 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Patients with chronic obstructive pulmonary disease (COPD) often complain about difficulties in performing activities with their arms above shoulders height. These difficulties have been associated with increased cardiorespiratory demand and altered lung mechanics; however, musculoskeletal-related mechanisms may also contribute to constrain the mechanics of the upper body quadrant, increasing the effort to perform the activities. This exploratory research aimed to assess potential changes in the kinematic chain of arm elevation in patients with COPD. A secondary analysis from a cross-sectional exploratory case-control and prediction study was conducted in 15 patients with COPD (2 females) and 15 controls (8 females) matched for age and body mass index. The sagittal alignment and active range of motion (ROM) of the head, thoracic spine and shoulder complex were measured, using a computer software, in digital lateral photographs obtained in three different testing positions: arms at rest, arms at 90° of shoulder flexion and full arm elevation. From rest to full arm elevation, both groups moved from a more flexed to a less flexed or more upright thoracic spine position (∼7°, p < 0.001, 0.419 < <0.767). However, the COPD group showed significantly less shoulder flexion (∼12°, p = 0.007, d = 1.05) and thoracic spine extension (∼6°, p = 0.015,
= 0.139) ROM than the control group in the full arm elevation position. These findings suggest that this population may show changes in the kinematic chain of arm elevation that possibly contribute to arm movement-related complains and limited performance in their daily living.
Introduction
Patients with chronic obstructive pulmonary disease (COPD) often complain about difficulties (e.g., dyspnoea, excessive effort) in performing activities with their arms above shoulders height, including dressing, bathing, shopping and many household tasks (Citation1). Whilst part of these difficulties could be explained by decreased strength and endurance of the shoulder muscles, altered ventilatory mechanics and cardiorespiratory demand in this arm position (Citation2–4), the presence of musculoskeletal-related postural and mobility impairments of the upper body quadrant (e.g., forward shoulder positioning, spinal joint mobility) may restrain the mechanics of the upper extremity (Citation5–7). Arm motion, particularly above shoulders height, involves complex synchronous interactions of the axial skeleton to assist the movements of the arm (kinematic chain of arm elevation) (Citation8, Citation9). Without proper axial skeleton alignment and motion, abnormal scapular kinematics, reduced range of arm elevation motion, disadvantaged force-length relationships and increased activity of agonist and synergistic muscles can be expected (Citation5–7). These changes may contribute to premature fatigue, excessive load, effort and discomfort/pain sensations in the upper body quadrant, hindering the performance of daily activities with the upper extremities.
Recently, differences in the cervico(scapulo)thoracic region were found between patients with COPD and healthy controls, such as increased forward head positioning, abnormal shoulder girdle posture, increased sensitivity and tightness of the pectorals muscles, and associations between pulmonary (dys)function and such impairments (Citation10–13). It is possible that these differences contribute to reducing the movement repertoire of the upper body quadrant, further limiting the exercise capacity and intensifying discomfort/pain experience and disability related with upper limb movements in this patient population. However, to date, potential changes in the kinematic chain of arm elevation in patients with COPD have not been considered. The main purpose of this study was to compare the contribution of head, scapula and thoracic spine posture and mobility to the full range of motion (ROM) of arm elevation in patients with COPD (kinematic chain of arm elevation) and healthy individuals.
