and Fisher exact test were used to analyze differences between dichotomous variables, depending on the sample size. p < 0.05 was considered statistically significant.
Data analysis were conducted with Statistical Package for the Social Sciences, version 23.0 (SPSS, Chicago, IL) and Microsoft Excel version 14.0 (Microsoft Corporation, Redmond, WA, USA).
Ethical aspects
The RHCC Institutional Review Board approved the study (approval number RMB-0430-16) and waived informed consent.
Results
During the pre-intervention phase, 577 patients were discharged after hospitalization due to AECOPD. Forty-one patients were excluded due to severe cognitive impairment (n = 20), advanced cancer (n = 14) and tracheostomy state (n = 7). Overall, 536 patients (92.9%) were included in the study and their medical records were reviewed.
After CDS implementation, 408 patients were screened, of which 41 patients were excluded due to severe cognitive impairment (n = 16), advanced cancer (n = 18) and tracheostomy state (n = 4), and three patients left against medical advice without getting a discharge letter. Overall, 367 patients (89.95%) met the inclusion criteria during the intervention phase.
The pre- and post-intervention patients groups did not differ in age (median age of 69.0 versus 69.95 years, p = 0.13), comorbidities (median Charlson index of 6.0 in both groups, p = 0.57), length of stay and level of pCO2 on admission (median of 4 days and 57.0 mmHg, respectively). More males were enrolled during the intervention phase (67.85 versus 60.82%, p = 0.037) and significantly more patients were using long-acting bronchodilators before admission in the intervention group (53.95% versus 36.75%, p < 0.001). The demographic and clinical characteristics of the entire cohort are presented in .
Table 1. Baseline characteristics of hospital admissions for AECOPD, before and after the integration of the CDS tool into the EHR system.
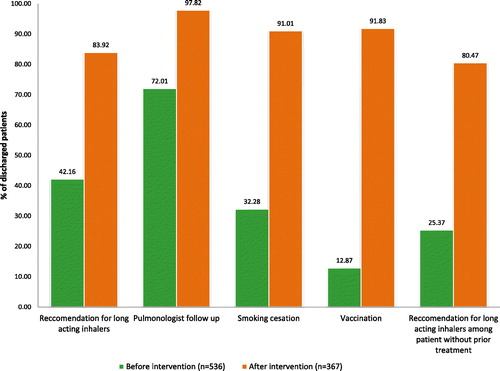
During the pre-intervention phase, only 42.16% of patients (n = 226) were discharged with recommendations for any long-acting medication. Moreover, of the 339 patients who presented without any long-acting inhaler treatment, only 25.37% (n = 86) were discharged with recommendations for such treatment. Recommendations for a follow-up visit in a pulmonology clinic were given in 72% (n = 386) of visits. Smoking cessation and vaccination against influenza and pneumococci were recommended in 32.28 and 12.87%, respectively.
After integration of the CDS tool, 83.92% (n = 308) of all patients and 80.47% (n = 136) of patients without prior treatment were discharged with prescription for long-acting bronchodilators. Follow-up visit in a pulmonology clinic was recommended in 97.82% (n = 359) of cases. Smoking cessation and appropriate vaccination were recommended in 91.01% (n = 334) and 91.83% (n = 337), respectively. Changes in the adherence to guidelines at discharge before and after the implementation of the CDS tool are shown in .
Figure 2. Changes in adherence to guideline-based discharge recommendations before and after implementation of the CDS tool. All the differences are statistically significant p < 0.001.
Information about fulfillment of the discharge-prescriptions at HMO pharmacies was available only in the CDS tool group. Among 136 patients prescribed long-acting bronchodilators and without such treatment prior to their hospitalization, information about prescription cashing was available for 117 of them (86%). Of these patients, 63 (54%) obtained the inhalers within 60 days. Among the 33 patients discharged without prescription for long-acting bronchodilators, information about medications supply at HMO pharmacies was available for 29 (87.87%). Only six (20.67%) of these patients purchased long-acting bronchodilators within 60 days. The differences between these two groups were statistically significant (p = 0.003).
Other post-discharge outcomes were not as accessible for assessment as the pharmaceutical outcomes. Records of post-discharge pulmonologist follow-up were available for 323/367 of the visits (88%). Of the 316 subjects with a recommendation for a pulmonologist follow-up and post-discharge data, 117 (37%) did see a pulmonologist within 60 days of discharge. As only 2.2% (n = 8) were discharged without these recommendations, we did not have statistical power to study the impact of these recommendation on the actual chances that the patient would be seen by a pulmonologist after discharge. No post-discharge information was available for the vaccinations and smoking-cessation outcomes.