Methods
Design and participants
A secondary analysis from a cross-sectional case-control and prediction study (Citation12), approved by the Ethics Committee of the Central Regional Health Administration, Coimbra, Portugal (2011-02-28), aimed to compare postural alignment and mobility variables of the upper body quadrant in patients with COPD (n = 15) and controls (n = 15) was conducted. A summary of baseline characteristics of the two samples is provided in [for further, clinical characteristics are given in the primary analysis study (Citation12)]. Patients with COPD and healthy individuals were recruited in primary care settings and in the community, respectively, and were informed about the purposes and measurement procedures of the study. Written informed consent was obtained from all participants before data collection. Patients were included if they were: (Citation1) ≥18 years old; (Citation2) clinically stable, i.e., without a respiratory exacerbation over the past month; (Citation3) living in the community; (Citation4) able to walk independently without an assistive device; and (Citation5) able to follow simple instructions. Patients were excluded if they had (self-reported and/or during physical examination with the researchers): (Citation1) a thoracic or abdominal surgery in the previous year; (Citation2) a recent fracture of the ribs, clavicle or upper limb; (Citation3) recurrent sub-luxation of the shoulder [routinely “giving away” or “out of place” sensations with positive apprehension and relocation tests (Citation14, Citation4) scoliosis [lateral misalignment of the axial skeleton and/or asymmetric shoulder/pelvic girdles in standing on visual inspection with a positive Adam’s forward bend test (Citation15)]; or (Citation5) a previous mastectomy. They were also excluded if they presented other severe musculoskeletal (e.g., osteoporosis), systemic (e.g., rheumatoid arthritis), neurological or cardiovascular disorders that could interfere with the measurements, or cognitive impairment that could prevent them from understanding and following simple instructions. The eligibility criteria for the control group were the same as for the COPD group, with the addition of normal lung function.
Table 1. Demographics, anthropometrics and lung function of patients with COPD and healthy controls.
Measurements
Angular position and displacement of the head, arm and thoracic spine during active shoulder flexion
Angular position and displacement of the head, arm and thoracic spine were assessed using digital lateral photographs obtained in three different testing positions: arms at rest, arms parallel to the ground (90° of shoulder flexion) and full arm elevation (). To capture upper body quadrant positions, a 12-megapixel digital camera (Canon PowerShot SX200, Canon Inc., Tokyo) with a 5–60 mm lens was set on a tripod with a multi-angle bubble level, to allow levelling the camera in horizontal and vertical planes. The camera was positioned at 1.50 m from a cross marked on the ground. Participants were instructed to remove their upper body clothing and stand in the middle of the cross mark in the upright position and to remain with their arms alongside the trunk, feet slightly apart, body weight even on both feet and a horizontal gaze. One researcher attached five rigid plastic screw anchors (height, 40 mm; base, 10 mm) over the skin of the spinous processes of the 7th cervical and the 1st, 4th, 8th and 12th thoracic vertebrae using double-sided tape, and marked with a pencil the skin over the angle of the acromion of the scapula and the lateral epicondyle of the humerus. Photographs were then acquired from the participants’ right side. Before data collection, all participants practiced the testing protocol with one researcher. Reasons for selecting a priori the right lateral side for capturing the body/segments position on photographs were: (a) side-to-side asymmetries in shoulder ROM were not expected in these populations (negligible or clinically unimportant) (Citation13), (b) most people are right-handed (Citation16) (all our participants were right-handed), (c) screening for the presence/absence (exclusion/inclusion criterion) of potential structural body abnormalities that could distort data collection, analysis and interpretation (e.g., three-dimensional abnormalities of the spine, i.e., scoliosis) was assured, (d) to control potential errors in data acquisition (e.g., controlling parallax effect) having participants practicing moving within the sagittal plane of motion throughout the testing protocol and (e) to minimize possible space conflicts made available, by adding more cameras for data collection, in primary care and community settings.
Figure 1. Angular measurements performed with the arms at rest (left), arms parallel to the ground and at full shoulder flexion (right), showing the upper and lower thoracic spine angles (°) and shoulder ROM (°).
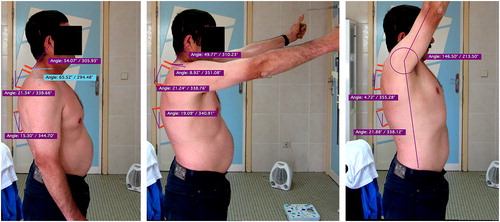
Sagittal alignment of the head, shoulder and thoracic spine at rest and during arm elevation (only thoracic spine) and ROM of full shoulder flexion were measured using a computer software (Osirix Imaging v5.0.2, Pixmeo SARL, Switzerland). Landmarks and angle definitions used to assess forward head posture, upper, lower and full thoracic spine (thoracic kyphosis) alignment and full shoulder flexion ROM were set according to previous studies (Citation17). The angles considered for analysis were those formed between the line joining the tip of two markers and the y-axis (vertical) as shown in . Positive angles represented rotations towards the positive y-axis and negative angles represented rotations towards the negative y-axis. Full thoracic spine angle (thoracic kyphosis) was the sum of upper and lower thoracic spine angles, in absolute values.
Previous analysis of repeated measurements performed on the same photographs revealed coefficients of variation ranging from 0.60% to 1.80% and 0.60% to 1.90%, with standard errors of measurement of 0.4° to 1.3° and 0.4° to 1.5°, for thoracic kyphosis measured in the neutral position and in full arm elevation, respectively (Citation18), indicating very good repeatability for conducting this investigation.
Alignment and positioning of the shoulder girdle
The position and motion of the shoulder girdle notably contributes to the amount and precision of shoulder/arm movements, particularly those performed above the shoulder’s height. The forward positioning/displacement of the scapula relative to the posterior thorax was assessed by: (a) the angle formed by the markers positioned at the 7th cervical spinous process and the posterolateral angle of the acromion (in digital photographs), using digital lateral photographs, and (b) the ratio between the distance from the sternal notch to the coracoid process and the distance from the thoracic spine to the posterolateral angle of the acromion (using a measuring tape), multiplied by 100. The latter measure is known as the scapula index (SI), which has shown correlations (Pearson’s r) up to 0.65 with scapular protraction, as measured by a 6 degrees of freedom motion tracking device (Citation19). SI was taken with the arms at rest immediately after acquiring a natural balanced upright posture according to a standardized protocol (Citation20) and before photographic capturing detailed in (a). Only the SI from the right side was considered for analysis.
Analysis
An independent samples t-test was used to compare the active ROM of full arm elevation in the sagittal plane (shoulder flexion) between groups. Three two-way analysis of variance (ANOVA) with interaction (group × arm position) were used to assess the effects (within-subject) of arm position on the (upper, lower and full) thoracic spine angles between groups. Post-hoc comparisons were performed using Bonferroni adjustment. Pearson’s correlation coefficient was used to assess the magnitude of association between head, thoracic spine and shoulder girdle measurements at rest and at full range of arm elevation. All data followed a normal distribution (Shapiro-Wilk test) and homoscedasticity was verified (Levene test). Significance level was set at 0.05.
Effect sizes, Cohen’s d and Eta2 partial (), were calculated to complement inferential statistics. Cohen’s d measures the size or the strength of the differences between two means. For d > 1 the effect is considered as very large; 1.0 ≥ d > 0.5 as large; 0.2 > d ≥ 0.5 as moderate; and d ≤ 0.2 as small. Eta2 partial measures the proportion of variation and error attributable to the factor excluding other factors from the total non-error variation. In other words, it describes the amount of variation of the dependent variables (thoracic spine angles) explained by the factors arm position and group. For values
> 0.5 the effect size is considered as very large; 0.5 ≥
> 0.25 as large; 0.25 ≥
< 0.05 as moderate; and
≤ 0.05 as small (Citation21). Analyses were conducted using SPSS v25.0 (IBM Corp., Armonk, NY) and G*Power v3.1.3 (G*Power Software Inc., Kiel, Germany).
Results
The active ROM of full shoulder flexion was significantly lower in the COPD group when compared to the control group (COPD = 136.7° ± 11.9° vs. control = 149.1° ± 11.6°; mean difference [95% CI] = 12.4° [21.2° – 3.6°], p = 0.007, d = 1.05). A significant main effect of arm position on the upper, lower and full thoracic spine angles was also found (p < 0.001, 0.419 < < 0.767). On average (95% CI), the upper and full thoracic spine (thoracic kyphosis) angles of both groups gradually decreased from rest to full shoulder flexion, 12.9° (10.5°–15.5°) and 7.1° (4.9°–9.3°) respectively, whereas lower thoracic spine angle increased 5.7° (3.1°–8.2°). The COPD group presented a greater magnitude in thoracic kyphosis (or less thoracic spine extension) throughout arm elevation than the control group (). No significant between-group differences were found when analysing the upper and lower thoracic spines separately (). However, in the full thoracic spine angle (or thoracic kyphosis), significant differences were found at full shoulder flexion (interaction effect of group × arm elevation, 5.9°, p = 0.015;
= 0.139; ). Considering that the full thoracic spine angle is the sum of the upper and lower thoracic spine angles, this finding is likely related to a more kyphotic (less vertical) lower thoracic spine in the COPD group ().