Discussion
Hospitalizations due to AECOPD are not only associated with a significant acceleration of the disease course but also serve as an opportunity for intervention (Citation4, Citation5). Unfortunately this opportunity is often missed and majority of patients do not get appropriate recommendations upon discharge (Citation7, Citation12–14, Citation23, Citation24). This was also the case at RHCC in 2014, as seen in a prior study published by our group (Citation12). As a result, an educational campaign was undertaken by the pulmonary division during 2015 to 2016. Nonetheless, as seen in the current paper, these efforts did not have a significant effect on the discharge recommendations, and compliance with the guidelines remained low.
In this pragmatic “real-world” trial, we found that implementation of an EHR integrated CDS system significantly improved the quality of recommendations given at discharge to patients hospitalized due to AECOPD. This study shows how such interventions can improve physician decision making at the point of care and improve patients care. We also provide a preliminary analysis of the effect of discharge recommendations on actions taken by the patient after discharge.
We believe that the success of this tool may be attributed to several distinct features: (A) it is user friendly—it is not a burden for the clinician to use this tool, rather it saves time by automatically completing the list of discharge-recommendations required for COPD patients. (B) It uses well-validated evidence-based guidelines. (C) Seamless integration into the EHR makes it easy to use and enables it to give the right information, at the right time, to the right person. (D) Reduces variability—clinicians are often distracted, work in a stressful environment, and overwhelmed by information. This tool reduced variability and overcomes human-errors by providing the clinician with a list of predefined instructions.
An expanding body of literature states that providing clinicians with access to automated CDS tools can improve quality of care and patient safety and reduce costs. Such tools were successfully evaluated in treatment of patients hospitalized due to pneumonia, gastrointestinal bleeding, heart failure and sepsis (Citation5). Parikh et al. showed that incorporation of COPD module, a simplified evidence-based care bundle, into hospital’s EHR, lead to significant improvement in in-hospital AECOPD care, reduced the length of hospital stay and readmission rate (Citation5).
Although our study was not powered to assess the effect of the CDS tool on clinical outcome, previously published trials have shown that prompt initiation of long-acting bronchodilators after hospitalization due to AECOPD is associated with better outcomes. For instance, Dalal et al. showed that for every 30-day delay in long-acting bronchodilators initiation, the risk of a COPD-related exacerbation requiring hospitalization or an ED visit increased by 9% (Citation25). Blee et al. showed that providing patients with long-acting bronchodilators at discharge was associated with reduced rates of 30 and 60 days hospital readmissions (Citation26). Casas-Mendez et al. showed that discharge with multiple inhalers was associated with a seven times reduction in 90-days mortality (Citation27). Early post-discharge follow-up visit with pulmonologist was also shown to reduce readmissions (Citation12–14).
The rates of prescription fulfillment in our study were relatively low. Only 54% of the patients with a prescription for long-acting bronchodilators bought these medications within 60 days of discharge. Nonetheless, these numbers are concordant with previously published rates of COPD patients’ adherence to the prescribed regimens (Citation16). Furthermore, when these medications were not prescribed at discharge, only 20% of patients procured these inhalers. Such low rates of treatment initiation at the outpatient setting can be explained by lack of knowledge of primary-care physicians or by low compliance of patients who do not continue outpatient follow up. These findings emphasize that hospital discharge is an important opportunity to improve the treatment of COPD patients and potentially change disease course. Also, while we could not measure the effect of the written recommendations on pulmonologist follow-up in our study, a previous study from Israel have shown that 49% (80/164) of patients with such recommendations saw a pulmonologist after discharge versus only 19% (6/31) without recommendations (Citation14).
Our study has several limitations. First, this is a single-center study with all the limitations that such a design holds. Specifically, the baseline rate of compliance with guidelines may not be applicable to other sites. That being said, our literature review has shown that this problem of deviation from guidelines is not unique to RHCC. In addition, other sites might find the suggested solution useful in other domains of care. Second, patients were included in the study according to the clinical diagnosis given by the discharging physician and prior pulmonary function testing results were not required for inclusion. Nonetheless, once a diagnosis of AECOPD was made, rather rightfully so or not, the guidelines should have been followed and the patient should have received the right discharge recommendations. Third, adherence to the GOLD report was measured only by the presence or lack-of recommendations in the written discharge letter, patient understanding of these recommendations was not measured. Not enough can be said on the importance of proper patient education (Citation28–30), the need to address psycho-social factors (Citation28, Citation31), and the need for confirmation of care-continuity post-discharge (Citation28, Citation32, Citation33). Yet, it is important to note that each discharge letter was electronically transferred to the patient’s primary care physician. Also, the discharging physician goes over these recommendations with the patient before discharge and answer any questions that may arise. Lastly, significantly more patients were using long-acting bronchodilators before admission in the intervention group than in the pre-intervention group. This could reflect efforts done at the outpatient setting to increase compliance with existing guidelines. Nonetheless, this fact does not undermine our findings that many more patients were discharged with the right recommendations after the introduction of the CDS tool (80.47% versus 25.37%) and that patients discharged with these recommendations were much more likely to get long-acting bronchodilators within 60 days from discharge than patients without such recommendations (54% versus 20%).