Table 2. Mean differences (±95% confidence intervals) in thoracic spine angles between patients with COPD and controls in the three arm elevation positions tested.
Correlations of the head, thoracic spine and shoulder girdle measurements with the arms resting on the side of the trunk and full range of arm motion are depicted in .
Table 3. Pearson's correlation coefficients (r) between head, thoracic spine and shoulder girdle measurements in the standing upright position and full range of arm elevation motion.
Discussion
This exploratory study showed that patients with COPD have reduced movement repertoire of the kinematic chain of arm elevation than their healthy counterparts: less active ROM of arm elevation and less extension of the overall thoracic spine at full arm elevation. These results suggest that differences in full arm elevation between groups may be related to less active mobility of the shoulder joint complex and reduced thoracic spine motion in patients with COPD.
Activities that require placing and moving the upper limb above shoulders height often involve complex interactions of the proximal body segments to assist in the movements of the arm. These interactions occur either to provide a stable postural basis for arm movement or to participate in the kinematic chain in a synergic way during the action of the arm (Citation6, Citation8, Citation9), and have been observed using different instrument, e.g., motion tracking devices (Citation6, Citation8, Citation9) and in different populations, e.g., healthy young adults (Citation6, Citation8, Citation9, Citation18). Results of this study support this rationale by showing a significant relationship between arm elevation and thoracic spine extension, irrespective of group differences.
The between-group differences in shoulder and thoracic spine mobility found in this study were related to the increased thoracic kyphosis angle (or less thoracic spine extension) in the COPD group. Increased thoracic kyphosis has been shown to alter shoulder girdle kinematics and reduce the capacity to actively and fully elevate the arms (Citation7). Changes in shoulder girdle kinematics included less upward rotation, retraction and posterior tilting of the scapula (or more downward rotation, protraction and anterior tilting), which can modify the operating length of the shoulder muscles and create a bony restraint between the acromion and the humerus thereby impairing arm elevation and predisposing the upper body quadrant to pain sensation/discomfort (Citation7). In this study, the relative contribution of each joint of the shoulder complex (glenohumeral, sternoclavicular, acromioclavicular and scapulothoracic) to full arm elevation was not assessed due to instrumental and methodological constraints; however, we partially measured the scapular orientation using clinical measures and found a moderate positive association between the scapula index and full range of arm elevation in the COPD group (r = 0.50). Dias et al. (Citation22) also found small yet significant differences in the resting scapulae position (greater scapular elevation, p < 0.05) of patients with COPD (n = 19; controls, n = 19) using gold standard instrumentation in motion capture and analysis (three-dimensional optical tracking technology). Scapular measurements other than the standing upright position with the arms resting aside the trunk were not acquired however, limiting our understanding of the scapular contributions during arm elevation tasks. Despite the different findings in scapular pattern compared with this study, which can be related to several reasons (e.g., different instrumentation, sample characteristics) it seems furthermore plausible the hypothesis of altered scapular and spinal motion in reducing arm elevation performance in the COPD population. Whether this is related greater dyspnoea and effort in performing upper limb activities (Citation2) can only be speculative at the time though. Associations between gains in shoulder ROM and lung function and dyspnoea perception after applying a stretching exercise to the pectorals muscles have been found (Citation13); yet, it is uncertain whether these are related to improvements in the mechanical efficiency of the shoulder region to perform or with modified sensations (e.g., increased tolerance in the perceptions of dyspnoea and/or stretch-induced pain) after the intervention. Future research in this field is therefore warranted, combining dynamic measuring systems (e.g., motion tracking devices, gas exchange analysis) with patient-reported measures (e.g., dyspnoea, pain) and other biomechanical/physical performance measures (e.g., scapulothoracic and shoulder muscles activity, power and endurance) during repetitive arm activities in different planes of orientation to uncover relationships between upper limb biomechanics, functional performance, cardiorespiratory demand and unpleasant sensations.
Patients with COPD presented less mobility of the thoracic spine (especially its lower segments) during arm elevation which might be explained by maladaptive structural and functional changes in the rib cage and the diaphragm muscle (part of this muscle inserts in the lower thoracic-superior lumbar vertebral bodies) that commonly occur in this population (Citation23). Such changes may stiffen the spine during arm elevation (Citation24–27) and contribute to adaptive shortening of the accessory respiratory muscles (e.g., pectoralis major and minor), furthermore restricting and increasing the exertion to elevate the arms (Citation13). Heneghan et al. (Citation11) reported recently also less thoracic spine mobility (∼15°, p = 0.01) in patients with COPD (n = 33) in comparison with age-matched controls (n = 55). Despite the interesting findings, such restriction in spinal mobility was observed in axial rotation, which is not the expected primary spinal motion occurring during bilateral arm elevation. Flexion/extension is (Citation6). In addition, spinal motion in Heneghan et al.’s study was captured with the arms resting aside the trunk. Alignment of the thoracic spine (thoracic spine angles) with the arms at rest or thoracic kyphosis, although significantly correlated with, do not clearly predict the spinal extension ROM during arm elevation as this and other studies have shown (Citation6, Citation17).
Exercises aiming to increase shoulder ROM are often included in pulmonary rehabilitation programmes to improve upper limb functioning (Citation28). Our findings support this practice, though thoracic spine extension exercises should also be considered because of their potential to improve arm elevation, which may reduce the muscular effort to perform activities above shoulders height (Citation29). Interventions directed at improving spinal mobility may have a dual-effect/interest by combining mechanical gains in upper body quadrant movement-related functions with improvements in respiratory function, particularly forced vital capacity. The latter is still disputed though, with conflicting results reported in the literature (Citation30–32). Assessing full range of arm elevation motion and associated spinal motion, as a supplement to the standard physical examination of the upper limbs (e.g., strength, exercise capacity) (Citation33), may help screening potential mobility impairments of the upper body quadrant, alerting the clinician to perform a more detailed examination and look for further mechanisms that may contribute to difficulties in performing activities above shoulders height in this population.
Some limitations should be acknowledged. Physical performance often differs between men and women. It could be expected that results have been influenced by the uneven distribution of sex in the two samples. However, previous studies have suggested that sex is not a factor of variation in posture and kinematics of the upper body quadrant (Citation34, Citation35). The analysis performed in this study supports these observations as no significant differences were found in shoulder and thoracic spine mobility between men and women (data not shown). Another limitation refers to the sample size. The number of participants examined in this study was relatively small given its exploratory nature and most of the patients had moderate COPD grade (GOLD 2, n = 11). Subgroup analysis according to the severity of the disease could not be performed but it could have strengthened our understanding of movement impairments of the upper extremity throughout COPD severity span. The design of future cross-sectional studies in this area should take this into account before proceeding to prospective studies. Finally, other biomechanical mechanisms related with mobility of the upper body quadrant, such as shoulder and cervicothoracic muscles activity, length, power and resistance were not assessed. Given their potential to influence mobility and performance of the upper body quadrant in a wide range of daily activities involving the upper limbs these should be included in future studies.
Conclusions
Patients with COPD showed reduced movement repertoire of the kinematic chain of arm elevation, less active full range of arm elevation and less extension the thoracic spine at full arm elevation, which may contribute to arm movement-related complains and limited performance in their daily living. Future studies should confirm these findings in a larger sample.
Authors’ contributions
N.M. and J.C. were responsible for the study conception and design. A.M. was involved in obtaining ethical approval, contacting the institutions and providing consulting during the conception and design of the research. N.M. and J.C. performed data collection and analysis. N.M. drafted the manuscript. All authors critically revised the paper for important intellectual content.
Disclosure statement
The authors report no conflict of interest.