Conclusions
A simple and inexpensive CDS tool, integrated into the EHR system, can significantly improve adherence to published guidelines among patients discharged after hospitalization due to AECOPD and potentially improve the clinical course of this population. Furthermore, the use of CDS systems which brings validated tools to the patient bedside could be expanded beyond COPD and improve care and resource use for many other clinical conditions.
Role of sponsors
The sponsor had no role in the design of the study, the collection and analysis of the data, or the preparation of the manuscript.
Declaration of interest
Danny Epstein, Yuval Barak-Corren, Yoni Isenberg and Gidon Berger declare that they have no conflict of interest.
Acknowledgments
D.E. had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis, including and especially any adverse effects. D.E., Y.B.C., Y.I. and G.B. contributed substantially to the study design, data analysis and interpretation, and the writing of the manuscript.
Additional information
Funding
References
- Shah T, Press VG, Huisingh-Scheetz M, et al. COPD readmissions: addressing COPD in the era of value-based healthcare. Chest. 2016;150(4):916–926. doi: 10.1016/j.chest.2016.05.002.
- Chalder MJE, Wright CL, Morton KJP, et al. Study protocol for an evaluation of the effectiveness of “care bundles” as a means of improving hospital care and reducing hospital readmission for patients with chronic obstructive pulmonary disease (COPD). BMC Pulm Med. 2016;16:35.
- Shah T, Churpek MM, Perraillon MC, et al. Understanding why patients with COPD get readmitted: a large national study to delineate the medicare population for the readmissions penalty expansion. Chest. 2015;147(5):1219–1226. doi: 10.1378/chest.14-2181.
- Jurado Gamez B, Feu Collado N, Jurado Garcia JC, et al. Home intervention and predictor variables for rehospitalization in chronic obstructive pulmonary disease exacerbations. Arch Bronconeumol. 2013;49(1):10–14. doi: 10.1016/j.arbr.2012.11.002.
- Parikh R, Shah TG, Tandon R. COPD exacerbation care bundle improves standard of care, length of stay, and readmission rates. Int J Chron Obstruct Pulmon Dis. 2016;11(1):577–583. doi: 10.2147/COPD.S100401.
- Mirza S, Clay RD, Koslow MA, et al. COPD guidelines: a review of the 2018 GOLD report. Mayo Clin Proc. 2018;93(10):1488–1502. doi: 10.1016/j.mayocp.2018.05.026.
- Yip NH, Yuen G, Lazar EJ, et al. Analysis of hospitalizations for COPD exacerbation: opportunities for improving care. COPD. 2010;7(2):85–92. doi: 10.3109/15412551003631683.
- Global Initiative for Chronic Obstructive Lung Disease Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (2018). 2018, available from www.goldcopd.org, published in Fontana, WI, USA.
- Price D, West D, Brusselle G, et al. Management of COPD in the UK primary-care setting: an analysis of real-life prescribing patterns. Int J Chron Obstruct Pulm Dis. 2014;9:889.
- Palmiotti GA, Lacedonia D, Liotino V, et al. Adherence to GOLD guidelines in real-life COPD management in the Puglia region of Italy. Int J Chron Obstruct Pulm Dis. 2018;13:2455–2462. doi: 10.2147/COPD.S157779.
- Chan KK, Ko F, Chan HS, et al. Adherence to a COPD treatment guideline among patients in Hong Kong. Int J Chron Obstruct Pulm Dis. 2017;12:3371–3379. doi: 10.2147/COPD.S147070.
- Nasser R, Epstein D, Azzam R, et al. The effect of clinical and physiological instability at discharge following hospitalization for acute exacerbation of COPD on early readmission: a cohort study. Chest. 2017;151(5):1192–1194. doi: 10.1016/j.chest.2017.01.028.
- Sharma G, Kuo Y-F, Freeman JL, et al. Outpatient follow-up visit and 30-day emergency department visit and readmission in patients hospitalized for chronic obstructive pulmonary disease. Arch Intern Med. 2010;170(18):1664–1670.
- Gavish R, Levy A, Dekel OK, et al. The association between hospital readmission and pulmonologist follow-up visits in patients with COPD. Chest. 2015;148(2):375–381. doi: 10.1378/chest.14-1453.