References
- Marques A, Jácome C, Gabriel R, et al. Comprehensive ICF core set for obstructive pulmonary diseases: validation of the activities and participation component through the patient’s perspective. Disabil Rehabil. 2013;35(20):1686–1691. doi: 10.3109/09638288.2012.750691.
- Lima VP, Iamonti VC, Velloso M, et al. Physiological responses to arm activity in individuals with chronic obstructive pulmonary disease compared with healthy controls. J Cardiopulm Rehabil Prev. 2016;36(6):402–412. doi: 10.1097/HCR.0000000000000190.
- Robles P, Araujo T, Brooks D, et al. Does limb partitioning and positioning affect acute cardiorespiratory responses during strength exercises in patients with COPD? Respirology. 2017;22(7):1336–1342. doi: 10.1111/resp.13056.
- Nyberg A, Saey D, Martin M, et al. Cardiorespiratory and muscle oxygenation responses to low-load/high-repetition resistance exercises in COPD and healthy controls. J Appl Physiol. 2017;124(4):877–887. doi: 10.1152/japplphysiol.00447.2017.
- Ludewig PM, Cook TM. The effect of head position on scapular orientation and muscle activity during shoulder elevation. J Occup Rehabil. 1996;6(3):147–158. doi: 10.1007/BF02110752.
- Fayad F, Hanneton S, Lefevre-Colau M-M, et al. The trunk as a part of the kinematic chain for arm elevation in healthy subjects and in patients with frozen shoulder. Brain Res. 2008;1191(0):107–115. doi: 10.1016/j.brainres.2007.11.046.
- Kebaetse M, McClure P, Pratt NA. Thoracic position effect on shoulder range of motion, strength, and three-dimensional scapular kinematics. Arch Phys Med Rehabil. 1999;80(8):945–950.
- Theodoridis D, Ruston S. The effect of shoulder movements on thoracic spine 3D motion. Clin Biomech (Bristol, Avon). 2002;17(5):418–421.
- Crosbie J, Kilbreath SL, Hollmann L, et al. Scapulohumeral rhythm and associated spinal motion. Clin Biomech (Bristol, Avon). 2008;23(2):184–192. doi: 10.1016/j.clinbiomech.2007.09.012.
- Lee AL, Goldstein RS, Chan C, et al. Postural deviations in individuals with chronic obstructive pulmonary disease (COPD). Can J Respir Crit Care Sleep Med. 2018;2(2):61–68. doi: 10.1080/24745332.2017.1409091.
- Heneghan N, Adab P, Jackman S, et al. Musculoskeletal dysfunction in chronic obstructive pulmonary disease (COPD): an observational study. Int J Ther Rehabil. 2015;22(3):119–128. doi: 10.12968/ijtr.2015.22.3.119.
- Morais N, Cruz J, Marques A. Posture and mobility of the upper body quadrant and pulmonary function in COPD: an exploratory study. Braz J Phys Ther. 2016;20(4):345–354. doi: 10.1590/bjpt-rbf.2014.0162.
- Putt MT, Watson M, Seale H, et al. Muscle stretching technique increases vital capacity and range of motion in patients with chronic obstructive pulmonary disease. Arch Phys Med Rehabil. 2008;89(6):1103–1107. doi: 10.1016/j.apmr.2007.11.033.
- Hegedus EJ, Goode AP, Cook CE, et al. Which physical examination tests provide clinicians with the most value when examining the shoulder? Update of a systematic review with meta-analysis of individual tests. Br J Sports Med. 2012;46(14):964. doi: 10.1136/bjsports-2012-091066.
- Simpson R, Gemmell H. Accuracy of spinal orthopaedic tests: a systematic review. Chiropr Osteopat. 2006;14(1):26.
- Frayer DW, Lozano M, Bermúdez de Castro JM, et al. More than 500,000 years of right-handedness in Europe. Laterality. 2012;17(1):51–69. doi: 10.1080/1357650X.2010.529451.
- Edmondston SJ, Christensen MM, Keller S, et al. Functional radiographic analysis of thoracic spine extension motion in asymptomatic men. J Manipulative Physiol Ther. 2012;35(3):203–208. doi: 10.1016/j.jmpt.2012.01.008.
- Edmondston SJ, Ferguson A, Ippersiel P, et al. Clinical and radiological investigation of thoracic spine extension motion during bilateral arm elevation. J Orthop Sports Phys Ther. 2012;42(10):861–869. doi: 10.2519/jospt.2012.4164.
- Morais N, Cruz J. The pectoralis minor muscle and shoulder movement-related impairments and pain: rationale, assessment and management. Phys Ther Sport. 2016;17:1–13. doi: 10.1016/j.ptsp.2015.10.003.
- Greenfield B, Catlin PA, Coats PW, et al. Posture in patients with shoulder overuse injuries and healthy individuals. J Orthop Sports Phys Ther. 1995;21(5):287–295. doi: 10.2519/jospt.1995.21.5.287.
- Maroco J. Análise Estatística com Utilização do SPSS. 3a Edição ed. Lisboa: Sílabo, Lda; 2007.
- Dias Cu S, Kirkwood RN, Parreira VnF, et al. Orientation and position of the scapula, head and kyphosis thoracic in male patients with COPD. Can J Respir Ther. 2009;45( 2):30–34.
- Jacono FJ. Control of ventilation in COPD and lung injury. Respir Physiol Neurobiol. 2013;189(2):371–376. doi: 10.1016/j.resp.2013.07.010.
- Decramer M. Hyperinflation and respiratory muscle interaction. Eur Respir J. 1997;10(4):934–941.
- Hodges PW, Gandevia SC. Activation of the human diaphragm during a repetitive postural task. J Physiol (Lond). 2000;522 Pt 1:165–175. doi: 10.1111/j.1469-7793.2000.t01-1-00165.xm.
- Shirley D, Hodges PW, Eriksson AEM, et al. Spinal stiffness changes throughout the respiratory cycle. J Appl Physiol. 2003;95(4):1467–1475. doi: 10.1152/japplphysiol.00939.2002.
- Kolar P, Sulc J, Kyncl M, et al. Stabilizing function of the diaphragm: dynamic MRI and synchronized spirometric assessment. J Appl Physiol. 2010;109(4):1064–1071. doi: 10.1152/japplphysiol.01216.2009.
- Spruit MA, Singh SJ, Garvey C, et al. An official American thoracic society/European respiratory society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):e13–e64.
- Barrett E, O’Keeffe M, O’Sullivan K, et al. Is thoracic spine posture associated with shoulder pain, range of motion and function? A systematic review. Man Ther. 2016;26:38–46. doi: 10.1016/j.math.2016.07.008.
- Cruz-Montecinos C, Godoy-Olave D, Contreras-Briceño FA, et al. The immediate effect of soft tissue manual therapy intervention on lung function in severe chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2017;12:691–696. doi: 10.2147/COPD.S127742.
- Clarke S, Munro EP, Lee LA. The role of manual therapy in patients with COPD. Healthcare (Basal). 2019;7(1). Pii: E21.
- Simonelli C, Vitacca M, Vignoni M, et al. Effectiveness of manual therapy in COPD: a systematic review of randomised controlled trials. Pulmonology. 2019. In press https://www.ncbi.nlm.nih.gov/pubmed/30738792 | https://www.sciencedirect.com/science/article/pii/S2531043719300078?via%3Dihub. No volume and page range yet available, although the number of pages is already known (#12)
- Janaudis-Ferreira T, Hill K, Goldstein RS, et al. Relationship and responsiveness of three upper-limb tests in patients with chronic obstructive pulmonary disease. Physiother Can. 2013;65(1):40–43. doi: 10.3138/ptc.2011-49.
- Raine S, Twomey LT. Head and shoulder posture variations in 160 asymptomatic women and men. Arch Phys Med Rehabil. 1997;78(11):1215–1223.
- Groot JH, Brand R. A three-dimensional regression model of the shoulder rhythm. Clin Biomech. 2001;16(9):735–743. doi: 10.1016/S0268-0033(01)00065-1.