- Perez X, Wisnivesky JP, Lurslurchachai L, et al. Barriers to adherence to COPD guidelines among primary care providers. Respir Med. 2012;106(3):374–381. doi: 10.1016/j.rmed.2011.09.010.
- Restrepo RD, Alvarez MT, Wittnebel LD, et al. Medication adherence issues in patients treated for COPD. Int J Chron Obstruct Pulm Dis. 2008;3(3):371–384. doi: 10.2147/COPD.S3036.
- Jones SS, Rudin RS, Perry T, et al. Health information technology: an updated systematic review with a focus on meaningful use. Ann Intern Med. 2014;160(1):48–54. doi: 10.7326/M13-1531.
- Vinson DR, Ballard DW, Huang J, et al. Outpatient management of emergency department patients with acute pulmonary embolism: variation, patient characteristics, and outcomes. Ann Emerg Med. 2018;72(1):62–72.e3. doi: 10.1016/j.annemergmed.2017.10.022.
- Barak-Corren Y, Castro VM, Javitt S, et al. Predicting suicidal behavior from longitudinal electronic health records. Am J Psychiatry. 2016;174(2):154–162. doi: 10.1176/appi.ajp.2016.16010077.
- Barak-Corren Y, Fine AM, Reis BY. Early prediction model of patient hospitalization from the Pediatric Emergency Department. Pediatrics. 2017;139(5):e20162785. doi: 10.1542/peds.2016-2785.
- Fathima M, Peiris D, Naik-Panvelkar P, et al. Effectiveness of computerized clinical decision support systems for asthma and chronic obstructive pulmonary disease in primary care: a systematic review. BMC Pulm Med. 2014;14(1):189.
- Global Strategy for Diagnosis, Management, and Prevention of COPD – 2016 – Global Initiative for Chronic Obstructive Lung Disease – GOLD [Internet]. [cited 2018 Nov 30]. Available from: https://goldcopd.org/global-strategy-diagnosis-management-prevention-copd-2016/
- Amin AN, Bollu V, Stensland MD, et al. Treatment patterns for patients hospitalized with chronic obstructive pulmonary disease. Am J Health Syst Pharm. 2018;75(6):359–366. doi: 10.2146/ajhp160979.
- Lipari M, Smith AL, Kale-Pradhan PB, et al. Adherence to GOLD guidelines in the inpatient COPD population. J Pharm Pract. 2018;31(1):29–33. doi: 10.1177/0897190017696949.
- Dalal AA, Shah MB, D’Souza AO, et al. Outcomes associated with timing of maintenance treatment for COPD exacerbation. Am J Manag Care. 2012;18(9):e338–e345.
- Blee J, Roux RK, Gautreaux S, et al. Dispensing inhalers to patients with chronic obstructive pulmonary disease on hospital discharge: effects on prescription filling and readmission. Am J Health Syst Pharm. 2015;72(14):1204–1208. doi: 10.2146/ajhp140621.
- Casas-Mendez F, Abadías MJ, Yuguero O, et al. Treatment strategies after acute exacerbations of chronic obstructive pulmonary disease: impact on mortality. PloS One. 2018;13(12):e0208847. doi: 10.1371/journal.pone.0208847.
- Euceda G, Kong W-T, Kapoor A, et al. The effects of a comprehensive care management program on readmission rates after acute exacerbation of COPD at a community-based academic hospital. Chronic Obstr Pulm Dis Miami. 2018;5(3):185–192. doi: 10.15326/jcopdf.5.3.2017.0177.
- Conley P, Kelechi TJ, Nemeth LS, et al. Chronic obstructive pulmonary disease discharge education and quality of life evaluation: a feasibility study. Res Theory Nurs Pract. 2018;32(3):328–348. doi: 10.1891/1541-6577.32.3.328.
- Gómez-Angelats E, Sánchez C. Care bundles after discharging patients with chronic obstructive pulmonary disease exacerbation from the Emergency Department. Med Sci Basel Switz. 2018;6(3):63.
- Ospina MB, Michas M, Deuchar L, et al. Development of a patient-centred, evidence-based and consensus-based discharge care bundle for patients with acute exacerbation of chronic obstructive pulmonary disease. BMJ Open Respir Res. 2018;5(1):e000265.
- Aboumatar H, Naqibuddin M, Chung S, et al. Effect of a program combining transitional care and long-term self-management support on outcomes of hospitalized patients with chronic obstructive pulmonary disease: a randomized clinical trial. JAMA. 2018;320(22):2335–2343. doi: 10.1001/jama.2018.17933.
- Swanson JO, Vogt V, Sundmacher L, et al. Continuity of care and its effect on readmissions for COPD patients: a comparative study of Norway and Germany. Health Policy Amst Neth. 2018;122(7):737–745. doi: 10.1016/j.healthpol.2018.05.013.
